Abstract
Climate change is a global problem, which affects the various geographical regions at different levels. It is also associated with a wide range of human health problems, which pose a burden to health systems, especially in regions such as Africa. Indeed, across the African continent public health systems are under severe pressure, partly due to their fragile socioeconomic conditions. This paper reports on a cross-sectional study in six African countries (Ghana, Nigeria, South Africa, Namibia, Ethiopia, and Kenya) aimed at assessing their vulnerabilities to climate change, focusing on its impacts on human health. The study evaluated the levels of information, knowledge, and perceptions of public health professionals. It also examined the health systems’ preparedness to cope with these health hazards, the available resources, and those needed to build resilience to the country’s vulnerable population, as perceived by health professionals. The results revealed that 63.1% of the total respondents reported that climate change had been extensively experienced in the past years, while 32% claimed that the sampled countries had experienced them to some extent. Nigerian respondents recorded the highest levels (67.7%), followed by Kenya with 66.6%. South Africa had the lowest level of impact as perceived by the respondents (50.0%) when compared with the other sampled countries. All respondents from Ghana and Namibia reported that health problems caused by climate change are common in the two countries. As perceived by the health professionals, the inadequate resources reiterate the need for infrastructural resources, medical equipment, emergency response resources, and technical support. The study’s recommendations include the need to improve current policies at all levels (i.e., national, regional, and local) on climate change and public health and to strengthen health professionals’ skills. Improving the basic knowledge of health institutions to better respond to a changing climate is also recommended. The study provides valuable insights which may be helpful to other nations in Sub-Saharan Africa.
1. Introduction
There is clear evidence that climate change is affecting countries around the world and that it poses a threat to the achievement of the UN Sustainable Development Goals (SDGs) [1]. Current systems in place aimed at implementing the SDGs (especially SDGs 6, 7, 13, 14, and 15) have prioritised tackling issues that address climate change and environmental sustainability [1]. The fourth and fifth assessment reports issued by the Intergovernmental Panel on Climate Change (IPCC) emphasised the need for stakeholders (i.e., governments, policymakers, and academics) to take urgent actions on climate change to ensure sustainable development. Recent studies have shared a similar agreement [2,3]. The United Nations Framework Convention on Climate Change through the Paris Agreement [4] has emphasised the need to reduce CO2 emissions as one of the measures to tackle the problem.
From a regional perspective, some of the fundamental drivers of climate in Africa are the Inter-Tropical Convergence Zone (ITCZ), the El Niño—Southern Oscillation (ENSO) and the West African Monsoon (W.A.M.) [5,6]. Climate distortions in the W.A.M. lead to changed wind and precipitation conditions in Africa’s tropical and sub-tropical regions. This provides favourable conditions for the transmission of vector-borne diseases [7]. The World Health Organization [8] identified Africa as the region most affected by malaria. Although significant measures to reduce the incidence of malaria in Africa are in place, the Institute of Health Metrics and Evaluation (IHME) and WHO estimated that nine in every ten deaths from malaria are from the African region [9].
Another index of environmental distortions is the warming of the earth’s climate, which creates offshoots of ITCZ and ENSO movements. The evidence of these movements appears principally in Southern Africa and the Sahelian part of Western Africa, where there are increases in sea and air warming, which result in heavy rainfall and floods [10,11]. These, in turn, are associated with losses of agricultural produce, which can cause famine, increases in the mortality rate, and increased exposure to infectious diseases, often with an increased exposure to toxic substances [12,13].
The United Nations (UN) reported in 2017 the impact of severe flooding in the West and Central Africa axes [1]. The incident resulted in acute human and physical losses, reflected in river overflows, displacement of people, and an increase in disease burdens and deaths in Sierra Leone, Guinea, Mali, Ghana, Nigeria, Burkina Faso, the Central African Republic, and Niger. In Niger, the official estimate of flood victims was 206,513, with 56 deaths, 1200 houses damaged, 16,000 herds of cattle lost, and 9800 hectares of cultivated land lost. The case of Nigeria was not so different, with more than 100,000 people affected by about 21 local government areas. Similarly, almost all the Burkina Faso regions were affected, with 30,862 people impacted by flooding and violent winds [1].
In the Eastern part of Africa, where dry weather is prevalent, there have also been drought experiences due to the ITCZ-ENSO movements [6]. ENSO’s progress reflects the processes that occur in the Pacific [5]. However, its impacts—which are in the form of increases in surface air temperature, and sea and land warming—gives rise to drought and water unavailability, which have spill over effects in Africa and particularly in Eastern Africa. Historically, the El Niño between 1997and 1998 resulted in droughts and forest fires in some Asian economies and in East Africa, where many health challenges were also recorded [6]. According to a study [13], the drought areal-extent decadal spans from 0.6% in Tanzania to 3.7% in Ethiopia. In contrast, the probabilities of experiencing drought can be as high as 40%, and most of the dryness in East Africa for 11 decades (1903–2013) spans between 14 and 24 months over two years.
Indeed, Africa is one of the most vulnerable regions to climate variability and change [14]. The literature identified some of the effects of the climate alterations in Africa, such as sea-level rise, glacier melting, water resources reduction, reduction in agricultural production and food security, lesser biodiversity increases in zoonotic diseases, and increase in erosion drought, and flood [6,15,16]. An increase in sea and land temperatures is an expression of the growth of warming, despite identifying water bodies, such as seas and oceans, as absorbers for climate distortions or ensuring eco-balance [17].
An increase in greenhouse gas discharges reflects increases in human socioeconomic activities [18]. These socioeconomic activities mainly depend on utilising environmental resources, which distort certain climatic conditions, such as the earth’s energy balance, which creates severe health implications. This distortion has resulted in two global goals: reducing greenhouse emissions and improving air quality. Evidence has shown that the air quality in many urban areas in Africa is the leading cause of respiratory disorders, such as lung cancer, asthma, dementia, chronic obstructive pulmonary disease, and cardiovascular diseases [7].
An increase in vector-borne diseases, such as malaria, lymphatic filariasis, onchocerciasis, schistosomiasis, African trypanosomiasis, and Rift Valley fever, is linked to climate change impacts. These diseases are, therefore, higher in developing economies than in developed economies [19]. Apart from the low-income challenge, poor health, and environmental conditions in Africa, vector-borne diseases directly bear on tropical climate areas, typical of the sub-Saharan African climate [19].
Climate change worsens the already precarious situation seen in low-income countries’ public health systems [20]. Africans are undoubtedly witnessing these pressures and even surprises from climate disorder dimensions, especially human health and sustainability [12]. Public health planners, policymakers, and other relevant stakeholders must understand how climate change will affect public health in their area to enable them to address such issues.
Globally, the impacts of climate change on public health are inconsistent. This inconsistency is because of geographical variations and the varying capacities of countries to adapt to these changes. Sensitisation on the part of the representatives of public health systems on the health impacts of climate change is needed [20]. Therefore, to effectively address these impacts, the various health systems need to understand and consider the relationship between climate change and human health, sharing this knowledge with the relevant stakeholders. The experience and sharing of knowledge regarding how climate change will affect human health will increase the preparedness of policymakers to respond to increases in the prevalence of some diseases. Therefore, this study highlights aspects of climate change experienced, using the sampled African countries, and their impact on human health. The study also assesses the extent of vulnerability to climate change impacts on human health and the health systems’ perception of them. Furthermore, this study determines the health systems’ preparedness in the sampled African countries to cope with climate change’s health impacts on human health.
Other areas of interest within the study include assessing the governments’ financial (budget) responses seen in the sampled African countries to deal with the observed human health impacts of climate change, the effectiveness of the available resources, and those needed to cope with the effects of climate change on human health. This study also aims to contribute to better policies to improve present and future generations’ livelihoods, despite the variabilities in Africa’s climate conditions. The overall aim of the study was to assess the preparedness of health systems, based on the responses by the surveyed respondents, who work in these countries and know the extent to which they are prepared to cope with the pressures posed by climate change. The use of the opinion of the respondents cannot be regarded as the sole criteria for the assessment of preparedness; however, it is an important one to the extent that such witness statements are unbiased and reflect the reality, being more reliable than government statements, which sometimes do reveal real trends.
Health Impacts of Climate Change in Africa
Conforming to the Intergovernmental Panel on Climate Change (IPCC) report, climate change impacts on Africans’ health have been quite enormous, especially for vulnerable groups, such as the poor, women, and children [19,21,22]. The challenge of water, food and vector-borne diseases, malnutrition, and mental health consequences can be attributed mainly to extreme weather events, temperature and rainfall patterns, thereby posing a health threat to the African continent [23].
Several studies have documented the impacts of climate change on health [19,21,24,25]. Direct effects include the following: extreme events-related injuries and mishaps; infectious diseases associated with water, vector biology and food contamination; manifestations of allergies coupled with increased allergen productions; air pollution causing respiratory and cardiovascular diseases; and malnutrition related to food insecurity [24,26]. Mental health consequences, population migration, and civil conflicts are among other indirect health effects for which data to assess their magnitude of occurrence are limited [24]. The U.C.L. Lancet Commission reports that climate change impacts account for 34% of the global disability-adjusted life years (DALYs) in Sub-Saharan Africa. The burden of the health risk associated with climate impacts is reported as three times as great in the worldwide population since Sub-Saharan Africa only accounts for 11% of its population [27].
Climate change will increase people’s exposure to water-related contaminants and cause illness by affecting fresh and marine water resources. Bacteria, viruses, protozoa, and other blue-green algae are pathogens and toxins that cause water-related diseases [28].
A review of cholera seasonality suggests a long association with climate change and poor sanitation. The outbreak of cholera is associated with heavy rainfall and floods, particularly in Ghana [29]; Nigeria [30]; and El Nino-Southern Oscillation in Southern [23] and Eastern [31] African countries. In Ghana, Namibia, South Africa and Ethiopia, precipitation and temperature increase the number of diarrhoeal cases, resulting in many deaths [32,33,34,35].
Other climate-sensitive water-borne diseases reported in many parts of the continent with severe health outcomes are the Buruli ulcer and schistosomiasis, occurring in Ghana [36] and Nigeria [37].
Malaria, leishmaniasis, Rift Valley fever, and tick and rodent-borne diseases are the most frequently occurring vector-borne diseases, causing myriads of premature morbidity and mortality rates in Africa [23]. As one significant disease associated with climate change [27], malaria varies regionally with temperature, with its highest occurrence at 25 °C and falls above 28 °C [23]. Studies investigated correlations of rainfall pattern, temperature variability, humidity, land and sea surface temperature and total precipitation with malaria in Africa [38,39,40,41]. The findings showed that temperature and precipitation patterns play a role in neglected tropical diseases, such as leishmaniasis and schistosomiasis. Leishmaniasis occurs mainly in Northern African countries with recent emergence in western regions due to co-infection. Meanwhile, changes in rainfall pattern are causing Rift Valley fever in the Horn of Africa. In addition, there is a rise in tick distribution and tick-borne diseases in Eastern and Southern Africa due to land use and cover change; prolonged Harmattan periods across Africa engender favourable meningitis conditions [23,30,42].
Further studies explored the health impacts of climate change on nutrition and food security across Africa. Stunted growth and underweight conditions among children in Mali, Kenya, Ethiopia, and Ghana (grey literature) due to malnutrition and food insecurity have a significant association with the severity of drought, floods, and extreme temperature [23,43,44,45,46]. Despite the availability of food sources and nutritional value in parts of Africa, low transportation networks due to floods hamper food distribution [47].
A study concluded that temperature and moisture influence fungal growth and aflatoxin production in cereals and legumes. Their presence inhibits infants’ growth due to the consumption of contaminated food ingredients [48]. The delayed and sharp decrease in rainfall gives way to drought and decreased crop yields, culminating in malnutrition in the savanna zones in countries like Ghana. The population livelihood depends on rain-fed agriculture [49].
The severity of atmospheric warming causes low crop production, which has, in turn, increased food insecurity and shifted the population’s attention to imported food, which affects the livelihood of the vulnerable in Nigeria, South Africa, and Ghana [50,51,52,53], as well as causing malnutrition among children in Ethiopia [54]. A study in Ethiopia concluded that about 2.7 million people required emergency food assistance in 2014, while 238,761 children had treatment for severe and acute malnutrition [54].
Some other studies extensively reviewed the health impacts of extreme weather events on the African continent. The effect of floods from severe precipitation caused numerous fatalities and victims’ enforcement to leave their homes in the Eastern African countries, Central and Western Africa [20,25,55,56,57,58]. Some impacts of mental health consequences from severe climate events are anxiety, depression, social dysfunction, and loss of confidence as part of the health effects that beset the surviving populace [59,60,61,62,63]. Heatwaves and heat-related health effects from extreme temperatures recently gained attention in Africa through increasing related death tolls. Heat rashes and multiple stressors in West African countries, involving Ghana, Nigeria, Burkina Faso, and Kenya in the East, and Zimbabwe and South Africa in the South [21,64,65,66,67,68], with children being the most affected [23]. Maintaining work levels and output due to extreme temperature decreases the agricultural workload in African countries. For instance, in a study conducted in South Africa, the reduced work capacities and outputs were attributed to heat waves, which caused severe sunburns, sleeplessness, irritability, and exhaustion in workers [69]. Risk assessments were conducted for extreme health impacts across African countries, especially Kenya, both at the regional and city scale. The findings showed that 10,000 to 86,000 people would be affected by severe floods by 2030, which will cost the country between ZAR 7 and ZAR 58 million [70].
From Figure 1 while some impacts are directly influenceable (e.g., malnutrition from droughts), others are indirect (e.g., mental health problems due to dislocation or losses in crops or livestock).
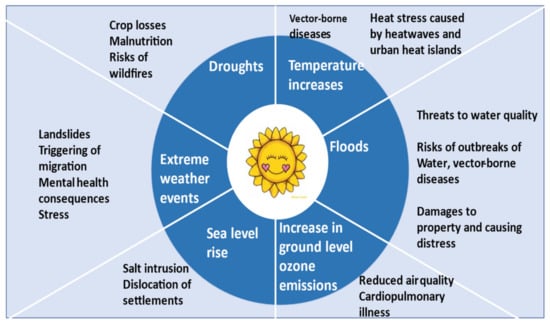
Figure 1.
Relations between climate change and some of its health impacts. Source: authors.
2. Methodology
A cross-sectional study was conducted in six (6) different African countries to understand the country’s vulnerability to climate change impacts on human health and assess their health systems’ preparedness towards these impacts. The selected countries were (1) Ghana and (2) Nigeria, in West Africa; (3) Namibia and (4) South Africa, in Southern Africa; and (5) Kenya and (6) Ethiopia in East Africa (see Figure 2). The population of each sampled country according to Worldometer in 2020 is 31,072,940 in Ghana; 206,139,589 in Nigeria; 59,308,690 in South Africa; 2,540,905 in Namibia; 114,963,588 in Ethiopia; and 53,771,296 in Kenya, respectively [71]. These 6 countries represent the various African regions because of their high vulnerability to climate impacts.
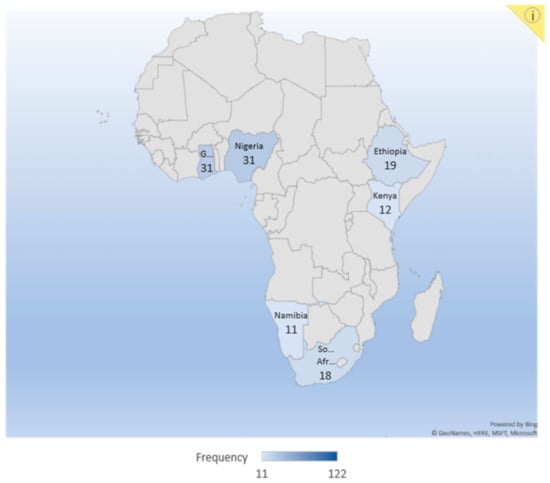
Figure 2.
Africa map highlighting the countries studied.
2.1. Data and Sample
2.1.1. Secondary Data
The authors searched for and tabulated some of the existing peer-reviewed literature (Table 1) from each sampled country between 2014 and 2019 through PubMed and Google Scholar. The search for evidence focused on five significant climate change impacts on human health from each sampled country: (1) impact on water-borne, water, and sanitation diseases; (2) impact on vector-borne diseases; (3) extreme weather events impact; (4) impacts on nutrition, food security and distribution; and (5) impacts on mental health and wellbeing. This was done to determine each country’s vulnerability to the impacts, their exposure to climate drivers, the study location within the country and the potential resulting outcomes from the exposure to enable authors to measure sampled country’s public health system’s preparedness towards these challenges through our survey.

Table 1.
A systematic review of the sampled countries’ literature to determine their vulnerabilities to the five significant climate change impacts: their exposure to climate drivers, the study location, and the potential resulting outcome from the exposure (see Appendix A). This was developed as a measure of the sampled country’s intensity to climate impacts on human health and the health systems’ preparedness against the impacts through the survey.
2.1.2. Primary Data Collection
The authors employed a questionnaire-based survey to complement the literature on the vulnerability of the sampled countries to climate change impacts. The survey again aims to assess these countries’ health systems’ readiness to cope with climate change impacts. Primary data were collected between April and the first week of June 2019 through an online survey using a structured questionnaire with several closed-ended and very few open-ended questions (see Appendix A). In the sampling stage, the authors purposely selected professionals in the field of health from government agencies, higher institutions, non-governmental agencies, and research institutions in each sampled country and reached out to them via e-mail contacts (see Table 2). The expected sample size from each participant country was about 30. Typically, it was widely disseminated in such surveys but attracted the interest of participants who had a substantial interest in the topic.

Table 2.
The number of respondents from the sampled countries.
One advantage of the sampled professionals is that they have expertise in climate change impacts on human health and improve resilience through adaptive measures. The authors divided the questionnaire into five (6) main parts. The first part addressed the background information of the respondents with their corresponding country. The second part examined the respondents’ knowledge and perception of climate variability and human health impacts in each sampled country; part three of the research question assesses each country’s vulnerability to climate change effects. Section four assesses the health professionals’ perception of the health systems’ preparedness in dealing with the health impacts of climate change in each country. The fifth section assesses the available interventions in dealing with the issues of climate change effects. The sixth section evaluates each sampled country’s available resources to deal with climate change impacts on human health and the health professionals’ resources to curb the effects. The authors analysed the survey data using IBM SPSS statistics 25, and the findings are presented in the subsequent parts of this paper.
3. Results
All the research questions relating to the study are presented in this section. Their discussion is followed in the next section. Tables are predominantly used in the results to give precise percentages. The necessary details of the respondents (e.g., workplace with their position) are described. Information on climate change in the sampled countries, with its impacts on human health, as observed by respondents, is also presented. Other analyses tabulated include respondents’ perceptions of health professionals’ preparedness to cope with climate change’s health hazards. Finally, the health resources available and those needed to curb the challenges of climate change impacts on public health are also described.
3.1. Respondents Background Information
A purposive sampling technique that targeted only professionals in the health systems at various sectors (see Table 3) with prior knowledge on climate change and its impacts on human health were selected. In the selection process, these professionals were professors, coordinators, consultants, public health administrators, directors, project safety supervisors, lecturers, students, the health ministries from sampled countries, climate change institutions, nurses, senior researchers, etc. All respondents from the sampled countries obtained their weather/climate information from meteorological agencies, radio/television stations, internet sources, as well as from different data providers (G.C.M. model outputs).

Table 3.
Respondents’ workplaces.
3.2. Respondents Knowledge and Perception of Climate Change and Health Impacts
It can be seen in Table 4 that all respondents knew the potential health impacts of climate change of which examples were given as follows:

Table 4.
Respondents’ understanding of climate change and human health impacts.
- Infectious diseases related to changes in vector biology, water, and food contamination.
- Injuries and fatalities related to extreme weather events and heatwaves.
- Allergic symptoms related to increased allergen production.
- Mental health consequences, civil conflicts, and population dislocation.
Our survey results showed that climate change had extensively been experienced in the past years, as reported by 63.1% of respondents. In comparison, 32.0% claimed that the sampled countries had experienced them to some extent. Nigeria was perceived to have the highest climate experience (67.7% within the country), and Kenya (66.6% within the country). South Africa had the lowest climate change experience as perceived by the respondents (50.0% within the country) compared to other sampled countries.
Respondents from West Africa (Ghana, Nigeria) reported that floods and extreme temperatures are frequent, and those from Eastern Africa (Ethiopia, Kenya) mentioned drought and extreme temperatures. Extreme temperatures appear to be common in the Western and Eastern part of Africa.
The Southern African countries (South African and Namibia) experienced much drought and extreme temperatures. To some extent, floods and erratic rainfall pattern were observed in all the sampled countries.
These responses confirm a reviewed article, Strengthening climate change adaptation capacity in Africa- case studies from six major African cities and policy implications [77], which indicated that cities in African countries have been vulnerable to climate change impacts.
3.3. Public Health’ Vulnerability to Climate Change Impacts as Perceived by Respondents in Sampled Countries
About half (50.8%) of the respondents revealed that the health impacts of climate change had been extensively observed in the sampled African countries, while 38.5% of the respondents reported that the effects were experienced only to some extent. All respondents from Ghana and Namibia (100%) revealed that the health problems caused by climate change are common in the two countries. In contrast, only 27.8% of South African respondents showed that climate change was observed. Malaria and other vector-borne diseases were reported in both Ghana (67.7%) and Nigeria (64.5%) as most prevalent. Nigeria and Ethiopia reported considerable percentages of food-borne illnesses, malnutrition, and food insecurity (48.4% and 57.9%).
The respondents’ perceptions regarding the trend of the diseases from the past until now were examined, as shown in Table 5. The table reveals that diseases caused by climate change have extensively been increased, with Nigeria having the highest percentage (80.8%) in the magnitude and severity of the disease. Though South Africa had the lowest percentage increase (66.7%), it is significant to conclude that sampled African countries face a significant challenge to infections caused by climate change impacts.

Table 5.
Sampled countries’ diseases trend from the past until now as perceived by respondents.
In total, 76.4% of total respondents predicted that the magnitude and severity of climate-induced diseases in sampled countries would increase in the following years if climate change were not accounted for in the planning and implementation of public health programs.
3.4. The Health Systems’ Preparedness in Dealing with the Health Impacts of Climate Change as Perceived by Respondents
The implications regarding the sampled country’s preparedness to effectively respond to climate change’s health impacts are presented in Table 6 to assess the necessary intervention to improve coping and adaptation strategies. The table indicates a severe deficit in all aspects of preparedness in the sampled countries to effectively respond to climate change impacts. Percentage differences in the impacts’ preparedness priority between the sampled countries, the insufficient healthcare professionals without enough training regarding climate change, and the lack of delivery systems to address health problems caused by climate change impacts are significant evidence of the ill-prepared situations of the sampled countries to improve on the coping and adaptation strategies effectively.

Table 6.
Respondents’ perceptions of the health system’s preparedness in dealing with the health impacts of climate (CI) change in sampled countries. Numbers are assigned to their respective survey questions on top of the table. Even though percentages summed up to 100, this table’s options are of greater importance to this study (see Appendix A). This applies to all other subsequent tables with similar instances. All percentages are recorded within each country’s number of respondents to identify specific features better.
3.5. Available Interventions in Sampled Countries as Perceived by Respondents in Dealing with Health Problems of Climate Change Impacts
Table 7 reveals some intervention programs to deal with climate change impacts as perceived by respondents. The table indicates that all sampled countries have programs to address water and vector-borne diseases and control, programs to secure the public health livelihood, especially the vulnerable ones in times of extreme events, and the coping and adaptation plan to build the country’s resilience regarding climate change impacts. Their effectiveness remains a big challenge, as seen in the table. All the respondents revealed considerable percentages to define the ineffectiveness of the existing intervention programs in each country. Some of the available programs mentioned by the respondents include the following: the ‘WASH’ campaign program to deal with water provision, sanitation and hygiene, borehole drilling, an emergency management agency, a climate-resilient water safety plan, environmental sanitation–drainage operations, a mosquito and vector spraying project, a planting for food and jobs program, climate watch and predictions, awareness creation using radio and television, disease and emergency notifications, afforestation programs to reduce the risk of extreme events, carbon dioxide removal and risk management, the National Disaster Management Organization (NADMO), flood warnings and a temporary shelter program in coastal and flood-prone areas, a South African expert on nutrition, food security/distribution during a famine, community awareness and a sensitisation program.

Table 7.
Sampled countries’ intervention programs to deal with the health impacts of climate change as perceived by respondents.
Respondents’ perceptions of disaster relief agencies in the sampled countries are presented in Table 8. Although these agencies/organisations exist in the sampled African countries, their practical implementation on a wide range of climate crises becomes challenging. It is seen from the table that those that exist are insufficient in operation in times of heavy impacts, such as flooding. Some of these existing organisations, as mentioned by the respondents, are as follows:

Table 8.
Respondents’ perception of sampled country’s disaster relief agencies/organisations helps victims of extreme food distribution and shelter victims.
The National Disaster Management Organization (NADMO); The United Nations International Children’s Emergency Fund (UNICEF); The National Emergency Management Agency; USAID; World Vision; ADRA, National Disaster Prevention and Management Agency; Disaster Risk Reduction Commission; The Red Cross; Gift of the Givers, providing support in drought-prone areas; NEMA; LASEMA; The AYA Foundation; EHPs Disaster Risk Management; Meals on Wheel (N.G.O.); Public Health Emergency and Preparedness Agency; Catholic Relief Agency; and F.A.O.
The financial response from the sampled country’s government and the needed funding/budget at the health sectors as perceived by the respondents are presented in Table 9. A total of 83.9% of responses, especially from Ghana, revealed that climate change is not well incorporated into public health intervention. A total of 77. 4% perceived that the intervention programs available are technically not well supported by the Ghanaian government. Due to this, 90% perceived the need for funding in the health systems’ resources to sufficiently build resilience to climate change anomalies, particularly for vulnerable populations. Compared with South Africa, respondents revealed a lower percentage, partly due to their excellent health systems managed by the government. The percentage differences in Table 7 and Table 8, on account of South Africa performance in times of climate change crises, are too low and, as such, confirm the assertion that the health system preparedness in response to climate change impacts with their support from the government is, in one way or the other, equipped with the necessary resources compared to other sampled African countries. However, 77.8% of responses still claimed that the health sector needs additional resources to fully prepare themselves for future uncertainties posed by a changing climate, as shown in Table 10.

Table 9.
Technical support from sampled countries’ government and the needed funding/budget in developing preparedness plans and communicating with the public about climate change’s health effects, as perceived by respondents.

Table 10.
Respondents’ perceptions about the health system’s available resources and those needed to curb climate change (CC) impact human health in the sampled countries.
3.6. Resources Availability in the Sampled African Countries and Those Needed to Deal with Climate Change Impacts as Perceived by Respondents
Respondents reacted to the resources available within each sampled country to respond to climate change health problems in Table 10. Respondents further mentioned the country’s additional resources needed to ultimately reduce the change impacts and build resilience, particularly for the vulnerable populations. From the table, despite some of the countries’ performance (South Africa, Ghana, Namibia), all the sampled countries have limited resource availability (higher than 60%). This confirms respondents’ perceptions of the escalation of health problems resulting from climate change impacts because of the unavailable resources in the health systems to effectively deal with the increasing prevalence of diseases and other uncertainties. Most of the respondents (higher than 60%) from each sampled country suggested that for their country to equip themselves fully and thoroughly prepare for current and future health hazards posed by a changing climate, the health systems need to construct more hospitals and healthcare centres. These must include all hard-to-reach communities in the country where the most vulnerable populations are. When these hospitals and healthcare centres are adequately resourced with medical equipment, sufficient health professionals in all fields with enough training, particularly in the mental health field, are needed to take care of victims of climate change impacts.
Having prepared for curative measures, most of the respondents further perceived preventive steps to control future climate change impacts by having an effective surveillance system in the country. When a coordination framework exists between the health systems and the meteorological department to access relevant weather and climate data, the health system plans and implements health programs towards future uncertainties. Again, South African surveillance systems undoubtedly perform better than other countries (44.4%).
More so, almost all the responses mentioned that all the sampled African countries needed emergency response resources. The health systems’ preparedness towards future health problems to involve equipping the country, in rural and urban communities, with ambulances, fire brigadiers, and possibly helicopters to help control and prevent health emergencies caused by climate change impacts are an essential factor to contribute to the sampled country’s coping and adaptation strategies towards resilience.
4. Discussion
This study principally focused on assessing the preparedness of public health systems in African countries to cope with climate change health hazards. Our results revealed that climate change had been extensively experienced within the sampled African countries, with floods and extreme temperatures being experienced in West Africa, mostly in Ghana and Nigeria. The revelation is confirmed by several studies in the reviewed literature of this study [50,59,64,65]. Drought and extreme temperatures have also been experienced in the Eastern African countries, specifically in Ethiopia and Kenya; meanwhile, the Southern African countries (South Africa and Namibia) also experienced much drought and extreme temperatures. This study shows that extreme temperatures are common impacts of climate change in all the sampled countries. Concurrently, floods and erratic rainfall had also been experienced in all the sampled countries.
4.1. Vulnerability to Climate Change Impacts on Human Health and the Health Systems’ Perception
Extreme weather events experienced in the sampled countries have caused an increase in disease prevalence, such as malaria (endemic in most African countries) and other vector-borne diseases, particularly in Ghana and Nigeria, as the most affected countries. Malnutrition, food insecurity and food-borne diseases are notably occurring in Ethiopia and Nigeria. This confirms the assertion that drought, floods, and extreme temperatures are the most occurring impacts in these countries. Among the sampled countries, Ghana reported the highest effects of climate change on human health. A confirmation of this is seen in a study that applied a series of five hypothetical cases to review the climate impacts on the health and wellbeing of individuals and the population in Sub-Saharan Africa [6]. Additionally, most of the respondents consented to the increase in the trend of climate-induced diseases from the past until now. The result of a study which demonstrated the populations’ impacts from multiple health and social stressors towards extreme weather events is a confirmation to this report [21]. The respondents revealed a significant increase in the trend of diseases and a projection of these diseases in the future if the impacts of climate change are not addressed. Several factors included the government’s inability to collaborate with the relevant stakeholders to ensure adequate training for all health professionals in the health system to address climate change impacts in the sampled African countries, limited funding from the government, insufficient healthcare centres and hospitals, inadequate staff members, inefficient disease surveillance systems, and unavailability of resources, such as medical equipment, rapid response units and their resources (ambulances, fire service van, helicopters in times of flooding and other extreme events).
Our survey again focused on relationships between climate change impacts and food insecurity. The findings showed that drought, caused by extreme temperatures, has a significant effect on food insecurity and affects the vulnerable population’s health in the sampled countries, most notably in Ethiopia and Nigeria, which respondents perceived to be the two most affected countries. A study conducted in the Horn and Southern Africa, where 14 million lives in Ethiopia, Kenya, Malawi, and Zimbabwe were endangered due to drought, confirmed this report regarding Ethiopia [78]. An ecological study in their findings again indicated that frequent drought increases the population’s food insecurity from 10% to 15% in Ethiopia [54]. From the outcome of this study, the strength of the local capacities in the sampled countries regarding the health system’s eagerness to respond to climate change is weak. According to the respondents’ perceptions, the various intervention programs of the government and N.G.O.s to assist with and address public health issues with food insecurity, vector control and infectious disease prevention in times of climate crises in the sampled countries are inadequate, and those available are ineffective, as seen in the results above. This calls for the sampled African countries to intensify local capacity building in response to their public health vulnerability to climate disasters.
4.2. Health System’s Preparedness
Climate change management in the sampled countries needs more attention regarding adaptation and resilience strategies. The justification is found in the diversity of impacts across the continent and each country’s preparedness based on its available resources to deal with the effects. From the studied sampled countries, it was observed that South Africa is making significant progress in its readiness to deal with climate change health impacts. A justification of this is a study that systematically assessed climate change adaptation in the health sector in South Africa and finds significant progress in policy frameworks for climate change, surveillance systems and training curricula for health workers [21].
Several studies argued that each affected nation’s emergency preparedness, response, and recovery activities should widely include human resilience building [79,80,81]. Such action actively needs health professionals with adequate skills and knowledge of handling impacts because healthcare workforces appear at the frontline when it comes to hazards that impact human health. However, the sampled countries’ cases are characterised by low skilled personnel to respond to the impacts. At this stage, the core mission of healthcare structures that provide and secure the public health’s wellbeing is questioning the concerning nations in the most affected areas of the globe.
Education on the climate change impact on human health in the healthcare sector fails to give adequate attention to the roles of the larger eco-systems within which it operates [82]. A study justifies this statement that health professionals’ knowledge of the climate change impact on health should be assessed and suggests the urgent need for education on climate matters [83]. The results of other studies argue that nurses play a vital role in the mitigation, adaptation, and resilience to the climate change impact on human health [84,85,86]. To follow this argument, medical schools in the sampled African countries should find it lawful to integrate climate change into the medical school curriculum to incorporate curricula practice, research, and policy regarding climate change impacts on the environment and human health [87,88,89]. Such action will improve hospital staff’s responsibilities, skills, and competencies regarding responses to climate change’s impact on human health.
The risk and effects of climate change on mental health are increasing, and intervention to address the issue needs to tackle the problem in a holistic manner [90]. A study reported that child psychological wellbeing is directly and indirectly affected by climate change, and the worst impact occurred in the developing world [91]. These studies confirm our survey, which revealed a lower number of mental health professionals in the health system, addressing the mental health consequences of extreme events on public health. The mental health professional’s role in mitigating climate change impacts and applying strategies to help humans cope with its effects is of more excellent value than reported in a study [91].
4.3. Available Interventions
This study revealed that the evidence of incorporating climate change into public health intervention is yet to be realised in the sampled countries. However, public health interventions or programs in the sampled countries are well observed. It is a compelling illustration of the local institutions’ weakness in response to climate change impacts on public health. This remark is in line with the result of a study that questioned how reinforcing the public health capacity to respond to extreme events had received less attention [92]. An admitted submission of a study reported the need to incorporate climate change management when implementing public health interventions [93]. South Africa, among the sampled countries, appears to perform with outstanding progress relating to this issue. It challenges other individual African countries in the engagement of long-term interventions in managing climate change impacts on public health.
4.4. Effectiveness of the Available Resources
This study’s critical findings provided clear evidence of ineffective and non-existent disaster relief agencies or programs to assist vulnerable populations and the state’s technical support on developing resources to help public health in case of climate disasters. Most respondents further perceived preventive steps to control future climate change impacts by having effective surveillance systems. When a coordination framework exists between the health systems and the meteorological department to access relevant weather and climate data, the health system plans and implements health programs towards future uncertainties. Again, South African surveillance systems undoubtedly perform better than those of other countries (44.4%).
4.5. Policy Application
Policy applications in the sampled African countries regarding improving the present and future generations’ livelihoods in Africa’s climates conditions are lacking. Therefore, we raise the need for the sampled African countries to execute the following:
- Improve policy frameworks to better consider the many health problems associated with climate change.
- Improve training provisions to raise awareness among professionals in the health sector about the connections between climate change and health.
- Improve frameworks for information exchange and the dissemination of best practice across Africa so that successful initiatives dealing with the nexus of climate change and health may be replicated.
Successful application of such policies will help close the gap and address the barriers to successfully implementing adequate coping and adaptation strategies.
Advantage and Limitations of the Methodology
The methodology used to perform this study has some advantages. For instance, a survey seemed to be an appropriate way to access a significant group of participants across the African continent as a method. In addition, the technique used permitted the authors to collect data from each participant at a single point in time. Additionally, it provided a picture of the regularity of health hazards in the sampled countries at a precise moment. Moreover, through this methodology, the massive health needs of sampled countries are assessed, providing a sound basis to inform the planning and health authorities about some of the items they may need to consider in allocating health resources. This study’s evidence is also timely since it may help African countries adjust their health systems to cope with climate change.
However, this study also presented some limitations. Firstly, it only focused on six African countries and did not have the ambition to cover the whole African continent. Additionally, some associations that were identified between climate change and health seemed challenging to interpret since they are not exclusive to climate change. Some structural problems also hinder the handling of various types of diseases. Moreover, because this methodology offers only a one-time measurement of exposure and outcome, it is challenging to evaluate the causal relationship from the data set available.
5. Conclusions
The paper presents an overview of some of the health problems associated with climate change across Africa. A cross-sectional study involving six African countries (Ghana and Nigeria in West Africa, Namibia and South Africa in Southern Africa, Kenya, and Ethiopia in East Africa) analysed the prevailing vulnerability to climate change’s impacts on human health on the one hand and the degree of preparedness of the health systems to cope with them, on the other.
It identifies several trends. First, the levels of knowledge and perceptions about climate variability and public health impacts in the sampled countries are varied. The study also shows that the health impacts of climate change have been extensive, to a greater or at least to some extent, illustrating the fact that they are part of the routine in the investigated countries. Most of the respondents also stated that climate-induced diseases might increase in the future and that future climate changes are not addressed.
The sampled health professionals’ view is that the degree of preparedness of their health systems to deal with the health impacts of climate change in their countries is somewhat limited, a trend that is a reason for concern due to expected increases in the intensity of climate change.
Overall, the responses and examples provided from the sampled countries offer helpful insights into the nature of the nexus of climate change and health, their scope, and possible consequences. It is evident from the study that urgent action is needed to place African countries in a better position to handle the many challenges that climate change poses to them presently and in the future.
The implications of the study are manifold. For instance, it shows that significant differences in the levels of interventions at the country level exist regarding their capacity to handle climate change’s health impacts. There also seems to be a perceived need for disaster relief agencies/organisations to emphasise climate change as part of their work.
Climate change and the effects on human health, the environment, and society will continue to be significant issues in African countries, for which answers need to be found. They pose a challenge to health systems, the governments and health professionals in the coming years. Our findings will be widely shared with health professionals in African countries to support this process to address the barriers to implementing coping and adaptation strategies of climate change impacts on public health.
There is a perceived need for a greater understanding of climate-related health impacts, which can only be addressed through interdisciplinary research across hierarchical levels and geographical and political boundaries. Because of the challenges that are and will be faced in Africa, it is necessary to sensitise the public and politicians to this topic and support health professionals’ work.
Author Contributions
W.L.F. concept, S.K.O. data collection and processing, F.H. data support, O.A., survey support. All authors have read and agreed to the published version of the manuscript.
Funding
International Climate Change Information and Research Programme (ICCIRP).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
All respondents were informed about the confidentiality of their data.
Data Availability Statement
All original data are available for consultation.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
The questionnaire aims to gather the information that can help assess the preparedness of the health systems in African countries to cope with the health hazards posed by climate change. Six African countries are under study: Ghana, Nigeria, Namibia, South Africa, Ethiopia, and Kenya. The survey seeks to assess the knowledge and perceptions of health professionals from these African countries on the anomalies of climate change on human health, to what extent the country is vulnerable to climate change impacts and how sustainable the preparedness is to deal with unforeseen climate impacts and identify best practices in dealing with climate change impacts on human health.
Background Information
Gender: Male…………… Female……… Prefer not to say………..
Age: ………………..
Country: Ghana…….. Nigeria……. South Africa……… Namibia……. Ethiopia…. Kenya………
City/region: ……….
Respondent’s workplace
N.G.O.…………………………………….
Government Agency………………….
Higher educational institution………..
Other……………………………………
Position of respondents
Answer…………………
Knowledge and perception of climate change and health impacts
1. Where do you obtain your climate/weather data?
Meteorological agent…………………
Radio/television……………………….
Internet…………………………………
Other……………………………………
2. Do you know the potential public health impacts of climate change?
Yes, a lot…………………..
Yes, some…………………
Yes, but just a little……….
3. If yes, would you please list down the potential health impacts of climate change that you know?
Your answer…………………………………………………………………………………
Public health’s vulnerability to climate change impacts in the country
4. Has the country experienced climate change in the past years?
Yes, very much so………………….
Yes, a little…………………………..
No, not at all…………………………
5. If yes, which of the following have been observed as impacts? Can you please tick and rank only the observed impacts according to their magnitude of occurrence?
| Climate Impacts | Most Frequent | More Frequent | Frequent | Less Frequent | Least Frequent |
| Floods | |||||
| Drought | |||||
| Wildfires | |||||
| Extreme temperature | |||||
| Sea level rise | |||||
| Change in Precipitation | |||||
| Increase carbon dioxide | |||||
| Other |
6. Have you observed any health problems associated with these impacts in the country?
Yes, very much so…………………..
Yes, a little…………………………..
No, not at all………………………..
7. If yes, which of the following public health problems have been observed in your country/regions? Can you please tick and rank only the observed effects according to their prevalence?
| Most Prevalent | More prevalent | Prevalent | Less Prevalent | Least Prevalent | |
| Malaria and other vector-borne diseases | |||||
| Diarrhoea, water-borne diseases, and sanitation | |||||
| Malnutrition, food-borne and food insecurity | |||||
| Climate-induced mental health consequences | |||||
| Extreme weather events |
8. What do you think about the trend of the diseases/ situations above, from the past until now?
Increased…………………………………….
Decreased……………………………………
No change, prevailing……………………..
I do not know………………………………
9. In the next 15–20 years, what do you think will likely trend the country’s health mentioned above problems following future climate change?
Increase………………………………………
Decrease……………………………………..
Stabilise………………………………………
Preparedness
10. Is preparedness to deal with climate change’s public health impacts a priority in the country/region?
Yes, very much so…………………..
Yes, a little……………………………
No, not at all………………………….
11. Are there enough experts/professionals in the country/region who can assess potential public health impacts associated with climate change?
Yes, enough……………………………..
Yes, but not enough…………………….
No, not at all……………………………..
12. Are there enough health care delivery systems in your country/regions —including the hospitals, health centres, and clinics, to address climate change impact on health?
Yes, enough…………………………………
Yes, but not enough……………………….
No, not at all…………………………………
13. Are there enough mental health professionals/centres in the country/region to address extreme public health’s cognitive consequences?
Yes, enough…………………………………
Yes, but not enough………………………..
No, not at all………………………………..
14. Do public health professionals in the country/region have enough training on health risks interventions related to climate change?
Yes, enough…………………………….
Yes, but not enough……………………
No, not at all…………………………….
15. Do hospitals, health centres and clinics in the country/region have enough health personnel to deal with health problems associated with climate change?
Yes, enough…………………………….
Yes, but not enough……………………
No, not at all……………………………
16. How prepared are the health systems in your country to respond to extreme events (floods, drought, wildfires, extreme temperature?
Very well prepared………………………..
Fairly well prepared………………………
Not so much prepared………………….
Not at all…………………………………..
Interventions
17. Do you think climate change is incorporated into public health intervention?
Yes, very much so……………………..
Yes, a little………………………………
No, not at all…………………………….
18. Do you have technical support from the government forecasting local effects, developing preparedness plans, and communicating with the public about climate change’s health effects?
Yes, very much so………………………...
Yes, a little…………………………………..
No, not at all………………………………..
19. Do you know of the following public health interventions/programs in your country/region to deal with climate change impacts; how effective or ineffective these interventions/programs are if they exist?
| Intervention programs | Yes, and Effective | Yes, but not Effective | No, they do not Exist |
| Water availability, sanitation, and water-borne diseases control | |||
| Vector control | |||
| Nutrition, food safety and distribution during a famine | |||
| Extreme events adaptation |
20. If yes, what are some of the interventions/programs to deal with climate change impacts in your country/region? Please give your answers according to the numbers provided on a separate line. Do not repeat the options, please (e.g., 1…..., 2....)
1. water availability, sanitation and water-borne; 2. Vector control
21. Are there enough disaster relief agencies/programs to assist public health with food distribution in case of climate disasters?
Yes, enough…………………………
Yes, but not enough………………..
No, Not at all………………………..
22. If yes, can you please give examples of those existing programs/agencies in question 21.?
Your answer…………………………….
23. Do you think the country’s public health systems are building resilience to unforeseen climate change impacts?
Yes, I strongly think so………………………
Yes, but not enough……………………….
No, I do not think so…………………………
Resources Availability
24. Do the health systems have available resources to deal with climate change impacts on human health?
Yes, Largely available…………………
Yes, to some extent……………………
Yes, but limited…………………………
No, not at all…………………………….
25. Which other resources below do you think are needed by the health systems to help curb climate change’s health impacts?
Expanding and construction of more health centres
Additional staff
Staff training
medical equipment
Budgets/Money/funding
Surveillance systems
Quick response or emergency relief resources (ambulances, helicopters, firefighting van etc.)
Other:
References
- Halim, S.A.; Dasgupta, P.; Hayward, B.; Kanninen, M. Chapter 5: Sustainable Development, Poverty Eradication 2 and Reducing Inequalities 2017. Available online: https://www.ipcc.ch/site/assets/uploads/sites/2/2019/03/SR15_FOD_Chapter5.pdf (accessed on 25 January 2021).
- Pachauri, D.R.K.; Reisinger, A. IPCC Fourth Assessment Report 2007; Synthesis Report. Contribution of Working Groups I II and III to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change; IPCC: Geneva, Switzerland, 2007; p. 17. [Google Scholar]
- Stocker, T.F.; Qin, D.; Plattner, G.-K.; Tignor, M.M.B.; Allen, S.K.; Boschung, J. Working Group I Contribution to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change 2014; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2007; p. 14. [Google Scholar]
- Falkner, R. The Paris agreement and the new logic of international climate politics. Int. Aff. 2016, 92, 1107–1125. [Google Scholar] [CrossRef]
- Tchilibou, M.; Delcroix, T.; Alory, G.; Arnault, S.; Reverdin, G. Variations of the tropical Atlantic and Pacific, S.S.S. minimum zones and their relations to the ITCZ and SPCZ rain bands (1979–2009). J. Geophys. Res. Ocean. 2015, 120, 5090–5100. [Google Scholar] [CrossRef]
- Mpelasoka, F.; Awange, J.L.; Zerihun, A. Influence of coupled ocean-atmosphere phenomena on the Greater Horn of Africa droughts and their implications. Sci. Total. Environ. 2018, 610–611, 691–702. [Google Scholar] [CrossRef] [PubMed]
- Erickson, L.E. Reducing greenhouse gas emissions and improving air quality: Two global challenges. Environ. Prog. Sustain. Energy 2017, 36, 982–988. [Google Scholar] [CrossRef]
- World Health Organization. Noncommunicable Diseases: Key Facts. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 26 October 2020).
- Ritchie, H.; Roser, M. Causes of Death; Published online at OurWorldInData.og. 2018. Available online: https://ourworldindata.org/causes-of-death (accessed on 25 January 2021).
- Siderius, C.; Gannon, K.E.; Ndiyoi, M.; Opere, A.; Batisani, N.; Olago, D.; Pardoe, J.; Conway, D. Hydrological response and complex impact pathways of the 2015/2016 El Niño in eastern and southern Africa. Earth’s Future 2018, 6, 2–22. [Google Scholar] [CrossRef]
- Dessalegn, O.G.; Akalu, D.S. The impacts of climate change on African continent and the way forward. J. Ecol. Nat. Environ. 2015, 7, 256–262. [Google Scholar] [CrossRef]
- Singh, V.P. Impact of climate change on the hydrologic cycle and implications for society. Environ. Soc. Psychol. 2015, 1, 36–49. [Google Scholar] [CrossRef]
- Ramin, B.M.; McMichael, A.J. Climate change and health in Sub-Saharan Africa: A case-based perspective. EcoHealth 2009, 6, 52–57. [Google Scholar] [CrossRef]
- De Souza, D.; Kelly-Hope, L.; Lawson, B.; Wilson, M.; Boakye, D. Environmental factors associated with the distribution of Anopheles Gambiae s.s in Ghana; an important vector of lymphatic filariasis and malaria. PLoS ONE 2010, 5, e9927. [Google Scholar] [CrossRef]
- De Souza, K.; Kituyi, E.; Harvey, B.; Leone, M.; Murali, K.S.; Ford, J.D. Vulnerability to climate change in three hot spots in Africa and Asia: Key issues for policy-relevant adaptation and resilience-building research. Reg. Environ. Chang. 2015, 15, 747–753. [Google Scholar] [CrossRef]
- Watts, N.; Adger, W.N.; Agnolucci, P.; Blackstock, J.; Byass, P.; Cai, W.; Chaytor, S.; Colbourn, T.; Collins, M.; Cooper, A.; et al. Health and climate change: Policy responses to protect public health. Lancet 2015, 386, 1861–1914. [Google Scholar] [CrossRef]
- Stern, D.I.; Kaufmann, R.K. Anthropogenic and natural causes of climate change. Clim. Chang. 2014, 122, 257–269. [Google Scholar] [CrossRef]
- Szulejko, J.E.; Kumar, P.; Deep, A.; Kim, K.-H. Global warming projections to 2100 using simple CO2 greenhouse gas modeling and comments on CO2 climate sensitivity factor. Atmospheric Pollut. Res. 2017, 8, 136–140. [Google Scholar] [CrossRef]
- Campbell-Lendrum, D.; Manga, L.; Bagayoko, M.; Sommerfeld, J. Climate change and vector-borne diseases: What are the implications for public health research and policy? Philos. Trans. R. Soc. B Biol. Sci. 2015, 370, 20130552. [Google Scholar] [CrossRef]
- Abaya, S.W.; Mandere, N.M.; Winqvist, N. Health officials’ perceptions of and preparedness for the impacts of climate variability on human health in the Somali region of Ethiopia. Mitig. Adapt. Strat. Glob. Chang. 2011, 16, 585–596. [Google Scholar] [CrossRef]
- Chersich, M.F.; Wright, C.Y.; Venter, F.; Rees, H.; Scorgie, F.; Erasmus, B. Impacts of climate change on health and wellbeing in South Africa. Int. J. Environ. Res. Public Health 2018, 15, 1884. [Google Scholar] [CrossRef]
- Brousse, O.; Georganos, S.; Demuzere, M.; Vanhuysse, S.; Wouters, H.; Wolff, E.; Linard, C.; van Lipzig, N.P.-M.; Dujardin, S. Using local climate zones in Sub-Saharan Africa to tackle urban health issues. Urban Clim. 2019, 27, 227–242. [Google Scholar] [CrossRef]
- Schulte-Uebbing LHansen, G.; Hernández, A.M.; Winter, M. Chapter scientists in the IPCC AR5—experience and lessons learned. Curr. Opin. Environ. Sustain. 2015, 14, 250–256. [Google Scholar] [CrossRef]
- Frumkin, H.; Hess, J.; Luber, G.; Malilay, J.; McGeehin, M. Climate change: The public health response. Am. J. Public Health 2008, 98, 435–445. [Google Scholar] [CrossRef]
- Hathaway, J.; Maibach, E.W. Health implications of climate change: A review of the literature about the perception of the public and health professionals. Curr. Environ. Health Rep. 2018, 5, 197–204. [Google Scholar] [CrossRef]
- Rahman, M.S.; Bin Mohamad, O.; Bin Abu Zarim, Z. Climate change: A review of its health impact and perceived awareness by the young citizens. Glob. J. Health Sci. 2014, 6, 196–204. [Google Scholar] [CrossRef]
- Byass, P. Climate change and population health in Africa: Where are the scientists? Glob. Health Action 2009, 2, 2065. [Google Scholar] [CrossRef]
- Trtanj, J.; Jantarasami, L.; Brunkard, J.; Collier, T.; Jacobs, J.; Lipp, E.; McLellan, S.; Moore, S.; Paerl, H.; Ravenscroft, J.; et al. 6: Climate Impacts on Water-Related Illness. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment; U.S. Global Change Research Program: Washington, DC, USA, 2016. [Google Scholar]
- De Magny, G.C.; Cazelles, B.; Guégan, J.-F. Cholera threat to humans in Ghana is influenced by both global and regional climatic variability. EcoHealth 2007, 3, 223–231. [Google Scholar] [CrossRef]
- Leckebusch, G.C.; Abdussalam, A.F. Climate and socioeconomic influences on interannual variability of cholera in Nigeria. Health Place 2015, 34, 107–117. [Google Scholar] [CrossRef]
- Nkoko, D.B.; Giraudoux, P.; Plisnier, P.-D.; Tinda, A.M.; Piarroux, M.; Sudre, B.; Horion, S.; Tamfum, J.-J.M.; Ilunga, B.K.; Piarroux, R. Dynamics of cholera outbreaks in great lakes region of Africa, 1978–2008. Emerg. Infect. Dis. 2011, 17, 2026–2034. [Google Scholar] [CrossRef]
- Abu, M.; Codjoe, S.N.A. Experience and future perceived risk of floods and diarrheal disease in urban poor communities in Accra, Ghana. Int. J. Environ. Res. Public Health 2018, 15, 2830. [Google Scholar] [CrossRef]
- Musengimana, G.; Mukinda, F.K.; Machekano, R.; Mahomed, H. Temperature variability and occurrence of diarrhoea in children under five-years-old in cape town metropolitan sub-districts. Int. J. Environ. Res. Public Health 2016, 13, 859. [Google Scholar] [CrossRef]
- Azage, M.; Kumie, A.; Worku, A.; Bagtzoglou, A.C.; Anagnostou, E. Effect of climatic variability on childhood diarrhea and its high risk periods in northwestern parts of Ethiopia. PLoS ONE 2017, 12, e0186933. [Google Scholar] [CrossRef] [PubMed]
- Gunnarsson, H.; Sanseovic, A.-M. Possible Linkages Between Algae Toxins in Drinking Water and Related illnesses in Windhoek, Namibia 2001; p. 34. Available online: http://urn.kb.se/resolve?urn=urn:nbn:se:hkr:diva-4761 (accessed on 25 January 2021).
- Tschakert, P.; Ricciardi, V.; Smithwick, E.; Machado, M.; Ferring, D.; Hausermann, H.; Bug, L. Situated knowledge of pathogenic landscapes in Ghana: Understanding the emergence of Buruli ulcer through qualitative analysis. Soc. Sci. Med. 2016, 150, 160–171. [Google Scholar] [CrossRef] [PubMed]
- Ekpo, U.F.; Mafiana, C.F.; O Adeofun, C.; Solarin, A.R.; Idowu, A.B. Geographical information system and predictive risk maps of urinary schistosomiasis in Ogun State, Nigeria. BMC Infect. Dis. 2008, 8, 74–111. [Google Scholar] [CrossRef]
- Adu-Prah, S.; Tetteh, E.K. Spatiotemporal analysis of climate variability impacts on malaria prevalence in Ghana. Appl. Geogr. 2015, 60, 266–273. [Google Scholar] [CrossRef]
- Weli, V.E.; Efe, S.I. Climate and epidemiology of malaria in port Harcourt region, Nigeria. Am. J. Clim. Chang. 2015, 4, 40–47. [Google Scholar] [CrossRef]
- Adeola, A.M.; Botai, J.O.; Rautenbach, H.; Adisa, O.M.; Ncongwane, K.P.; Botai, C.M.; Adebayo-Ojo, T.C. Climatic variables and malaria morbidity in Mutale local municipality, South Africa: A 19-year data analysis. Int. J. Environ. Res. Public Health 2017, 14, 1360. [Google Scholar] [CrossRef] [PubMed]
- Komen, K.; Olwoch, J.; Rautenbach, H.; Botai, J.; Adebayo, A. Long-run relative importance of temperature as the main driver to Malaria transmission in Limpopo province, South Africa: A simple econometric approach. EcoHealth 2014, 12, 131–143. [Google Scholar] [CrossRef]
- Codjoe, S.N.A.; Nabie, V.A. Climate change and Cerebrospinal Meningitis in the Ghanaian Meningitis Belt. Int. J. Environ. Res. Public Health 2014, 11, 6923–6939. [Google Scholar] [CrossRef]
- Bauer, J.M.; Mburu, S. Effects of drought on child health in Marsabit district, northern Kenya. Econ. Hum. Biol. 2017, 24, 74–79. [Google Scholar] [CrossRef]
- Grace, K.; Davenport, F.; Funk, C.; Lerner, A.M. Child malnutrition and climate in Sub-Saharan Africa: An analysis of recent trends in Kenya. Appl. Geogr. 2012, 35, 405–413. [Google Scholar] [CrossRef]
- Hagos, S.; Lunde, T.; Mariam, D.H.; Woldehanna, T.; Lindtjørn, B. Climate change, crop production and child under nutrition in Ethiopia; a longitudinal panel study. BMC Public Health 2014, 14, 884. [Google Scholar] [CrossRef]
- Atitsogbey, P. The impact of climate change on food and nutrition security in the Bongo district of the upper east region of Ghana. Bachelor’s Thesis, University of Ghana, Accra, Ghana, 2016; p. 153. [Google Scholar]
- Codjoe, S.N.A.; Owusu, G. Climate change/variability and food systems: Evidence from the Afram Plains, Ghana. Reg. Environ. Chang. 2011, 11, 753–765. [Google Scholar] [CrossRef]
- Achaglinkame, M.A.; Opoku, N.; Amagloh, F.K. Aflatoxin contamination in cereals and legumes to reconsider usage as complementary food ingredients for Ghanaian infants: A review. J. Nutr. Intermed. Metab. 2017, 10, 1–7. [Google Scholar] [CrossRef]
- Armah, F.A.; Odoi, J.O.; Yengoh, G.T.; Obiri, S.; Yawson, D.O.; Afrifa, E.K.A. Food security and climate change in drought-sensitive savanna zones of Ghana. Mitig. Adapt. Strat. Glob. Chang. 2010, 16, 291–306. [Google Scholar] [CrossRef]
- Onafeso, O.D.; Akanni, C.O.; Badejo, B.A. Climate change dynamics and imperatives for food security in Nigeria. Indones. J. Geogr. 2016, 47, 151. [Google Scholar] [CrossRef]
- Idoko, I.D. An impact assessment of flooding on food security among rural farmers in dagiri community, of Gwagwalada area council, Abuja, Nigeria. Agric. Dev. 2016, 1, 6–13. [Google Scholar] [CrossRef]
- Masipa, T.S. The impact of climate change on food security in South Africa: Current realities and challenges ahead. Jàmbá J. Disaster Risk Stud. 2017, 9, 7. [Google Scholar] [CrossRef]
- Akudugu, M.A.; Alhassan, A.-R. Climate change menace, food security, livelihoods, and social safety in northern Ghana. Int. J. Sustain. Dev. 2012, 1, 80–95. [Google Scholar]
- Endalew, B.; Muche, M.; Tadesse, S. Assessment of food security situation in Ethiopia: A review. Asian J. Agric. Res. 2015, 9, 55–68. [Google Scholar] [CrossRef]
- Hooli, L.J. Resilience of the poorest: Coping strategies and indigenous knowledge of living with the floods in northern Namibia. Reg. Environ. Chang. 2015, 16, 695–707. [Google Scholar] [CrossRef]
- Anthonj, C.; Nkongolo, O.T.; Schmitz, P.; Hango, J.N.; Kistemann, T. The impact of flooding on people living with HIV: A case study from the Ohangwena region, Namibia. Glob. Health Action 2015, 8, 26441. [Google Scholar] [CrossRef]
- Shifidi, V.T.; Tuwilika, S.V. Impact of flooding on rural livelihoods of the Cuvelai Basin in northern Namibia. J. Geogr. Reg. Plan. 2016, 9, 104–121. [Google Scholar] [CrossRef]
- Angula, M.N.; Kaundjua, M.B. The changing climate and human vulnerability in north-central Namibia. Jàmbá: J. Disaster Risk Stud. 2016, 8, 7. [Google Scholar] [CrossRef]
- Addo, I.Y.; Danso, S. Sociocultural factors and perceptions associated with voluntary and permanent relocation of flood victims: A case study of Sekondi-Takoradi Metropolis in Ghana. Jàmbá J. Disaster Risk Stud. 2017, 9, 157. [Google Scholar] [CrossRef]
- Dziwornu, E.; Kugbey, N. Mental health problems and coping among flood victims in Ghana: A comparative study of victims and non-victims. Curr. Res. Psychol. 2015, 6, 15–21. [Google Scholar] [CrossRef]
- Shabu, T.; Adaaku, E.M. Natural disaster and household vulnerability to crime in flood-prone areas of urban centres in Nigeria. Ph.D. Thesis, Benue State University, Makurdi, Nigeria, 2018; p. 16. [Google Scholar]
- Acharibasam, J.W.; Anuga, S.W. Psychological distance of climate change and mental health risks assessment of smallholder farmers in northern Ghana: Is habituation a threat to climate change? Clim. Risk Manag. 2018, 21, 16–25. [Google Scholar] [CrossRef]
- Ajibade, I.; McBean, G.; Bezner-Kerr, R. Urban flooding in Lagos, Nigeria: Patterns of vulnerability and resilience among women. Glob. Environ. Chang. 2013, 23, 1714–1725. [Google Scholar] [CrossRef]
- Eludoyin, O.M.; Adelekan, I.O.; Webster, R.; Eludoyin, A.O. Air temperature, relative humidity, climate regionalization and thermal comfort of Nigeria. Int. J. Clim. 2013, 34, 2000–2018. [Google Scholar] [CrossRef]
- Daniel, O.A. Urban extreme weather: A challenge for a healthy living environment in Akure, Ondo State, Nigeria. Climate 2015, 3, 775–791. [Google Scholar] [CrossRef]
- Wichmann, J. Heat effects of ambient apparent temperature on all-cause mortality in Cape Town, Durban and Johannesburg, South Africa: 2006–2010. Sci. Total. Environ. 2017, 587–588, 266–272. [Google Scholar] [CrossRef]
- Frimpong, K.; MPHIL development studies; Van Etten, E.J.E.; Oosthuzien, J.; Nunfam, V.F. Heat exposure on farmers in northeast Ghana. Int. J. Biometeorol. 2016, 61, 397–406. [Google Scholar] [CrossRef]
- Ngwenya, B.; Oosthuizen, J.; Cross, M.; Frimpong, K.; Chaibva, C.N. A review of heat stress policies in the context of climate change and its impacts on outdoor workers. Int. J. Soc. Ecol. Sustain. Dev. 2018, 9, 1–11. [Google Scholar] [CrossRef]
- Mathee, A.; Oba, J.; Rose, A. Climate change impacts on working people (the HOTHAPS initiative): Findings of the South African pilot study. Glob. Health Action 2010, 3, 5612. [Google Scholar] [CrossRef]
- Oa, O.V.A.O. A review of the future of tourism in coastal Kenya: The challenges and opportunities posed by climate change. J. Earth Sci. Clim. Chang. 2014, 5. [Google Scholar] [CrossRef]
- United Nations. African Countries by Population (2021)—Worldometer 2019. Available online: https://www.worldometers.info/population/countries-in-africa-by-population/ (accessed on 25 January 2021).
- Saidi, S.M.; Lijima, Y.; Sang, W.K.; Mwangudza, A.K.; Oundo, J.O.; Taga, K.; Aihara, M.; Nagayama, K.; Yamamoto, H.; Waiyaki, P.G.; et al. Epidemiological study on infectious diarrheal diseases in children in a coastal rural area of Kenya. Microbiol. Immunol. 1997, 41, 773–778. [Google Scholar] [CrossRef] [PubMed]
- Tsegaw, T.; Gadisa, E.; Seid, A.; Abera, A.; Teshome, A.; Mulugeta, A.; Herrero, M.; Argaw, D.; Jorge, A.; Aseffa, A. Identification of environmental parameters and risk mapping of visceral leishmaniasis in Ethiopia by using geographical information systems and a statistical approach. Geospat. Health 2013, 7, 299. [Google Scholar] [CrossRef] [PubMed]
- Kipruto, E.K.; Ochieng, A.O.; Anyona, D.N.; Mbalanya, M.; Mutua, E.N.; Onguru, D.; Nyamongo, I.K.; Estambale, B.B.A. Effect of climatic variability on malaria trends in Baringo county, Kenya. Malar. J. 2017, 16, 220. [Google Scholar] [CrossRef]
- Delbiso, T.D.; Altare, C.; Rodriguez-Llanes, J.M.; Doocy, S.; Guha-Sapir, D. Drought and child mortality: A meta-analysis of small-scale surveys from Ethiopia. Sci. Rep. 2017, 7, 2212. [Google Scholar] [CrossRef]
- Hendriks, S.L.; Van Der Merwe, C.; Ngidi, M.S.; Manyamba, C.; Mbele, M.; McIntyre, A.M.; Mkandawire, E.; Molefe, Q.N.; Mphephu, M.Q.; Ngwane, L. What are we measuring? Comparison of household food security indicators in the eastern cape province, South Africa. Ecol. Food Nutr. 2016, 55, 141–162. [Google Scholar] [CrossRef]
- Filho, W.L.; Balogun, A.-L.; Ayal, D.Y.; Bethurem, E.M.; Murambadoro, M.; Mambo, J.; Taddese, H.; Tefera, G.W.; Nagy, G.J.; Fudjumdjum, H.; et al. Strengthening climate change adaptation capacity in Africa—Case studies from six major African cities and policy implications. Environ. Sci. Policy 2018, 86, 29–37. [Google Scholar] [CrossRef]
- Watkins, K.; Ugaz, C.; Gaye, A.; Ha, W.; Johansson, C.; Kennedy, A. Human Development Report 2007–2008: Fighting Climate Change: Human Solidarity in a Divided World; United Nations Development Programme (UNDP): New York, NY, USA, 2007. [Google Scholar]
- Keim, M.E. Building human resilience. Am. J. Prev. Med. 2008, 35, 508–516. [Google Scholar] [CrossRef]
- Newman, L.; Dale, A. Network structure, diversity, and proactive resilience building: A response to Tompkins and Adger. Ecol. Soc. 2005, 10, 10. [Google Scholar] [CrossRef]
- Hughes, T.P.; Baird, A.H.; Bellwood, D.R.; Card, M.; Connolly, S.R.; Folke, C.; Grosberg, R.; Hoegh-Guldberg, O.; Jackson, J.B.C.; Kleypas, J.; et al. Climate change, human impacts, and the resilience of coral reefs. Science 2003, 301, 929–933. [Google Scholar] [CrossRef]
- Ulhøi, J.P.; Ulhøi, B.P. Beyond climate focus and disciplinary myopia. The roles and responsibilities of hospitals and healthcare professionals. Int. J. Environ. Res. Public Health 2009, 6, 1204–1214. [Google Scholar] [CrossRef]
- Bell, J.; Herring, S.; Jantarasami, L.; Adrianopoli, C.; Benedict, K.; Conlon, K.; Escobar, V.; Hess, J.; Luvall, J.; Garcia-Pando, C.; et al. 4: Impacts of Extreme Events on Human Health. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment; U.S. Global Change Research Program: Washington, DC, USA, 2016. [Google Scholar]
- Nichols, M.; Sarfo, F.S.; Singh, A.; Qanungo, S.; Treiber, F.; Ovbiagele, B.; Saulson, R.; Patel, S.; Jenkins, C.; Stephen, S.F. Assessing mobile health capacity and task shifting strategies to improve hypertension among Ghanaian stroke survivors. Am. J. Med. Sci. 2017, 354, 573–580. [Google Scholar] [CrossRef]
- McDermott-Levy, R.; Jackman-Murphy, K.P.; Leffers, J.M.; Jordan, L. Integrating climate change into nursing curricula. Nurse Educ. 2019, 44, 43–47. [Google Scholar] [CrossRef]
- Leffers, J.; Levy, R.M.; Nicholas, P.K.; Sweeney, C.F. Mandate for the nursing profession to address climate change through nursing education. J. Nurs. Sch. 2017, 49, 679–687. [Google Scholar] [CrossRef]
- Finkel, M.L. A call for action: Integrating climate change into the medical school curriculum. Perspect. Med. Educ. 2019, 8, 265–266. [Google Scholar] [CrossRef]
- Wellbery, C.; Sheffield, P.; Timmireddy, K.; Sarfaty, M.; Teherani, A.; Fallar, R. It’s time for medical schools to introduce climate change into their curricula. Acad. Med. 2018, 93, 1774–1777. [Google Scholar] [CrossRef]
- Saltzman, H.M. Medical school curricula should highlight environmental health. Acad. Med. 2019, 94, 1406. [Google Scholar] [CrossRef]
- Hayes, K.; Blashki, G.; Wiseman, J.; Burke, S.; Reifels, L. Climate change and mental health: Risks, impacts and priority actions. Int. J. Ment. Health Syst. 2018, 12, 28. [Google Scholar] [CrossRef]
- Burke, S.E.L.; Sanson, A.V.; Van Hoorn, J. The psychological effects of climate change on children. Curr. Psychiatry Rep. 2018, 20, 35. [Google Scholar] [CrossRef]
- Hess, J.J.; McDowell, J.Z.; Luber, G. Integrating climate change adaptation into public health practice: Using adaptive management to increase adaptive capacity and build resilience. Environ. Health Perspect. 2012, 120, 171–179. [Google Scholar] [CrossRef]
- Shezi, B.; Mathee, A.; Siziba, W.; Street, R.A.; Naicker, N.; Kunene, Z.; Wright, C.Y. Environmental health practitioners potentially play a key role in helping communities adapt to climate change. BMC Public Health 2019, 19, 54. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).