Epidemiological Study of Return to Work and Mortality in Lung Cancer Survivors
Abstract
1. Introduction
2. Materials and Methods
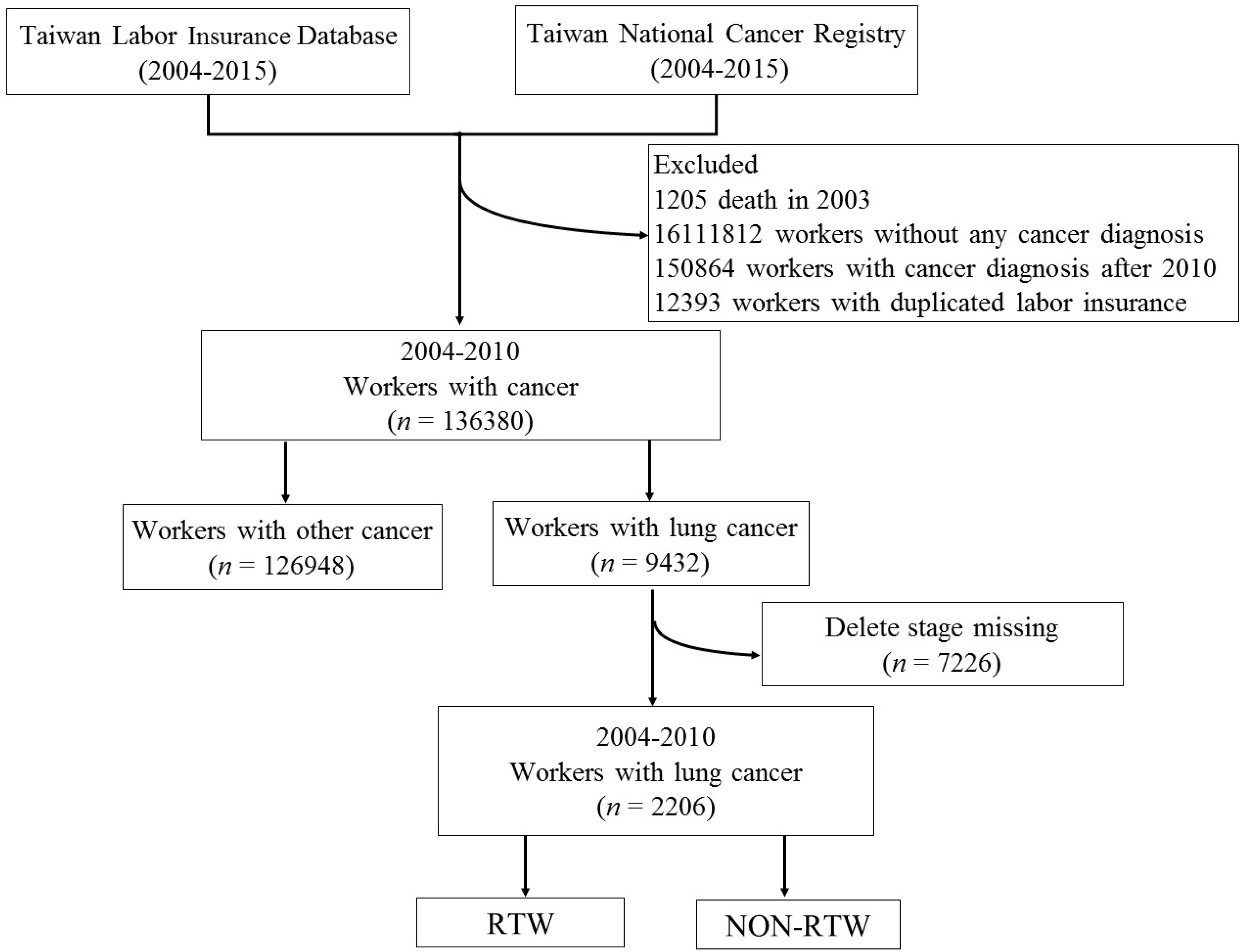
2.1. Study Population and Database
2.2. Sociodemographic and Disease-Related Information
2.3. Outcome Assessment
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Study Population
3.2. Univariate Analysis of Independent Factors Associated with RTW in Cox Proportional Hazards Models
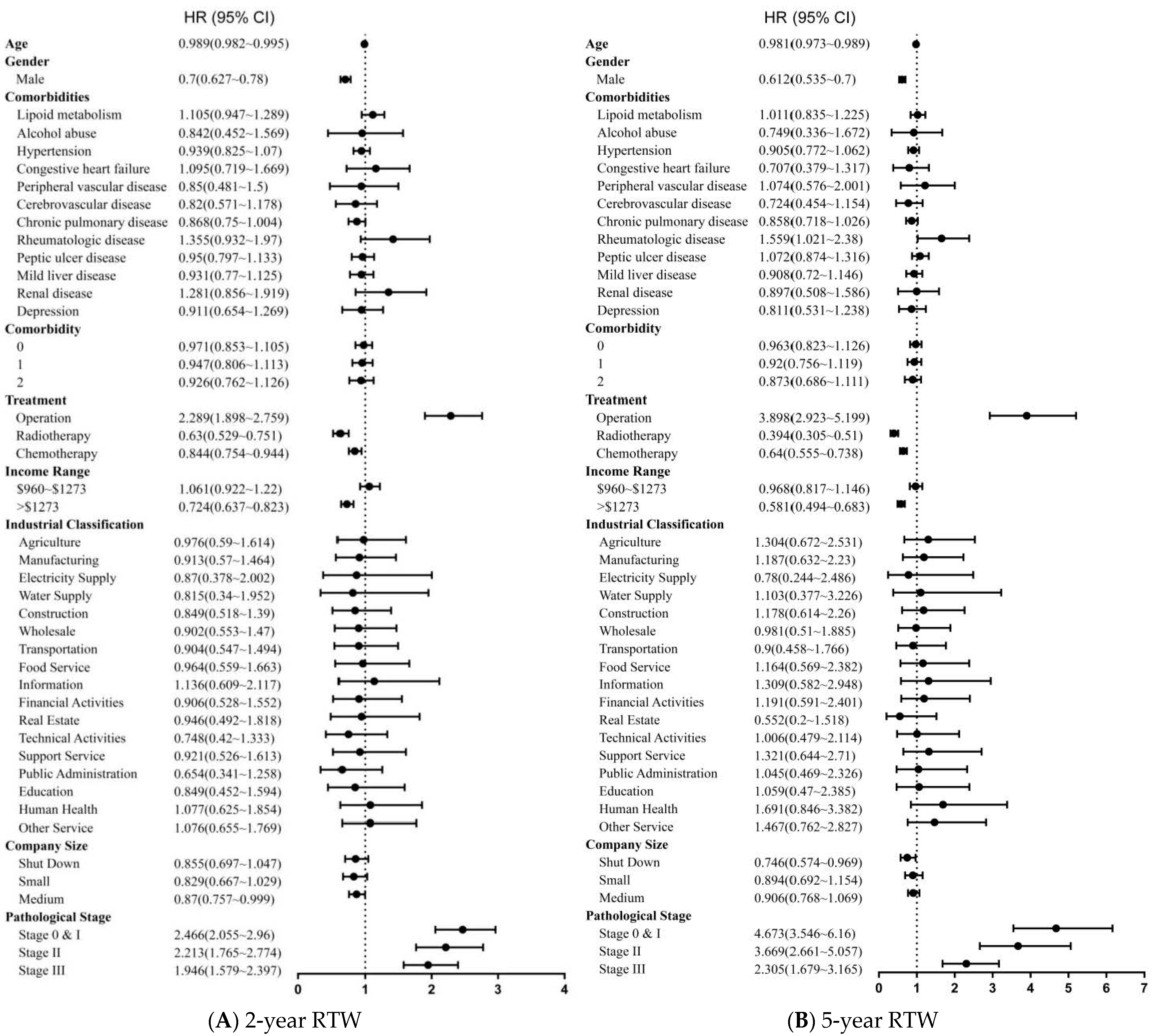
3.3. Multivariate Analysis of Independent Factors Associated with RTW in Cox Proportional Hazards Models
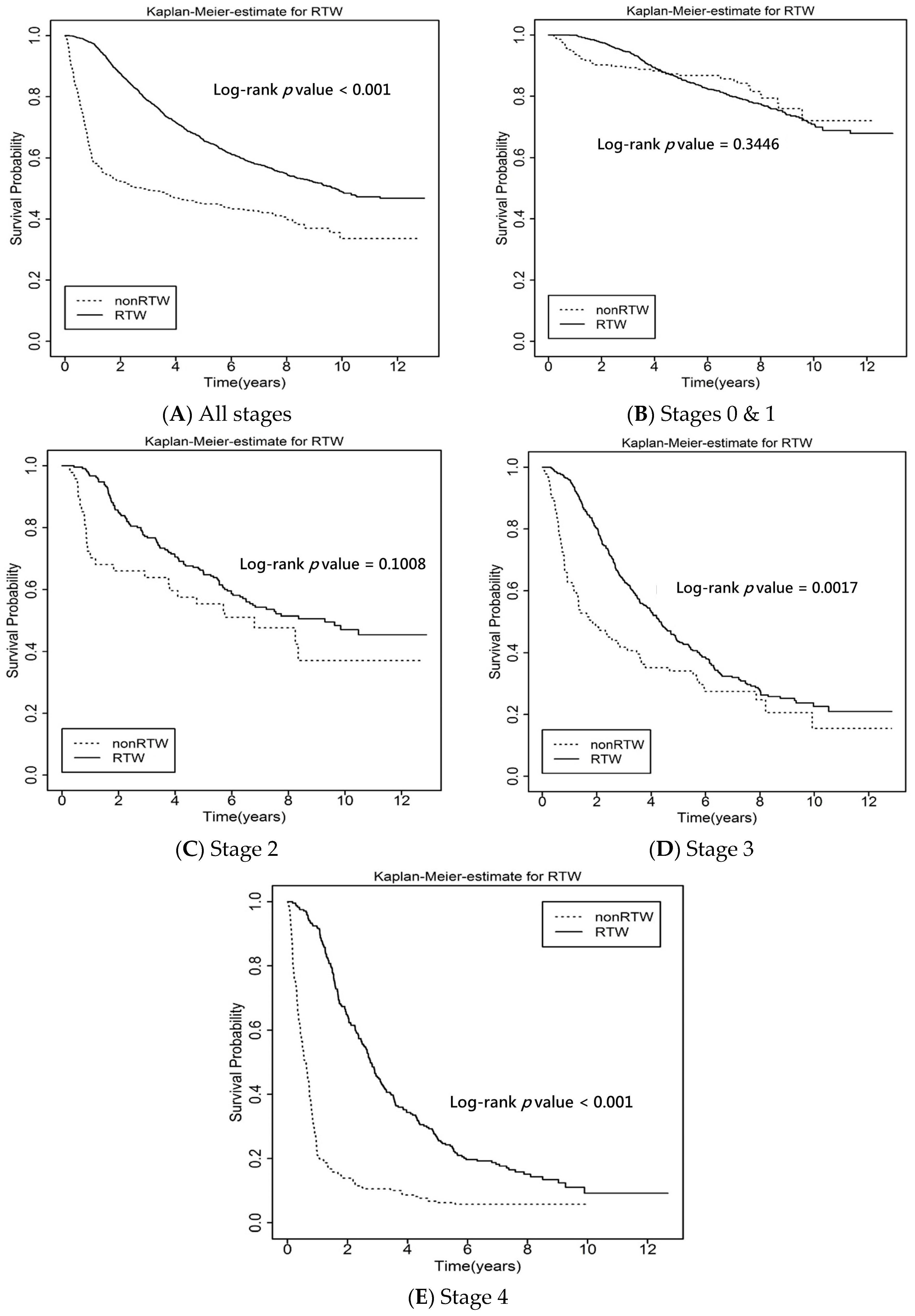
3.4. Survival Rates by RTW and Non-RTW
3.5. Multivariate Analysis of RTW and All-Cause Mortality in Cox Proportional Hazards Models
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics, 2021. CA Cancer J. Clin. 2021, 71, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Malhotra, J.; Malvezzi, M.; Negri, E.; La Vecchia, C.; Boffetta, P. Risk factors for lung cancer worldwide. Eur. Respir. J. 2016, 48, 889–902. [Google Scholar] [CrossRef] [PubMed]
- Torre, L.A.; Siegel, R.L.; Jemal, A. Lung Cancer Statistics. Adv. Exp. Med. Biol. 2016, 893, 1–19. [Google Scholar] [CrossRef]
- Latimer, K.M.; Mott, T.F. Lung cancer: Diagnosis, treatment principles, and screening. Am. Fam. Physician 2015, 91, 250–256. [Google Scholar]
- Chirieac, L.R.; Dacic, S. Targeted Therapies in Lung Cancer. Surg. Pathol. Clin. 2010, 3, 71–82. [Google Scholar] [CrossRef][Green Version]
- Corrales, L.; Scilla, K.; Caglevic, C.; Miller, K.; Oliveira, J.; Rolfo, C. Immunotherapy in Lung Cancer: A New Age in Cancer Treatment. Adv. Exp. Med. Biol. 2018, 995, 65–95. [Google Scholar] [CrossRef]
- Jonas, D.E.; Reuland, D.S.; Reddy, S.M.; Nagle, M.; Clark, S.D.; Weber, R.P.; Enyioha, C.; Malo, T.L.; Brenner, A.T.; Armstrong, C.; et al. Screening for Lung Cancer with Low-Dose Computed Tomography: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2021, 325, 971–987. [Google Scholar] [CrossRef]
- Howlader, N.; Forjaz, G.; Mooradian, M.J.; Meza, R.; Kong, C.Y.; Cronin, K.A.; Mariotto, A.B.; Lowy, D.R.; Feuer, E.J. The Effect of Advances in Lung-Cancer Treatment on Population Mortality. N. Engl. J. Med. 2020, 383, 640–649. [Google Scholar] [CrossRef]
- Polanski, J.; Jankowska-Polanska, B.; Rosinczuk, J.; Chabowski, M.; Szymanska-Chabowska, A. Quality of life of patients with lung cancer. Onco. Targets Ther. 2016, 9, 1023–1028. [Google Scholar] [CrossRef]
- Vijayvergia, N.; Shah, P.C.; Denlinger, C.S. Survivorship in Non-Small Cell Lung Cancer: Challenges Faced and Steps Forward. J. Natl. Compr. Cancer Netw. 2015, 13, 1151–1161. [Google Scholar] [CrossRef] [PubMed]
- Hechtner, M.; Eichler, M.; Wehler, B.; Buhl, R.; Sebastian, M.; Stratmann, J.; Schmidberger, H.; Gohrbandt, B.; Peuser, J.; Kortsik, C.; et al. Quality of Life in NSCLC Survivors—A Multicenter Cross-Sectional Study. J. Thorac. Oncol. 2019, 14, 420–435. [Google Scholar] [CrossRef] [PubMed]
- Khue, P.M.; Thom, V.T.; Minh, D.Q.; Quang, L.M.; Hoa, N.L. Depression and Anxiety as Key Factors Associated with Quality of Life Among Lung Cancer Patients in Hai Phong, Vietnam. Front. Psychiatry 2019, 10. [Google Scholar] [CrossRef] [PubMed]
- Arrieta, O.; Angulo, L.P.; Nunez-Valencia, C.; Dorantes-Gallareta, Y.; Macedo, E.O.; Martinez-Lopez, D.; Alvarado, S.; Corona-Cruz, J.F.; Onate-Ocana, L.F. Association of depression and anxiety on quality of life, treatment adherence, and prognosis in patients with advanced non-small cell lung cancer. Ann. Surg. Oncol. 2013, 20, 1941–1948. [Google Scholar] [CrossRef]
- Nekhlyudov, L.; Walker, R.; Ziebell, R.; Rabin, B.; Nutt, S.; Chubak, J. Cancer survivors’ experiences with insurance, finances, and employment: Results from a multisite study. J. Cancer Surviv. 2016, 10, 1104–1111. [Google Scholar] [CrossRef]
- Carrera, P.M.; Kantarjian, H.M.; Blinder, V.S. The financial burden and distress of patients with cancer: Understanding and stepping-up action on the financial toxicity of cancer treatment. CA Cancer J. Clin. 2018, 68, 153–165. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, S.; Liu, Y.; Du, J.; Fu, W.; Zhao, X.; Huang, W.; Zhao, X.; Liu, G.; Mao, Z.; et al. Economic Burden for Lung Cancer Survivors in Urban China. Int. J. Environ. Res. Public Health 2017, 14, 308. [Google Scholar] [CrossRef]
- Kim, Y.A.; Yun, Y.H.; Chang, Y.J.; Lee, J.; Kim, M.S.; Lee, H.S.; Zo, J.I.; Kim, J.; Choi, Y.S.; Shim, Y.M.; et al. Employment status and work-related difficulties in lung cancer survivors compared with the general population. Ann. Surg. 2014, 259, 569–575. [Google Scholar] [CrossRef]
- Torp, S.; Nielsen, R.A.; Fosså, S.D.; Gudbergsson, S.B.; Dahl, A.A. Change in employment status of 5-year cancer survivors. Eur. J. Public Health 2012, 23, 116–122. [Google Scholar] [CrossRef]
- Sjövall, K.; Attner, B.; Englund, M.; Lithman, T.; Noreen, D.; Gunnars, B.; Thomé, B.; Olsson, H.; Petersson, I.F. Sickness absence among cancer patients in the pre-diagnostic and the post-diagnostic phases of five common forms of cancer. Support. Care Cancer 2012, 20, 741–747. [Google Scholar] [CrossRef]
- Bradburn, M.J.; Clark, T.G.; Love, S.B.; Altman, D.G. Survival analysis part II: Multivariate data analysis--an introduction to concepts and methods. Br. J. Cancer 2003, 89, 431–436. [Google Scholar] [CrossRef]
- Goel, M.K.; Khanna, P.; Kishore, J. Understanding survival analysis: Kaplan-Meier estimate. Int. J. Ayurveda Res. 2010, 1, 274–278. [Google Scholar] [CrossRef]
- van Muijen, P.; Weevers, N.L.; Snels, I.A.; Duijts, S.F.; Bruinvels, D.J.; Schellart, A.J.; van der Beek, A.J. Predictors of return to work and employment in cancer survivors: A systematic review. Eur. J. Cancer Care 2013, 22, 144–160. [Google Scholar] [CrossRef]
- Mehnert, A. Employment and work-related issues in cancer survivors. Crit. Rev. Oncol. Hematol. 2011, 77, 109–130. [Google Scholar] [CrossRef]
- Mehnert, A.; Koch, U. Predictors of employment among cancer survivors after medical rehabilitation—A prospective study. Scand. J. Work Environ. Health 2013, 39, 76–87. [Google Scholar] [CrossRef]
- Kiasuwa Mbengi, R.; Otter, R.; Mortelmans, K.; Arbyn, M.; Van Oyen, H.; Bouland, C.; de Brouwer, C. Barriers and opportunities for return-to-work of cancer survivors: Time for action—Rapid review and expert consultation. Syst. Rev. 2016, 5, 35. [Google Scholar] [CrossRef]
- Earle, C.C.; Chretien, Y.; Morris, C.; Ayanian, J.Z.; Keating, N.L.; Polgreen, L.A.; Wallace, R.; Ganz, P.A.; Weeks, J.C. Employment among survivors of lung cancer and colorectal cancer. J. Clin. Oncol. 2010, 28, 1700–1705. [Google Scholar] [CrossRef] [PubMed]
- Rashid, H.; Eichler, M.; Hechtner, M.; Gianicolo, E.; Wehler, B.; Buhl, R.; Schmidberger, H.; Stratmann, J.A.; Gohrbandt, B.; Kortsik, C.; et al. Returning to work in lung cancer survivors—A multi-center cross-sectional study in Germany. Support. Care Cancer 2021, 29, 3753–3765. [Google Scholar] [CrossRef]
- Taskila, T.; Lindbohm, M.L. Factors affecting cancer survivors’ employment and work ability. Acta. Oncol. 2007, 46, 446–451. [Google Scholar] [CrossRef] [PubMed]
- Hung, M.-C.; Lai, W.-W.; Chen, H.H.W.; Lee, J.-C.; Lin, Y.-J.; Hsiao, J.-R.; Cheng, Y.-M.; Shan, Y.-S.; Su, W.-C.; Wang, J.-D. Cost effectiveness of cancer treatment in Taiwan. J. Formos. Med. Assoc. 2016, 115, 609–618. [Google Scholar] [CrossRef] [PubMed]
- Feuerstein, M.; Todd, B.L.; Moskowitz, M.C.; Bruns, G.L.; Stoler, M.R.; Nassif, T.; Yu, X. Work in cancer survivors: A model for practice and research. J. Cancer Surviv. 2010, 4, 415–437. [Google Scholar] [CrossRef]
- Schmidt, M.E.; Scherer, S.; Wiskemann, J.; Steindorf, K. Return to work after breast cancer: The role of treatment-related side effects and potential impact on quality of life. Eur. J. Cancer Care 2019, 28, e13051. [Google Scholar] [CrossRef] [PubMed]
- Kuroki, L.M.; Morris, D.H.; Greenwade, M.; Landon, M.; Hagemann, A.R.; Thaker, P.H.; Massad, L.S.; McCourt, C.K.; Fuh, K.C.; Powell, M.A.; et al. Impact of employment and insurance status on distress in gynecologic oncology patients. Gynecol. Oncol. 2021, 161, 477–482. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Total | RTW Group | Non-RTW Group | |||||
|---|---|---|---|---|---|---|---|---|
| Number of Patient | % | 2-Year RTW n = 1332 | 5-Year RTW n = 908 | p Value | 2-Year RTW n = 874 | 5-Year RTW n = 1298 | p Value | |
| Age(year) a | 53.5 ± 8.2 (26–91) | - | 52.8 ± 8 (26–81) | 52.3 ± 8 (26–81) | 54.6 ± 8.4 (26–91) | 54.4 ± 8.2 (26–91) | ||
| Gender | ||||||||
| Male | 1095 | 49.63 | 553 | 346 | 0.1059 | 542 | 749 | 0.0449 |
| Comorbidities | ||||||||
| Lipoid metabolism | 289 | 13.1 | 188 | 120 | 0.5445 | 101 | 169 | 0.3106 |
| Alcohol abuse | 20 | 0.9 | 10 | 6 | 0.804 | 10 | 14 | 0.886 |
| Hypertension | 501 | 22.71 | 289 | 191 | 0.708 | 212 | 310 | 0.8417 |
| Congestive heart failure | 34 | 1.54 | 22 | 10 | 0.2812 | 12 | 24 | 0.3942 |
| Peripheral vascular disease | 23 | 1.04 | 12 | 10 | 0.6368 | 11 | 13 | 0.5741 |
| Cerebrovascular disease | 60 | 2.71 | 30 | 18 | 0.665 | 30 | 42 | 0.8017 |
| Chronic pulmonary disease | 396 | 17.95 | 215 | 144 | 0.8582 | 181 | 252 | 0.4589 |
| Rheumatologic disease | 36 | 1.63 | 28 | 22 | 0.6138 | 8 | 14 | 0.7094 |
| Peptic ulcer disease | 240 | 10.87 | 139 | 104 | 0.4467 | 101 | 136 | 0.4292 |
| Mild liver disease | 206 | 9.33 | 117 | 78 | 0.8733 | 89 | 128 | 0.8063 |
| Renal disease | 32 | 1.45 | 24 | 12 | 0.3749 | 8 | 20 | 0.2051 |
| Depression | 65 | 2.94 | 36 | 22 | 0.6823 | 29 | 43 | 0.9946 |
| Comorbidity | ||||||||
| 0 | 1097 | 49.72 | 676 | |||||
| 1 | 578 | 26.2 | 348 | |||||
| 2 | 322 | 14.59 | 189 | |||||
| ≥3 | 209 | 9.47 | 119 | |||||
| Treatment | ||||||||
| OP | 1805 | 81.82 | 1211 | 859 | 0.0012 | 594 | 946 | 0.0133 |
| RTB | 343 | 15.54 | 141 | 62 | 0.0024 | 202 | 281 | 0.4212 |
| CH | 870 | 39.43 | 477 | 272 | 0.0039 | 393 | 598 | 0.6121 |
| Monthly income (USD) | 0.1728 | 0.312 | ||||||
| ≤$960 | 1109 | 50.27 | 715 | 519 | 394 | 590 | ||
| >$960–$1273 | 395 | 17.9 | 270 | 182 | 125 | 213 | ||
| >$1273 | 702 | 31.82 | 347 | 207 | 355 | 495 | ||
| Employee’s industry | 0.9589 | 0.9977 | ||||||
| Agriculture | 154 | 6.98 | 97 | 69 | 57 | 85 | ||
| Manufacturing | 692 | 31.36 | 415 | 290 | 277 | 402 | ||
| Electricity and Gas Supply | 14 | 0.63 | 8 | 4 | 6 | 10 | ||
| Water Supply | 13 | 0.58 | 7 | 5 | 6 | 8 | ||
| Construction | 232 | 10.51 | 129 | 95 | 103 | 137 | ||
| Wholesale and Retail Trade | 254 | 11.51 | 152 | 90 | 102 | 164 | ||
| Transportation and Storage | 168 | 7.61 | 99 | 54 | 69 | 114 | ||
| Food Service | 74 | 3.35 | 46 | 30 | 28 | 44 | ||
| Information | 30 | 1.35 | 22 | 14 | 8 | 16 | ||
| Financial | 82 | 3.71 | 50 | 36 | 32 | 46 | ||
| Real Estate Activities | 29 | 1.31 | 18 | 6 | 11 | 23 | ||
| Technical Activities | 63 | 2.85 | 32 | 23 | 31 | 40 | ||
| Support Service Activities | 63 | 2.85 | 38 | 29 | 25 | 34 | ||
| Public Administration | 40 | 1.81 | 18 | 15 | 22 | 25 | ||
| Education | 36 | 1.63 | 21 | 14 | 15 | 22 | ||
| Human Health | 67 | 3.03 | 47 | 40 | 20 | 27 | ||
| Arts | 28 | 1.26 | 18 | 10 | 10 | 18 | ||
| Other Service Activities | 167 | 7.57 | 115 | 84 | 52 | 83 | ||
| Company size b | 0.8169 | 0.6518 | ||||||
| Company closed | 187 | 8.47 | 104 | 62 | 83 | 125 | ||
| Small | 167 | 7.57 | 90 | 65 | 77 | 102 | ||
| Medium | 260 | 183 | 200 | 277 | ||||
| Large | 878 | 598 | 514 | 794 | ||||
| Pathological stage | <0.0001 | 0.0586 | ||||||
| 0 & I | 1068 | 48.41 | 776 | 611 | 292 | 457 | ||
| II | 257 | 11.65 | 168 | 116 | 89 | 141 | ||
| III | 433 | 19.62 | 252 | 126 | 181 | 307 | ||
| IV | 448 | 20.3 | 136 | 55 | 312 | 393 | ||
| Unadjusted All-Cause Mortality | p | Adjusted All-Cause Mortality | p | |
|---|---|---|---|---|
| RTW | 0.508 (0.447–0.578) | <0.0001 | 0.508 (0.441–0.586) | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Z.-Y.; Lai, C.-H.; Ho, C.-L.; Wang, C.-C. Epidemiological Study of Return to Work and Mortality in Lung Cancer Survivors. Int. J. Environ. Res. Public Health 2022, 19, 309. https://doi.org/10.3390/ijerph19010309
Yang Z-Y, Lai C-H, Ho C-L, Wang C-C. Epidemiological Study of Return to Work and Mortality in Lung Cancer Survivors. International Journal of Environmental Research and Public Health. 2022; 19(1):309. https://doi.org/10.3390/ijerph19010309
Chicago/Turabian StyleYang, Zhe-Yu, Ching-Huang Lai, Ching-Liang Ho, and Chung-Ching Wang. 2022. "Epidemiological Study of Return to Work and Mortality in Lung Cancer Survivors" International Journal of Environmental Research and Public Health 19, no. 1: 309. https://doi.org/10.3390/ijerph19010309
APA StyleYang, Z.-Y., Lai, C.-H., Ho, C.-L., & Wang, C.-C. (2022). Epidemiological Study of Return to Work and Mortality in Lung Cancer Survivors. International Journal of Environmental Research and Public Health, 19(1), 309. https://doi.org/10.3390/ijerph19010309







