Health Risks and Consequences of a COVID-19 Infection for People with Disabilities: Scoping Review and Descriptive Thematic Analysis
Abstract
1. Introduction
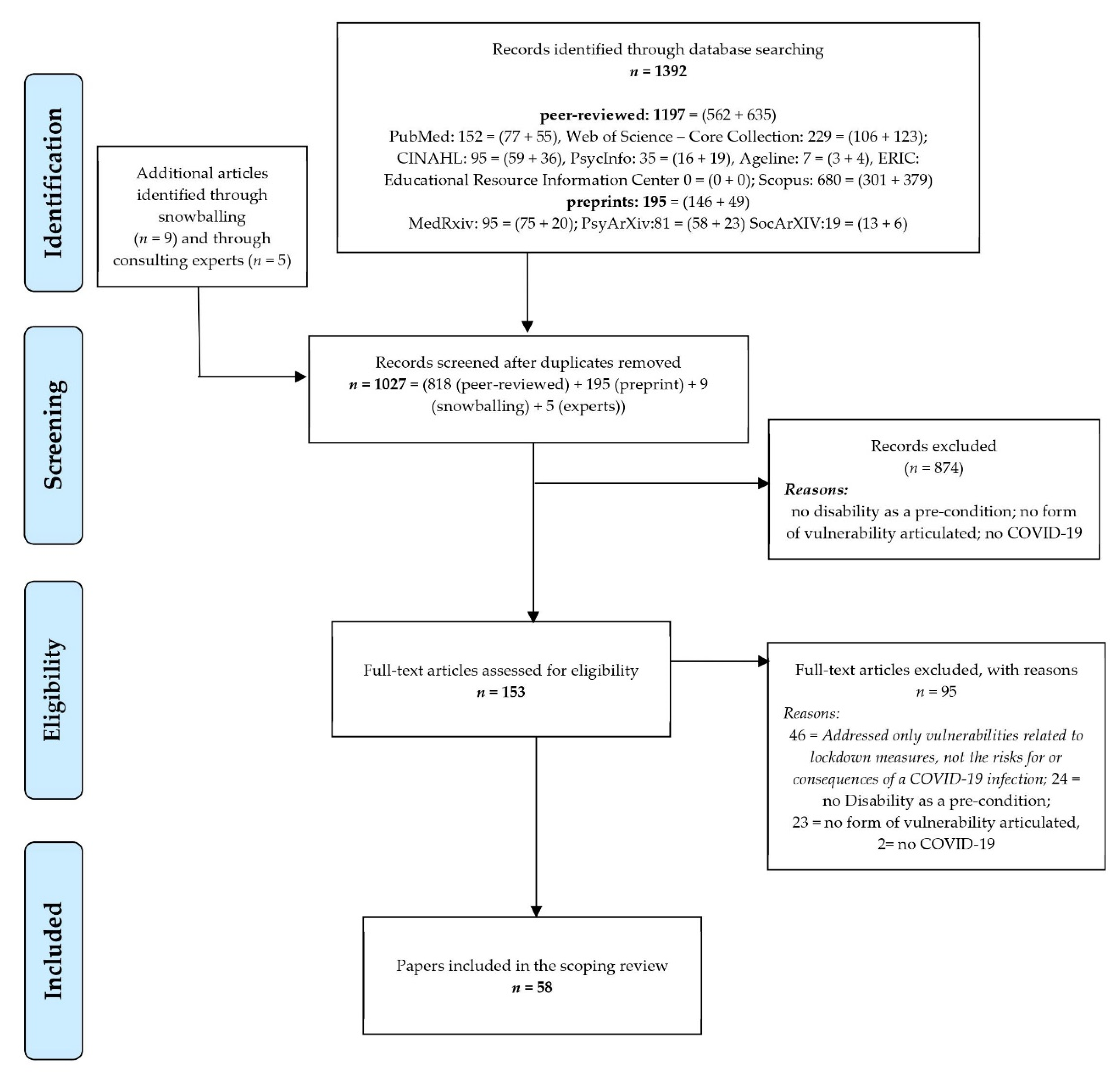
2. Methods
2.1. Eligibility Criteria
2.2. Information Sources and Search
2.3. Selection Process
2.4. Data Charting and Items
2.5. Critical Appraisal
2.6. Synthesis of the Results
3. Results
3.1. People with Disabilities Living in Residential or Long-Term Care Facilities Were More Likely to Have Greater Infection Rates
3.2. Intersecting Mediators of Greater Infection Risks
3.3. People with Disabilities often Face Greater Health Consequences When Infected
3.4. The Unethical Disadvantage in the Rationing of Lifesaving and Critical Care
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The Lancet. Redefining vulnerability in the era of COVID-19. Lancet (Lond. Engl.) 2020, 395, 1089. [Google Scholar] [CrossRef]
- Shadmi, E.; Chen, Y.; Dourado, I.; Faran-Perach, I.; Furler, J.; Hangoma, P.; Hanvoravongchai, P.; Obando, C.; Petrosyan, V.; Rao, K.D.; et al. Health equity and COVID-19: Global perspectives. Int. J. Equity Health 2020, 19, 104. [Google Scholar] [CrossRef]
- Glover, R.E.; van Schalkwyk, M.C.I.; Akl, E.A.; Kristjannson, E.; Lotfi, T.; Petkovic, J.; Petticrew, M.P.; Pottie, K.; Tugwell, P.; Welch, V. A framework for identifying and mitigating the equity harms of COVID-19 policy interventions. J. Clin. Epidemiol. 2020, 128, 35–48. [Google Scholar] [CrossRef]
- Ahmad, A.; Chung, R.; Eckenwiler, L.; Ganguli-Mitra, A.; Hunt, M.; Richards, R.; Saghai, Y.; Schwartz, L.; Scully, J.L.; Wild, V. What does it mean to be made vulnerable in the era of COVID-19? Lancet (Lond. Engl.) 2020, 395, 1481–1482. [Google Scholar] [CrossRef]
- Rozenfeld, Y.; Beam, J.; Maier, H.; Haggerson, W.; Boudreau, K.; Carlson, J.; Medows, R. A model of disparities: Risk factors associated with COVID-19 infection. Int. J. Equity Health 2020, 19, 126. [Google Scholar] [CrossRef]
- Sakellariou, D.; Malfitano, A.P.S.; Rotarou, E.S. Disability inclusiveness of government responses to COVID-19 in South America: A framework analysis study. Int. J. Equity Health 2020, 19. [Google Scholar] [CrossRef]
- Rotarou, E.S.; Sakellariou, D.; Kakoullis, E.J.; Warren, N. Disabled people in the time of COVID-19: Identifying needs, promoting inclusivity. J. Glob. Health 2021, 11, 03007. [Google Scholar] [CrossRef]
- Rowland, M.; Peterson-Besse, J.; Dobbertin, K.; Walsh, E.S.; Horner-Johnson, W. Health outcome disparities among subgroups of people with disabilities: A scoping review. Disabil. Health J. 2014, 7, 136–150. [Google Scholar] [CrossRef]
- Mithen, J.; Aitken, Z.; Ziersch, A.; Kavanagh, A.M. Inequalities in social capital and health between people with and without disabilities. Soc. Sci. Med. 2015, 126, 26–35. [Google Scholar] [CrossRef]
- Peterson-Besse, J.J.; Walsh, E.S.; Horner-Johnson, W.; Goode, T.D.; Wheeler, B. Barriers to health care among people with disabilities who are members of underserved racial/ethnic groups: A scoping review of the literature. Med. Care 2014, 52, S51–63. [Google Scholar] [CrossRef]
- Shakespeare, T. Disability Rights and Wrongs Revisited, 2nd ed.; Routledge: New York, NY, USA, 2014. [Google Scholar]
- Scully, J.L. Disability, Disablism, and COVID-19 Pandemic Triage. J. Bioethical Inq. 2020, 1–5. [Google Scholar] [CrossRef]
- Goggin, G.; Ellis, K. Disability, communication, and life itself in the COVID-19 pandemic. Health Sociol. Rev. 2020, 29, 168–176. [Google Scholar] [CrossRef]
- Katz, A.S.; Hardy, B.-J.; Firestone, M.; Lofters, A.; Morton-Ninomiya, M.E. Vagueness, power and public health: Use of ‘vulnerable‘ in public health literature. Crit. Public Health 2020, 30, 601–611. [Google Scholar] [CrossRef]
- Armitage, R.; Nellums, L.B. The COVID-19 response must be disability inclusive. Lancet. Public Health 2020, 5, e257. [Google Scholar] [CrossRef]
- Kuper, H.; Banks, L.M.; Bright, T.; Davey, C.; Shakespeare, T. Disability-inclusive COVID-19 response: What it is, why it is important and what we can learn from the United Kingdom’s response. Wellcome Open Res. 2020, 5, 79. [Google Scholar] [CrossRef]
- Banks, L.M.; Davey, C.; Shakespeare, T.; Kuper, H. Disability-inclusive responses to COVID-19: Lessons learnt from research on social protection in low- and middle-income countries. World Dev. 2021, 137, 105178. [Google Scholar] [CrossRef] [PubMed]
- Jesus, T.S.; Kamalakannan, S.; Bhattacharjya, S.; Bogdanova, Y.; Arango-Lasprilla, J.C.; Bentley, J.; Gibson, B.E.; Papadimitriou, C. People with Disabilities and Other Forms of Vulnerability to the COVID-19 Pandemic: Study Protocol for a Scoping Review and Thematic Analysis. Arch. Rehabil. Res. Clin. Transl. 2020, 2, 100079. [Google Scholar] [CrossRef]
- Jesus, T.S.; Bhattacharjya, S.; Papadimitriou, C.; Bogdanova, Y.; Bentley, J.; Arango-Lasprilla, J.C.; Kamalakannan, S.; RETF&ING, A. Lockdown-related disparities experienced by People with Disabilities during the first wave of the COVID-19 pandemic: Scoping review and thematic synthesis. Int. J. Environ. Res. Public Health 2021. Under review (twin submission). [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Gianola, S.; Jesus, T.S.; Bargeri, S.; Castellini, G. Characteristics of academic publications, preprints, and registered clinical trials on the COVID-19 pandemic. PLoS ONE 2020, 15, e0240123. [Google Scholar] [CrossRef]
- Colquhoun, H.L.; Levac, D.; O’Brien, K.K.; Straus, S.; Tricco, A.C.; Perrier, L.; Kastner, M.; Moher, D. Scoping reviews: Time for clarity in definition, methods, and reporting. J. Clin. Epidemiol. 2014, 67, 1291–1294. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. Jbi Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef]
- Colquhoun, H.L.; Jesus, T.S.; O’Brien, K.K.; Tricco, A.C.; Chui, A.; Zarin, W.; Lillie, E.; Hitzig, S.L.; Seaton, S.; Engel, L.; et al. Scoping Review on Rehabilitation Scoping Reviews. Arch. Phys. Med. Rehabil. 2020, 101, 1462–1469. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Reflecting on reflexive thematic analysis. Qual. Res. Sportexercise Health 2019, 11, 589–597. [Google Scholar] [CrossRef]
- Sholas, M.G. The actual and potential impact of the novel 2019 coronavirus on pediatric rehabilitation: A commentary and review of its effects and potential disparate influence on Black, Latinx and Native American marginalized populations in the United States. J. Pediatric Rehabil. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Cox, D.J.; Plavnick, J.B.; Brodhead, M.T. A Proposed Process for Risk Mitigation During the COVID-19 Pandemic. Behav. Anal. Pract. 2020, 13, 1–7. [Google Scholar] [CrossRef]
- Ben-Pazi, H.; Beni-Adani, L.; Lamdan, R. Accelerating Telemedicine for Cerebral Palsy During the COVID-19 Pandemic and Beyond. Front. Neurol. 2020, 11, 746. [Google Scholar] [CrossRef] [PubMed]
- Safta-Zecheria, L. Challenges posed by COVID-19 to the health of people with disabilities living in residential care facilities in Romania. Disabil. Soc. 2020, 35, 837–843. [Google Scholar] [CrossRef]
- Guidry-Grimes, L.; Savin, K.; Stramondo, J.A.; Reynolds, J.M.; Tsaplina, M.; Burke, T.B.; Ballantyne, A.; Kittay, E.F.; Stahl, D.; Scully, J.L.; et al. Disability Rights as a Necessary Framework for Crisis Standards of Care and the Future of Health Care. Hastings Cent. Rep. 2020, 50, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Pineda, V.S.; Corburn, J. Disability, Urban Health Equity, and the Coronavirus Pandemic: Promoting Cities for All. J. Urban Health: Bull. N. Y. Acad. Med. 2020, 97, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Senjam, S.S. Impact of COVID-19 pandemic on people living with visual disability. Indian J. Ophthalmol. 2020, 68, 1367–1370. [Google Scholar] [CrossRef]
- Waldman, H.B.; Rader, R.; Perlman, S.P. What Are We Learning? Except. Parent 2020, 50, 17–19. [Google Scholar]
- Waldman, H.B.; Rader, R.; Keller, S.M.; Perlman, S.P. Who’s Next? Except. Parent 2020, 50, 16–18. [Google Scholar]
- Brown, E.E.; Kumar, S.; Rajji, T.K.; Pollock, B.G.; Mulsant, B.H. Anticipating and Mitigating the Impact of the COVID-19 Pandemic on Alzheimer’s Disease and Related Dementias. Am. J. Geriatr. Psychiatry 2020, 28, 712–721. [Google Scholar] [CrossRef]
- Palipana, D. COVID-19 and spinal cord injuries: The viewpoint from an emergency department resident with quadriplegia. Ema Emerg. Med. Australas. 2020, 32, 692–693. [Google Scholar] [CrossRef]
- McKinney, E.L.; McKinney, V.; Swartz, L. COVID-19, disability and the context of healthcare triage in South Africa: Notes in a time of pandemic. Afr. J. Disabil. 2020, 9. [Google Scholar] [CrossRef]
- Lund, E.M. Interpersonal violence against people with disabilities: Additional concerns and considerations in the COVID-19 pandemic. Rehabil. Psychol. 2020, 65, 199–205. [Google Scholar] [CrossRef]
- Eskytė, I.; Lawson, A.; Orchard, M.; Andrews, E. Out on the Streets-Crisis, Opportunity and Disabled People in the Era of Covid-19: Reflections from the UK. Alter 2020. [Google Scholar] [CrossRef]
- Tohidast, S.A.; Mansuri, B.; Bagheri, R.; Azimi, H. Provision of speech-language pathology services for the treatment of speech and language disorders in children during the COVID-19 pandemic: Problems, concerns, and solutions. Int. J. Pediatr. Otorhinolaryngol. 2020, 138. [Google Scholar] [CrossRef]
- Devita, M.; Bordignon, A.; Sergi, G.; Coin, A. The psychological and cognitive impact of Covid-19 on individuals with neurocognitive impairments: Research topics and remote intervention proposals. Aging Clin. Exp. Res. 2021. [Google Scholar] [CrossRef]
- Jesus, T.S.; Landry, M.D.; Jacobs, K. A ’new normal’ following COVID-19 and the economic crisis: Using systems thinking to identify challenges and opportunities in disability, telework, and rehabilitation. Work (Read. Mass.) 2020, 67, 37–46. [Google Scholar] [CrossRef]
- Lund, E.M.; Ayers, K.B. Raising awareness of disabled lives and health care rationing during the COVID-19 pandemic. Psychol. Trauma: Theoryresearchpractice Policy 2020, 12, S210–S211. [Google Scholar] [CrossRef]
- Parsons, J.A.; Johal, H.K. Best interests versus resource allocation: Could COVID-19 cloud decision-making for the cognitively impaired? J. Med Ethics 2020, 46, 447–450. [Google Scholar] [CrossRef]
- Chase, J. Caring for Frail Older Adults During COVID-19: Integrating Public Health Ethics into Clinical Practice. J. Am. Geriatr. Soc. 2020, 68, 1666–1670. [Google Scholar] [CrossRef]
- Chen, B.; McNamara, D.M. Disability Discrimination, Medical Rationing and COVID-19. Asian Bioeth. Rev. 2020, 1–8. [Google Scholar] [CrossRef]
- Singh, S. Disability ethics in the coronavirus crisis. J. Fam. Med. Prim. Care 2020, 9, 2167–2171. [Google Scholar] [CrossRef]
- Sabatello, M.; Burke, T.B.; McDonald, K.E.; Appelbaum, P.S. Disability, Ethics, and Health Care in the COVID-19 Pandemic. Am. J. Public Health 2020, 110, 1523–1527. [Google Scholar] [CrossRef]
- Sabatello, M.; Landes, S.D.; McDonald, K.E. People With Disabilities in COVID-19: Fixing Our Priorities. Am. J. Bioeth. 2020, 20, 187–190. [Google Scholar] [CrossRef]
- Llanes Mabalot, C. Advocacy During Covid-19. Except. Parent 2020, 50, 14–16. [Google Scholar]
- Iaboni, A.; Cockburn, A.; Marcil, M.; Rodrigues, K.; Marshall, C.; Garcia, M.A.; Quirt, H.; Reynolds, K.B.; Keren, R.; Flint, A.J. Achieving Safe, Effective, and Compassionate Quarantine or Isolation of Older Adults With Dementia in Nursing Homes. Am. J. Geriatr. Psychiatry Off. J. Am. Assoc. Geriatr. Psychiatry 2020, 28, 835–838. [Google Scholar] [CrossRef]
- Andrews, E.E.; Ayers, K.B.; Brown, K.S.; Dunn, D.S.; Pilarski, C.R. No body is expendable: Medical rationing and disability justice during the COVID-19 pandemic. Am. Psychol. 2020. [Google Scholar] [CrossRef]
- Boyle, C.A.; Fox, M.H.; Havercamp, S.M.; Zubler, J. The public health response to the COVID-19 pandemic for people with disabilities. Disabil. Health J. 2020, 13, 100943. [Google Scholar] [CrossRef]
- Courtenay, K.; Perera, B. COVID-19 and people with intellectual disability: Impacts of a pandemic. Ir. J. Psychol. Med. 2020, 37, 231–236. [Google Scholar] [CrossRef]
- Mello, M.M.; Persad, G.; White, D.B. Respecting Disability Rights—Toward Improved Crisis Standards of Care. N. Engl. J. Med. 2020, 383, e26. [Google Scholar] [CrossRef]
- Solomon, M.Z.; Wynia, M.K.; Gostin, L.O. Covid-19 Crisis Triage—Optimizing Health Outcomes and Disability Rights. N. Engl. J. Med. 2020, 383, e27. [Google Scholar] [CrossRef]
- Korupolu, R.; Stampas, A.; Gibbons, C.; Hernandez Jimenez, I.; Skelton, F.; Verduzco-Gutierrez, M. COVID-19: Screening and triage challenges in people with disability due to Spinal Cord Injury. Spinal Cord Ser. Cases 2020, 6, 35. [Google Scholar] [CrossRef] [PubMed]
- Okonkwo, N.E.; Aguwa, U.T.; Jang, M.; Barré, I.A.; Page, K.R.; Sullivan, P.S.; Beyrer, C.; Baral, S. COVID-19 and the US response: Accelerating health inequities. BMJ Evid. Based Med. 2020. [Google Scholar] [CrossRef]
- Favalli, E.G.; Ingegnoli, F.; De Lucia, O.; Cincinelli, G.; Cimaz, R.; Caporali, R. COVID-19 infection and rheumatoid arthritis: Faraway, so close! Autoimmun. Rev. 2020, 19, 102523. [Google Scholar] [CrossRef]
- Alexander, R.; Ravi, A.; Barclay, H.; Sawhney, I.; Chester, V.; Malcolm, V.; Brolly, K.; Mukherji, K.; Zia, A.; Tharian, R.; et al. Guidance for the Treatment and Management of COVID-19 Among People with Intellectual Disabilities. J. Policy Pract. Intellect. Disabil. 2020. [Google Scholar] [CrossRef]
- Manto, M.; Dupre, N.; Hadjivassiliou, M.; Louis, E.D.; Mitoma, H.; Molinari, M.; Shaikh, A.G.; Soong, B.W.; Strupp, M.; Van Overwalle, F.; et al. Medical and Paramedical Care of Patients with Cerebellar Ataxia During the COVID-19 Outbreak: Seven Practical Recommendations of the COVID 19 Cerebellum Task Force. Front. Neurol. 2020, 11, 516. [Google Scholar] [CrossRef]
- Turk, M.A.; McDermott, S. The COVID-19 pandemic and people with disability. Disabil. Health J. 2020, 13. [Google Scholar] [CrossRef]
- Ibanez, A.; Kosik, K.S. COVID-19 in older people with cognitive impairment in Latin America. Lancet. Neurol. 2020, 19, 719–721. [Google Scholar] [CrossRef]
- Landi, D.; Ponzano, M.; Nicoletti, C.G.; Cecchi, G.; Cola, G.; Mataluni, G.; Mercuri, N.B.; Sormani, M.P.; Marfia, G.A. Adherence to social distancing and use of personal protective equipment and the risk of SARS-CoV-2 infection in a cohort of patients with multiple sclerosis. Mult. Scler. Relat. Disord. 2020, 45, 102359. [Google Scholar] [CrossRef]
- Muruganandam, P.; Neelamegam, S.; Menon, V.; Alexander, J.; Chaturvedi, S.K. COVID-19 and Severe Mental Illness: Impact on patients and its relation with their awareness about COVID-19. Psychiatry Res. 2020, 291, 113265. [Google Scholar] [CrossRef]
- Umucu, E.; Lee, B. Examining the impact of COVID-19 on stress and coping strategies in individuals with disabilities and chronic conditions. Rehabil. Psychol. 2020, 65, 193–198. [Google Scholar] [CrossRef]
- Stillman, M.D.; Capron, M.; Alexander, M.; Di Giusto, M.L.; Scivoletto, G. COVID-19 and spinal cord injury and disease: Results of an international survey. Spinal Cord Ser. Cases 2020, 6, 21. [Google Scholar] [CrossRef]
- Turk, M.A.; Landes, S.D.; Formica, M.K.; Goss, K.D. Intellectual and developmental disability and COVID-19 case-fatality trends: TriNetX analysis. Disabil. Health J. 2020, 13, 100942. [Google Scholar] [CrossRef]
- Landes, S.D.; Turk, M.A.; Formica, M.K.; McDonald, K.E.; Stevens, J.D. COVID-19 outcomes among people with intellectual and developmental disability living in residential group homes in New York State. Disabil. Health J. 2020, 13, 100969. [Google Scholar] [CrossRef]
- Azarpazhooh, M.R.; Amiri, A.; Morovatdar, N.; Steinwender, S.; Rezaei Ardani, A.; Yassi, N.; Biller, J.; Stranges, S.; Tokazebani Belasi, M.; Neya, S.K.; et al. Correlations between COVID-19 and burden of dementia: An ecological study and review of literature. J. Neurol. Sci. 2020, 416, 117013. [Google Scholar] [CrossRef]
- Abedi, V.; Olulana, O.; Avula, V.; Chaudhary, D.; Khan, A.; Shahjouei, S.; Li, J.; Zand, R. Racial, Economic, and Health Inequality and COVID-19 Infection in the United States. J. Racial Ethn. Health Disparities 2020, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Manchanda, E.C.C.; Sanky, C.; Appel, J.M. Crisis Standards of Care in the USA: A Systematic Review and Implications for Equity Amidst COVID-19. J. Racial Ethn. Health Disparities 2020, 1–13. [Google Scholar] [CrossRef]
- Yap, J.; Chaudhry, V.; Jha, C.K.; Mani, S.; Mitra, S. Are responses to the pandemic inclusive? A rapid virtual audit of COVID-19 press briefings in LMICs. World Dev. 2020, 136, 105122. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Díaz, E.; Iglesias-Sánchez, P.P.; Jambrino-Maldonado, C. Exploring WHO Communication during the COVID 19 Pandemic through the WHO Website Based on W3C Guidelines: Accessible for All? Int. J. Environ. Res. Public Health 2020, 17, 5663. [Google Scholar] [CrossRef]
- De Cauwer, H.; Spaepen, A. Are patients with Down syndrome vulnerable to life-threatening COVID-19? Acta Neurol. Belg. 2020, 1–3. [Google Scholar] [CrossRef]
- Olulana, O.; Abedi, V.; Avula, V.; Chaudhary, D.; Khan, A.; Shahjouei, S.; Li, J.; Zand, R. Regional Association of Disability and SARS-CoV-2 Infection in 369 Counties of the United States. medRxiv 2020. [Google Scholar] [CrossRef]
- Balestrini, S.; Koepp, M.J.; Gandhi, S.; Rickman, H.; Shin, G.Y.; Houlihan, C.; Anders-Cannon, J.; Silvennoinen, K.; Xiao, F.; Zagaglia, S.; et al. Clinical outcomes of SARS-CoV-2 pandemic in long-term care facilities for people with epilepsy: Observational study. medRxiv 2020. [Google Scholar] [CrossRef]
- Kendall, E.; Ehrlich, C.; Chapman, K.; Shirota, C.; Allen, G.; Gall, A.; Kek-Pamenter, J.A.; Cocks, K.; Palipana, D. Immediate and Long-Term Implications of the COVID-19 Pandemic for People with Disabilities. Am J Public Health 2020, 110, 1774–1779. [Google Scholar] [CrossRef]
- D’Cruz, M.; Banerjee, D. ’An invisible human rights crisis’: The marginalization of older adults during the COVID-19 pandemic-An advocacy review. Psychiatry Res. 2020, 292, 113369. [Google Scholar] [CrossRef] [PubMed]
- Latteck Ä, D.; Bruland, D. Inclusion of People with Intellectual Disabilities in Health Literacy: Lessons Learned from Three Participative Projects for Future Initiatives. Int. J. Environ. Res. Public Health 2020, 17, 2455. [Google Scholar] [CrossRef] [PubMed]
- Dyer, C. COVID-19: Adults with learning disabilities should have priority access to vaccination, say lawyers. BMJ (Clin. Res. Ed.) 2020, 371, m4824. [Google Scholar] [CrossRef]
- HHS Office for Civil Rights in Action. BULLETIN: Civil Rights, HIPAA, and the Coronavirus Disease 2019 (COVID-19), March 28, 2020. Available online: https://www.hhs.gov/sites/default/files/ocr-bulletin-3-28-20.pdf (accessed on 29 January 2020).
- Banks, L.M.; Kuper, H.; Polack, S. Poverty and disability in low- and middle-income countries: A systematic review. PLoS ONE 2017, 12, e0189996. [Google Scholar] [CrossRef] [PubMed]
- Bright, T.; Kuper, H. A Systematic Review of Access to General Healthcare Services for People with Disabilities in Low and Middle Income Countries. Int. J. Environ. Res. Public Health 2018, 15, 1879. [Google Scholar] [CrossRef] [PubMed]
- Kamenov, K.; Mills, J.A.; Chatterji, S.; Cieza, A. Needs and unmet needs for rehabilitation services: A scoping review. Disabil. Rehabil. 2019, 41, 1227–1237. [Google Scholar] [CrossRef] [PubMed]
- Magnusson, D.; Sweeney, F.; Landry, M. Provision of rehabilitation services for children with disabilities living in low- and middle-income countries: A scoping review. Disabil. Rehabil. 2019, 41, 861–868. [Google Scholar] [CrossRef] [PubMed]
- Perera, B.; Laugharne, R.; Henley, W.; Zabel, A.; Lamb, K.; Branford, D.; Courtanay, K.; Alexander, R.; Purandare, K.; Wijeratne, A.; et al. COVID-19 deaths in people with intellectual disability in the UK and Ireland: Descriptive study. Bjpsych Open 2020, 6, e123. [Google Scholar] [CrossRef] [PubMed]
- Lebrasseur, A.; Fortin-Bédard, N.; Lettre, J.; Bussières, E.L.; Best, K.; Boucher, N.; Hotton, M.; Beaulieu-Bonneau, S.; Mercier, C.; Lamontagne, M.E.; et al. Impact of COVID-19 on people with physical disabilities: A rapid review. Disabil. Health J. 2021, 14, 101014. [Google Scholar] [CrossRef]
- Reed, N.S.; Meeks, L.M.; Swenor, B.K. Disability and COVID-19: Who counts depends on who is counted. Lancet Public Health 2020, 5, e423. [Google Scholar] [CrossRef]
- Witham, M.D.; Anderson, E.; Carroll, C.B.; Dark, P.M.; Down, K.; Hall, A.S.; Knee, J.; Maher, E.R.; Maier, R.H.; Mountain, G.A.; et al. Ensuring that COVID-19 research is inclusive: Guidance from the NIHR INCLUDE project. BMJ Open 2020, 10, e043634. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | n (%) | Citations |
|---|---|---|
| Publications Type And Source | ||
| Perspective papers (e.g., viewpoints, commentaries, essays, ethics/advocacy) | 34 (58%) | [12,13,16,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57] |
| Narrative summary/review (non-systematic) | 3 (5%) | [58,59,60] |
| Framework or Experts recommendations | 3 (5%) | [3,61,62] |
| Editorial or Letter to the editor | 3 (5%) | [15,63,64] |
| Non-empirical (peer-reviewed): SUB-TOTAL | 41 (73 %) | - |
| Cross-sectional surveys | 4 (7%) | [65,66,67,68] |
| Systematic analysis of electronic medical/ administrative records | 2 (4%) | [69,70] |
| Ecological study | 2 (4%) | [71,72] |
| Systematic review | 1 (2%) | [73] |
| Analysis of COVID-19 press conferences | 1 (2%) | [74] |
| Analysis of webpages on accessibility compliance | 1 (2%) | [75] |
| Documentary research and framework analysis | 1 (2%) | [6] |
| Case report (4 patients) | 1 (2%) | [76] |
| Empirical studies (peer-reviewed): SUB-TOTAL | 13 (23%) | - |
| Ecological study | 1 (2%) | [77] |
| Observational multicenter study | 1 (2%) | [78] |
| Preprint studies: SUB-TOTAL | 2 (4%) | - |
| Geographical Focus | ||
| No geographical focus (e.g., applicable across locations) | 37 (63%) | [3,12,13,15,28,29,31,32,33,34,35,36,37,39,41,42,43,44,46,47,48,49,50,51,52,53,54,55,58,60,62,68,69,71,75,76] |
| United States of America (USA) | 9 (15%) | [27,56,57,59,67,70,72,73,77] |
| United Kingdom (UK) | 5 (8%) | [16,40,45,61,78] |
| Latin America | 2 (4%) | [6,64] |
| Low- and Middle-Income countries (LMICs) | 1 (2%) | [74] |
| South Africa | 1 (2%) | [38] |
| India | 1 (2%) | [66] |
| Romania | 1 (2%) | [30] |
| Italy | 1 (2%) | [65] |
| Health Conditions | ||
| People with disabilities, overall | 32 (56%) | [3,6,12,13,15,16,31,32,34,35,38,39,40,43,44,47,48,49,50,51,53,54,56,57,59,63,67,72,73,74,75,77] |
| Adults with cognitive impairment (e.g., dementia) or intellectual disabilities | 8 (14%) | [36,42,45,52,55,61,64,71] |
| People with disabilities living in residential or long-term facilities | 3 (5%) | [30,70,78] |
| Spinal cord injury | 3 (5%) | [37,58,68] |
| Children with disabilities (overall) | 2 (4%) | [27,41] |
| Older adults experiencing disabilities | 1 (2%) | [46] |
| People with developmental disabilities (overall) | 1 (2%) | [69] |
| Visual impairments | 1 (2%) | [33] |
| Autism spectrum disorder | 1 (2%) | [28] |
| Cerebral palsy | 1 (2%) | [29] |
| Cerebellar ataxia | 1 (2%) | [62] |
| Down’s syndrome | 1 (2%) | [76] |
| Severe mental illness | 1 (2%) | [66] |
| Multiple sclerosis | 1 (2%) | [65] |
| Rheumatoid arthritis | 1 (2%) | [60] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kamalakannan, S.; Bhattacharjya, S.; Bogdanova, Y.; Papadimitriou, C.; Arango-Lasprilla, J.C.; Bentley, J.; Jesus, T.S.; Refugee Empowerment Task Force, International Networking Group of the American Congress of Rehabilitation Medicine. Health Risks and Consequences of a COVID-19 Infection for People with Disabilities: Scoping Review and Descriptive Thematic Analysis. Int. J. Environ. Res. Public Health 2021, 18, 4348. https://doi.org/10.3390/ijerph18084348
Kamalakannan S, Bhattacharjya S, Bogdanova Y, Papadimitriou C, Arango-Lasprilla JC, Bentley J, Jesus TS, Refugee Empowerment Task Force, International Networking Group of the American Congress of Rehabilitation Medicine. Health Risks and Consequences of a COVID-19 Infection for People with Disabilities: Scoping Review and Descriptive Thematic Analysis. International Journal of Environmental Research and Public Health. 2021; 18(8):4348. https://doi.org/10.3390/ijerph18084348
Chicago/Turabian StyleKamalakannan, Sureshkumar, Sutanuka Bhattacharjya, Yelena Bogdanova, Christina Papadimitriou, Juan Carlos Arango-Lasprilla, Jacob Bentley, Tiago S. Jesus, and Refugee Empowerment Task Force, International Networking Group of the American Congress of Rehabilitation Medicine. 2021. "Health Risks and Consequences of a COVID-19 Infection for People with Disabilities: Scoping Review and Descriptive Thematic Analysis" International Journal of Environmental Research and Public Health 18, no. 8: 4348. https://doi.org/10.3390/ijerph18084348
APA StyleKamalakannan, S., Bhattacharjya, S., Bogdanova, Y., Papadimitriou, C., Arango-Lasprilla, J. C., Bentley, J., Jesus, T. S., & Refugee Empowerment Task Force, International Networking Group of the American Congress of Rehabilitation Medicine. (2021). Health Risks and Consequences of a COVID-19 Infection for People with Disabilities: Scoping Review and Descriptive Thematic Analysis. International Journal of Environmental Research and Public Health, 18(8), 4348. https://doi.org/10.3390/ijerph18084348








