Exertional Heat Stroke Knowledge and Management among Emergency Medical Service Providers
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Questionnaire
2.3. Procedures
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Epstein, Y.; Yanovich, R. Heatstroke. N. Engl. J. Med. 2019, 380, 2449–2459. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, L.E.; Casa, D.J.; Millard-Stafford, M.; Moran, D.S.; Pyne, S.W.; Roberts, W.O. American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med. Sci. Sports Exerc. 2007, 39, 556–572. [Google Scholar] [CrossRef] [PubMed]
- Casa, D.J.; DeMartini, J.K.; Bergeron, M.F.; Csillan, D.; Eichner, E.R.; Lopez, R.M.; Ferrara, M.S.; Miller, K.C.; O’Connor, F.; Sawka, M.N.; et al. National Athletic Trainers’ Association Position Statement: Exertional Heat Illnesses. J. Athl. Train. 2015, 50, 986–1000. [Google Scholar] [CrossRef] [PubMed]
- Kerr, Z.Y.; Yeargin, S.W.; Hosokawa, Y.; Hirschhorn, R.M.; Pierpoint, L.A.; Casa, D.J. The Epidemiology and Management of Exertional Heat Illnesses in High School Sports During the 2012/2013-2016/2017 Academic Years. J. Sport Rehabil. 2020, 29, 332–338. [Google Scholar] [CrossRef]
- Yeargin, S.W.; Dompier, T.P.; Casa, D.J.; Hirschhorn, R.M.; Kerr, Z.Y. Epidemiology of Exertional Heat Illnesses in National Collegiate Athletic Association Athletes During the 2009–2010 Through 2014–2015 Academic Years. J. Athl. Train. 2019, 54, 55–63. [Google Scholar] [CrossRef]
- Yeargin, S.W.; Kerr, Z.Y.; Casa, D.J.; Djoko, A.; Hayden, R.; Parsons, J.T.; Dompier, T.P. Epidemiology of Exertional Heat Illnesses in Youth, High School, and College Football. Med. Sci. Sports Exerc. 2016, 48, 1523–1529. [Google Scholar] [CrossRef]
- DeMartini, J.K.; Casa, D.J.; Belval, L.N.; Crago, A.; Davis, R.J.; Jardine, J.J.; Stearns, R.L. Environmental conditions and the occurrence of exertional heat illnesses and exertional heat stroke at the Falmouth Road Race. J. Athl. Train. 2014, 49, 478–485. [Google Scholar] [CrossRef]
- Bureau, Armed Forces Health Surveillance. Update: Heat illness, active component, U.S. Armed Forces, 2019. MSMR 2020, 27, 4–9. [Google Scholar]
- Alele, F.O.; Malau-Aduli, B.S.; Malau-Aduli AEO, J.; Crowe, M. Epidemiology of Exertional Heat Illness in the Military: A Systematic Review of Observational Studies. Int. J. Environ. Res. Public Health 2020, 17, 7037. [Google Scholar] [CrossRef]
- Carter, R., 3rd; Cheuvront, S.N.; Williams, J.O.; Kolka, M.A.; Stephenson, L.A.; Sawka, M.N.; Amoroso, P.J. Epidemiology of hospitalizations and deaths from heat illness in soldiers. Med. Sci. Sports Exerc. 2005, 37, 1338–1344. [Google Scholar] [CrossRef]
- DeGroot, D.W.; Mok, G.; Hathaway, N.E. International Classification of Disease Coding of Exertional Heat Illness in U.S. Army Soldiers. Mil. Med. 2017, 182, e1946–e1950. [Google Scholar] [CrossRef] [PubMed]
- Arbury, S.; Jacklitsch, B.; Farquah, O.; Hodgson, M.; Lamson, G.; Martin, H.; Profitt, A. Heat illness and death among workers—United States, 2012–2013. MMWR Morb. Mortal Wkly. Rep. 2014, 63, 661–665. [Google Scholar] [PubMed]
- Nelson, N.G.; Collins, C.L.; Comstock, R.D.; McKenzie, L.B. Exertional heat-related injuries treated in emergency departments in the U.S., 1997–2006. Am. J. Prev. Med. 2011, 40, 54–60. [Google Scholar] [CrossRef]
- Yeargin, S.; Hirschhorn, R.; Grundstein, A. Heat-Related Illnesses Transported by United States Emergency Medical Services. Medicina (Kaunas) 2020, 56, 543. [Google Scholar] [CrossRef] [PubMed]
- Demartini, J.K.; Casa, D.J.; Stearns, R.; Belval, L.; Crago, A.; Davis, R.; Jardine, J. Effectiveness of cold water immersion in the treatment of exertional heat stroke at the Falmouth Road Race. Med. Sci. Sports Exerc. 2015, 47, 240–245. [Google Scholar] [CrossRef]
- Heled, Y.; Rav-Acha, M.; Shani, Y.; Epstein, Y.; Moran, D.S. The “golden hour” for heatstroke treatment. Mil. Med. 2004, 169, 184–186. [Google Scholar] [CrossRef]
- Casa, D.J.; Armstrong, L.E.; Kenny, G.P.; O’Connor, F.G.; Huggins, R.A. Exertional Heat Stroke: New Concepts Regarding Cause and Care. Curr. Sports Med. Rep. 2012, 11, 115–123. [Google Scholar] [CrossRef]
- Belval, L.N.; Casa, D.J.; Adams, W.M.; Chiampas, G.T.; Holschen, J.C.; Hosokawa, Y.; Jardine, J.; Kane, S.F.; Labotz, M.; Lemieux, R.S.; et al. Consensus Statement- Prehospital Care of Exertional Heat Stroke. Prehosp. Emerg. Care 2018, 22, 392–397. [Google Scholar] [CrossRef]
- Bagley, J.R.; Judelson, D.A.; Spiering, B.A.; Beam, W.C.; Bartolini, J.A.; Washburn, B.V.; Carney, K.R.; Munoz, C.X.; Yeargin, S.W.; Casa, D.J. Validity of field expedient devices to assess core temperature during exercise in the cold. Aviat. Space Environ. Med. 2011, 82, 1098–1103. [Google Scholar] [CrossRef]
- Casa, D.J.; Becker, S.M.; Ganio, M.S.; Brown, C.M.; Yeargin, S.W.; Roti, M.W.; Siegler, J.; Blowers, J.A.; Glaviano, N.R.; Huggins, R.A.; et al. Validity of devices that assess body temperature during outdoor exercise in the heat. J. Athl. Train. 2007, 42, 333–342. [Google Scholar]
- Ganio, M.S.; Brown, C.M.; Casa, D.J.; Becker, S.M.; Yeargin, S.W.; McDermott, B.P.; Boots, L.M.; Boyd, P.W.; Armstrong, L.E.; Maresh, C.M. Validity and reliability of devices that assess body temperature during indoor exercise in the heat. J. Athl. Train. 2009, 44, 124–135. [Google Scholar] [CrossRef]
- Ronneberg, K.; Roberts, W.O.; McBean, A.D.; Center, B.A. Temporal artery temperature measurements do not detect hyperthermic marathon runners. Med. Sci. Sports Exerc. 2008, 40, 1373–1375. [Google Scholar] [CrossRef]
- McDermott, B.P.; Casa, D.J.; Ganio, M.S.; Lopez, R.M.; Yeargin, S.W.; Armstrong, L.E.; Maresh, C.M. Acute whole-body cooling for exercise-induced hyperthermia: A systematic review. J. Athl. Train. 2009, 44, 84–93. [Google Scholar] [CrossRef]
- Filep, E.M.; Murata, Y.; Endres, B.D.; Kim, G.; Stearns, R.L.; Casa, D.J. Exertional Heat Stroke, Modality Cooling Rate, and Survival Outcomes: A Systematic Review. Medicina (Kaunas) 2020, 56, 589. [Google Scholar] [CrossRef]
- Gaudio, F.G.; Grissom, C.K. Cooling Methods in Heat Stroke. J. Emerg. Med. 2016, 50, 607–616. [Google Scholar] [CrossRef] [PubMed]
- Szymanski, M.R.; Scarneo-Miller, S.E.; Smith, M.S.; Bruner, M.L.; Casa, D.J. Emergency Medical Service Directors’ Protocols for Exertional Heat Stroke. Medicina (Kaunas) 2020, 56, 494. [Google Scholar] [CrossRef] [PubMed]
- Mazerolle, S.M.; Scruggs, I.C.; Casa, D.J.; Burton, L.J.; McDermott, B.P.; Armstrong, L.E.; Maresh, C.M. Current knowledge, attitudes, and practices of certified athletic trainers regarding recognition and treatment of exertional heat stroke. J. Athl. Train. 2010, 45, 170–180. [Google Scholar] [CrossRef]
- Rivard, M.K.; Cash, R.E.; Mercer, C.B.; Chrzan, K.; Panchal, A.R. Demography of the National Emergency Medical Services Workforce: A Description of Those Providing Patient Care in the Prehospital Setting. Prehosp. Emerg. Care 2021, 25, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Grundstein, A.J.; Hosokawa, Y.; Casa, D.J. Fatal Exertional Heat Stroke and American Football Players: The Need for Regional Heat-Safety Guidelines. J. Athl. Train. 2018, 53, 43–50. [Google Scholar] [CrossRef]
- National Association of EMS Physicians. A National Strategy to Promote Prehospital Evidence-Based Guideline Development, Implementation, and Evaluation; National Association of EMS Physicians: Overland Park, KS, USA, 2015. [Google Scholar]
- Kerr, Z.Y.; Marshall, S.W.; Comstock, R.D.; Casa, D.J. Exertional heat stroke management strategies in United States high school football. Am. J. Sports Med. 2014, 42, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Nedimyer, A.K.; Chandran, A.; Hirschhorn, R.M.; Adams, W.A.; Pryor, R.R.; Casa, D.J.; Register-Mihalik, J.K.; Kerr, Z.Y. Exertional Heat-Stroke Management Practices and Intentions Among Secondary School Football Athletic Trainers. J. Athl. Train. 2020. [Google Scholar] [CrossRef] [PubMed]
- Boden, B.P.; Breit, I.; Beachler, J.A.; Williams, A.; Mueller, F.O. Fatalities in high school and college football players. Am. J. Sports Med. 2013, 41, 1108–1116. [Google Scholar] [CrossRef] [PubMed]
- Yau, R.; Kucera, K.L.; Thomas, L.C.; Price, H.M.; Cantu, R.C. Catastrophic Sports Injury Research: Thirty-Fifth Annual Report Fall 1982—Spring 2017; National Center for Catastrophic Sport Injury Research: Chapel Hill, NC, USA, 2018. [Google Scholar]
- Vicario, S.J.; Okabajue, R.; Haltom, T. Rapid cooling in classic heatstroke: Effect on mortality rates. Am. J. Emerg. Med. 1986, 4, 394–398. [Google Scholar] [CrossRef]
- Casa, D.; Almquist, J.; Anderson, S. Inter-association task force on exertional heat illnesses consensus statement. NATA News 2003, 6, 24–29. [Google Scholar]
- Scarneo-Miller, S.E.; Lopez, R.M.; Miller, K.C.; Adams, W.M.; Kerr, Z.Y.; Casa, D.J. High Schools Struggle to Adopt Evidence Based Practices for the Management of Exertional Heat Stroke. J. Athl. Train. 2021. [Google Scholar] [CrossRef]

| Variable | n (%) |
|---|---|
| Age (mean, SD, [range]) | 42.0 (13.0), [19–77] |
| Gender | |
| Male | 163 (75.5) |
| Female | 53 (24.5) |
| Non-binary | 0 (0.0) |
| Prefer Not to Identify | 0 (0.0) |
| Race/Ethnicity | |
| White | 176 (81.5) |
| Asian | 12 (5.6) |
| Black or African American | 1 (0.5) |
| Hispanic or Latino | 4 (1.9) |
| American Indian or Alaskan Native | 1 (0.5) |
| Native Hawaiian or Other Pacific Islander | 7 (3.2) |
| More Than One Race/Ethnicity | 10 (4.6) |
| Prefer Not to Identify | 5 (2.3) |
| Highest Level of Education Completed | |
| High School/GED | 6 (2.8) |
| Some College | 60 (27.8) |
| Associate Degree | 57 (26.4) |
| Bachelor’s Degree | 63 (29.2) |
| Master’s Degree | 25 (11.6) |
| Doctorate Degree | 5 (2.3) |
| State | n (%) | State | n (%) |
|---|---|---|---|
| Alabama | 41 (19.0) | Missouri | 1 (0.5) |
| Alaska | 3 (1.4) | Montana | 3 (1.4) |
| Arizona | 9 (4.2) | New Hampshire | 3 (1.4) |
| Arkansas | 7 (3.2) | New Jersey | 4 (1.9) |
| Colorado | 12 (5.6) | New Mexico | 1 (0.5) |
| Connecticut | 1 (0.5) | New York | 1 (0.5) |
| Florida | 1 (0.5) | Pennsylvania | 1 (0.5) |
| Hawaii | 34 (15.7) | Rhode Island | 1 (0.5) |
| Idaho | 1 (0.5) | South Carolina | 9 (4.2) |
| Illinois | 6 (2.8) | South Dakota | 10 (4.6) |
| Iowa | 1 (0.5) | Texas | 1 (0.5) |
| Kentucky | 4 (1.8) | Vermont | 1 (0.5) |
| Louisiana | 48 (22.2) | Virginia | 1 (0.5) |
| Maryland | 10 (4.6) | Wisconsin | 1 (0.5) |
| Variable | n (%) |
|---|---|
| State Certification Level (n = 216) | |
| EMR | 3 (1.4) |
| EMT | 77 (35.7) |
| AEMT | 20 (9.3) |
| Paramedic | 110 (50.9) |
| Other | 6 (2.8) |
| Years of EMS Experience (n = 214) | |
| 2 Years or Less | 18 (8.3) |
| 3–7 Years | 35 (16.4) |
| 8–15 Years | 52 (24.3) |
| 16 Years or More | 109 (50.9) |
| Type of Position (n = 214) | |
| Volunteer-Compensated | 5 (2.3) |
| Volunteer- Non-compensated | 22 (10.3) |
| Career-Part-time | 21 (9.8) |
| Career-Full-time | 166 (77.6) |
| Type of Agency (n = 214) | |
| Fire Department | 104 (48.6) |
| Private | 30 (14.0) |
| Governmental Non-fire | 49 (22.9) |
| Hospital | 11 (5.1) |
| Volunteer/Rescue Squad | 7 (3.3) |
| Other | 13 (6.1) |
| Type of Agency Service (n = 214) | |
| Primarily 9-1-1 | 153 (71.5) |
| Combination 9-1-1 and Medical Transport | 46 (21.5) |
| Primarily Medical Transport (Convalescent) | 3 (1.4) |
| Clinical Services | 3 (1.4) |
| Other | 9 (4.2) |
| Question and Response Options | n (%) | Correct Responses (n, %) | Incorrect Responses (n, %) |
|---|---|---|---|
| True or False. Exertional heat stroke is considered a life-threatening medical emergency. | |||
| True * | 181 (98.9) | 181 (98.9) | 2 (1.1) |
| False | 2 (1.1) | ||
| Please select the two primary signs and symptoms that characterize exertional heat stroke. | |||
| Hot, dry skin | 103 (27.3) | 50 (27.3) | 133 (72.7) |
| Cool, clammy skin | 11 (2.9) | ||
| Unconsciousness | 19 (5.0) | ||
| Elevated core body temperature (>40.5 °C or 105 °F) * | 102 (27.1) | ||
| Profuse sweating | 5 (1.3) | ||
| CNS dysfunction (e.g., confusion, altered mental status) * | 120 (31.8) | ||
| Vomiting | 10 (2.7) | ||
| Dehydration | 7 (1.9) | ||
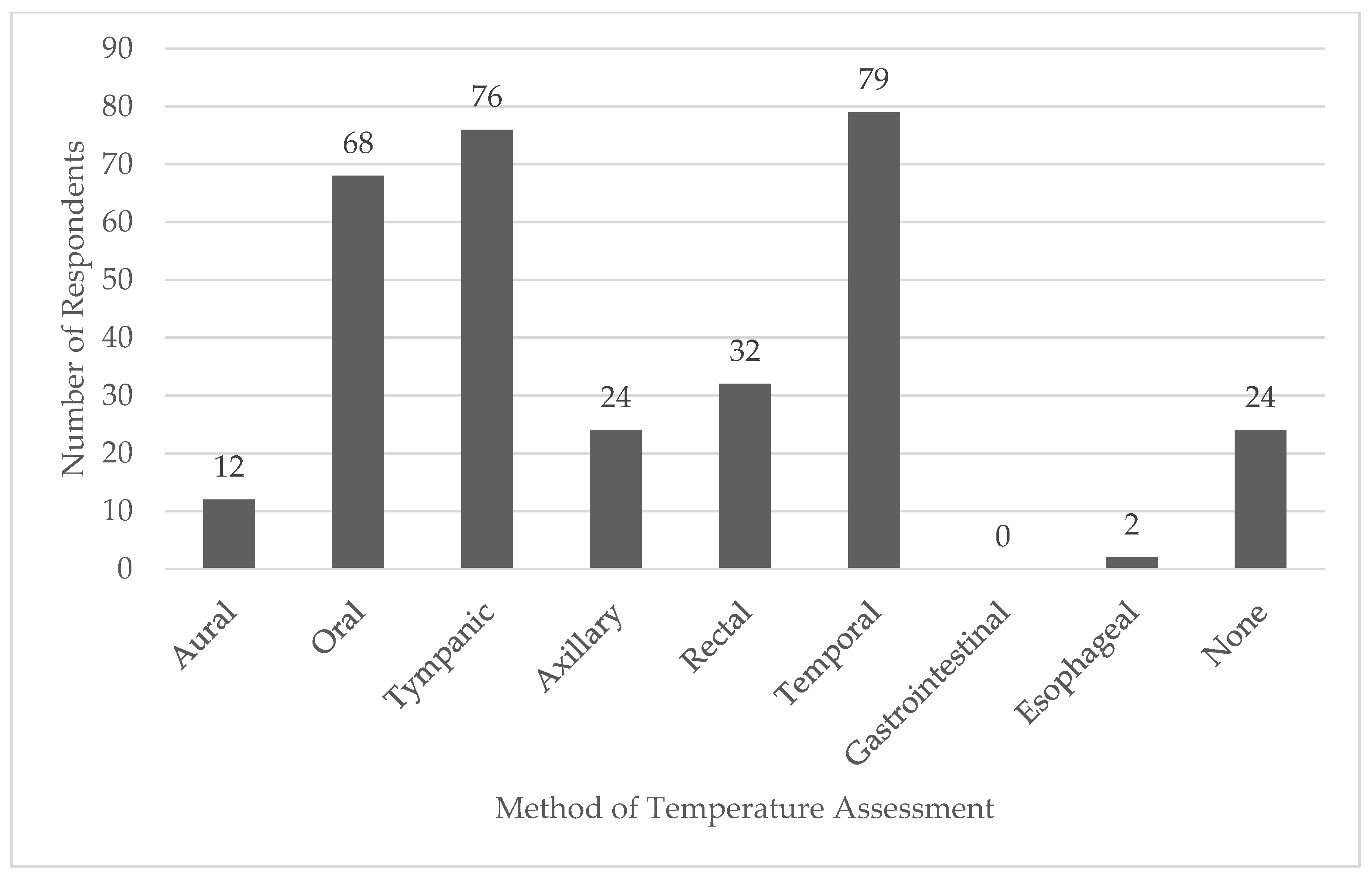
| What is the most acceptable method of temperature assessment for the diagnosis of exertional heat stroke in the prehospital setting? | |||
| Aural | 4 (2.2) | 62 (33.9) | 121 (66.1) |
| Oral | 43 (23.5) | ||
| Tympanic | 31 (16.9) | ||
| Axillary | 19 (10.4) | ||
| Rectal * | 62 (33.9) | ||
| Temporal | 22 (12.0) | ||
| Gastrointestinal | 1 (0.6) | ||
| Esophageal | 1 (0.6) | ||
| Rapid cooling of a patient with exertional heat stroke should occur within ___ minutes from the time of collapse. | |||
| 15 min | 152 (83.1) | 30 (16.4) | 153 (83.6) |
| 30 min* | 30 (16.4) | ||
| 45 min | 0 (0.0) | ||
| 60 min | 1 (0.6) | ||
| True or False. A patient with exertional heat stroke should be transported by EMS to the hospital immediately upon EMS arrival and assessment on scene, regardless of any treatments initiated and being provided on-scene. | |||
| True | 118 (64.5) | 65 (35.5) | 118 (64.5) |
| False * | 65 (35.5) | ||
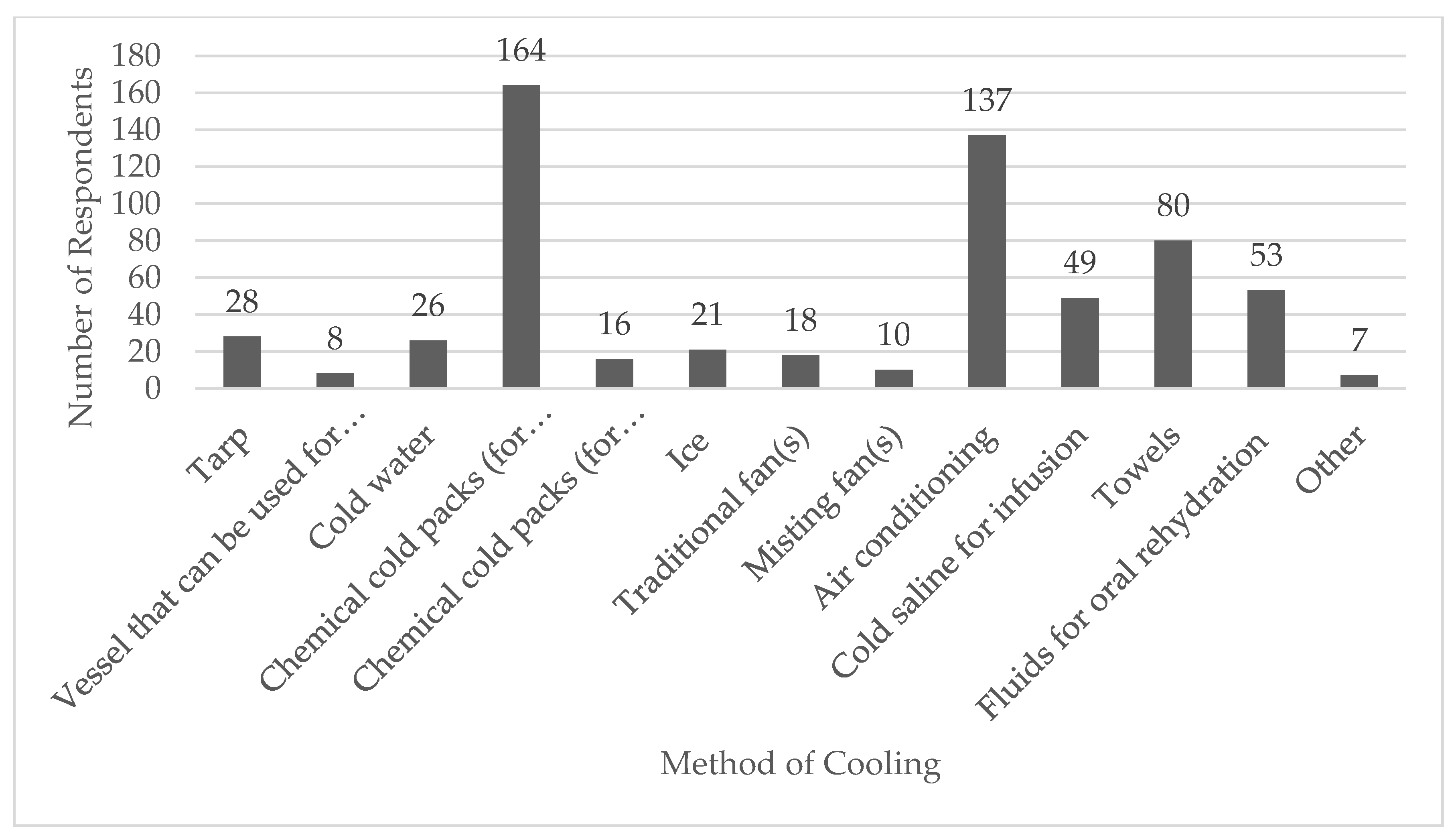
| Select all appropriate methods of cooling for the management of exertional heat stroke. | |||
| Tarp-assisted cooling * | 33 (4.1) | 0 (0.0) | 183 (100.0) |
| Cold-water immersion (from neck down) * | 62 (7.8) | ||
| Ice packs on major arteries | 153 (19.1) | ||
| Ice packs on whole body | 28 (3.5) | ||
| Ice-water immersion * | 38 (4.8) | ||
| Fanning the patient | 81 (10.1) | ||
| Move the patient to an area with air conditioning | 142 (17.8) | ||
| Cold-water dousing with ice massage | 21 (2.6) | ||
| Intravenous cold saline infusion | 73 (9.1) | ||
| Placing wet towels on the patient | 111 (13.9) | ||
| Providing the patient with oral fluids for rehydration | 58 (7.3) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hirschhorn, R.; DadeMatthews, O.; Sefton, J. Exertional Heat Stroke Knowledge and Management among Emergency Medical Service Providers. Int. J. Environ. Res. Public Health 2021, 18, 5016. https://doi.org/10.3390/ijerph18095016
Hirschhorn R, DadeMatthews O, Sefton J. Exertional Heat Stroke Knowledge and Management among Emergency Medical Service Providers. International Journal of Environmental Research and Public Health. 2021; 18(9):5016. https://doi.org/10.3390/ijerph18095016
Chicago/Turabian StyleHirschhorn, Rebecca, Oluwagbemiga DadeMatthews, and JoEllen Sefton. 2021. "Exertional Heat Stroke Knowledge and Management among Emergency Medical Service Providers" International Journal of Environmental Research and Public Health 18, no. 9: 5016. https://doi.org/10.3390/ijerph18095016
APA StyleHirschhorn, R., DadeMatthews, O., & Sefton, J. (2021). Exertional Heat Stroke Knowledge and Management among Emergency Medical Service Providers. International Journal of Environmental Research and Public Health, 18(9), 5016. https://doi.org/10.3390/ijerph18095016







