Psychological Distress and Coping Ability of Women at High Risk of Hereditary Breast and Ovarian Cancer before Undergoing Genetic Counseling—An Exploratory Study from Germany
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
- ⁃
- three women with breast cancer or
- ⁃
- two women with breast cancer, one of them under the age of 51 years or
- ⁃
- one woman with breast cancer and one woman with ovarian cancer or
- ⁃
- two women with ovarian cancer or
- ⁃
- one woman with breast cancer and one man with breast cancer or
- ⁃
- one woman with ovarian cancer and one man with breast cancer or
- ⁃
- one woman with breast cancer under the age of 36 years or
- ⁃
- one woman with bilateral breast cancer and first diagnosis with 50 years or before or
- ⁃
- one woman with breast and ovarian cancer.
2.2. Measures
2.3. Data Analysis
3. Results
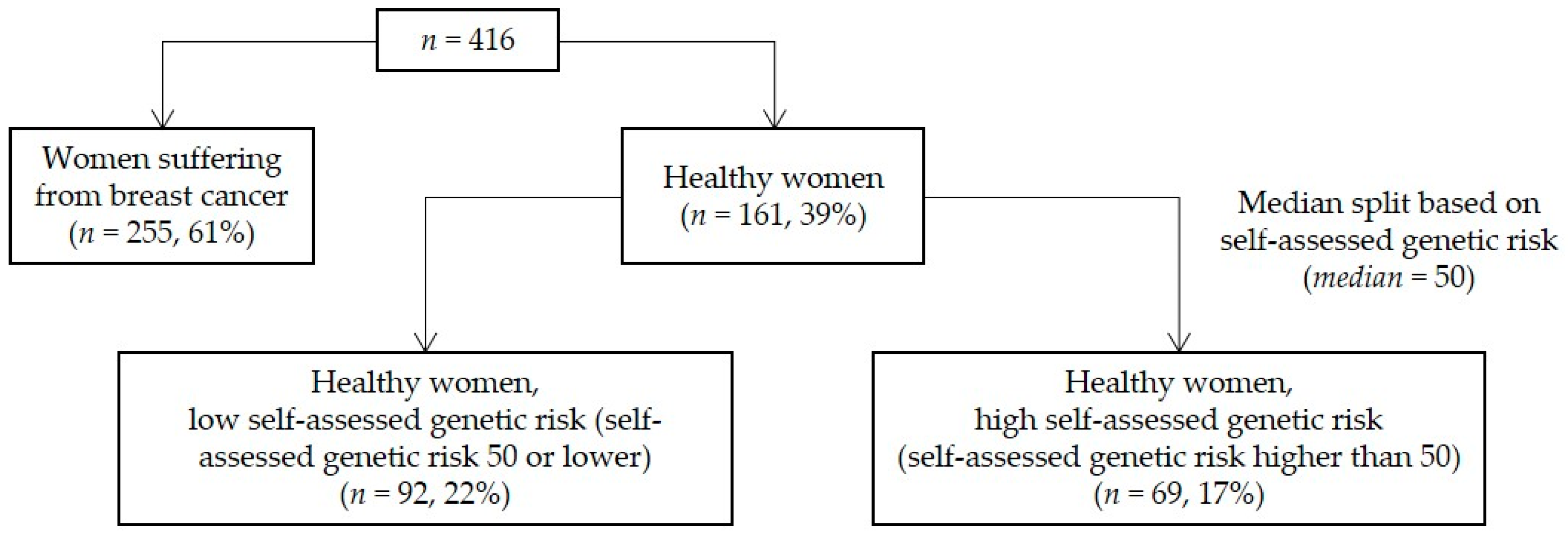
3.1. Sample Characteristics
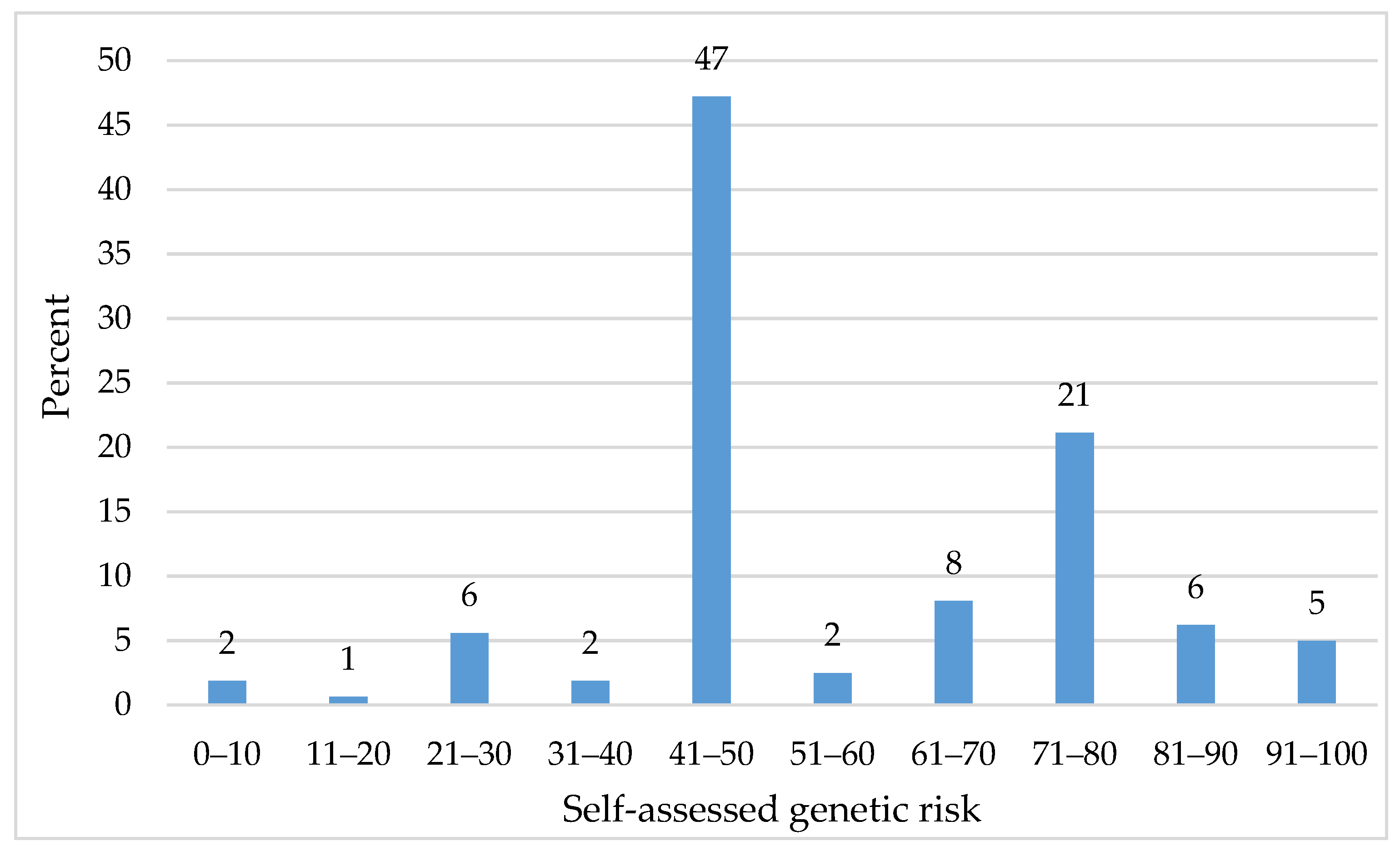
3.2. Most Healthy Women Considered Their Genetic Risk to Be High
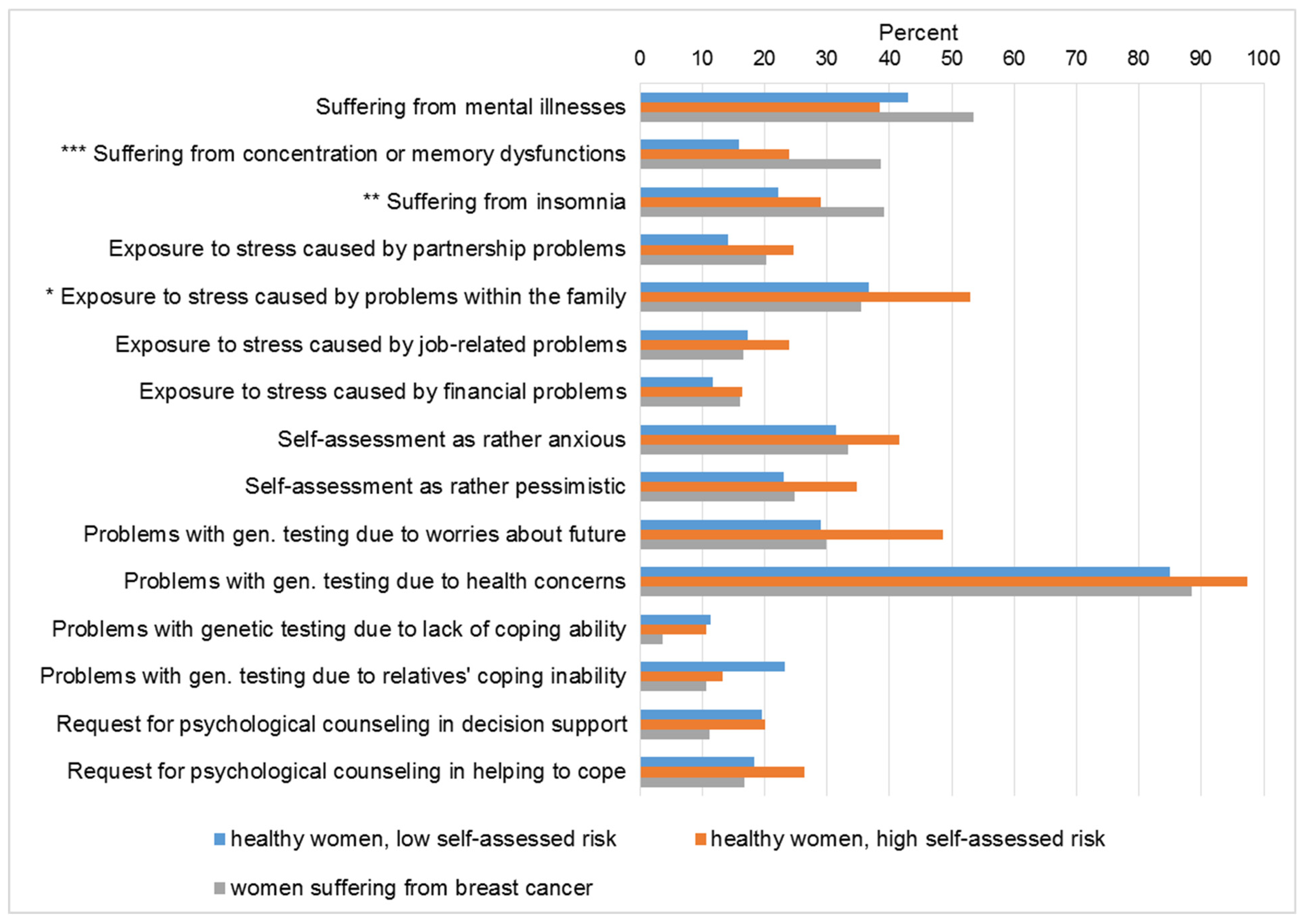
3.3. Women with Breast Cancer Showed the Highest Level of Suffering from Concentration and Memory Disfunctions as Well as Insomnia
3.4. Healthy Women with a High Self-Assessed Risk Showed the Highest Level of Stress Exposure and Were More Inclined to Request Psychological Support
3.5. Women without Children Worried Significantly More about the Future Than Women with Children
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nielsen, F.C.; van Overeem Hansen, T.; Sorensen, C.S. Hereditary breast and ovarian cancer: New genes in confined pathways. Nat. Rev. Cancer 2016, 16, 599–612. [Google Scholar] [CrossRef]
- Easton, D.F.; Pharoah, P.D.; Antoniou, A.C.; Tischkowitz, M.; Tavtigian, S.V.; Nathanson, K.L.; Devilee, P.; Meindl, A.; Couch, F.J.; Southey, M.; et al. Gene-panel sequencing and the prediction of breast-cancer risk. N. Engl. J. Med. 2015, 372, 2243–2257. [Google Scholar] [CrossRef]
- Kuchenbaecker, K.B.; Hopper, J.L.; Barnes, D.R.; Phillips, K.A.; Mooij, T.M.; Roos-Blom, M.J.; Jervis, S.; van Leeuwen, F.E.; Milne, R.L.; Andrieu, N.; et al. Risks of Breast, Ovarian, and Contralateral Breast Cancer for BRCA1 and BRCA2 Mutation Carriers. JAMA 2017, 317, 2402–2416. [Google Scholar] [CrossRef] [PubMed]
- Brewer, H.R.; Jones, M.E.; Schoemaker, M.J.; Ashworth, A.; Swerdlow, A.J. Family history and risk of breast cancer: An analysis accounting for family structure. Breast Cancer Res. Treat. 2017, 165, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Hampel, H.; Bennett, R.L.; Buchanan, A.; Pearlman, R.; Wiesner, G.L.; Guideline Development Group of the American College of Medical Genetics and Genomics Professional Practice and Guidelines Committee and of the National Society of Genetic Counselors Practice Guidelines Committee. A practice guideline from the American College of Medical Genetics and Genomics and the National Society of Genetic Counselors: Referral indications for cancer predisposition assessment. Genet. Med. 2015, 17, 70–87. [Google Scholar] [CrossRef] [PubMed]
- Linden, W.; Vodermaier, A.; Mackenzie, R.; Greig, D. Anxiety and depression after cancer diagnosis: Prevalence rates by cancer type, gender, and age. J. Affect. Disord. 2012, 141, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Voorwinden, J.S.; Jaspers, J.P. Prognostic Factors for Distress After Genetic Testing for Hereditary Cancer. J. Genet. Couns. 2016, 25, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Bonadona, V.; Saltel, P.; Desseigne, F.; Mignotte, H.; Saurin, J.C.; Wang, Q.; Sinilnikova, O.; Giraud, S.; Freyer, G.; Plauchu, H.; et al. Cancer patients who experienced diagnostic genetic testing for cancer susceptibility: Reactions and behavior after the disclosure of a positive test result. Cancer Epidemiol. Biomark. Prev. 2002, 11, 97–104. [Google Scholar]
- Yanes, T.; Willis, A.M.; Meiser, B.; Tucker, K.M.; Best, M. Psychosocial and behavioral outcomes of genomic testing in cancer: A systematic review. Eur. J. Hum. Genet. 2019, 27, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Ringwald, J.; Wochnowski, C.; Bosse, K.; Giel, K.E.; Schaffeler, N.; Zipfel, S.; Teufel, M. Psychological Distress, Anxiety, and Depression of Cancer-Affected BRCA1/2 Mutation Carriers: A Systematic Review. J. Genet. Couns. 2016, 25, 880–891. [Google Scholar] [CrossRef]
- Chad-Friedman, E.; Coleman, S.; Traeger, L.N.; Pirl, W.F.; Goldman, R.; Atlas, S.J.; Park, E.R. Psychological distress associated with cancer screening: A systematic review. Cancer 2017, 20, 3882–3894. [Google Scholar] [CrossRef]
- Schmutzler, R.; Schlegelberger, B.; Meindl, A.; Gerber, W.D.; Kiechle, M. Beratung, Genetische Testung und Prävention von Frauen mit einer familiären Belastung für das Mamma- und Ovarialkarzinom. Interdisziplinäre Empfehlungen des Verbundprojektes “Familiärer Brust- und Eierstockkrebs” der Deutschen Krebshilfe. Medgen 2003, 15, 385–395. [Google Scholar]
- Rutherford, E.J.; Kelly, J.; Lehane, E.A.; Livingstone, V.; Cotter, B.; Butt, A.; O’Sullivan, M.J.; O’Connell, F.; Redmond, H.P.; Corrigan, M.A. Health literacy and the perception of risk in a breast cancer family history clinic. Surgeon 2018, 16, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Glassey, R.; O’Connor, M.; Ives, A.; Saunders, C.; kConFab Investigators; O’Sullivan, S.; Hardcastle, S.J. Heightened perception of breast cancer risk in young women at risk of familial breast cancer. Fam. Cancer 2018, 17, 15–22. [Google Scholar] [CrossRef]
- Walter, F.M.; Emery, J. Perceptions of family history across common diseases: A qualitative study in primary care. Fam. Pract. 2006, 23, 472–480. [Google Scholar] [CrossRef] [PubMed]
- Vansenne, F.; Bossuyt, P.M.; de Borgie, C.A. Evaluating the psychological effects of genetic testing in symptomatic patients: A systematic review. Genet. Test. Mol. Biomark. 2009, 13, 555–563. [Google Scholar] [CrossRef]
- Mehnert, A.; Brahler, E.; Faller, H.; Harter, M.; Keller, M.; Schulz, H.; Wegscheider, K.; Weis, J.; Boehncke, A.; Hund, B.; et al. Four-Week Prevalence of Mental Disorders in Patients With Cancer Across Major Tumor Entities. J. Clin. Oncol. 2014, 32, 3540–3546. [Google Scholar] [CrossRef] [PubMed]
- Hamann, H.A.; Somers, T.J.; Smith, A.W.; Inslicht, S.S.; Baum, A. Posttraumatic stress associated with cancer history and BRCA1/2 genetic testing. Psychosom. Med. 2005, 67, 766–772. [Google Scholar] [CrossRef]
- Lindberg, N.M.; Wellisch, D.K. Identification of traumatic stress reactions in women at increased risk for breast cancer. Psychosomatics 2004, 45, 7–16. [Google Scholar] [CrossRef]
- Gibbons, A.; Groarke, A.; Sweeney, K. Predicting general and cancer-related distress in women with newly diagnosed breast cancer. BMC Cancer 2016, 16, 935–944. [Google Scholar] [CrossRef]
- Groarke, A.; Curtis, R.; Kerin, M. Global stress predicts both positive and negative emotional adjustment at diagnosis and post-surgery in women with breast cancer. Psycho-Oncol. 2013, 22, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Hopman, P.; Rijken, M. Illness perceptions of cancer patients: Relationships with illness characteristics and coping. Psycho-Oncol. 2015, 24, 11–18. [Google Scholar] [CrossRef]
- Young, A.L.; Butow, P.N.; Rhodes, P.; Tucker, K.M.; Williams, R.; Healey, E.; Wakefield, C.E. Talking across generations: Family communication about BRCA1 and BRCA2 genetic cancer risk. J. Genet. Couns. 2019, 28, 516–532. [Google Scholar] [CrossRef]
| Healthy Women, Low Self-Assessed Risk (n = 92, 22%) | Healthy Women, High Self-Assessed Risk (n = 69, 17%) | Women Suffering from Breast Cancer (n = 255, 61%) | ||||
|---|---|---|---|---|---|---|
| Valid Answers % | n (%) [Valid %]/ M (SD) | Valid Answers % | n (%) [Valid %]/ M (SD) | Valid Answers % | n (%) [Valid %]/ M (SD) | |
| Age | 100% | 39.20 (SD = 11.26) | 100% | 36.99 (SD = 9.91) | 100% | 51.45 (SD = 11.67) |
| Age at first diagnosis of breast cancer | 99% | 47.57 (SD = 11.06) | ||||
| Family situation | ||||||
| Having children | 100% | 52 (57%) [57%] | 100% | 46 (67%) [67%] | 100% | 203 (80%) [80%] |
| Number of children | 100% | 0.98 (SD = 1.01) | 100% | 1.14 (SD = 1.03) | 100% | 1.55 (SD = 1.06) |
| Age of youngest child | 55% | 14.33 (SD = 9.58) | 64% | 9.30 (SD = 8.74) | 78% | 22.22 (SD = 12.46) |
| Breast cancer family history | ||||||
| Mother diagnosed with breast cancer | 99% | 55 (60% [60%] | 100% | 44 (64%) [64%] | 99% | 75 (29%) [30%] |
| Mother’s age at first diagnosis of breast cancer | 60% | 48.35 (SD = 10.56) | 61% | 47.05 (SD = 13.69) | 29% | 57.80 (SD = 14.41) |
| Mother died from breast cancer | 60% | 29 (32%) [53%] | 64% | 24 (35%) [55%] | 29% | 44 (17%) [59%] |
| At least one sister diagnosed with breast cancer | 61% | 19 (21%) [34%] | 61% | 15 (22%) [36%] | 64% | 41 (16%) [25%] |
| Youngest affected sister’s age at first diagnosis of breast cancer | 21% | 40.32 (SD = 9.67) | 22% | 40.13 (SD = 8.68) | 16% | 52.57 (SD = 10.37) |
| At least one sister died from breast cancer | 21% | 4 (4%) [21%] | 20% | 2 (3%) [14%] | 17% | 10 (10%) [23%] |
| Number of other relatives diagnosed with breast cancer | 100% | 1.63 (SD = 1.40) | 100% | 1.96 (SD = 1.59) | 99% | 1.12 (SD = 1.23) |
| Number of other relatives diagnosed with ovarian cancer | 100% | 0.46 (SD = 0.79) | 100% | 0.62 (SD = 1.16) | 99% | 0.30 (SD = 0.61) |
| Number of other relatives diagnosed with other cancer types | 100% | 2.41 (SD = 2.24) | 100% | 2.54 (SD = 1.95) | 99% | 2.51 (SD = 2.02) |
| Women without Children (n = 114, 28%) | Women with Children (n = 301, 73%) | |||
|---|---|---|---|---|
| Valid Answers% | n (%) [Valid %] | Valid Answers% | n (%) [Valid %] | |
| Problems with genetic testing, because | ||||
| I cannot cope with the test result | 39% | 34% | ||
| No | 41 (36%) [93%] | 95 (32%) [93%] | ||
| Yes | 3 (3%) [7%] | 7 (2%) [7%] | ||
| my relatives cannot cope with the test result | 33% | 32% | ||
| No | 33 (29%) [87%] | 83 (28%) [86%] | ||
| Yes | 5 (4%) [13%] | 14 (5%) [14%] | ||
| I am afraid of the future *** | 48% | 38% | ||
| No | 27 (24%) [49%] | 86 (29%) [75%] | ||
| Yes | 28 (25%) [51%] | 29 (10%) [25%] | ||
| I am concerned about my health | 49% | 42% | ||
| No | 3 (3%) [5%] | 16 (5%) [13%] | ||
| Yes | 53 (47%) [95%] | 109 (36%) [87%] | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vajen, B.; Rosset, M.; Wallaschek, H.; Baumann, E.; Schlegelberger, B. Psychological Distress and Coping Ability of Women at High Risk of Hereditary Breast and Ovarian Cancer before Undergoing Genetic Counseling—An Exploratory Study from Germany. Int. J. Environ. Res. Public Health 2021, 18, 4338. https://doi.org/10.3390/ijerph18084338
Vajen B, Rosset M, Wallaschek H, Baumann E, Schlegelberger B. Psychological Distress and Coping Ability of Women at High Risk of Hereditary Breast and Ovarian Cancer before Undergoing Genetic Counseling—An Exploratory Study from Germany. International Journal of Environmental Research and Public Health. 2021; 18(8):4338. https://doi.org/10.3390/ijerph18084338
Chicago/Turabian StyleVajen, Beate, Magdalena Rosset, Hannah Wallaschek, Eva Baumann, and Brigitte Schlegelberger. 2021. "Psychological Distress and Coping Ability of Women at High Risk of Hereditary Breast and Ovarian Cancer before Undergoing Genetic Counseling—An Exploratory Study from Germany" International Journal of Environmental Research and Public Health 18, no. 8: 4338. https://doi.org/10.3390/ijerph18084338
APA StyleVajen, B., Rosset, M., Wallaschek, H., Baumann, E., & Schlegelberger, B. (2021). Psychological Distress and Coping Ability of Women at High Risk of Hereditary Breast and Ovarian Cancer before Undergoing Genetic Counseling—An Exploratory Study from Germany. International Journal of Environmental Research and Public Health, 18(8), 4338. https://doi.org/10.3390/ijerph18084338






