The Effectiveness of Massage Therapy for Improving Sequelae in Post-Stroke Survivors. A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Data Items
2.4. Search
2.5. Risk of Bias in Individual Studies
2.6. Synthesis of Results
3. Results
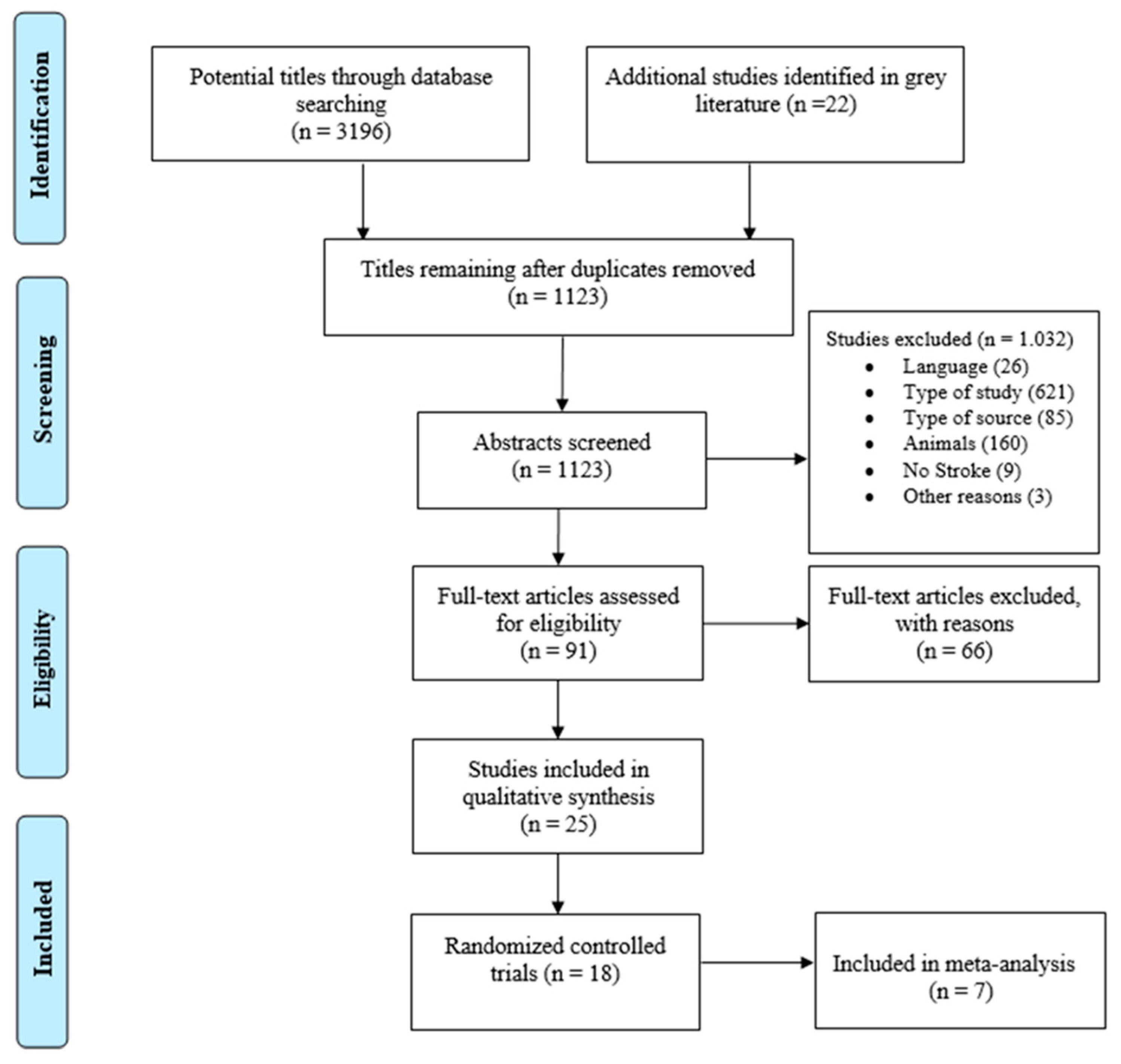
3.1. Study Selection
3.2. Risk of Bias within Studies
3.3. Study Characteristics
3.4. Efficacy of Therapeutic Massage
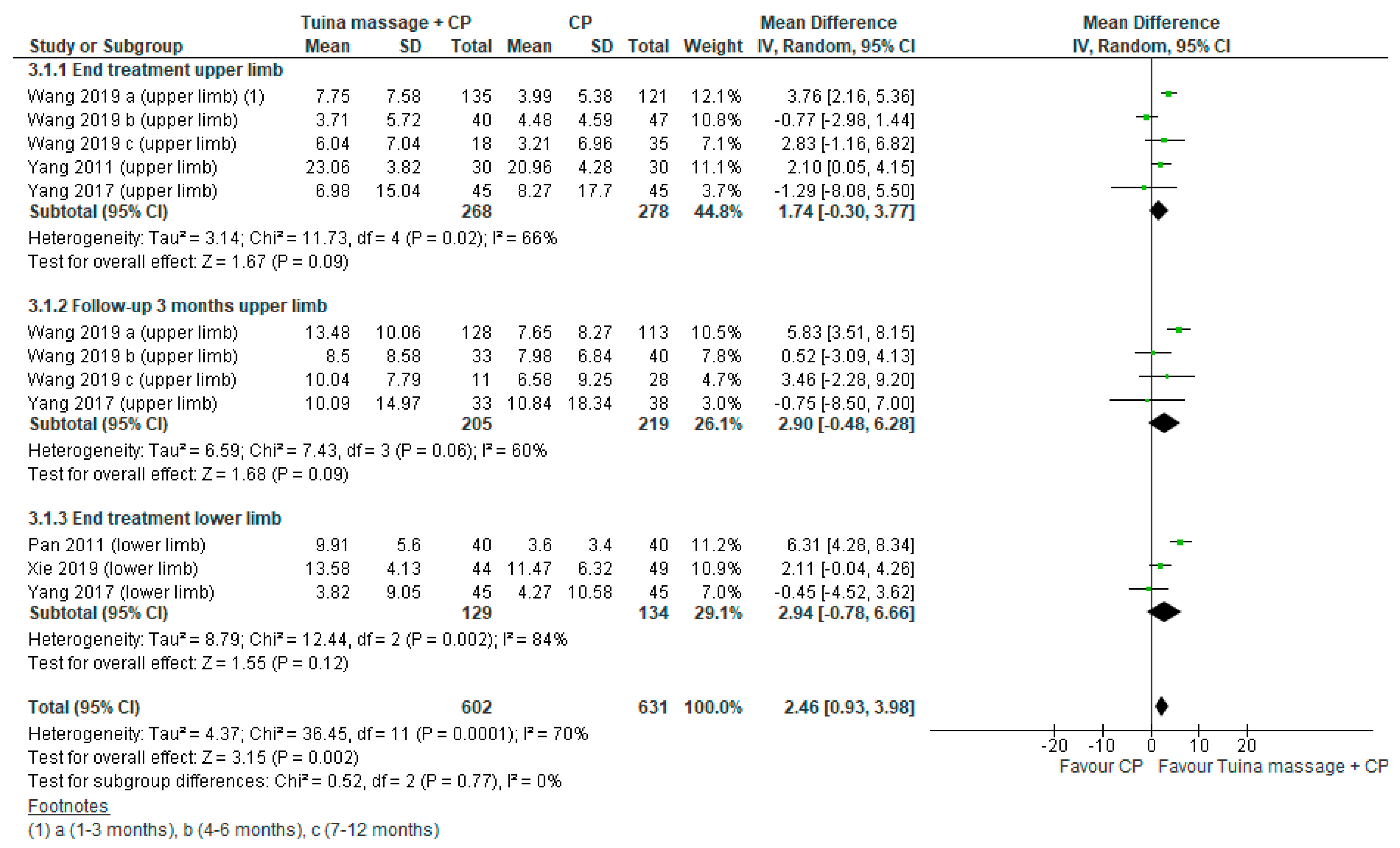
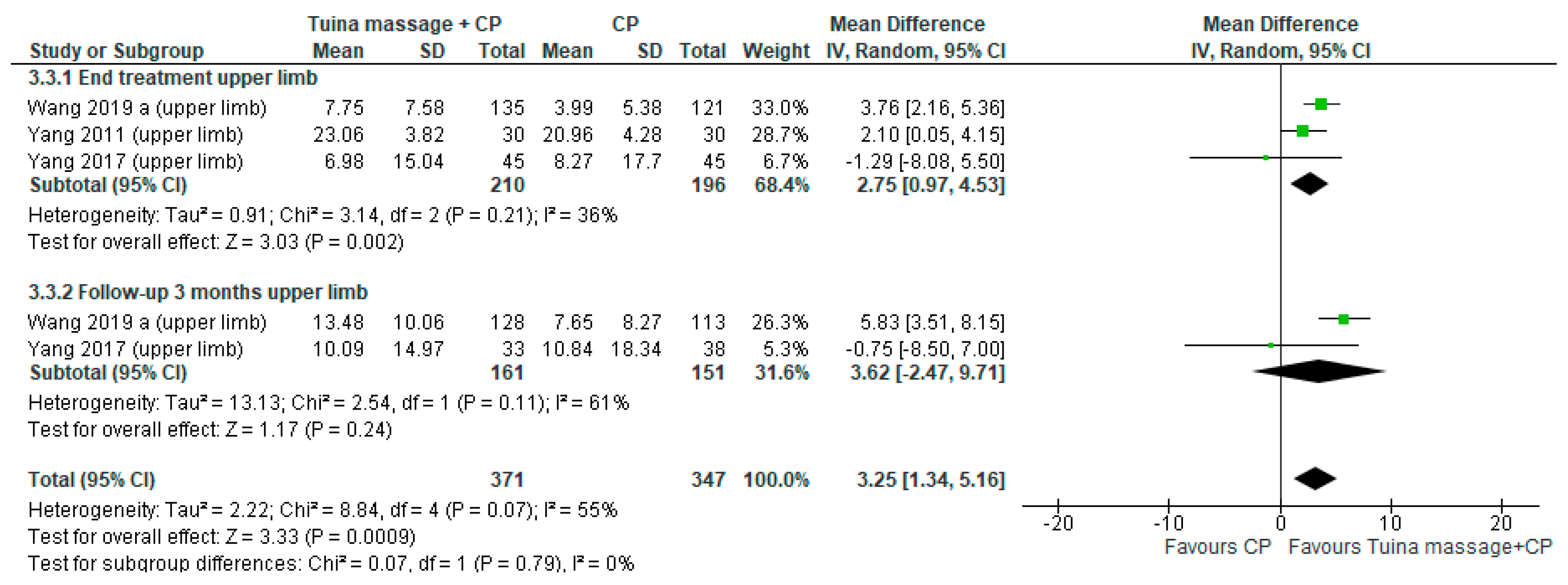
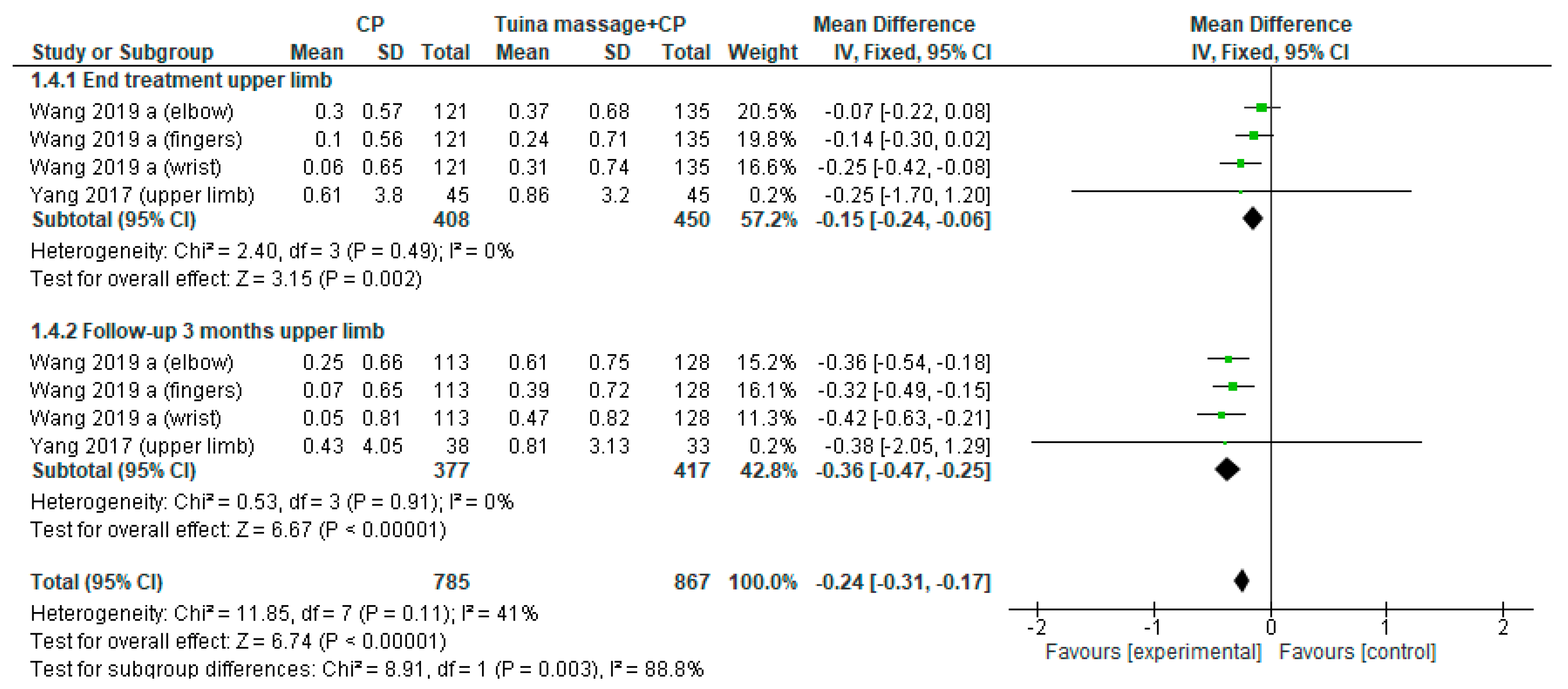
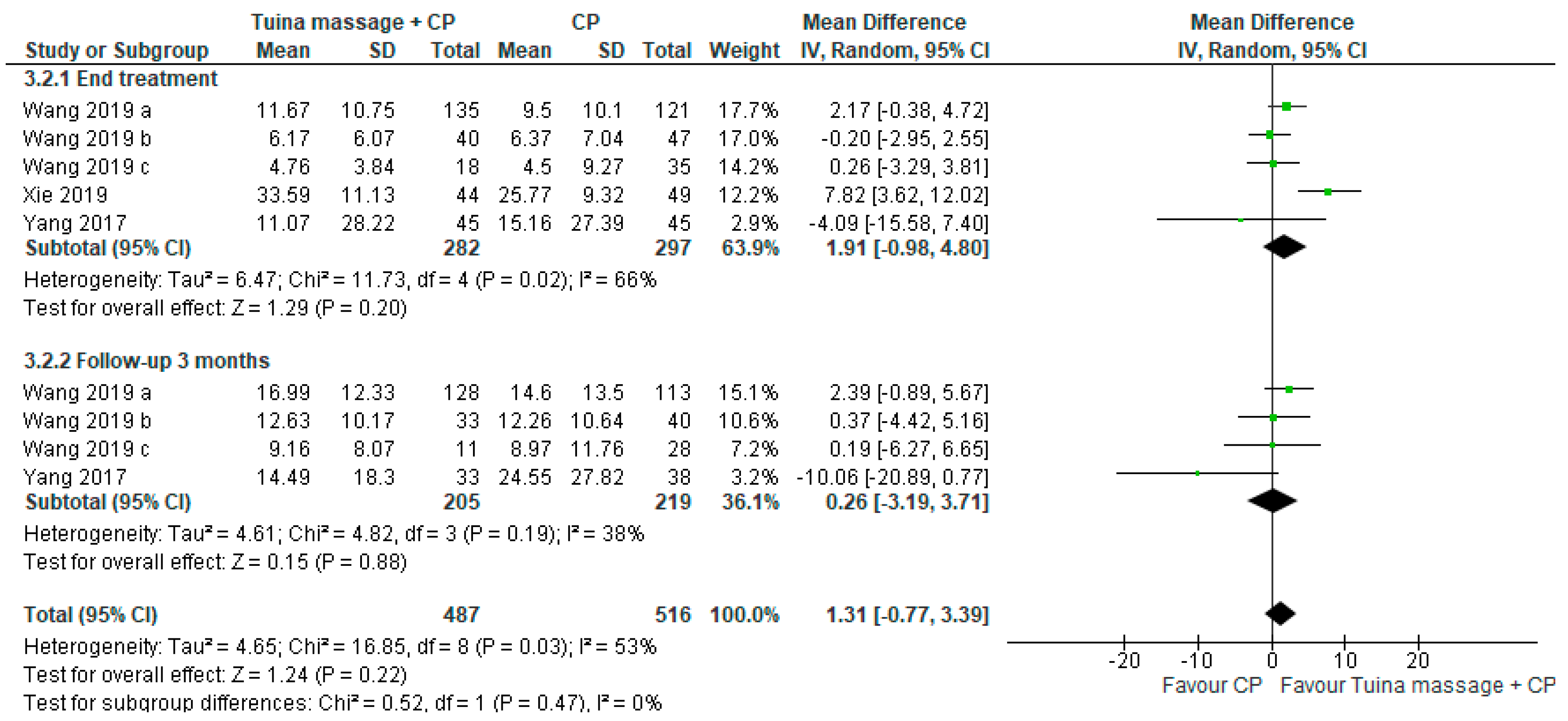
3.5. Upper/Lower Limbs Motor Function
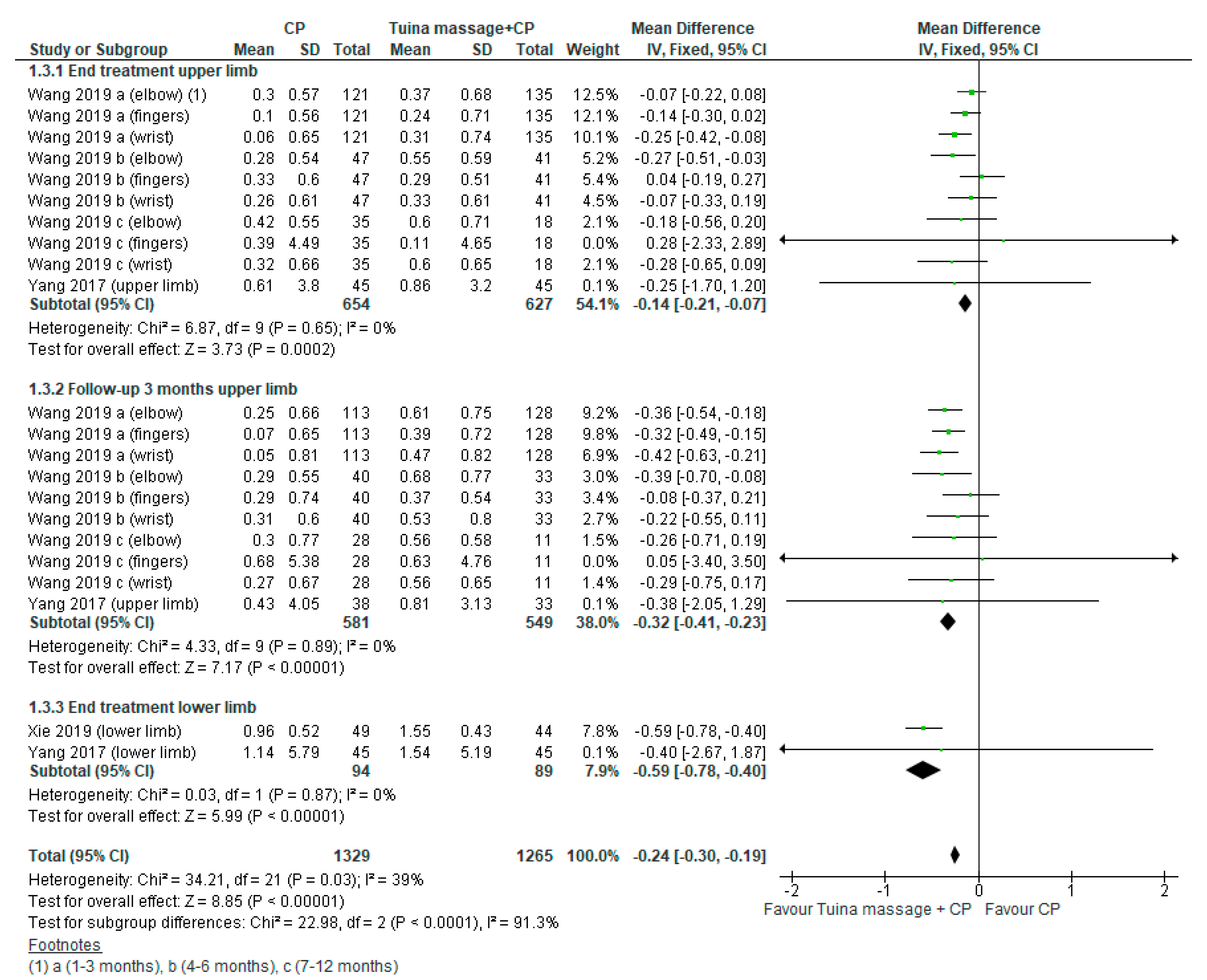
3.6. Spasticity
3.7. Activities of Daily Living
3.8. Anxiety and Stress
3.9. Pain
3.10. Gait and Balance
3.11. Adverse Events
3.12. Risk of Bias Publication
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADL | Activities of daily living |
| AG | Acupuncture group |
| CENTRAL | Cochrane Central Register of Controlled Trials |
| CG | Control group |
| CI | Confidence interval |
| EG | Experimental group |
| MD | Mean difference |
| MG | Massage group |
| NDT | Neuro-Developmental Treatment |
| NIHSS | National Institutes of Health Stroke Scale |
| PEDro | Physiotherapy Evidence Database |
| RCT | Randomized controlled clinical trials |
| ROM | Range of motion |
Appendix A
- Search strategy PubMed/Medline: Total 958
- “stroke”[MeSH Terms] OR “stroke”[All Fields] OR “strokes”[All Fields] OR “stroke s”[All Fields] OR (“paresis”[MeSH Terms] OR “paresis”[All Fields] OR “hemiparesis”[All Fields]) OR (“hemiplegia”[MeSH Terms] OR “hemiplegia”[All Fields] OR “hemiplegias”[All Fields]) OR (“cerebrovascular disorders”[MeSH Terms] OR (“cerebrovascular”[All Fields] AND “disorders”[All Fields]) OR “cerebrovascular disorders”[All Fields] OR (“cerebrovascular”[All Fields] AND “disorder”[All Fields]) OR “cerebrovascular disorder”[All Fields]) OR (“infarctation”[All Fields] OR “infarcted”[All Fields] OR “infarctic”[All Fields] OR “infarcting”[All Fields] OR “infarction”[MeSH Terms] OR “infarction”[All Fields] OR “infarct”[All Fields] OR “infarctions”[All Fields] OR “infarcts”[All Fields] OR “infarctive”[All Fields]) OR (“brain injuries”[MeSH Terms] OR (“brain”[All Fields] AND “injuries”[All Fields]) OR “brain injuries”[All Fields] OR (“brain”[All Fields] AND “injury”[All Fields]) OR “brain injury”[All Fields]) AND “massage”[MeSH Terms] OR “massage”[All Fields] OR “massages”[All Fields] OR “massaged”[All Fields] OR “massager”[All Fields] OR “massagers”[All Fields] OR “massaging”[All Fields] OR” therapeutic massage” OR “musculoskeletal manipulation”[All Fields] OR “massage therapy”[All Fields] OR “tuina”[All Fields] OR “dalk”[All Fields] OR “Tui Na”[All Fields]OR soft manipulation)): 959
- Tripdatabase; stroke AND massage: 643 articlesPEDro; stroke AND massage OR Tui Na: 268 articlesCochrane library; stroke AND massage: 243Web and Science; stroke AND massage: 228Scopus; stroke AND massage: 413Web of science; stroke AND massage: 235CINHAL; stroke or cerebrovascular accident or cva) AND massage therapy: 207SCIELO; stroke AND massage: 2Epistemonikos; stroke AND massage: 39
- Total: 3195
References
- Donkor, E.S. Stroke in the21stCentury: A Snapshot of the Burden, Epidemiology, and Quality of Life. Stroke Res. Treat. 2018, 2018, 3238165. [Google Scholar] [CrossRef]
- Francisco, G.E.; McGuire, J.R. Poststroke Spasticity Management. Stroke 2012, 43, 3132–3136. [Google Scholar] [CrossRef] [PubMed]
- Veerbeek, J.M.; Van Wegen, E.; Van Peppen, R.; Van Der Wees, P.J.; Hendriks, E.; Rietberg, M.; Kwakkel, G. What Is the Evidence for Physical Therapy Poststroke? A Systematic Review and Meta-Analysis. PLoS ONE 2014, 9, e87987. [Google Scholar] [CrossRef]
- Pettman, E. A History of Manipulative Therapy. J. Man. Manip. Ther. 2007, 15, 165–174. [Google Scholar] [CrossRef]
- Eubanks, J.E.; Chang Chien, G.C.; Atchison, J.W. Manipulation, Mobilization, Massage and Traction in Pain Manage-ment. In Pain; Springer International Publishing: New York, NY, USA, 2019; pp. 1047–1049. [Google Scholar]
- Gasibat, Q.; Suwehli, W. Determining the Benefits of Massage Mechanisms: A Review of Literature. Artic. J. Rehabil. Sci. 2017, 2, 58–67. [Google Scholar] [CrossRef]
- Mustafa, K.; Furmanek, M.; Knapik, P.A.; Bacik, B.; Juras, G. The Impact of the Swedish Massage on the Kinesthetic Differentiation in Healthy Individuals. Int. J. Ther. Massage Bodyw. 2015, 8, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Barreto, D.M.; Batista, M.V.A. Swedish Massage: A Systematic Review of its Physical and Psychological Benefits. Adv. Mind Body Med. 2017, 31, 16–20. [Google Scholar]
- Pritchard, S. Tui na: A Manual of Chinese Massage Therapy, 2nd ed.; Singing Dragon: London, UK, 2015. [Google Scholar]
- Fazil, M. A Review on Dalk (Massage) with Special Reference to the Prescribed Medications. Trad Integr. Med. Mar. 2017, 2, 39–52. [Google Scholar]
- Buttagat, V.; Eungpinichpong, W.; Chatchawan, U.; Kharmwan, S. The immediate effects of traditional Thai massage on heart rate variability and stress-related parameters in patients with back pain associated with myofascial trigger points. J. Bodyw. Mov. Ther. 2011, 15, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Field, T. Massage therapy research review. Complement. Ther. Clin. Pract. 2016, 24, 19–31. [Google Scholar] [CrossRef]
- Cassileth, B.R.; Vickers, A.J. Massage therapy for symptom control: Outcome study at a major cancer center. J. Pain Symptom Manag. 2004, 28, 244–249. [Google Scholar] [CrossRef]
- Kennedy, A.B.; Trilk, J.L. A standardized, evidence-based massage therapy program for decentralized elite paracyclists: Creating the model. Int. J. Ther. Massage Bodywork: Res. Educ. Pract. 2015, 8, 3–9. [Google Scholar] [CrossRef]
- Angelopoulou, E.; Anagnostouli, M.; Chrousos, G.P.; Bougea, A. Massage therapy as a complementary treatment for Parkinson’s disease: A Systematic Literature Review. Complement. Ther. Med. 2020, 49, 102340. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Wang, Y.; Wang, Z. The effectiveness of massage and touch on behavioral and psychological symptoms of dementia: A quantitative systematic review and meta-analysis. J. Adv. Nurs. 2017, 73, 2283–2295. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.-S.; Liu, Y.; Zou, X.-N.; Ma, Y.-L.; Liu, G.-L. Evaluating the Efficacy of Massage Intervention for the Treatment of Poststroke Constipation: A Meta-Analysis. Evid. Based Complement. Altern. Med. 2020, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.T.J. Cochrane Handbook for Systematic Reviews of Interventions. 2019. Available online: https://training.cochrane.org/handbook/current (accessed on 28 March 2019).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Kennedy, A.B.; Cambron, J.A.; Sharpe, P.A.; Travillian, R.S.; Saunders, R.P. Process for massage therapy practice and essential assessment. J. Bodyw. Mov. Ther. 2016, 20, 484–496. [Google Scholar] [CrossRef]
- Alvarez, G.; Cerritelli, F.; Urrutia, G. Using the template for intervention description and replication (TIDieR) as a tool for improving the design and reporting of manual therapy interventions. Man. Ther. 2016, 24, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef]
- Murie-Fernández, M.; Irimia, P.; Martínez-Vila, E.; Meyer, M.J.; Teasell, R. Neuro-rehabilitation after stroke. Neurología 2010, 25, 189–196. [Google Scholar] [CrossRef]
- Review Manager (RevMan) [Computer Program]; Version 5.3; The Nordic Cochrane Centre, The Cochrane Collaboration: Copenhagen, Denmark, 2014.
- Turner, R.M.; Bird, S.M.; Higgins, J.P.T. The Impact of Study Size on Meta-analyses: Examination of Underpowered Studies in Cochrane Reviews. PLoS ONE 2013, 8, e59202. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- DerSimonian, R.; Kacker, R. Random-effects model for meta-analysis of clinical trials: An update. Contemp. Clin. Trials 2007, 28, 105–114. [Google Scholar] [CrossRef]
- Mok, E.; Woo, C.P. The effects of slow-stroke back massage on anxiety and shoulder pain in elderly stroke patients. Complement. Ther. Nurs. Midwifery 2004, 10, 209–216. [Google Scholar] [CrossRef]
- Jin-Su, W. Effect of acupuncture and Tuina on stroke. J. Acupunct. Tuina Sci. 2005, 3, 31–32. [Google Scholar] [CrossRef]
- Thanakiatpinyo, T.; Suwannatrai, S.; Suwannatrai, U.; Khumkaew, P.; Wiwattamongkol, D.; Vannabhum, M.; Pianmanakit, S.; Kuptniratsaikul, V. The efficacy of traditional Thai massage in decreasing spasticity in elderly stroke patients. Clin. Interv. Aging 2014, 9, 1311–1319. [Google Scholar] [CrossRef]
- Han, S.-K.; Ma, Z.-W.; Zhang, N.; Chen, C.-P.; Ren, Z.-C. Tuina along the meridians combined with Chinese medicine for motor functions and activities of daily living in patients with post-stroke upper limb spasticity. J. Acupunct. Tuina Sci. 2015, 13, 295–299. [Google Scholar] [CrossRef]
- Ahmed, A.; Nasir Ansari, A.; Javed Ali, S.; Yasir, M. Efficacy of Munzij Wa Mushil-E-Balgham (Poly Herbal Formulations) and Massage With Roghan-E-Malkangani in Falij Nisfi (Hemiplegia): A Randomised Controlled Clinical Trial. Int. J. Pharm. Sci. Res. 2015, 6, 453. [Google Scholar] [CrossRef]
- Di, H.-Y.; Han, S.-K.; Du, X.-L.; Li, W.-W.; Jia, J. Applying tuina to exterior-interiorly connected meridians for post-stroke upper limb spasticity. J. Acupunct. Tuina Sci. 2017, 15, 27–30. [Google Scholar] [CrossRef]
- Lee, J.H.; Seo, E.K.; Shim, J.S.; Chung, S.P. The effects of aroma massage and foot bath on psychophysiological response in stroke patients. J. Phys. Ther. Sci. 2017, 29, 1292–1296. [Google Scholar] [CrossRef]
- Yang, Y.-J.; Zhang, J.; Hou, Y.; Jiang, B.-Y.; Pan, H.-F.; Wang, J.; Zhong, D.-Y.; Guo, H.-Y.; Zhu, Y.; Cheng, J. Effectiveness and safety of Chinese massage therapy (Tui Na) on post-stroke spasticity: A prospective multicenter randomized controlled trial. Clin. Rehabil. 2017, 31, 904–912. [Google Scholar] [CrossRef]
- Wang, M.; Liu, S.; Peng, Z.; Zhu, Y.; Feng, X.; Gu, Y.; Sun, J.; Tang, Q.; Chen, H.; Huang, X.; et al. Effect of Tui Na on upper limb spasticity after stroke: A randomized clinical trial. Ann. Clin. Transl. Neurol. 2019, 6, 778–787. [Google Scholar] [CrossRef]
- Xie, C. Clinical observation of tuina plus rehabilitation therapy for lower limb extensor spasticity in recovery stage of stroke. J. Acupunct. Tuina Sci. 2019, 17, 44–48. [Google Scholar] [CrossRef]
- Amanullah, H.; Mohd, A.; Nasir, A.A.; Ghulamuddin, S.; Hussain, S.A. Efficacy of massage with rogan seer in motor recovery in hemiplegia secondary to ischaemic stroke. Indian J. Tradit. Knowl. 2011, 10, 731–735. [Google Scholar]
- Pan, H.P.; Feng, H.; Li, Y.J. Effects of Unblocking Meridians and Du-channel Massage Combined with Rehabilitation Training on the Motor Function Improvement of Cerebral Ischemic Stroke Patients. Second Clin. Med. Coll. Nanjing Tradit. Chin. Med. 2011, 31, 1474. [Google Scholar]
- Yang, L.; Xuemei, G.; Xianhu, L.; Hao, W. Curative effect observation of massage therapy and control training of scapula on shoulder-hand syndrome in hemiplegic patients. Mod. J. Integr. Tradit. Chinese West. Med. 2011, 19, 19. [Google Scholar]
- Rahaman, A. Role of dalak (massage) and riyazat (exercise) in the rehabilitation of patients with post stroke hemiplegia. Indian J. Tradit. Knowl. 2012, 11, 738–744. [Google Scholar]
- Li, N.; Tian, F.; Wang, C.; Yu, P.; Zhou, X.; Wen, Q.; Qiao, X.; Huang, L. Therapeutic effect of acupuncture and massage for shoulder-hand syndrome in hemiplegia patients: A clinical two-center randomized controlled trial. J. Tradit. Chin. Med. 2012, 32, 343–349. [Google Scholar] [CrossRef]
- Wu, J.; Cui, X.; Wang, J.; Shi, J.-C.; Ye, W.-C. Effect of combining tuina with balance training on balance functions of stroke patients. J. Acupunct. Tuina Sci. 2013, 11, 160–164. [Google Scholar] [CrossRef]
- Zhang, X.L.; Qi, R.; Yan, J.T. Clinical research on post-stroke hemiplegia treated with the optimized rehabilitation program of integrated Chinese and Western Medicine. Chin. Acupunct. Moxibustion 2013, 33, 1113–1117. [Google Scholar]
- Zhang, Y.; Jin, H.; Ma, D.; Fu, Y.; Xie, Y.; Li, Z.; Zou, Y. Efficacy of Integrated Rehabilitation Techniques of Traditional Chinese Medicine for Ischemic Stroke: A Randomized Controlled Trial. Am. J. Chin. Med. 2013, 41, 971–981. [Google Scholar] [CrossRef]
- Sullivan, K.J.; Tilson, J.K.; Cen, S.Y.; Rose, D.K.; Hershberg, J.; Correa, A.; Gallichio, J.; McLeod, M.; Moore, C.; Wu, S.S.; et al. Fugl-Meyer Assessment of Sensorimotor Function After Stroke: Standardized training procedure for clinical practice and clinical trials. Stroke 2011, 42, 427–432. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Smith, M.B. Interrater Reliability of a Modified Ashworth Scale of Muscle Spasticity. Phys. Ther. 1987, 67, 206–207. [Google Scholar] [CrossRef]
- Pollock, A.; George, B.S.; Fenton, M.; Firkins, L. Top 10 research priorities relating to life after stroke—Consensus from stroke survivors, caregivers, and health professionals. Int. J. Stroke 2014, 9, 313–320. [Google Scholar] [CrossRef]
- Gholami-Motlagh, F.; Jouzi, M.; Soleymani, B. Comparing the effects of two Swedish massage techniques on the vital signs and anxiety of healthy women. Iran. J. Nurs. Midwifery Res. 2016, 21, 402–409. [Google Scholar] [CrossRef] [PubMed]
- Backus, D.; Manella, C.; Bender, A.; Sweatman, M. Impact of massage therapy on fatigue, pain, and spasticity in people with multiple sclerosis: A pilot study. Int. J. Ther. Massage Bodywork Res. Educ. Pract. 2016, 9, 4–13. [Google Scholar] [CrossRef]
- Negahban, H.; Rezaie, S.; Goharpey, S. Massage therapy and exercise therapy in patients with multiple sclerosis: A randomized controlled pilot study. Clin. Rehabil. 2013, 27, 1126–1136. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Reif, M.; Field, T.; Largie, S.; Diego, M.; Manigat, N.; Seoanes, J.; Bornstein, J. Cerebral palsy symptoms in children decreased following massage therapy. Early Child Dev. Care 2005, 175, 445–456. [Google Scholar] [CrossRef]
- Mahmood, Q.; Habibullah, S.; Babur, M.N. Potential effects of traditional massage on spasticity and gross motor function in children with spastic cerebral palsy: A randomized controlled trial. Pak. J. Med Sci. 2019, 35, 1210–1215. [Google Scholar] [CrossRef]
- Wissel, J.; Verrier, M.; Simpson, D.M.; Charles, D.; Guinto, P.; Papapetropoulos, S.; Sunnerhagen, K.S. Post-stroke Spasticity: Predictors of Early Development and Considerations for Therapeutic Intervention. PM&R 2014, 7, 60–67. [Google Scholar] [CrossRef]
- Gracies, J.-M. Pathophysiology of spastic paresis. I: Paresis and soft tissue changes. Muscle Nerve 2005, 31, 535–551. [Google Scholar] [CrossRef]
- Ryu, J.S.; Lee, J.W.; Lee, S.I.; Chun, M.H. Factors Predictive of spasticity and their effects on motor recovery and functional outcomes in stroke patients. Top. Stroke Rehabil. 2010, 17, 380–388. [Google Scholar] [CrossRef]
- Li, S. Spasticity, motor recovery, and neural plasticity after stroke. Front. Neurol. 2017, 8, 120. [Google Scholar] [CrossRef]
- Urban, P.P.; Wolf, T.; Uebele, M.; Marx, J.J.; Vogt, T.; Stoeter, P.; Bauermann, T.; Weibrich, C.; Vucurevic, G.D.; Schneider, A.; et al. Occurence and clinical predictors of spasticity after ischemic stroke. Stroke 2010, 41, 2016–2020. [Google Scholar] [CrossRef]
- Pundik, S.; Falchook, A.D.; McCabe, J.; Litinas, K.; Daly, J.J. Functional brain correlates of upper limb spasticity and its mitigation following rehabilitation in chronic stroke survivors. Stroke Res. Treat. 2014, 2014, 1–8. [Google Scholar] [CrossRef]
- Li, L.; Tong, K.Y.; Hu, X. The Effect of poststroke impairments on brachialis muscle architecture as measured by ultrasound. Arch. Phys. Med. Rehabil. 2007, 88, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Gao, F.; Grant, T.H.; Roth, E.J.; Zhang, L.-Q. Changes in passive mechanical properties of the gastrocnemius muscle at the muscle fascicle and joint levels in stroke survivors. Arch. Phys. Med. Rehabil. 2009, 90, 819–826. [Google Scholar] [CrossRef] [PubMed]
- Leng, Y.; Wang, Z.; Bian, R.; Lo, W.L.A.; Xie, X.; Wang, R.; Huang, D.; Li, L. Alterations of Elastic Property of Spastic Muscle With Its Joint Resistance Evaluated From Shear Wave Elastography and Biomechanical Model. Front. Neurol. 2019, 10, 736. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Chen, Y.-T.; Francisco, G.E.; Zhou, P.; Rymer, W.Z. A unifying pathophysiological account for post-stroke spasticity and disordered motor control. Front. Neurol. 2019, 10, 468. [Google Scholar] [CrossRef]
- Baker, S.N. The primate reticulospinal tract, hand function and functional recovery. J. Physiol. 2011, 589, 5603–5612. [Google Scholar] [CrossRef]
- Zeng, H.; Butterfield, T.A.; Agarwal, S.; Haq, F.; Best, T.M.; Zhao, Y. An engineering approach for quantitative analysis of the lengthwise strokes in massage therapies. J. Med. Devices Trans. ASME 2008, 2, 041003. [Google Scholar] [CrossRef]
- Miake-Lye, I.M.; Mak, S.; Lee, J.; Luger, T.; Taylor, S.L.; Shanman, R.; Beroes-Severin, J.M.; Shekelle, P.G. Massage for pain: An evidence map. J. Altern. Complement. Med. 2019, 25, 475–502. [Google Scholar] [CrossRef] [PubMed]
- Mescher, A.L.; Neff, A.W.; King, M.W. Inflammation and immunity in organ regeneration. Dev. Comp. Immunol. 2017, 66, 98–110. [Google Scholar] [CrossRef] [PubMed]
- Uvnäs-Moberg, K.; Handlin, L.; Petersson, M. Self-soothing behaviors with particular reference to oxytocin release induced by non-noxious sensory stimulation. Front. Psychol. 2015, 5, 1529. [Google Scholar] [CrossRef]
- Alimohammad, H.S.; Ghasemi, Z.; Shahriar, S.S.; Morteza, S.; Arsalan, K. Effect of hand and foot surface stroke massage on anxiety and vital signs in patients with acute coronary syndrome: A randomized clinical trial. Complement. Ther. Clin. Pract. 2018, 31, 126–131. [Google Scholar] [CrossRef]
- Biering-Sørensen, F.; Nielsen, J.B.; Klinge, K. Spasticity-assessment: A review. Spinal Cord 2006, 44, 708–722. [Google Scholar] [CrossRef] [PubMed]
- Lindgren, L.; Westling, G.; Brulin, C.; Lehtipalo, S.; Andersson, M.; Nyberg, L. Pleasant human touch is represented in pregenual anterior cingulate cortex. NeuroImage 2012, 59, 3427–3432. [Google Scholar] [CrossRef]
- Lamp, G.; Goodin, P.; Palmer, S.; Low, E.; Barutchu, A.; Carey, L.M. Activation of bilateral secondary somatosensory cortex with right hand touch stimulation: A meta-analysis of functional neuroimaging studies. Front. Neurol. 2019, 9, 1129. [Google Scholar] [CrossRef] [PubMed]
- Goats, G.C. Massage—The scientific basis of an ancient art: Part 1. The techniques. Br. J. Sports Med. 1994, 28, 149–152. [Google Scholar] [CrossRef]
- Guo, T.; Zhu, B.; Zhang, X.; Xu, N.; Wang, H.; Tai, X. Tuina for children with cerebral palsy. Medicine 2018, 97, e9697. [Google Scholar] [CrossRef]
- Zheng, Q.; Tang, B. Differentiation of Yin–Yang and Prescriptions for Some Common Diseases. In Handbook of Traditional Chinese Medicine; World Scientific Publishing Co.: Singapore, 2014; pp. 869–922. [Google Scholar]
- Fang, L.; Fang, M. Research progress on the standardization of Chinese Tuina therapy: A short review. Chin. J. Integr. Med. 2013, 19, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Tong, X.; Liu, D.-D.; Wei, Y.; Kou, J.-Y.; Yang, T.-S.; Qiao, L.-D. Effect observation on point-through-point needling combined with tuina for post-stroke shoulder-hand syndrome. J. Acupunct. Tuina Sci. 2012, 10, 104–108. [Google Scholar] [CrossRef]
- Ernst, E. The safety of massage therapy. Rheumatology 2003, 42, 1101–1106. [Google Scholar] [CrossRef] [PubMed]
- Na, K.; He, J.E.; Hu, L.; Wu, L.; Li, Y.; Zhao, D.Y.; Li, R.Z.; Fan, W.J. Early treatment of acute ischemic stroke by integrated traditional and Western medicine. Int. J. Clin. Exp. Med. 2018, 11, 2901. [Google Scholar]
- Geri, T.; Viceconti, A.; Minacci, M.; Testa, M.; Rossettini, G. Manual therapy: Exploiting the role of human touch. Musculoskelet. Sci. Pract. 2019, 44, 102044. [Google Scholar] [CrossRef]

| Author, Year, Country | Groups (n) | Age (Years) Mean (SD) | Gender (Male/ Female) | Stroke Type (Ischemic/ Hemorrhagic) | Time Since Stroke Mean (SD) | Affected Side (Right/Left/ Bilateral) | Stroke Severity Mean (SD) |
|---|---|---|---|---|---|---|---|
| Mok, 2004 [28] China | EG:51 CG:51 | EG:73.3 ± 6.63 CG:73.1 ± 6.64 | 51/51 | NR | NR | NR | NR |
| Jin-su, 2005, [29] China | EG:52 CG:40 | Ranged from 32 to 86 y Mean age 62.7 | 61/31 | NR | From 2 h. to 24 d. | NR | MESSS scale: EG: mild (10), moderate (25), severe (17) CG: mild (8), moderate (23), severe (11) |
| Amanullah, 2011 [38] India | EG:20 CG:20 | EG:55.57 ± 11.56 CG:54.30 ± 11.99 | 36/4 | 100% ischemic | Stroke onset between 4 w. to 5 y | 13/ 27 | NR |
| Pan, 2011 [39] China | EG:40 CG:40 | 53.65 ± 7.82 | EG:28/12 CG:25/11 | 100% ischemic | EG:41.1 ± 12.9 d. CG:42.9 ± 13.2 d. | EG:24/16 CG:22/18 | EG:55.31 ± 7.54 CG:54.68 ± 8.21 |
| Yang, 2011 [40] China | EG:30 CG:30 | EG:58.15 ± 10.26 CG:57.98 ± 10.91 | EG:20/11 CG:19/11 | EG:14/16 CG:17/13 | EG:35.95 ± 10.02 d CG:36.21 ± 9.59 d | EG:17/13 CG:18/12 | NR |
| Zarnigar, 2012 [41] India | EGa:20 EGb:20 CG:20 | Ranged from 50 to 59 19 patients | 50/20 | NR | NR | NR | NR |
| Li, 2012 [42] China | EG:60 CG:60 | EG:62 ± 12 CG:61 ± 13 | EG:40/20 CG:41/19 | 100% ischemic | EG:28 ± 6 d CG:27 ± 5 d | EG:28/32 CG:24/36 | NR |
| Wu, 2013 [43] China | EG:60 CG:60 | EG:60.1 ± 10 CG:62.7 ± 11.3 | EG:33/27 CG:32/28 | EG:22/38 CG:24/36 | NR | NR | NR |
| Zhang X, [44] 2013 China | MG:30 AG:30 | MG:63.7 ± 7 AG:64 ± 7 | MG:22/8 AG:20/10 | NR | MG:52 ± 13 d AG:52 ± 15 d | NR | NR |
| Zhang Y, [45] 2013 China | EG:46 CG:23 | EG:65.74 ± 10.28 CG:66.95 ± 10.95 | EG:33/9 CG:13/6 | 100% ischemic | EG:38.00 ± 40.04 h CG:31.79 ± 37.38 h | NR | NIHSS scale EG:8.36 ± 3.03 CG:7.68 ± 2.38 |
| Thanakiatpinyo, 2014 [30] Thailand | EG:24 CG:26 | EG:60.0 ± 6.9 CG:65.8 ± 8.1 | EG:22/2 CG:15/11 | EG:12/12 CG:15/12 | onset ≥ 3 m | NR | NR |
| Han, 2015 [31] China | EG:110 CG:110 | EG:51.2 ± 2.1 CG:52.8 ± 1.7 | EG: 56/54 CG: 58/52 | EG:69/41 CG:72/38 | EG:13.3 ± 5.2 d CG:13.9 ± 4.7 d | NR | NR |
| Ahmed, 2015 [32] India | EG:20 CG:20 | From 18–70 y | NR | 100% ischemic | From 4 w to 5 y | NR | NR |
| Di, 2017 [33] China | EG:75 CG:75 | EG:61.4 ± 5.2 CG:61.7 ± 5.3 | EG:48/27 CG:46/29 | EG:42/33 CG:39/36 | ≤3 m | NR | NR |
| Lee, 2017 [34] Korea | EG:7 CG:7 | EG: 64.3 ± 2.2 CG: 65.0 ± 5.0 | EG:4/3 CG:4/3 | EG:3/4 CG:3/4 | EG:13.0 ± 3.1 m CG:13.6 ± 1.4 m | NR | NR |
| Yang, 2017 [35] China | EG:45 CG:45 | EG:59.93 ± 16.87 CG:62.73 ± 11.22 | EG:34/11 CG:27/18 | NR | EG:3.0 ± 5.0 m CG:3.0 ± 7.0 m | EG:21/26 CG:24/19 | NR |
| Wang, 2019 [36] China | EG:193 CG:204 | a:EG:55.57 ± 11.56 CG:54.30 ± 11.99 b:EG:57.80 ± 11.34 CG:51.43 ± 13.07 c:EG:52.90 ± 12.89 GC:57.17 ± 10.97 | a:EG: 99/44 CG: 93/34 b:EG: 35/13 GC: 40/13 c:EG: 20/6 CG:29/12 | a:EG:96/47 CG:85/42 b:EG:32/16 CG:35/18 c:EG:17/9 CG:27/14 | a:CG:1.69 ± 0.77 CG:1.70 ± 0.76 b:EG:4.84 ± 0.83 CG:4.77 ± 0.78 c:EG: 9.24 ± 1.43 CG:9.42 ± 1.53 | a:EG:61/62/20 CG:55/54/18 b:EG:20/21/7 CG:22/23/8 c:EG:12/11/3 CG:17/17/7 | NR |
| Xie,2019 [37] China | EG:44 CG:49 | EG:51.6 ± 4.9 CG:52.48 ± 5.4 | EG:27/17 CG:29/20 | EG:24/20 CG:26/23 | EG:43.9 ± 20.4 d CG:44.3 ± 21.4 d | GE:19/25 CG:22/27 | NR |
| Author, Year | Evaluation | Groups | Results | ||
|---|---|---|---|---|---|
| Outcome | Tool | Period | |||
| Mok, 2004 | Pain perception shoulder Anxiety level Blood pressure Heart rate Patients’massage perceptions | VAS Stai Dinamap Monitor Questionnaire | T0: Before treatment T1: After treatment T2: 3 days Follow-up | EG: Slow-stroke back massage CG:CP | Pain, anxiety, blood pressure, heart rate Better EG after treatment and follow-up |
| Jin-su, 2005 | Stroke disability | MESSS scale | T0: Before treatment T1: After treatment | EG: Tuina massage + acupuncture CG: Western medicine (drugs) | Neurologic impairment degree Better EG |
| Amanullah, 2011 | Motor function upper/lower limb | STREAM | T0: Before treatment T1:15th day T2: 0th day T3: After treatment | EG: Dalk massage with Roghan Seer CG: Sham Dalk massage with petroleum jelly | Voluntary movement lower limb and basic mobility Better EG after treatment Voluntary movement of upper limb * |
| Pan, 2011 | Motor function lower limb Gait Gait analysis | FMA-L 10-MWT Motion Analysis | T0: Before treatment T1: After treatment | EG: Tuina massage + CP CG:CP | FMA-L Better EG 10 MWT Better EG Gait analysis Better EG |
| Yang, 2011 | Motor function upper limb Pain shoulder-hand Edema | FMA-U VAS 4-point Likert scale | T0: Before treatment T1: After treatment | EG: Tuina massage + CP CG:CP | FMA-U, VAS and edema Better EG after treatment |
| Zarnigar, 2012 | Motor function upper limb Stroke disability Gait | FMA-U FIM 10-MWT | T0: Before treatment T1: After treatment | EGa: Dalk Massage EGb: Exercises CG: Unani medicine drugs | FMA-U Better EGa after treatment FMI Better EGb 10 MWT Better EGb |
| Li, 2012 | Motor function upper limb/ hand Pain shoulder-hand Stage of shoulder-hand syndrome Stroke disability | FMA-U FMA-H NPRS Steinbrocker classification mRS | T0: Before treatment T1: After treatment T2: 3 months Follow-up | EG: Tuina massage + electrical acupuncture CG:NDT + PNF + scapular mobilizations | NPRS scores shoulder passive movement 90°, Stage of shoulder-hand syndrome and mRS Better EG after treatment and follow-up FMA-U Better EG after treatment FMA-H * |
| Wu, 2013 | Balance | FM-B | T0: Before treatment T1: After treatment | EG: Tuina massage + balance training CG: Balance training | FM-B Better after treatment EG |
| Zhang X, 2013 | Motor function upper limb ADL Stroke disability Quality of life | FMA-U BI mRS SS-QOL | T0: Before treatment T1: After treatment | EG: Tuina massage + CP CG: Acupuncture + CP | FMA-U, BI, mRS and SS-QOL * |
| Zhang Y, 2013 | Motor function upper/lower limb Stroke severity ADL Stroke disability | FMA-U FMA-L NIHSS BI mRS | T0: Before treatment T1: After treatment T2: 3 months Follow-up | EG: Tuina massage + acupuncture CG: CP | FMA lower limb and NIHSS Better EG after treatment and follow-up FMA upper limb * BI * mRS * |
| Thanakiatpinyo, 2014 | Spasticity elbow and knee ADL Anxiety and Depression QoL | MAS BI HADS Pictorial Thai QoL test | T0: Before treatment T1: After treatment | EG: Thai massage CG:CP | Trends in decreasing spasticity, anxiety, and depression scores but no difference between groups ADL * QoL * |
| Han, 2015 | Motor function upper limb Spasticity upper limb ADL | FMA-U MAS mBI | T0: Before treatment T1: After treatment | EG: Tuina massage + medicinal herbs (oral) CG:CP | MAS, mBI and FMA-U Better EG |
| Ahmed, 2015 | Motor function upper/lower limb | STREAM | T0: Before treatment T1: After treatment | EG: Dalk massage with Roghan Malkangani + Unani medicine drugs CG: Western medicine (drugs) | Voluntary movement upper/lower limb and basic mobility Better EG |
| Di, 2017 | Spasticity upper limb Stroke severity | MAS NIHSS | T0: Before treatment T1: After treatment | EG: Tuina massage CG:CP | MAS and NIHSS Better EG |
| Lee, 2017 | Anxiety Mood state Sleep satisfaction Body temperature | 4-point Likert scale MAACL VAS Infrared thermography | T0: Before treatment T1: After treatment | EG: Swedish massage + foot bath + CP CG:CP | 4-point Likert scale, MAACL, VAS Infrared thermography Better EG after treatment |
| Yang, 2017 | Motor function upper limb Spasticity upper limb ADL | FMA-U MAS mBI | T0: Before treatment T1: After treatment T2:Follow-up 3 months | EG: Tuina massage + CP CG: Sham Tuina Massage + CP | MAS elbow flexors, wrist flexors, knee flexors, knee extensors. Better EG after treatment and 3 months follow-up FMA-U * mBI * |
| Wang, 2019 | Motor function upper/lower limbs Spasticity elbow, wrist and finger flexors ADL | FMA-Total FMA-U MAS mBI | T0: Before treatment T1: After treatment T2: Follow-up 3 months T3: Follow-up 6 months | EG: Tuina massage + CP CG:CP | MAS elbow, wrist and fingers flexors Better EG within 1-3 weeks after stroke onset and 3-6 months’ follow-up FMA upper limb Better EG after treatment and 3-6 months’ follow-up ADL * |
| Xie, 2019 | Motor function lower limb Spasticity lower limb ADL | FMA-L MAS mBI | T0: Before treatment T1: After treatment | EG: Tuina massage + CP CG: CP | MAS lower limb, FMA-L and mBI Better EG after treatment ADL * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cabanas-Valdés, R.; Calvo-Sanz, J.; Serra-Llobet, P.; Alcoba-Kait, J.; González-Rueda, V.; Rodríguez-Rubio, P.R. The Effectiveness of Massage Therapy for Improving Sequelae in Post-Stroke Survivors. A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 4424. https://doi.org/10.3390/ijerph18094424
Cabanas-Valdés R, Calvo-Sanz J, Serra-Llobet P, Alcoba-Kait J, González-Rueda V, Rodríguez-Rubio PR. The Effectiveness of Massage Therapy for Improving Sequelae in Post-Stroke Survivors. A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2021; 18(9):4424. https://doi.org/10.3390/ijerph18094424
Chicago/Turabian StyleCabanas-Valdés, Rosa, Jordi Calvo-Sanz, Pol Serra-Llobet, Joana Alcoba-Kait, Vanessa González-Rueda, and Pere Ramón Rodríguez-Rubio. 2021. "The Effectiveness of Massage Therapy for Improving Sequelae in Post-Stroke Survivors. A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 18, no. 9: 4424. https://doi.org/10.3390/ijerph18094424
APA StyleCabanas-Valdés, R., Calvo-Sanz, J., Serra-Llobet, P., Alcoba-Kait, J., González-Rueda, V., & Rodríguez-Rubio, P. R. (2021). The Effectiveness of Massage Therapy for Improving Sequelae in Post-Stroke Survivors. A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 18(9), 4424. https://doi.org/10.3390/ijerph18094424







