We’re Not Gonna Fall: Depressive Complaints, Personal Resilience, Team Social Climate, and Worries about Infections among Hospital Workers during a Pandemic
Abstract
1. Introduction
Hypotheses
2. Materials and Methods
2.1. Study Design
2.2. Study Variables
2.3. Statistical Analysis
3. Results
3.1. Participants
3.2. Descriptives for the Main Study Variables
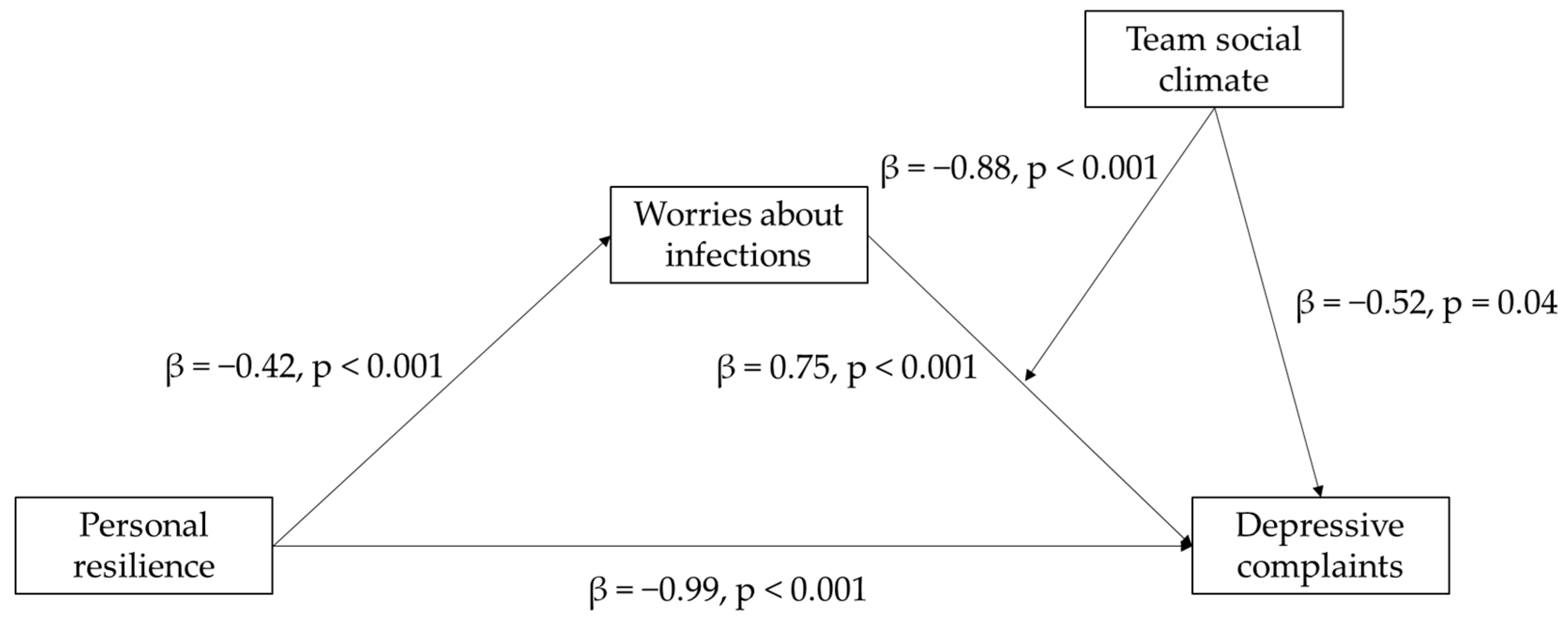
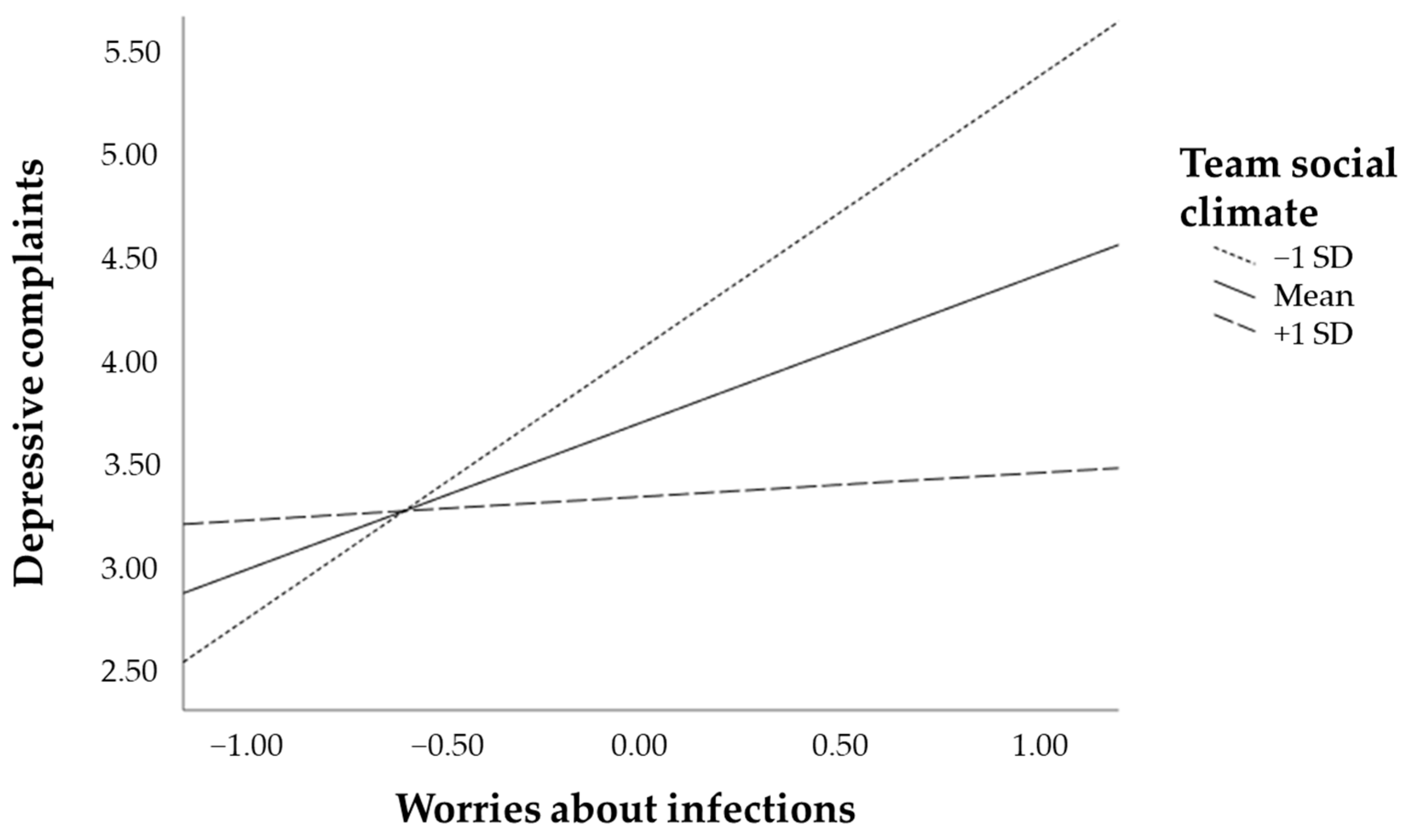
3.3. Moderated Mediation Model
4. Discussion
Potential Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Demographic/Occupational Characteristic | Category | n | % or Mean (± SD) |
|---|---|---|---|
| Gender | Female | 872 | 77.4% |
| Male | 232 | 20.6% | |
| Other | 2 | 0.2% | |
| Missing values | 20 | 1.8% | |
| Total | 1126 | 100% | |
| Age (in years) | 1112 | 45.2 (±12.2) | |
| Highest level of education | Secondary education | 96 | 8.5% |
| Vocational education | 261 | 23.2% | |
| Higher education | 653 | 58.0% | |
| PhD/MD | 100 | 8.9% | |
| Missing | 16 | 1.4% | |
| Total | 1126 | 100% | |
| Type of contract | Permanent contract | 983 | 87.3% |
| Temporary contract | 75 | 6.7% | |
| Self-employed | 7 | 0.6% | |
| Internship/student | 25 | 2.2% | |
| Other | 18 | 1.6% | |
| Missing values | 18 | 1.6% | |
| Total | 1126 | 100% | |
| Working hours a week | <20 h | 63 | 5.6% |
| 20–29 h | 357 | 31.7% | |
| 30–40 h | 623 | 55.3% | |
| >40 h | 47 | 4.2% | |
| Missing values | 36 | 3.2% | |
| Total | 1126 | 100% | |
| Occupational group | Medical specialists | 67 | 6.0% |
| Medical interns, non-specialized physicians, and residents | 32 | 2.8% | |
| Registered nurses & licensed practical nurses | 376 | 33.4% | |
| Paramedical professions | 74 | 6.6% | |
| Clinical support staff | 172 | 15.3% | |
| Research and education staff | 44 | 3.9% | |
| Management | 35 | 3.1% | |
| Administrative staff | 217 | 19.3% | |
| Facility staff | 64 | 5.7% | |
| Interns (paramedical professions and non-medical professions) | 26 | 2.3% | |
| Missing values | 19 | 1.7% | |
| Total | 1126 | 100% |
References
- Arabi, Y.M.; Murthy, S.; Webb, S. COVID-19: A novel coronavirus and a novel challenge for critical care. Intensive Care Med. 2020, 46, 833–836. [Google Scholar] [CrossRef] [PubMed]
- Emanuel, E.J.; Persad, G.; Upshur, R.; Thome, B.; Parker, M.; Glickman, A.; Zhang, C.; Boyle, C.; Smith, M.; Phillips, J.P. Fair Allocation of Scarce Medical Resources in the Time of Covid-19. N. Engl. J. Med. 2021, 382, 2049–2055. [Google Scholar] [CrossRef]
- Martin, B.I.; Brodke, D.S.; Wilson, F.A.; Chaiyakunapruk, N.; Nelson, R.E. The impact of halting elective admissions in anticipation of a demand surge due to the coronavirus pandemic (COVID-19). Med. Care 2021, 59, 213–219. [Google Scholar]
- Nembhard, I.M.; Burns, L.R.; Shortell, S.M. Responding to Covid-19: Lessons from management research. N. Engl. J. Med. 2020. Available online: https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0111 (accessed on 12 March 2021).
- Van Giessen, A.; de Wit, A.; van den Brink, C.; Degeling, K.; Deuning, C.; Eeuwijk, J.; van den Ende, C.; van Gestel, I.; Gijsen, R.; van Gils, P.; et al. Impact Van de Eerste COVID-19 Golf op de Reguliere Zorg en Gezondheid: Inventarisatie Van de Omvang Van Het Probleem en Eerste Schatting Van Gezondheidseffecten; Rijksinstituut voor Volksgezondheid en Milieu RIVM: Bilthoven, The Netherlands, 2020. [Google Scholar]
- De Brier, N.; Stroobants, S.; Vandekerckhove, P.; De Buck, E. Factors affecting mental health of health care workers during coronavirus disease outbreaks (SARS, MERS & COVID-19): A rapid systematic review. PLoS ONE 2020, 15, e0244052. [Google Scholar]
- Chen, H.; Sun, L.; Du, Z.; Zhao, L.; Wang, L. A cross-sectional study of mental health status and self-psychological adjustment in nurses who supported Wuhan for fighting against the COVID-19. J. Clin. Nurs. 2020, 29, 4161–4170. [Google Scholar] [CrossRef]
- Kerlin, M.P.; McPeake, J.; Mikkelsen, M.E. Burnout and joy in the profession of critical care medicine. Crit. Care 2020, 24, 98. [Google Scholar] [CrossRef] [PubMed]
- De Kock, J.H.; Latham, H.A.; Leslie, S.J.; Grindle, M.; Munoz, S.-A.; Ellis, L.; Polson, R.; O’Malley, C.M. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: Implications for supporting psychological well-being. BMC Public Health 2020, 21. [Google Scholar] [CrossRef]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brainbehav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- Da Silva, F.C.T.; Neto, M.L.R. Psychiatric symptomatology associated with depression, anxiety, distress, and insomnia in health professionals working in patients affected by COVID-19: A systematic review with meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 104, 110057. [Google Scholar] [CrossRef] [PubMed]
- Salazar de Pablo, G.; Vaquerizo-Serrano, J.; Catalan, A.; Arango, C.; Moreno, C.; Ferre, F.; Il Shin, J.; Sullivan, S.; Brondino, N.; Solmi, M.; et al. Impact of coronavirus syndromes on physical and mental health of health care workers: Systematic review and meta-analysis. J. Affect. Disord. 2020, 275, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Mithani, M.A. Adaptation in the Face of the New Normal. Acad. Manag. Perspect. 2020, 34, 508–530. [Google Scholar] [CrossRef]
- Rangachari, P.; Woods, J.L. Preserving Organizational Resilience, Patient Safety, and Staff Retention during COVID-19 Requires a Holistic Consideration of the Psychological Safety of Healthcare Workers. Int. J. Environ. Res. Public Health 2020, 17, 4267. [Google Scholar] [CrossRef] [PubMed]
- Singhal, S.; Reddy, P.; Dash, P.; Weber, K. From “Wartime” to “Peacetime”: Five Stages for Healthcare Institutions in the Battle against COVID-19. Available online: https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/from-wartime-to-peacetime-five-stages-for-healthcare-institutions-in-the-battle-against-covid-19 (accessed on 12 March 2021).
- Mintzberg, H. The professional bureaucracy. In Structures in Fives: Designing Effective Organizations; Prentice Hall Inc.: Englewood Cliffs, NJ, USA, 1993. [Google Scholar]
- Nicholson, S.; Propper, C. Medical Workforce. In Handbook of Health Economics; Elsevier: Amsterdam, The Netherlands, 2011; pp. 873–925. [Google Scholar]
- Younis, M.Z.; Jaber, S.; Mawson, A.R.; Hartmann, M. Estimating the unit costs of public hospitals and primary healthcare centers. Int. J. Health Plan. Manag. 2013, 28, 320–332. [Google Scholar] [CrossRef]
- EU Expert Group on Health Systems Performance Assessment (HSPA). Assessing the Resilience of Health Systems in Europe: An Overview of the Theory, Current Practice and Strategies for Improvement; Publications Office of the EU: Luxembourg, 2020. [Google Scholar]
- Al Thobaity, A.; Alshammari, F. Nurses on the Frontline against the COVID-19 Pandemic: An Integrative Review. Dubai Med. J. 2020, 3, 87–92. [Google Scholar] [CrossRef]
- Pappa, S.; Athanasiou, N.; Sakkas, N.; Sakka, S.P.; Barmparessou, Z.; Tsikrika, S.; Adraktas, A.; Pataka, A.; Migdalis, I.; Gida, S.; et al. From recession to depression? prevalence and correlates of depression, anxiety, traumatic stress and burnout in healthcare workers during the COVID-19 pandemic in Greece: A multi-center, cross-sectional study. Int. J. Environ. Res. Public Health 2021, 18, 2390. [Google Scholar] [CrossRef]
- Cai, H.; Tu, B.; Ma, J.; Chen, L.; Fu, L.; Jiang, Y.; Zhuang, Q. Psychological impacts and coping strategies of front-line medical staff during COVID-19 outbreak in Hunan, China. Med. Sci. Monit. 2020, 26, e924171-1–e924171-16. [Google Scholar] [CrossRef]
- Shanafelt, T.; Ripp, J.; Trockel, M. Understanding and Addressing Sources of Anxiety Among Health Care Professionals During the COVID-19 Pandemic. JAMA 2020, 323, 2133–2134. [Google Scholar] [CrossRef]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef]
- Zhang, W.; Wang, K.; Yin, L.; Zhao, W.; Xue, Q.; Peng, M.; Wang, H. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother. Psychosom. 2020, 89, 242–250. [Google Scholar] [CrossRef]
- Mo, Y.; Deng, L.; Zhang, L.; Lang, Q.; Liao, C.; Wang, N.; Qin, M.; Huang, H. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J. Nurs. Manag. 2020, 28, 1002–1009. [Google Scholar] [CrossRef] [PubMed]
- Urooj, U.; Ansari, A.; Siraj, A.; Khan, S.; Tariq, H. Expectations, Fears and Perceptions of doctors during Covid-19 Pandemic. Pak. J. Med. Sci. 2020, 36, S37–S42. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Wei, J.; Zhu, H.; Duan, Y.; Geng, W.; Hong, X.; Jiang, J.; Zhao, X.; Zhu, B. A Study of Basic Needs and Psychological Wellbeing of Medical Workers in the Fever Clinic of a Tertiary General Hospital in Beijing during the COVID-19 Outbreak. Psychother. Psychosom. 2020, 89, 252–254. [Google Scholar] [CrossRef] [PubMed]
- Temsah, M.-H.; Al-Sohime, F.; Alamro, N.; Al-Eyadhy, A.; Al-Hasan, K.; Jamal, A.; Somily, A.M. The psychological impact of COVID-19 pandemic on health care workers in a MERS-CoV endemic country. J. Infect. Public Health 2020, 13, 877–882. [Google Scholar] [CrossRef] [PubMed]
- Fleuren, B.P.I.; de Grip, A.; Jansen, N.W.H.; Kant, I.; Zijlstra, F.R.H. Unshrouding the sphere from the clouds: Towards a comprehensive conceptual framework for sustainable employability. Sustainability 2020, 12, 6366. [Google Scholar] [CrossRef]
- Cai, W.; Lian, B.; Song, X.; Hou, T.; Deng, G.; Li, H. A cross-sectional study on mental health among health care workers during the outbreak of Corona Virus Disease 2019. Asian J. Psychiatry 2020, 51, 102111. [Google Scholar] [CrossRef]
- Hu, T.; Zhang, D.; Wang, J. A meta-analysis of the trait resilience and mental health. Personal. Individ. Differ. 2015, 76, 18–27. [Google Scholar] [CrossRef]
- Labrague, L.J.; Santos, J.A.A. COVID-19 anxiety among front-line nurses: Predictive role of organisational support, personal resilience and social support. J. Nurs. Manag. 2020, 28, 1653–1661. [Google Scholar] [CrossRef]
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The brief resilience scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef]
- Dowrick, C.; Kokanovic, R.; Hegarty, K.; Griffiths, F.; Gunn, J. Resilience and depression: Perspectives from primary care. Health Interdiscip. J. Soc. Study Healthillness Med. 2008, 12, 439–452. [Google Scholar] [CrossRef]
- Ylipaavalniemi, J.; Kivimäki, M.; Elovainio, M.; Virtanen, M.; Keltikangas-Järvinen, L.; Vahtera, J. Psychosocial work characteristics and incidence of newly diagnosed depression: A prospective cohort study of three different models. Soc. Sci. Med. 2005, 61, 111–122. [Google Scholar] [CrossRef] [PubMed]
- Sun, N.; Wei, L.; Shi, S.; Jiao, D.; Song, R.; Ma, L.; Wang, H.; Wang, C.; Wang, Z.; You, Y.; et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am. J. Infect. Control 2020, 48, 592–598. [Google Scholar] [CrossRef]
- Hobfoll, S.E. Conservation of resources: A new attempt at conceptualizing stress. Am. Psychol. 1989, 44, 513–524. [Google Scholar] [CrossRef] [PubMed]
- Halbesleben, J.R.B.; Neveu, J.; Paustian-Underdahl, S.C.; Westman, M. Gettin to the “COR”: Understanding the role of resources in conservation of resources theory. J. Manag. 2014, 40, 1334–1364. [Google Scholar]
- Hobfoll, S.E. Conservation of resource caravans and engaged settings. J. Occup. Organ. Psychol. 2011, 84, 116–122. [Google Scholar] [CrossRef]
- Viola, M.M.; Musso, P.; Ingoglia, S.; Lo Coco, A.; Inguglia, C. Relationships between career indecision, search for work self-efficacy, and psychological well-being in Italian never-employed young adults. Eur. J. Psychol. 2017, 13, 231–250. [Google Scholar] [CrossRef]
- Kuntz, J.R.C.; Malinen, S.; Näswall, K. Employee resilience: Directions for resilience development. Consult. Psychol. J. Pract. Res. 2017, 69, 223–242. [Google Scholar] [CrossRef]
- Robertson, I.T.; Cooper, C.L.; Sarkar, M.; Curran, T. Resilience training in the workplace from 2003 to 2014: A systematic review. J. Occup. Organ. Psychol. 2015, 88, 533–562. [Google Scholar] [CrossRef]
- Rammstedt, B. Who worries and who is happy? Explaining individual differences in worries and satisfaction by personality. Personal. Individ. Differ. 2007, 43, 1626–1634. [Google Scholar] [CrossRef]
- Breznitz, S. A study of worrying. Br. J. Soc. Clin. Psychol. 1971, 10, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Beckwé, M.; Deroost, N.; Koster, E.H.W.; de Lissnyder, E.; de Raedt, R. Worrying and rumination are both associated with reduced cognitive control. Psychol. Res. 2014, 78, 651–660. [Google Scholar] [CrossRef]
- Ho, S.M.; Kwong-Lo, R.S.; Mak, C.W.; Wong, J.S. Fear of severe acute respiratory syndrome (SARS) among health care workers. J. Consult. Clin. Psychol. 2005, 73, 344–349. [Google Scholar] [CrossRef]
- Shacham, M.; Hamama-Raz, Y.; Kolerman, R.; Mijiritsky, O.; Ben-Ezra, M.; Mijiritsky, E. COVID-19 factors and psychological factors associated with elevated psychological distress among dentists and dental hygienists in Israel. Int. J. Environ. Res. Public Health 2020, 17, 2900. [Google Scholar] [CrossRef] [PubMed]
- Major, B.; Richards, C.; Cooper, M.L.; Cozzarelli, C.; Zubek, J. Personal resilience, cognitive appraisals, and coping: An integrative model of adjustment to abortion. J. Personal. Soc. Psychol. 1998, 74, 735–752. [Google Scholar] [CrossRef]
- Schock, M.L.; Kleber, R.J.; Lensvelt-Mulders, G.J.L.M. A model of resilience and meaning after military deployment: Personal resources in making sense of war and peacekeeping experiences. Aging Ment. Health 2010, 14, 328–338. [Google Scholar] [CrossRef] [PubMed]
- Troy, A.S.; Mauss, I.B. Resilience in the face of stress: Emotion regulation as a protective factor. In Resilience and Mental Health; Southwick, S.M., Litz, B., Charney, D., Friedman, M.J., Eds.; Cambridge University Press: Cambridge, UK, 2011. [Google Scholar]
- Schneider, B.S.; Ehrhart, M.G.; Macey, W.H. Organizational climate and culture. Annu. Rev. Psychol. 2013, 64, 361–388. [Google Scholar] [CrossRef] [PubMed]
- Loo, R. Assessing “team climate” in project teams. Int. J. Proj. Manag. 2003, 21, 511–517. [Google Scholar] [CrossRef]
- Williams, K.J.; Nida, S.A. Ostracism, Exclusion, and Rejection; Routledge: New York, NY, USA, 2016. [Google Scholar]
- Baumeister, R.F.; Leary, M.R. The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Psychol. Bull. 1995, 117, 497–529. [Google Scholar] [CrossRef] [PubMed]
- Grant, F.; Hogg, M.A. Self-uncertainty, social identity prominence and group identification. J. Exp. Soc. Psychol. 2012, 48, 538–542. [Google Scholar] [CrossRef]
- Hogg, M.A.; Terry, D.J. Social identity and self-categorization processes in organizational contexts. Acad. Manag. Rev. 2000, 25, 121–140. [Google Scholar] [CrossRef]
- Cohen, S.; Wills, T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985, 98, 310–357. [Google Scholar] [CrossRef]
- Jennings, B.M. Stress, locus of control, social support, and psychological symptoms among head nurses. Res. Nurs. Health 1990, 13, 393–401. [Google Scholar] [CrossRef]
- Hines, S.E.; Chin, K.H.; Glick, D.R.; Wickwire, E.M. Trends in moral injury, distress and resilience factors among healthcare workers at the beginning of the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 488. [Google Scholar] [CrossRef]
- van den Broeck, A.; vander Elst, T.; Baillien, E.; Sercu, M.; Schouteden, M.; de Witte, H.; Godderis, L. Job demands, job resources, burnout, work engagement, and their relationships. J. Occup. Environ. Med. 2017, 59, 369–376. [Google Scholar] [CrossRef]
- Day, A.; Crown, S.N.; Ivany, M. Organisational change and employee burnout: The moderating effects of support and job control. Saf. Sci. 2017, 100, 4–12. [Google Scholar] [CrossRef]
- Szkody, E.; Stearns, M.; Stanhope, L.; McKinney, C. Stress-buffering role of social support during COVID-19. Fam. Process 2021. [Google Scholar] [CrossRef]
- Fiedler, K.; Harris, C.; Schott, M. Unwarranted inferences from statistical mediation tests—An analysis of articles published in 2015. J. Exp. Soc. Psychol. 2018, 75, 95–102. [Google Scholar] [CrossRef]
- RIVM. Epidemiologische Situatie van SARS-CoV-2 in Nederland; Rijksinstituut voor Volksgezondheid en Milieu–RIVM: Bilthoven, The Netherlands, 2020. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Volker, D.; Zijlstra-Vlasveld, M.C.; Brouwers, E.P.M.; Homans, W.A.; Emon, W.H.M.; van der Feltz-Cornelis, C.M. Validation of the Patient Health Questionnaire-9 for Major Depressive Disorder in the Occupational Health Setting. J. Occup. Rehabil. 2016, 26, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Van Vliet, M. Aanbevelingen Voor Het Meten Van Positieve Gezondheid; Stichting Institute for Positive Health: Utrecht, The Netherlands, 2019. [Google Scholar]
- Alvarado, R.; Susser, E.; Mascayano, F. The Impact of the Covid-19 Pandemic on the Mental Health of Workers in Health Services: The Covid-19 HEalth caRe wOrkErS (HEROES) Study. 2020. [Google Scholar]
- Hoegl, M.; Gemuenden, H.G. Teamwork quality and the success of innovative projects: A theoretical concept and empirical evidence. Organ. Sci. 2001, 12, 435–449. [Google Scholar] [CrossRef]
- Simons, T.L.; Peterson, R.S. Task conflict and relationship conflict in top management teams: The pivotal role of intragroup trust. J. Appl. Psychol. 2000, 85, 102–111. [Google Scholar] [CrossRef] [PubMed]
- Jehn, K.A. A multimethod examination of the benefits and detriments of intragroup conflict. Adm. Sci. Q. 1995, 40, 256–282. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; The Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Kaplan, J.B.; Bergman, A.L.; Christopher, M.; Bowen, S.; Hunsinger, M. Role of resilience in mindfulness training for first responders. Mindfulness 2017, 8, 1373–1380. [Google Scholar] [CrossRef]
- Kunzler, A.M.; Helmreich, I.; Chmitorz, A.; König, J.; Binder, H.; Wessa, M.; Lieb, K. Psychological interventions to foster resilience in healthcare professionals. Cochrane Database Syst. Rev. 2020. [Google Scholar] [CrossRef]
- Skalski, S.; Uram, P.; Dobrakowski, P.; Kwiatkowska, A. The link between ego-resiliency, social support, SARS-CoV-2 anxiety, and trauma effects: Polish adaptation of the Coronavirus Anxiety Scale. Personal. Individ. Differ. 2020, 171, 110540. [Google Scholar] [CrossRef] [PubMed]
- Chan, D. So why ask me? Are self-report data really that bad? In Statistical and Methodological Myths and Urban Legends; Lance, C.E., Vandenberg, R.J., Eds.; Routledge: New York, NY, USA, 2010; pp. 329–356. [Google Scholar]
- Conway, J.M.; Lance, C.E. What reviewers should expect from authors regardign common method bias in organizational research. J. Bus. Psychol. 2010, 25, 325–334. [Google Scholar] [CrossRef]
- Podsakoff, P.M.; MacKenzie, S.B.; Lee, J.Y.; Podsakoff, N.P. Common method biases in behavioral research: A critical review of the literature and recommended remedies. J. Appl. Psychol. 2003, 88, 879–903. [Google Scholar] [CrossRef]
- Gruijters, S.L.K. Baseline comparisons and covariate fishing: Bad statistical habits we should have broken yesterday. Eur. Health Psychol. 2016, 18, 205–209. [Google Scholar]
- Li, C.Y.; Sung, F.C. A review of the healthy worker effect in occupational epidemiology. Occup. Med. 1999, 49, 225–229. [Google Scholar] [CrossRef]
| 1 | 2 | 3 | 4 | Mean | n | SD | Range | |
|---|---|---|---|---|---|---|---|---|
| 1. Personal resilience | 0.72 | - | - | - | 3.67 | 1068 | 0.70 | 1–5 |
| 2. Worrying about infections | −0.29 a | 0.84 | - | - | 2.99 | 1034 | 0.86 | 1–5 |
| 3. Team social climate | 0.18 a | −0.08 b | 0.87 | - | 3.73 | 1025 | 0.74 | 1–5 |
| 4. Depressive complaints | −0.29 a | 0.26 a | −0.18 a | 0.85 | 3.83 | 584 | 3.84 | 0–27 |
| β | SE(HC4) | t-Value | p-Value | 95% CI | |
| Step 1: Effect of personal resilience on worries about infections | |||||
| Personal resilience | −0.42 b | 0.04 | −9.34 | <0.001 | −0.50–−0.33 |
| Model R2 = 0.12 b, p < 0.001, df(1) = 1, df(2) = 570 | |||||
| β | SE(HC4) | t-Value | p-Value | 95% CI | |
| Step 2: Concurrently estimated effects of predictor variables on depressive complaints | |||||
| Personal resilience | −0.99 b | 0.23 | −4.23 | <0.001 | −1.45–−0.53 |
| Worries about infections | 0.75 b | 0.22 | 3.35 | <0.001 | 0.31–1.19 |
| Team social climate | −0.52 a | 0.26 | −2.03 | 0.04 | −1.02–−0.02 |
| Interaction Worries * Climate | −0.88 a | 0.40 | −2.18 | 0.03 | −1.68–−0.09 |
| Model R2 = 0.14 b, p < 0.001, df(1) = 4, df(2) = 567; R2-change= 0.02 a, p = 0.03, df(1) = 1, df(2) = 567 | |||||
| Index | SE(Boot) | 95% CI (Boot) | |||
| Step 3: Test of the full moderated mediation effect | |||||
| Index of moderated mediation | 0.37 c | 0.16 | 0.07–0.73 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fleuren, B.P.I.; Poesen, L.T.; Gifford, R.E.; Zijlstra, F.R.H.; Ruwaard, D.; van de Baan, F.C.; Westra, D.D. We’re Not Gonna Fall: Depressive Complaints, Personal Resilience, Team Social Climate, and Worries about Infections among Hospital Workers during a Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 4701. https://doi.org/10.3390/ijerph18094701
Fleuren BPI, Poesen LT, Gifford RE, Zijlstra FRH, Ruwaard D, van de Baan FC, Westra DD. We’re Not Gonna Fall: Depressive Complaints, Personal Resilience, Team Social Climate, and Worries about Infections among Hospital Workers during a Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(9):4701. https://doi.org/10.3390/ijerph18094701
Chicago/Turabian StyleFleuren, Bram P. I., Lieze T. Poesen, Rachel E. Gifford, Fred R. H. Zijlstra, Dirk Ruwaard, Frank C. van de Baan, and Daan D. Westra. 2021. "We’re Not Gonna Fall: Depressive Complaints, Personal Resilience, Team Social Climate, and Worries about Infections among Hospital Workers during a Pandemic" International Journal of Environmental Research and Public Health 18, no. 9: 4701. https://doi.org/10.3390/ijerph18094701
APA StyleFleuren, B. P. I., Poesen, L. T., Gifford, R. E., Zijlstra, F. R. H., Ruwaard, D., van de Baan, F. C., & Westra, D. D. (2021). We’re Not Gonna Fall: Depressive Complaints, Personal Resilience, Team Social Climate, and Worries about Infections among Hospital Workers during a Pandemic. International Journal of Environmental Research and Public Health, 18(9), 4701. https://doi.org/10.3390/ijerph18094701






