Help-Seeking as a Maladaptive Coping Style in the Pandemic Scenario: What Worked and What Did Not for Facing This New Stressor
Abstract
:1. Introduction
1.1. Understanding How to Cope with Lockdown-Related Stress Is Fundamental
1.2. Alternative Strategies Suggested by Public Health Institutes
1.3. The Present Research
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Measures
2.4. Data Analysis
3. Results
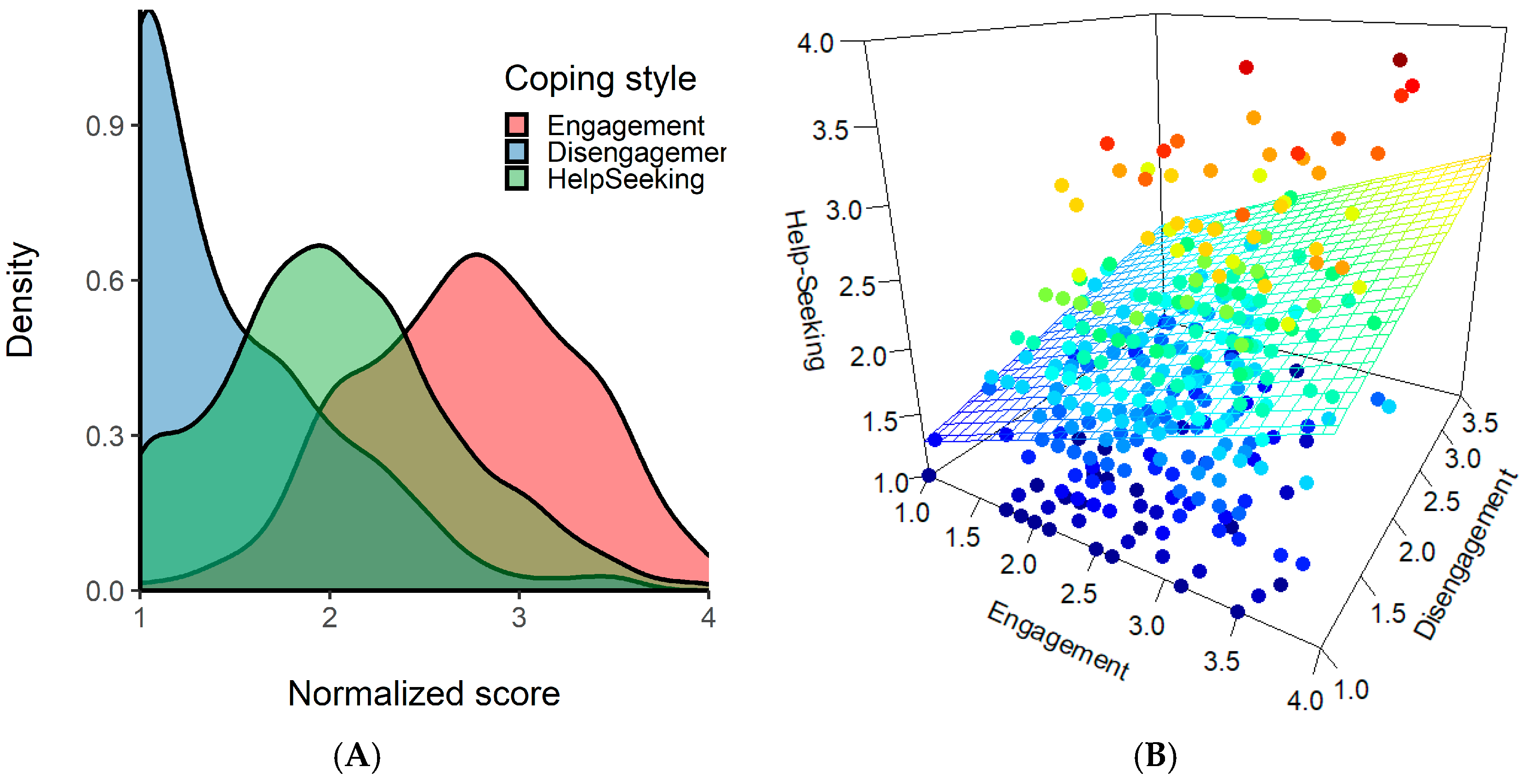
3.1. Descriptive Statistics
3.2. Brief-COPE Factor Structure
3.3. Relationships between Coping, Socio-Demographic, and Psychological Variables
3.4. Control Analysis on Help-Seeking: The Role of Venting
4. Discussion
4.1. Help-Seeking as a Maladaptive Coping Style during the Lockdown
4.2. Pandemic and Lockdown Were Faced as Traumatic Events
4.3. Effectiveness of Alternative Coping Strategies and Activities
4.4. Effect of Housing Condition and Stressful Events
4.5. Limitations of Our Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Remuzzi, A.; Remuzzi, G. COVID-19 and Italy: What Next? Lancet 2020, 395, 1225–1228. [Google Scholar] [CrossRef]
- Ho, C.S.H.; Chee, C.Y.I.; Ho, R.C.M. Mental Health Strategies to Combat the Psychological Impact of COVID-19 beyond Paranoia and Panic. Ann. Acad. Med. Singap. 2020, 49, 1–6. [Google Scholar]
- Khalid, I.; Khalid, T.J.; Qabajah, M.R.; Barnard, A.G.; Qushmaq, I.A. Healthcare Workers Emotions, Perceived Stressors and Coping Strategies during a MERS-CoV Outbreak. Clin. Med. Res. 2016, 14, 7–14. [Google Scholar] [CrossRef] [Green Version]
- Shear, M.K. Grief and Mourning Gone Awry: Pathway and Course of Complicated Grief. Dialogues Clin. Neurosci. 2012, 14, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Liu, N.; Zhang, F.; Wei, C.; Jia, Y.; Shang, Z.; Sun, L.; Wu, L.; Sun, Z.; Zhou, Y.; Wang, Y.; et al. Prevalence and Predictors of PTSS during COVID-19 Outbreak in China Hardest-Hit Areas: Gender Differences Matter. Psychiatry Res. 2020, 287, 112921. [Google Scholar] [CrossRef] [PubMed]
- Ajlouni, A.O.; Almahaireh, A.S. Relationship Between Coronavirus-Related Anxiety and Coronavirus-Related Anxiety and Optimism Among Undergraduates At the University of Jordan. J. Crit. Rev. 2020, 9, 19. [Google Scholar] [CrossRef]
- Kar, N.; Kar, B.; Kar, S. Stress and Coping during COVID-19 Pandemic: Result of an Online Survey. Psychiatry Res. 2021, 295, 113598. [Google Scholar] [CrossRef]
- Choi, E.P.H.; Hui, B.P.H.; Wan, E.Y.F. Depression and Anxiety in Hong Kong during COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 3740. [Google Scholar] [CrossRef]
- D′Agostino, A.; D’Angelo, S.; Giordano, B.; Cigognini, A.C.; Chirico, M.L.; Redaelli, C.; Gambini, O. Brief Psychotic Disorder During the National Lockdown in Italy: An Emerging Clinical Phenomenon of the COVID-19 Pandemic. Schizophr. Bull. 2021, 47, 15–22. [Google Scholar] [CrossRef]
- Hawryluck, L.; Gold, W.L.; Robinson, S.; Pogorski, S.; Galea, S.; Styra, R. SARS Control and Psychological Effects of Quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004, 10, 1206–1212. [Google Scholar] [CrossRef] [PubMed]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Cohen Silver, R.; Everall, I.; et al. Multidisciplinary Research Priorities for the COVID-19 Pandemic: A Call for Action for Mental Health Science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer Publishing Company: Berlin/Heidelberg, Germany, 1984; ISBN 0826141900. [Google Scholar]
- McIlvane, J.M. Disentangling the Effects of Race and SES on Arthritis-Related Symptoms, Coping, and Well-Being in African American and White Women. Aging Ment. Health 2007, 11, 556–569. [Google Scholar] [CrossRef] [PubMed]
- Carver, C.S.; Scheier, M.F. Situational Coping and Coping Dispositions in a Stressful Transaction. J. Personal. Soc. Psychol. 1994, 66, 184–195. [Google Scholar] [CrossRef]
- Clarke, A.T. Coping with Interpersonal Stress and Psychosocial Health among Children and Adolescents: A Meta-Analysis. J. Youth Adolesc. 2006, 35, 11–24. [Google Scholar] [CrossRef]
- Carver, C.S.; Scheier, M.F.; Weintraub, K.J. Assessing Coping Strategies: A Theoretically Based Approach. J. Personal. Soc. Psychol. 1989, 56, 267–283. [Google Scholar] [CrossRef]
- Charles, S. Carver You Want to Measure Coping but Your Protocol’s Too Long: Consider the Brief COPE. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar]
- Ben-Zur, H. Coping Styles and Affect. Int. J. Stress Manag. 2009, 16, 87–101. [Google Scholar] [CrossRef]
- Litman, J.A. The COPE Inventory: Dimensionality and Relationships with Approach- and Avoidance-Motives and Positive and Negative Traits. Personal. Individ. Differ. 2006, 41, 273–284. [Google Scholar] [CrossRef]
- Gutiérrez, F.; Peri, J.M.; Torres, X.; Caseras, X.; Valdés, M. Three Dimensions of Coping and a Look at Their Evolutionary Origin. J. Res. Personal. 2007, 41, 1032–1053. [Google Scholar] [CrossRef]
- Canestrari, C.; Bongelli, R.; Fermani, A.; Riccioni, I.; Bertolazzi, A.; Muzi, M.; Burro, R. Coronavirus Disease Stress Among Italian Healthcare Workers: The Role of Coping Humor. Front. Psychol. 2021, 11. [Google Scholar] [CrossRef] [PubMed]
- Rettie, H.; Daniels, J. Coping and Tolerance of Uncertainty: Predictors and Mediators of Mental Health during the COVID-19 Pandemic. Am. Psychol. 2020, 76, 427–437. [Google Scholar] [CrossRef] [PubMed]
- Shamblaw, A.L.; Rumas, R.L.; Best, M.W. Coping during the COVID-19 Pandemic: Relations with Mental Health and Quality of Life. Can. Psychol. Can. 2021, 62, 92–100. [Google Scholar] [CrossRef]
- Grey, I.; Arora, T.; Thomas, J.; Saneh, A.; Tomhe, P.; Abi-Habib, R. The Role of Perceived Social Support on Depression and Sleep during the COVID-19 Pandemic. Psychiatry Res. 2020, 293, 113452. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Li, M.; Li, Z.; Xiang, W.; Yuan, Y.; Liu, Y.; Li, Z.; Xiong, Z. Coping Style, Social Support and Psychological Distress in the General Chinese Population in the Early Stages of the COVID-19 Epidemic. BMC Psychiatry 2020, 20, 1–11. [Google Scholar] [CrossRef]
- Qi, M.; Zhou, S.J.; Guo, Z.C.; Zhang, L.G.; Min, H.J.; Li, X.M.; Chen, J.X. The Effect of Social Support on Mental Health in Chinese Adolescents During the Outbreak of COVID-19. J. Adolesc. Health 2020, 67, 514–518. [Google Scholar] [CrossRef]
- Li, F.; Luo, S.; Mu, W.; Li, Y.; Ye, L.; Zheng, X.; Xu, B.; Ding, Y.; Ling, P.; Zhou, M.; et al. Effects of Sources of Social Support and Resilience on the Mental Health of Different Age Groups during the COVID-19 Pandemic. BMC Psychiatry 2021, 21, 1–14. [Google Scholar] [CrossRef]
- Saltzman, L.Y.; Hansel, T.C.; Bordnick, P.S. Loneliness, Isolation, and Social Support Factors in Post-COVID-19 Mental Health. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, S55–S57. [Google Scholar] [CrossRef]
- Ye, Z.; Yang, X.; Zeng, C.; Wang, Y.; Shen, Z.; Li, X.; Lin, D. Resilience, Social Support, and Coping as Mediators between COVID-19-Related Stressful Experiences and Acute Stress Disorder among College Students in China. Appl. Psychol. Health Well-Being 2020, 12, 1074–1094. [Google Scholar] [CrossRef]
- World Health Organization Coping with Stress during the 2019-NCoV Outbreak. Available online: https://www.who.int/docs/default-source/coronaviruse/coping-with-stress.pdf?sfvrsn=9845bc3a_8 (accessed on 1 November 2021).
- Ozbay, F.; Johnson, D.C.; Dimoulas, E.; Morgan, C.A.; Charney, D.; Southwick, S. Social Support and Resilience to Stress: From Neurobiology to Clinical Practice. Psychiatry 2007, 4, 35–40. [Google Scholar]
- Ministero della Salute Italiano Gestire lo Stress ai Tempi di COVID-19. Available online: Salute.gov.it/portale/nuovocoronavirus/dettaglioNotizieNuovoCoronavirus.jsp?lingua=italiano&menu=notizie&p=dalministero&id=4229 (accessed on 1 November 2021).
- Hanfstingl, B.; Gnambs, T.; Fazekas, C.; Gölly, K.I.; Matzer, F.; Tikvić, M. The Dimensionality of the Brief COPE before and during the COVID-19 Pandemic. Assessment 2021. [Google Scholar] [CrossRef] [PubMed]
- Simione, L.; Gnagnarella, C. Differences between Health Workers and General Population in Risk Perception, Behaviors, and Psychological Distress Related to COVID-19 Spread in Italy. Front. Psychol. 2020, 11, 2166. [Google Scholar] [CrossRef]
- Shigemura, J.; Ursano, R.J.; Morganstein, J.C.; Kurosawa, M.; Benedek, D.M. Public Responses to the Novel 2019 Coronavirus (2019-nCoV) in Japan: Mental Health Consequences and Target Populations. Psychiatry Clin. Neurosci. 2020, 74, 281–282. [Google Scholar] [CrossRef]
- Trnka, R.; Lorencova, R. Fear, Anger, and Media-Induced Trauma During the Outbreak of COVID-19 in the Czech Republic. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, 546–549. [Google Scholar] [CrossRef]
- Lopes, B.; Bortolon, C.; Jaspal, R. Paranoia, Hallucinations and Compulsive Buying during the Early Phase of the COVID-19 Outbreak in the United Kingdom: A Preliminary Experimental Study. Psychiatry Res. 2020, 293, 113455. [Google Scholar] [CrossRef]
- Wang, A.W.T.; Cheng, C.P.; Chang, C.S.; Chen, D.R.; Chen, S.T.; Shieh, V.; Lo, A.; Hsu, W.Y. Does the Factor Structure of the Brief COPE Fit Different Types of Traumatic Events?: A Test of Measurement Invariance. Eur. J. Psychol. Assess. 2018, 34, 162–173. [Google Scholar] [CrossRef]
- Monzani, D.; Steca, P.; Greco, A.; D’Addario, M.; Cappelletti, E.; Pancani, L. The Situational Version of the Brief COPE: Dimensionality and Relationships with Goal-Related Variables. Eur. J. Psychol. 2015, 11, 295–310. [Google Scholar] [CrossRef]
- Eisinga, R.; Grotenhuis, M.T.; Pelzer, B. The Reliability of a Two-Item Scale: Pearson, Cronbach, or Spearman-Brown? Int. J. Public Health 2013, 58, 637–642. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 2006, 24, 385. [Google Scholar] [CrossRef]
- Marteau, T.M.; Bekker, H. The Development of a Six-item Short-form of the State Scale of the Spielberger State—Trait Anxiety Inventory (STAI). Br. J. Clin. Psychol. 1992, 31, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Piccinelli, M.; Politi, P. Struttura Fattoriale Della Versione a 12 Domande Del General Health Questionnaire in Un Campione Di Giovani Maschi Adulti. Epidemiol. Psichiatr. Soc. 1993, 2, 173–181. [Google Scholar] [CrossRef]
- van Bruggen, V.; ten Klooster, P.; Westerhof, G.; Vos, J.; de Kleine, E.; Bohlmeijer, E.; Glas, G. The Existential Concerns Questionnaire (ECQ)–Development and Initial Validation of a New Existential Anxiety Scale in a Nonclinical and Clinical Sample. J. Clin. Psychol. 2017, 73, 1692–1703. [Google Scholar] [CrossRef]
- Prunas, A.; Sarno, I.; Preti, E.; Madeddu, F.; Perugini, M. Psychometric Properties of the Italian Version of the SCL-90-R: A Study on a Large Community Sample. Eur. Psychiatry 2012, 27, 591–597. [Google Scholar] [CrossRef]
- Holmes, T.H.; Rahe, R.H. The Social Readjustment Rating Scale. J. Psychosom. Res. 1967, 11, 213–218. [Google Scholar] [CrossRef]
- Goldberg, D.P.; Gater, R.; Sartorius, N.; Ustun, T.B.; Piccinelli, M.; Gureje, O.; Rutter, C. The Validity of Two Versions of the GHQ in the WHO Study of Mental Illness in General Health Care. Psychol. Med. 1997, 27, 191–197. [Google Scholar] [CrossRef]
- Cohen, J.; Cohen, P.; West, S.G.; Aiken, L.S. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences, 3rd ed.; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 2003; ISBN 0-8058-2223-2. [Google Scholar]
- Nielsen, M.B.; Knardahl, S. Coping Strategies: A Prospective Study of Patterns, Stability, and Relationships with Psychological Distress. Scand. J. Psychol. 2014, 55, 142–150. [Google Scholar] [CrossRef]
- Skinner, E.A.; Edge, K.; Altman, J.; Sherwood, H. Searching for the Structure of Coping: A Review and Critique of Category Systems for Classifying Ways of Coping. Psychol. Bull. 2003, 129, 216–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biondi, M.; Iannitelli, A. COVID-19 and Stress in the Pandemic: “Sanity Is Not Statistical”. Riv. Psichiatr. 2020, 55, E1–E6. [Google Scholar] [CrossRef]
- Schwarzer, R.; Leppin, A. Social Support and Health: A Theoretical and Empirical Overview. J. Soc. Personal. Relatsh. 1991, 8, 99–127. [Google Scholar] [CrossRef]
- Penley, J.A.; Tomaka, J.; Wiebe, J.S. The Association of Coping to Physical and Psychological Health Outcomes: A Meta-Analytic Review. J. Behav. Med. 2002, 25, 551–603. [Google Scholar] [CrossRef] [PubMed]
- Tahara, M.; Mashizume, Y.; Takahashi, K. Coping Mechanisms: Exploring Strategies Utilized by Japanese Healthcare Workers to Reduce Stress and Improve Mental Health during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 131. [Google Scholar] [CrossRef]
- Yao, M.Z.; Zhong, Z.J. Loneliness, Social Contacts and Internet Addiction: A Cross-Lagged Panel Study. Comput. Hum. Behav. 2014, 30, 164–170. [Google Scholar] [CrossRef]
- Chong, Y.Y.; Chien, W.T.; Cheng, H.Y.; Lamnisos, D.; Ļubenko, J.; Presti, G.; Squatrito, V.; Constantinou, M.; Nicolaou, C.; Papacostas, S.; et al. Patterns of Psychological Responses among the Public during the Early Phase of COVID-19: A Cross-Regional Analysis. Int. J. Environ. Res. Public Health 2021, 18, 4143. [Google Scholar] [CrossRef] [PubMed]
- Stanisławski, K. The Coping Circumplex Model: An Integrative Model of the Structure of Coping with Stress. Front. Psychol. 2019, 10, 694. [Google Scholar] [CrossRef] [PubMed]
- Gurvich, C.; Thomas, N.; Thomas, E.H.X.; Hudaib, A.R.; Sood, L.; Fabiatos, K.; Sutton, K.; Isaacs, A.; Arunogiri, S.; Sharp, G.; et al. Coping Styles and Mental Health in Response to Societal Changes during the COVID-19 Pandemic. Int. J. Soc. Psychiatry 2020. [Google Scholar] [CrossRef] [PubMed]
- Pyszczynski, T.; Lockett, M.; Greenberg, J.; Solomon, S. Terror Management Theory and the COVID-19 Pandemic. J. Humanist. Psychol. 2021, 61, 173–189. [Google Scholar] [CrossRef]
- Alcover, C.M.; Rodríguez, F.; Pastor, Y.; Thomas, H.; Rey, M.; Del Barrio, J.L. Group Membership and Social and Personal Identities as Psychosocial Coping Resources to Psychological Consequences of the COVID-19 Confinement. Int. J. Environ. Res. Public Health 2020, 17, 7413. [Google Scholar] [CrossRef]
- Margetić, B.; Peraica, T.; Stojanović, K.; Ivanec, D. Predictors of Emotional Distress during the COVID-19 Pandemic; a Croatian Study. Personal. Individ. Differ. 2021, 175, 110691. [Google Scholar] [CrossRef]
- Stewart, D.E.; Appelbaum, P.S. COVID-19 and Psychiatrists’ Responsibilities: A WPA Position Paper. World Psychiatry 2020, 19, 406–407. [Google Scholar] [CrossRef]
- McDaid, D. Viewpoint: Investing in Strategies to Support Mental Health Recovery from the COVID-19 Pandemic. Eur. Psychiatry 2021, 64, 28. [Google Scholar] [CrossRef]
- Duan, H.; Yan, L.; Ding, X.; Gan, Y.; Kohn, N.; Wu, J. Impact of the COVID-19 Pandemic on Mental Health in the General Chinese Population: Changes, Predictors and Psychosocial Correlates. Psychiatry Res. 2020, 293, 113396. [Google Scholar] [CrossRef]
- Zhu, Z.; Xu, S.; Wang, H.; Liu, Z.; Wu, J.; Li, G.; Miao, J.; Zhang, C.; Yang, Y.; Sun, W.; et al. COVID-19 in Wuhan: Sociodemographic Characteristics and Hospital Support Measures Associated with the Immediate Psychological Impact on Healthcare Workers. EClinicalMedicine 2020, 24, 100443. [Google Scholar] [CrossRef] [PubMed]
- Scully, D. Physical Exercise and Psychological Well Being: A Critical Review. Br. J. Sports Med. 1998, 32, 111–120. [Google Scholar] [CrossRef] [Green Version]
- Prati, G. Mental Health and Its Psychosocial Predictors during National Quarantine in Italy against the Coronavirus Disease 2019 (COVID-19). Anxiety Stress Coping 2021, 34, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.; Lau, H.P.B.; Chan, M.P.S. Coping Flexibility and Psychological Adjustment to Stressful Life Changes: A Meta-Analytic Review. Psychol. Bull. 2014, 140, 1582–1607. [Google Scholar] [CrossRef] [Green Version]
- Kato, T. Development of the Coping Flexibility Scale: Evidence for the Coping Flexibility Hypothesis. J. Couns. Psychol. 2012, 59, 262–273. [Google Scholar] [CrossRef] [PubMed]
- Wadsworth, M.E. Development of Maladaptive Coping: A Functional Adaptation to Chronic, Uncontrollable Stress. Child Dev. Perspect. 2015, 9, 96–100. [Google Scholar] [CrossRef] [PubMed]
| Variable | Mean | SD | Skewness | Kurtosis | Cronbach’α | Outliers | |
|---|---|---|---|---|---|---|---|
| Demographics and others | Age | 40.99 | 11.04 | - | - | - | - |
| Education (in years) | 15.08 | 4.09 | - | - | - | - | |
| Physical condition | 0.27 | 0.61 | - | - | - | - | |
| Stress factors | HDI (house distress index) | 1.38 | 1.53 | - | - | - | - |
| HR stressful events | 113.9 | 73.13 | - | - | - | 4 | |
| Time spent in… | Training outdoor | 0.30 | 0.68 | - | - | - | - |
| Training at home | 0.98 | 0.98 | - | - | - | - | |
| Hobby and fun | 1.29 | 0.96 | - | - | - | - | |
| Relaxing activity | 0.45 | 0.81 | - | - | - | - | |
| Taking care of family | 1.91 | 1.12 | - | - | - | - | |
| Brief COPE | Self-distraction | 5.14 | 1.57 | −0.08 | −0.63 | 0.48 | - |
| Active coping | 5.17 | 1.56 | −0.07 | −0.66 | 0.63 | - | |
| Denial | 3.02 | 1.46 | 1.54 | 1.75 | 0.78 | - | |
| Substance use | 2.18 | 0.71 | 5.13 | 30.86 | 0.91 | - | |
| Use of emotional support | 3.97 | 1.55 | 0.56 | −0.21 | 0.86 | - | |
| Use of instrumental support | 3.98 | 1.47 | 0.55 | −0.01 | 0.72 | - | |
| Behavioral disengagement | 2.89 | 1.15 | 1.31 | 1.44 | 0.54 | - | |
| Venting | 4.23 | 1.31 | 0.14 | −0.38 | 0.49 | - | |
| Positive reframing | 5.13 | 1.60 | 0.01 | −0.72 | 0.76 | - | |
| Planning | 5.31 | 1.61 | −0.13 | −0.70 | 0.71 | - | |
| Humor | 3.61 | 1.34 | 0.71 | 0.01 | 0.56 | - | |
| Acceptance | 6.29 | 1.49 | −0.55 | −0.38 | 0.80 | - | |
| Religion | 3.41 | 1.68 | 1.00 | 0.03 | 0.84 | - | |
| Self-blame | 3.74 | 1.13 | 0.77 | 1.06 | 0.33 | - | |
| Psychological symptoms | PSS | 19.33 | 6.63 | 0.14 | −0.26 | 0.81 | - |
| STAI | 14.27 | 4.24 | 0.03 | −0.78 | 0.87 | - | |
| ECQ Death anxiety | 8.63 | 5.70 | 0.35 | −0.91 | 0.90 | - | |
| GHQ | 16.77 | 4.86 | −0.23 | −0.10 | 0.86 | - | |
| SCL-90R Som | 14.06 | 10.46 | 0.79 | −0.09 | 0.91 | 1 | |
| SCL-90R Hos | 4.48 | 4.05 | 1.23 | 1.08 | 0.85 | 3 | |
| SCL-90R Psy | 5.38 | 5.66 | 1.31 | 1.06 | 0.81 | 6 | |
| SCL-90R Par | 4.90 | 4.58 | 1.02 | 0.34 | 0.84 | 4 |
| Factor 1 | Factor 2 | Factor 3 | ||
|---|---|---|---|---|
| Brief COPE Scale | Engagement | Help-Seeking | Disengagement | Uniqueness |
| Acceptance | 0.70 | −0.14 | −0.12 | 0.50 |
| Positive reframing | 0.70 | 0.10 | −0.09 | 0.48 |
| Planning | 0.69 | 0.25 | −0.09 | 0.41 |
| Humor | 0.65 | −0.31 | 0.38 | 0.42 |
| Active coping | 0.60 | 0.27 | −0.21 | 0.49 |
| Use of instrumental support | 0.05 | 0.86 | 0.03 | 0.24 |
| Use of emotional support | −0.04 | 0.86 | 0.01 | 0.28 |
| Venting | 0.17 | 0.61 | 0.15 | 0.53 |
| Behavioral disengagement | −0.04 | 0.01 | 0.84 | 0.29 |
| Denial | −0.26 | 0.31 | 0.58 | 0.49 |
| Self-distraction | 0.37 | 0.28 | 0.33 | 0.63 |
| Self-blame | 0.40 | 0.25 | 0.31 | 0.64 |
| Religion | 0.23 | 0.34 | −0.08 | 0.81 |
| Substance use | 0.10 | −0.14 | 0.22 | 0.93 |
| Cumulative variance | 0.20 | 0.38 | 0.49 | |
| Proportion explained | 0.37 | 0.40 | 0.23 |
| Engagement | Disengagement | Help-Seeking | |
|---|---|---|---|
| Engagement | - | −0.16 | 0.29 |
| Disengagement | - | - | 0.21 |
| PSS | −0.20 | 0.38 | 0.28 |
| STAI | −0.25 | 0.36 | 0.31 |
| ECQ Death anxiety | −0.06 | 0.34 | 0.27 |
| GHQ | −0.22 | 0.29 | 0.16 |
| SCL-90R Som | −0.05 | 0.29 | 0.28 |
| SCL-90R Hos | −0.10 | 0.20 | 0.20 |
| SCL-90R Psy | −0.13 | 0.41 | 0.27 |
| SCL-90R Par | −0.06 | 0.24 | 0.18 |
| Demographic Variables | Lockdown Activities | Stress Factors | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Age | Edu. | RW | Psychic Condition | Physical Condition | Training Outdoor | Training at Home | Hobby and Fun | Relax | Family | HDI | HR | |
| Engagement | −0.01 | 0.06 | 0.17 | 0.09 | −0.11 | 0.12 | 0.05 | 0.12 | 0.16 | 0.14 | 0.15 | −0.01 | 0.10 |
| Disengagement | 0.07 | 0.09 | −0.20 | −0.10 | 0.17 | 0.11 | 0.02 | −0.08 | −0.19 | −0.01 | −0.08 | 0.05 | 0.17 |
| Help-Seeking | 0.16 | −0.13 | 0.02 | −0.04 | 0.03 | −0.02 | −0.09 | 0.05 | −0.04 | 0.03 | 0.03 | 0.10 | 0.19 |
| PSS | 0.14 | −0.19 | −0.18 | −0.10 | 0.22 | 0.01 | −0.04 | −0.11 | −0.14 | −0.15 | −0.12 | 0.29 | 0.28 |
| STAI | 0.12 | −0.16 | −0.12 | −0.09 | 0.23 | 0.03 | −0.07 | −0.09 | −0.16 | −0.13 | −0.13 | 0.30 | 0.28 |
| ECQ Death anx. | 0.14 | 0.01 | −0.17 | −0.07 | 0.16 | 0.09 | −0.06 | −0.11 | −0.09 | −0.13 | −0.06 | 0.17 | 0.19 |
| GHQ | 0.03 | −0.10 | −0.10 | −0.11 | 0.07 | 0.01 | −0.11 | −0.11 | −0.20 | −0.19 | −0.14 | 0.18 | 0.05 |
| SCL-90R Som | 0.19 | −0.13 | −0.24 | −0.08 | 0.21 | 0.16 | −0.07 | −0.09 | −0.11 | −0.04 | −0.08 | 0.29 | 0.34 |
| SCL-90R Hos | 0.07 | −0.25 | −0.08 | −0.06 | 0.04 | −0.12 | −0.04 | −0.02 | −0.05 | −0.11 | 0.01 | 0.29 | 0.19 |
| SCL-90R Psy | 0.03 | −0.12 | −0.21 | −0.17 | 0.21 | 0.01 | −0.02 | −0.05 | −0.15 | −0.06 | −0.11 | 0.26 | 0.27 |
| SCL-90R Par | 0.10 | −0.12 | −0.22 | −0.14 | 0.11 | −0.07 | −0.06 | −0.04 | −0.15 | −0.10 | −0.07 | 0.28 | 0.25 |
| Engagement | Disengagement | Help-Seeking | |
|---|---|---|---|
| PSS | −0.17 | 0.27 | 0.32 |
| STAI | −0.28 | 0.24 | 0.38 |
| ECQ Death anxiety | −0.06 | 0.21 | 0.28 |
| GHQ | −0.22 | 0.24 | 0.28 |
| SCL-90R Som | −0.07 | 0.17 | 0.28 |
| SCL-90R Hos | −0.08 | 0.16 | 0.19 |
| SCL-90R Psy | −0.10 | 0.32 | 0.30 |
| SCL-90R Par | 0.01 | 0.17 | 0.17 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simione, L.; Gnagnarella, C.; Spina, G.; Bersani, G. Help-Seeking as a Maladaptive Coping Style in the Pandemic Scenario: What Worked and What Did Not for Facing This New Stressor. Int. J. Environ. Res. Public Health 2022, 19, 319. https://doi.org/10.3390/ijerph19010319
Simione L, Gnagnarella C, Spina G, Bersani G. Help-Seeking as a Maladaptive Coping Style in the Pandemic Scenario: What Worked and What Did Not for Facing This New Stressor. International Journal of Environmental Research and Public Health. 2022; 19(1):319. https://doi.org/10.3390/ijerph19010319
Chicago/Turabian StyleSimione, Luca, Camilla Gnagnarella, Giulia Spina, and Giuseppe Bersani. 2022. "Help-Seeking as a Maladaptive Coping Style in the Pandemic Scenario: What Worked and What Did Not for Facing This New Stressor" International Journal of Environmental Research and Public Health 19, no. 1: 319. https://doi.org/10.3390/ijerph19010319
APA StyleSimione, L., Gnagnarella, C., Spina, G., & Bersani, G. (2022). Help-Seeking as a Maladaptive Coping Style in the Pandemic Scenario: What Worked and What Did Not for Facing This New Stressor. International Journal of Environmental Research and Public Health, 19(1), 319. https://doi.org/10.3390/ijerph19010319







