Wasting and Associated Factors among Children under 5 Years in Five South Asian Countries (2014–2018): Analysis of Demographic Health Surveys
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Variables
2.2. Potential Confounding Factors
2.3. Statistical Analysis
3. Results
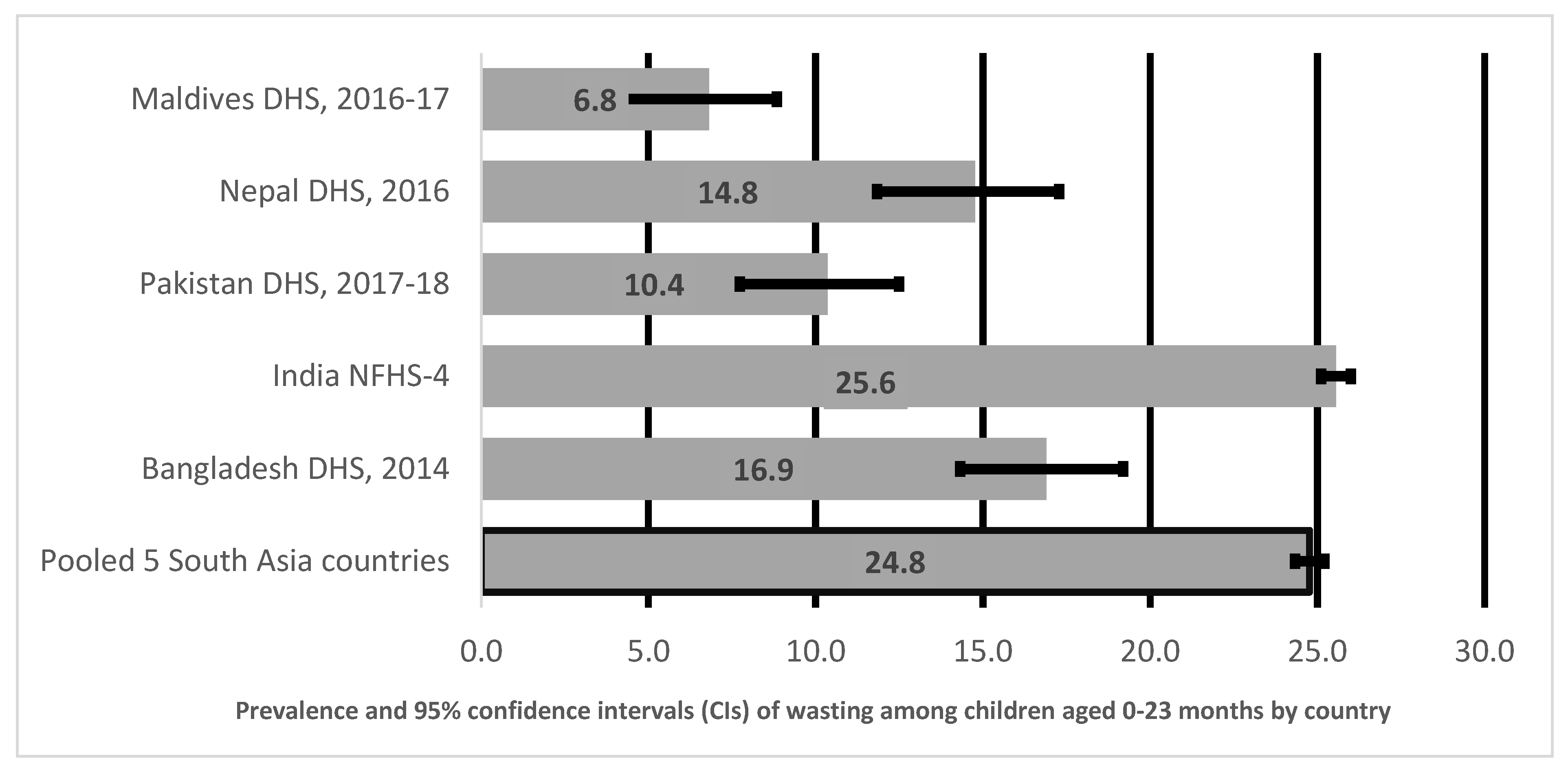
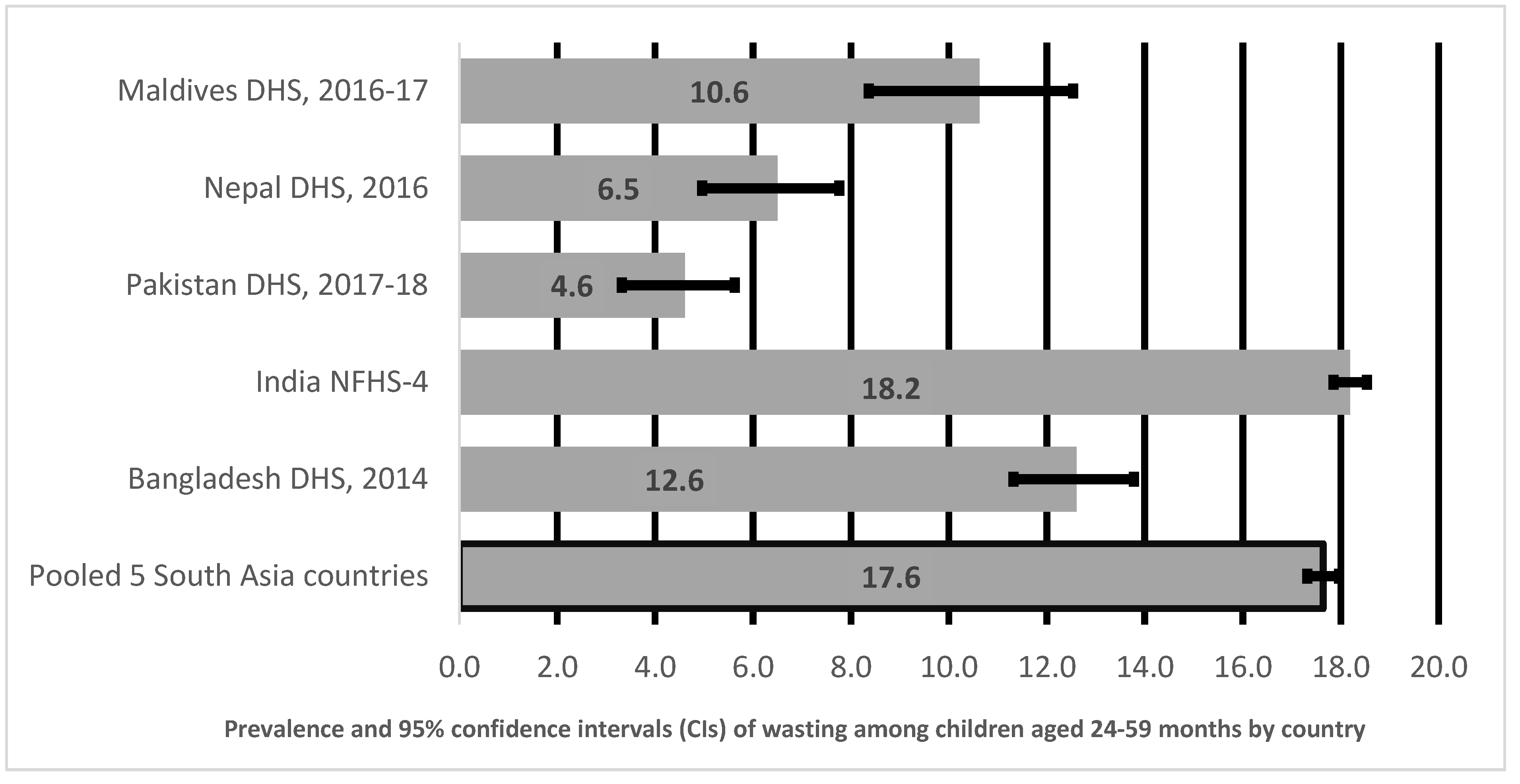
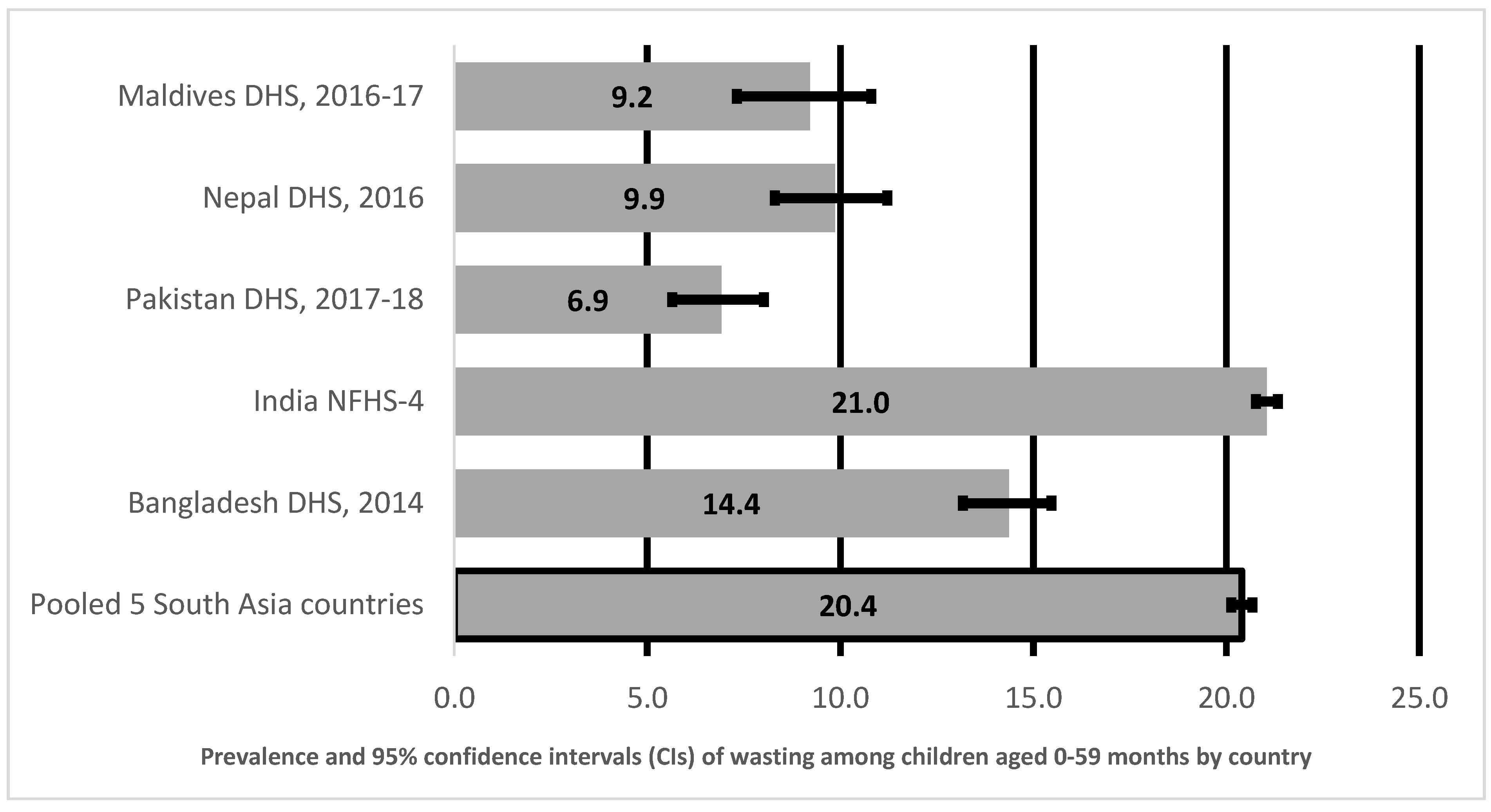
3.1. Prevalence of Wasting in Children Aged 0–23 Months, 24–59 Months and 0–59 Months
3.2. Factors Associated with Child Wasting for Children Aged 0–23 Months
3.3. Factors Associated with Child Wasting for Children Aged 24–59 Months
3.4. Factors Associated with Child Wasting for Children Aged 0–59 Months
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fernandez, I.D.; Himes, J.H.; De Onis, M. Prevalence of nutritional wasting in populations: Building explanatory models using secondary data. Bull. World Heath Organ. 2002, 80, 282–291. [Google Scholar]
- Aguayo, V.M.; Badgaiyan, N.; Dzed, L. Determinants of child wasting in Bhutan. Insights from nationally representative data. Public Health Nutr. 2016, 20, 315–324. [Google Scholar] [CrossRef]
- Khara, T.; Dolan, C. Associations between Wasting and Stunting. Policy, Programming and Research Implications; Technical Briefing Paper; Emergency Nutrition Network: London, UK, 2014. [Google Scholar]
- Kinyoki, D.K.; Osgood-Zimmerman, A.E.; Pickering, B.; Schaeffer, L.E.; Marczak, L.; Lazzar-Atwood, A.; Collison, M.L.; Henry, N.; Abebe, Z.; Adamu, A.A.; et al. Mapping child growth failure across low- and middle-income countries. Nat. Cell Biol. 2020, 577, 231–234. [Google Scholar] [CrossRef]
- De Onis, M.; Borghi, E.; Arimond, M.; Webb, P.; Croft, T.; Saha, K.; De-Regil, L.M.; Thuita, F.; Heidkamp, R.; Krasevec, J.; et al. Prevalence thresholds for wasting, overweight and stunting in children under 5 years. Public Heath Nutr. 2018, 22, 175–179. [Google Scholar] [CrossRef]
- Torlesse, H.; Le Tram, M. South Asia and Child Wasting—Unravelling the Conundrum; Field Exchange 63, October 2020. p. 7. Available online: www.ennonline.net/fex/63/southasiachildwasting (accessed on 26 December 2020).
- United Nations International Children’s Fund. Multi-Sectoral Approaches to Nutrition: Nutrition-Specific and Nutrition-Sensitive Interventions to Accelerate Progress; UNICEF: New York, NY, USA, 2014. [Google Scholar]
- Guatam, S.; Ruchal, S.; Timalsina, B.; Acharya, D.; Khadka, B.; Gautam, V.; Singh, J.K. Effect of Maternal Socio-demographic Factors and Child Feeding Practice on Wasting Among under Five Years Children in Slum Area of Rupandehi District in Nepal. J. Nepal Med. Assoc. 2017, 56, 256–261. [Google Scholar] [CrossRef]
- Rahman, M.L.; Howlader, T.; Masud, M.S. Association of Low-Birth Weight with Malnutrition in Children under Five Years in Bangladesh: Do Mother’s Education, Socio-Economic Status, and Birth Interval Matter? PLoS ONE 2016, 11, e0157814. [Google Scholar] [CrossRef] [PubMed]
- Raihan, M.J.; Farzana, F.D.; Sultana, S.; Haque, A.; Rahman, A.S.; Waid, J.L.; McCormick, B.; Choudhury, N.; Ahmed, T. Examining the relationship between socio-economic status, WASH practices and wasting. PLoS ONE 2017, 12, e0172134. [Google Scholar] [CrossRef] [PubMed]
- Tigga, P.L.; Sen, J.; Mondal, N. Association of some socio-economic and socio-demographic variables with wasting among pre-school children of North Bengal, India. Ethiop. J. Heath Sci. 2015, 25, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Harding, K.L.; Aguayo, V.M.; Webb, P. Factors associated with wasting among children under five years old in South Asia: Implications for action. PLoS ONE 2018, 13, e0198749. [Google Scholar] [CrossRef]
- Ramalingaswami, V.; Jonsson, U.; Rohde, J. Commentary: The Asian Enigma. Available online: https://www.unicef.org/pon96/nuenigma.htm (accessed on 28 December 2020).
- Headey, D.; Hoddinott, J.; Ali, D.; Tesfaye, R.; Dereje, M. The Other Asian Enigma: Explaining the Rapid Reduction of Undernutrition in Bangladesh. World Dev. 2015, 66, 749–761. [Google Scholar] [CrossRef]
- Akhmat, G.; Zaman, K.; Shukui, T.; Javed, Y.; Khan, S.R. Social Health Indicators and Economic Growth: Evidence from East Asia and Pacific, Middle East and North Africa, South Asia, and Sub-Saharan Africa. Soc. Indic. Res. 2013, 119, 663–686. [Google Scholar] [CrossRef]
- World Bank. South Asia Economic Focus Spring 2016: Fading Tailwinds; World Bank: Washington, DC, USA, 2016. [Google Scholar]
- WHO. WHO Global Nutrition Targets 2025; Stunting Policy Brief (WHO/NMH/NHD/14.3); World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- The Lancet. Maternal and Child Nutrition: Executive Summary of the Lancet Maternal and Child Nutrition Series; Elsevier: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Dewey, K.G.; Begum, K. Long-term consequences of stunting in early life. Matern. Child Nutr. 2011, 7, 5–18. [Google Scholar] [CrossRef] [PubMed]
- Corsi, D.J.; Neuman, M.; Finlay, J.E.; Subramanian, S.V. Demographic and health surveys: A profile. Int. J. Epidemiol. 2012, 41, 1602–1613. [Google Scholar] [CrossRef] [PubMed]
- Measure DHS. The Demographic and Health Survey Program. Available online: https://dhsprogram.com/publications/index.cfm (accessed on 27 February 2020).
- WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development; World Health Organization: Geneva, Switzerland, 2006; 312p. [Google Scholar]
- WHO. Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Padiatr. 2006, 450, 76–85. [Google Scholar] [CrossRef]
- Titaley, C.R.; Dibley, M.J.; Agho, K.; Roberts, C.L.; Hall, J. Determinants of neonatal mortality in Indonesia. BMC Public Heath 2008, 8, 232. [Google Scholar] [CrossRef]
- Wali, N.; Agho, K.E.; Renzaho, A.M. Factors associated with stunting among children under 5 years in five South Asian countries (2014–2018): Analysis of demographic health surveys. Nutrients 2020, 12, 3875. [Google Scholar] [CrossRef]
- Li, Z.; Kim, R.; Vollmer, S.; Subramanian, S.V. Factors associated with child stunting, wasting, and underweight in 35 low- and middle-income countries. JAMA Netw. Open 2020, 3, e203386. [Google Scholar] [CrossRef]
- WHO. Indicators for Assessing Infant and Young Child Feeding Practices: Conclusions of a Consensus Meeting Held 6–8 November 2007; WHO: Washington, DC, USA, 2007. [Google Scholar]
- United Nations. Population. Available online: https://www.un.org/en/sections/issues-depth/population/index.html (accessed on 4 January 2021).
- United Nations Population Fund. Maldives Population Projections 2014–2054. Available online: http://statisticsmaldives.gov.mv/nbs/wp-content/uploads/2018/07/Maldives-Population-Projections-2014-2054.pdf (accessed on 4 January 2021).
- Daniel, A.I.; Bandsma, R.H.; Lytvyn, L.; Voskuijl, W.P.; Potani, I.; Heuvel, M.V.D. Psychosocial stimulation interventions for children with severe acute malnutrition: A systematic review. J. Glob. Heath 2017, 7, 010405. [Google Scholar]
- Wrottesley, S.V.; Lamper, C.; Pisa, P.T. Review of the importance of nutrition during the first 1000 days: Maternal nutritional status and its associations with fetal growth and birth, neonatal and infant outcomes among African women. J. Dev. Orig. Heath Dis. 2016, 7, 144–162. [Google Scholar] [CrossRef]
- King, J.C. A Summary of Pathways or Mechanisms Linking Preconception Maternal Nutrition with Birth Outcomes. J. Nutr. 2016, 146, 1437S–1444S. [Google Scholar] [CrossRef]
- UNICEF. Nutrition: Because Every Child Deserves Healthy and Nutrition Food. Available online: https://www.unicef.org/maldives/what-we-do/nutrition (accessed on 1 November 2020).
- Mutunga, M.; Frison, S.; Rava, M.; Bahwere, P. The Forgotten Agenda of Wasting in Southeast Asia: Burden, Determinants and Overlap with Stunting: A Review of Nationally Representative Cross-Sectional Demographic and Health Surveys in Six Countries. Nutrients 2020, 12, 559. [Google Scholar] [CrossRef]
- UNICEF. Water, Sanitation and Hygiene (WASH). Available online: https://www.unicef.org/rosa/water-sanitation-and-hygiene-wash (accessed on 5 January 2021).
- Khatun, W.; Rasheed, S.; Alam, A.; Huda, T.M.; Dibley, M.J. Assessing the Intergenerational Linkage between Short Maternal Stature and Under-Five Stunting and Wasting in Bangladesh. Nutrients 2019, 11, 1818. [Google Scholar] [CrossRef]
- Subramanian, S.V. Association of maternal height with child mortality, anthropometric failure, and anemia in India. JAMA 2009, 301, 1691–1701. [Google Scholar] [CrossRef]
- Özaltin, E. Association of maternal stature with offspring mortality, underweight, and stunting in low- to middle-income countries. JAMA 2010, 303, 1507–1516. [Google Scholar] [CrossRef]
- Woldeamanuel, B.T.; Tesfaye, T.T. Risk Factors Associated with under-Five Stunting, Wasting, and Underweight Based on Ethiopian Demographic Health Survey Datasets in Tigray Region, Ethiopia. J. Nutr. Metab. 2019, 2019, 6967170. [Google Scholar] [CrossRef]
- Wemakor, A.; Garti, H.; Azongo, T.; Garti, H.; Atosona, A. Young maternal age is a risk factor for child undernutrition in Tamale Metropolis, Ghana. BMC Res. Notes 2018, 11, 877. [Google Scholar] [CrossRef]
- Nguyen, P.H.; Sanghvi, T.; Tran, L.M.; Afsana, K.; Mahmud, Z.; Aktar, B.; Haque, R.; Menon, P. The nutrition and health risks faced by pregnant adolescents: Insights from a cross-sectional study in Bangladesh. PLoS ONE 2017, 12, e0178878. [Google Scholar] [CrossRef] [PubMed]
- Workicho, A.; Belachew, T.; Argaw, A.; Roba, A.; Ghosh, S.; Kershaw, M.; Lachat, C.; Kolsteren, P. Maternal nutritional status mediates the association between maternal age and birth outcomes. Matern. Child Nutr. 2020, 16, e13015. [Google Scholar] [CrossRef] [PubMed]
- Rutstein, S. Effects of preceding birth intervals on neonatal, infant and under-five years mortality and nutritional status in developing countries: Evidence from the demographic and health surveys. Int. J. Gynecol. Obstet. 2005, 89, S7–S24. [Google Scholar] [CrossRef]
- Roy, M.P.; Mohan, U.; Singh, S.K.; Singh, V.K.; Srivastava, A.K. Determinants of Utilization of Antenatal Care Services in Rural Lucknow, India. J. Fam. Med. Prim. Care 2013, 2, 55–59. [Google Scholar] [CrossRef] [PubMed]
- Efendi, F.; Chen, C.-M.; Kurniati, A.; Berliana, S.M. Determinants of utilization of antenatal care services among adolescent girls and young women in Indonesia. Women Heath 2016, 57, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; Huang, Z.J.; Yang, S.; Pan, J.; Smith, B.; Xu, B. The utilization of antenatal care among rural-to-urban migrant women in Shanghai: A hospital-based cross-sectional study. BMC Public Heath 2012, 12, 1012. [Google Scholar] [CrossRef]
- Hamel, C.; Enne, J.; Omer, K.; Ayara, N.; Yarima, Y.; Cockcroft, A.; Andersson, N. Childhood malnutrition is associated with maternal care during pregnancy and childbirth: A cross-sectional study in Bauchi and cross River States, Nigeria. J. Public Heath Res. 2015, 4, 408. [Google Scholar] [CrossRef] [PubMed]
- Kim, R.; Mejía-Guevara, I.; Corsi, D.J.; Aguayo, V.M.; Subramanian, S. Relative importance of 13 correlates of child stunting in South Asia: Insights from nationally representative data from Afghanistan, Bangladesh, India, Nepal, and Pakistan. Soc. Sci. Med. 2017, 187, 144–154. [Google Scholar] [CrossRef]
- Kavosi, E.; Rostami, Z.H.; Nasihatkon, A.; Moghadami, M.; Heidari, M. Prevalence and determinants of under-nutrition among children under six: A cross-sectional survey in fars province, Iran. Int. J. Heath Policy Manag. 2014, 3, 71–76. [Google Scholar] [CrossRef]
- Sarmento, D.R. Traditional Birth Attendance (TBA) in a health system: What are the roles, benefits and challenges: A case study of incorporated TBA in Timor-Leste. Asia Pac. Fam. Med. 2014, 13, 12. [Google Scholar] [CrossRef]
- Oona, M.R.C.; Wendy, J.G.; Carine, R.; Jo, B. Maternal Survival 2: Strategies for reducing maternal mortality: Getting on with what works. Lancet 2006, 368, 1284. [Google Scholar]
- Khamis, A.G.; Mwanri, A.W.; Ntwenya, J.E.; Kreppel, K. The influence of dietary diversity on the nutritional status of children between 6 and 23 months of age in Tanzania. BMC Pediatr. 2019, 19, 1–9. [Google Scholar] [CrossRef]
| N | % | N * | % * | |
|---|---|---|---|---|
| IMMEDIATE FACTORS | ||||
| Dietary diversity score | ||||
| <4 food inadequate | 502,720 | 89.1 | 261,538 | 90.8 |
| 4+ food adequate | 61,799 | 11.0 | 26,662 | 9.3 |
| Initiation of breastfeeding ^^ | ||||
| More than 1 h | 98,960 | 55.6 | 54,004 | 57.8 |
| Within 1 h | 78,999 | 44.4 | 39,360 | 42.2 |
| Currently breastfeeding ^^ | ||||
| Yes | 152,577 | 85.7 | 82,092 | 87.9 |
| No | 25,382 | 14.3 | 11,272 | 12.1 |
| Duration of breastfeeding ^^ | ||||
| Up to 12 months | 104,612 | 60.3 | 54,918 | 60.6 |
| >12 months | 68,841 | 39.7 | 35,758 | 39.4 |
| Had diahrrea recently | ||||
| No | 497,294 | 91.6 | 248,960 | 90.7 |
| Yes | 45,449 | 8.4 | 25,432 | 9.3 |
| Had fever in last two weeks | ||||
| No | 489,556 | 87.0 | 246,288 | 85.8 |
| Yes | 73,202 | 13.0 | 40,904 | 14.2 |
| Vitamin A supplement | ||||
| Yes | 330,858 | 61.5 | 146,375 | 54.0 |
| No | 207,088 | 38.5 | 124,667 | 46.0 |
| Vaccination | ||||
| No | ||||
| Yes ** | ||||
| Child’s age in months | ||||
| 0 to 5 | 46,475 | 8.2 | 26,459 | 9.2 |
| 6 to 11 | 57,785 | 10.2 | 29,444 | 10.2 |
| 12 to 17 | 57,219 | 10.1 | 29,097 | 10.1 |
| 18 to 23 | 56,863 | 10.1 | 28,191 | 9.8 |
| 24 to 29 | 59,833 | 10.6 | 28,712 | 10.0 |
| 30 to 35 | 54,883 | 9.7 | 28,490 | 9.9 |
| 36 to 41 | 61,009 | 10.8 | 30,288 | 10.5 |
| 42 to 47 | 56,638 | 10.0 | 29,601 | 10.3 |
| 48 to 53 | 58,309 | 10.3 | 28,799 | 10.0 |
| 54 to 59 | 55,503 | 9.8 | 29,119 | 10.1 |
| Sex of child | ||||
| Male | 298,109 | 52.8 | 149,820 | 52.0 |
| Female | 266,409 | 47.2 | 138,380 | 48.0 |
| UNDERLYING FACTORS | ||||
| Mother’s characteristics | ||||
| Mother’s age | ||||
| 15–24 | 203,772 | 36.1 | 94,191 | 32.7 |
| 25–34 | 315,204 | 55.8 | 163,376 | 56.7 |
| 35–49 | 45,543 | 8.1 | 30,633 | 10.6 |
| Maternal age at child’s birth | ||||
| less than 20 | 85,396 | 15.1 | 36,792 | 12.8 |
| 20–29 | 404,288 | 71.6 | 202,997 | 70.4 |
| 30–39 | 71,155 | 12.6 | 44,975 | 15.6 |
| 40+ | 3679 | 0.7 | 3436 | 1.2 |
| Maternal height | ||||
| ≥160 cm | 39,546 | 7.4 | 21,122 | 7.7 |
| 155–159 | 104,417 | 19.6 | 54,914 | 20.0 |
| 150–154 | 179,901 | 33.8 | 93,376 | 34.0 |
| 145–149 | 141,057 | 26.5 | 73,505 | 26.8 |
| <145 cm | 68,079 | 12.8 | 31,462 | 11.5 |
| Maternal BMI (kg/m2) | ||||
| 25+ | 89,949 | 16.9 | 48,632 | 17.8 |
| 18.5–25 | 341,610 | 64.2 | 184,644 | 67.4 |
| ≤18.5 | 100,822 | 18.9 | 40,768 | 14.9 |
| Birth order | ||||
| 1 | 234,944 | 41.6 | 105,439 | 36.6 |
| 2–4 | 298,296 | 52.8 | 157,198 | 54.5 |
| ≥5 | 31,278 | 5.5 | 25,563 | 8.9 |
| Birth interval (preceding) | ||||
| no previous birth | 236,359 | 41.9 | 106,197 | 36.9 |
| <24 months | 87,271 | 15.5 | 47,999 | 16.7 |
| >24 months | 240,798 | 42.7 | 133,924 | 46.5 |
| Combined birth rank and birth interval | ||||
| 1st birth rank | 234,944 | 41.6 | 105,439 | 36.6 |
| 2nd/3rd birth rank, more than 2 years | 209,159 | 37.1 | 110,447 | 38.3 |
| 2nd/3rd birth rank, less than or equal to 2 | 89,137 | 15.8 | 46,751 | 16.2 |
| 4th birth rank, more than 2 yrs interval | 21,728 | 3.8 | 18,033 | 6.3 |
| 4th birth rank, less than or equal to 2 | 9550 | 1.7 | 7530 | 2.6 |
| Mother’s marital status | ||||
| Currently married | 557,795 | 98.9 | 283,875 | 98.6 |
| Formerly married $ | 6246 | 1.1 | 3934 | 1.4 |
| Working status | ||||
| Not working | 539,465 | 95.6 | 273,808 | 95.0 |
| Working | 25,053 | 4.4 | 14,389 | 5.0 |
| Mother’s education | ||||
| No education | 132,099 | 23.4 | 90,502 | 31.4 |
| Primary | 81,114 | 14.4 | 43,428 | 15.1 |
| Secondary or higher | 351,305 | 62.2 | 154,270 | 53.5 |
| Paternal occupation | ||||
| Non-agriculture | 96,051 | 17.0 | 50,218 | 17.4 |
| Agriculture | 30,003 | 5.3 | 19,651 | 6.8 |
| Not working | 438,244 | 77.7 | 218,182 | 75.7 |
| Power over earnings (Woman has money autonomy) | ||||
| By husband alone | 494,969 | 87.7 | 248,523 | 86.2 |
| Woman alone or joint decision | 69,549 | 12.3 | 39,677 | 13.8 |
| Power over household decision making | ||||
| By husband alone | 464,605 | 82.3 | 233,624 | 81.1 |
| Woman alone or joint decision | 99,913 | 17.7 | 54,576 | 18.9 |
| Woman has health care autonomy | ||||
| By husband alone | 477,134 | 84.5 | 240,663 | 83.5 |
| Woman alone or joint decision | 87,384 | 15.5 | 47,537 | 16.5 |
| Household | ||||
| Pooled household wealth index | ||||
| Poorest | 78,060 | 13.8 | 57,642 | 20.0 |
| Poorer | 83,593 | 14.8 | 57,641 | 20.0 |
| Middle | 99,919 | 17.7 | 57,637 | 20.0 |
| Richer | 140,627 | 24.9 | 57,641 | 20.0 |
| Richest | 162,320 | 28.8 | 57,639 | 20.0 |
| Source of drinking water | ||||
| Not improved | 58,376 | 10.3 | 42,551 | 14.8 |
| Improved | 506,142 | 89.7 | 245,649 | 85.2 |
| Type of toilet facility | ||||
| Improved | 319,836 | 56.7 | 142,679 | 49.5 |
| Unimproved | 244,603 | 43.3 | 145,453 | 50.5 |
| Access to services | ||||
| Healthcare utilisation factors | ||||
| Place of delivery | ||||
| Home | 101,719 | 18.2 | 73,821 | 25.9 |
| Health Facility | 457,175 | 81.8 | 211,213 | 74.1 |
| Mode of delivery | ||||
| Non-caesarean | 421,582 | 75.5 | 244,091 | 85.7 |
| Caesarean section | 136,657 | 24.5 | 40,674 | 14.3 |
| Combined mode and place of delivery | ||||
| Home | 101,179 | 18.1 | 73,645 | 25.9 |
| Vaginal birth | 320,398 | 57.4 | 170,442 | 59.9 |
| Caesarean and Health Facility | 136,656 | 24.5 | 40,672 | 14.3 |
| Delivery Assistance | ||||
| Health professional | 404,219 | 72.7 | 185,946 | 65.8 |
| Traditional birth attendant | 48,560 | 8.7 | 34,565 | 12.2 |
| Other untrained & | 103,133 | 18.6 | 62,303 | 22.0 |
| Antenatal clinic visits | ||||
| ≥ 8 | 87,381 | 16.3 | 24,789 | 8.9 |
| 4 to 7 | 139,816 | 26.1 | 66,440 | 23.8 |
| 1 to 3 | 110,784 | 20.6 | 71,963 | 25.7 |
| None | 198,638 | 37.0 | 116,360 | 41.6 |
| Media | ||||
| Reads newspaper | ||||
| Not all | 357,336 | 63.3 | 201,210 | 69.8 |
| Yes ++ | 207,160 | 36.7 | 86,966 | 30.2 |
| Listening to radio | ||||
| Not all | 481,048 | 85.2 | 244,719 | 84.9 |
| Yes ++ | 83,471 | 14.8 | 43,481 | 15.1 |
| Watches television | ||||
| Not all | 136,315 | 24.2 | 95,183 | 33.0 |
| Yes ++ | 428,203 | 75.9 | 193,017 | 67.0 |
| BASIC FACTORS | ||||
| Countries | ||||
| Bangladesh | 14,853 | 2.6 | 7886 | 2.7 |
| India | 519,243 | 92.0 | 259,627 | 90.1 |
| Maldives | 4708 | 0.8 | 3085 | 1.1 |
| Nepal | 6739 | 1.2 | 4994 | 1.7 |
| Pakistan | 18,975 | 3.4 | 12,608 | 4.4 |
| Type of place of residence | ||||
| Urban | 251,655 | 44.6 | 72,552 | 25.2 |
| Rural | 312,863 | 55.4 | 215,648 | 74.8 |
| Variables | 0–23 Months | |||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95%CI | p-Value | AOR | 95%CI | p-Value | |||
| Countries | ||||||||
| Maldives | 1.00 | 1.00 | ||||||
| India | 4.20 | 2.22 | 7.97 | <0.001 | 3.63 | 1.92 | 6.87 | <0.001 |
| Bangladesh | 2.15 | 0.83 | 5.54 | 0.113 | 1.97 | 0.76 | 5.12 | 0.162 |
| Nepal | 2.00 | 0.99 | 4.04 | 0.053 | 1.70 | 0.85 | 3.39 | 0.131 |
| Pakistan | 1.20 | 0.58 | 2.48 | 0.632 | 1.03 | 0.50 | 2.13 | 0.928 |
| Maternal height | ||||||||
| ≥160 cm | 1.00 | 1.00 | ||||||
| 155–159 | 1.31 | 0.93 | 1.86 | 0.124 | 1.29 | 0.92 | 1.80 | 0.141 |
| 150–154 | 1.36 | 1.01 | 1.83 | 0.040 | 1.35 | 0.99 | 1.86 | 0.061 |
| 145–149 | 1.40 | 1.06 | 1.85 | 0.020 | 1.38 | 1.04 | 1.84 | 0.025 |
| <145 cm | 1.32 | 0.89 | 1.95 | 0.161 | 1.33 | 0.93 | 1.91 | 0.118 |
| Maternal BMI (kg/m2) | ||||||||
| 25+ | 1.00 | 1.00 | ||||||
| 18.5–25 | 1.35 | 1.11 | 1.64 | 0.003 | 1.19 | 0.96 | 1.48 | 0.120 |
| ≤18.5 | 2.25 | 1.76 | 2.88 | <0.001 | 2.02 | 1.52 | 2.68 | <0.001 |
| Combined birth rank and birth interval | ||||||||
| 1st birth rank | 1.00 | 1.00 | ||||||
| 2nd/3rd birth rank, more than 2 years | 0.84 | 0.66 | 1.07 | 0.152 | 0.82 | 0.67 | 1.02 | 0.074 |
| 2nd/3rd birth rank, less than or equal 2 | 1.07 | 0.84 | 1.37 | 0.565 | 1.00 | 0.81 | 1.26 | 0.933 |
| 4th birth rank, more than 2 yrs interval | 1.38 | 1.06 | 1.79 | 0.015 | 1.31 | 1.04 | 1.65 | 0.021 |
| 4th birth rank, less than or equal to 2 | 0.99 | 0.75 | 1.31 | 0.936 | 0.99 | 0.77 | 1.27 | 0.948 |
| Combined mode and place of delivery | ||||||||
| Caesarean and Health Facility | 1.00 | 1.00 | ||||||
| Vaginal and Health Facility | 1.50 | 1.17 | 1.94 | 0.002 | 1.36 | 1.04 | 1.76 | 0.023 |
| Home | 1.36 | 1.07 | 1.72 | 0.011 | 1.29 | 1.01 | 1.64 | 0.042 |
| Child age in months | ||||||||
| 0 to 5 months | 1.00 | 1.00 | ||||||
| 6 to 11 months | 0.67 | 0.52 | 0.86 | 0.002 | 0.64 | 0.51 | 0.82 | <0.001 |
| 12 to 17 months | 0.54 | 0.40 | 0.74 | <0.001 | 0.51 | 0.39 | 0.69 | <0.001 |
| 18–23 months | 0.47 | 0.34 | 0.65 | <0.001 | 0.45 | 0.33 | 0.61 | <0.001 |
| Pooled Household wealth index | ||||||||
| Poorest | 1.00 | 1.00 | ||||||
| Poorer | 0.73 | 0.64 | 0.83 | <0.001 | 0.78 | 0.68 | 0.89 | <0.001 |
| Middle | 0.72 | 0.62 | 0.83 | <0.001 | 0.80 | 0.69 | 0.93 | 0.003 |
| Richer | 0.76 | 0.60 | 0.96 | 0.022 | 0.91 | 0.73 | 1.13 | 0.397 |
| Richest | 0.72 | 0.52 | 0.98 | 0.037 | 0.98 | 0.70 | 1.38 | 0.909 |
| Variables | 24–59 Months | |||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95%CI | p-Value | AOR | 95%CI | p-Value | |||
| Countries | ||||||||
| Maldives | 1.00 | 1.00 | ||||||
| India | 1.99 | 1.29 | 3.08 | 0.002 | 1.83 | 1.06 | 3.16 | 0.029 |
| Bangladesh | 1.19 | 0.75 | 1.88 | 0.461 | 1.15 | 0.66 | 2.02 | 0.615 |
| Nepal | 0.59 | 0.36 | 0.97 | 0.037 | 0.53 | 0.29 | 0.96 | 0.036 |
| Pakistan | 0.33 | 0.19 | 0.58 | <0.001 | 0.36 | 0.20 | 0.67 | 0.001 |
| Mother’s age | ||||||||
| 15–24 | 1.00 | 1.00 | ||||||
| 25–34 | 1.14 | 0.95 | 1.36 | 0.170 | 1.24 | 1.02 | 1.51 | 0.034 |
| 35–49 | 1.32 | 0.91 | 1.92 | 0.145 | 1.49 | 1.01 | 2.20 | 0.044 |
| Maternal BMI (kg/m2) | ||||||||
| 25+ | 1.00 | 1.00 | ||||||
| 18.5–25 | 1.68 | 1.15 | 2.45 | 0.007 | 1.82 | 1.29 | 2.55 | 0.001 |
| ≤18.5 | 2.39 | 1.60 | 3.55 | <0.001 | 2.54 | 1.83 | 3.54 | <0.001 |
| Antenatal clinic visits | ||||||||
| ≥8 | 1.00 | 1.00 | ||||||
| 4 to 7 | 0.85 | 0.59 | 1.22 | 0.376 | 0.83 | 0.59 | 1.18 | 0.305 |
| 1 to 3 | 0.78 | 0.53 | 1.14 | 0.194 | 0.72 | 0.50 | 1.04 | 0.077 |
| None | 0.73 | 0.52 | 1.03 | 0.073 | 0.68 | 0.49 | 0.94 | 0.021 |
| Watches television | ||||||||
| Not all | 1.00 | 1.00 | ||||||
| Yes | 1.05 | 0.90 | 1.22 | 0.561 | 1.25 | 1.06 | 1.46 | 0.006 |
| Pooled household wealth index | ||||||||
| Poorest | 1.00 | 1.00 | ||||||
| Poorer | 1.03 | 0.90 | 1.17 | 0.692 | 1.03 | 0.90 | 1.18 | 0.629 |
| Middle | 0.98 | 0.83 | 1.15 | 0.791 | 0.93 | 0.77 | 1.13 | 0.472 |
| Richer | 0.76 | 0.64 | 0.89 | 0.001 | 0.72 | 0.61 | 0.86 | <0.001 |
| Richest | 0.88 | 0.68 | 1.15 | 0.366 | 0.89 | 0.71 | 1.12 | 0.328 |
| Variables | 0–59 Months | |||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95%CI | p-Value | AOR | 95%CI | p-Value | |||
| Countries | ||||||||
| Maldives | 1.00 | 1.00 | ||||||
| India | 2.66 | 1.77 | 4.01 | <0.001 | 2.10 | 1.34 | 3.27 | 0.001 |
| Bangladesh | 1.51 | 0.92 | 2.48 | 0.101 | 1.42 | 0.85 | 2.37 | 0.177 |
| Nepal | 1.04 | 0.66 | 1.65 | 0.851 | 0.82 | 0.50 | 1.34 | 0.438 |
| Pakistan | 0.61 | 0.38 | 0.99 | 0.043 | 0.57 | 0.35 | 0.93 | 0.024 |
| Maternal height | ||||||||
| ≥160 cm | 1.00 | 1.00 | ||||||
| 155–159 | 1.32 | 1.03 | 1.70 | 0.030 | 1.32 | 1.01 | 1.71 | 0.039 |
| 150–154 | 1.28 | 1.03 | 1.58 | 0.024 | 1.24 | 0.99 | 1.56 | 0.062 |
| 145–149 | 1.31 | 1.04 | 1.64 | 0.019 | 1.25 | 0.98 | 1.59 | 0.071 |
| <145 cm | 1.11 | 0.79 | 1.57 | 0.538 | 1.14 | 0.85 | 1.51 | 0.386 |
| Maternal BMI (kg/m2) | ||||||||
| 25+ | 1.00 | 1.00 | ||||||
| 18.5–25 | 1.59 | 1.25 | 2.03 | <0.001 | 1.47 | 1.18 | 1.83 | 0.001 |
| ≤18.5 | 2.47 | 1.88 | 3.23 | <0.001 | 2.18 | 1.72 | 2.77 | <0.001 |
| Antenatal clinic visits | ||||||||
| ≥8 | 1.00 | 1.00 | ||||||
| 4 to 7 | 0.88 | 0.70 | 1.09 | 0.242 | 0.85 | 0.68 | 1.07 | 0.174 |
| 1 to 3 | 0.93 | 0.72 | 1.20 | 0.588 | 0.83 | 0.64 | 1.08 | 0.167 |
| None | 0.73 | 0.59 | 0.91 | 0.005 | 0.76 | 0.60 | 0.95 | 0.015 |
| Combined mode and place of delivery | ||||||||
| Caesarean and Health Facility | 1.00 | 1.00 | ||||||
| Vaginal and Health Facility | 1.41 | 1.14 | 1.74 | 0.002 | 1.29 | 1.07 | 1.55 | 0.008 |
| Home | 1.25 | 0.99 | 1.58 | 0.059 | 1.15 | 0.96 | 1.39 | 0.126 |
| Dietary diversity score | ||||||||
| <4 food inadequate | 1.00 | 1.00 | ||||||
| 4+ food adequate | 0.86 | 0.68 | 1.09 | 0.218 | 0.73 | 0.58 | 0.91 | 0.004 |
| Child age in months | ||||||||
| 0–23 months | 1.00 | 1.00 | ||||||
| 24–59 months | 0.66 | 0.58 | 0.75 | <0.001 | 0.68 | 0.59 | 0.78 | <0.001 |
| Pooled Household wealth index | ||||||||
| Poorest | 1.00 | 1.00 | ||||||
| Poorer | 0.89 | 0.82 | 0.96 | 0.004 | 0.90 | 0.83 | 0.98 | 0.019 |
| Middle | 0.86 | 0.76 | 0.97 | 0.011 | 0.89 | 0.78 | 1.03 | 0.112 |
| Richer | 0.76 | 0.66 | 0.88 | <0.001 | 0.82 | 0.70 | 0.95 | 0.010 |
| Richest | 0.80 | 0.65 | 0.98 | 0.034 | 0.97 | 0.79 | 1.20 | 0.792 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wali, N.; Agho, K.E.; Renzaho, A.M.N. Wasting and Associated Factors among Children under 5 Years in Five South Asian Countries (2014–2018): Analysis of Demographic Health Surveys. Int. J. Environ. Res. Public Health 2021, 18, 4578. https://doi.org/10.3390/ijerph18094578
Wali N, Agho KE, Renzaho AMN. Wasting and Associated Factors among Children under 5 Years in Five South Asian Countries (2014–2018): Analysis of Demographic Health Surveys. International Journal of Environmental Research and Public Health. 2021; 18(9):4578. https://doi.org/10.3390/ijerph18094578
Chicago/Turabian StyleWali, Nidhi, Kingsley E. Agho, and Andre M. N. Renzaho. 2021. "Wasting and Associated Factors among Children under 5 Years in Five South Asian Countries (2014–2018): Analysis of Demographic Health Surveys" International Journal of Environmental Research and Public Health 18, no. 9: 4578. https://doi.org/10.3390/ijerph18094578
APA StyleWali, N., Agho, K. E., & Renzaho, A. M. N. (2021). Wasting and Associated Factors among Children under 5 Years in Five South Asian Countries (2014–2018): Analysis of Demographic Health Surveys. International Journal of Environmental Research and Public Health, 18(9), 4578. https://doi.org/10.3390/ijerph18094578







