Tackling Airborne Virus Threats in the Food Industry: A Proactive Approach
Abstract
1. Introduction
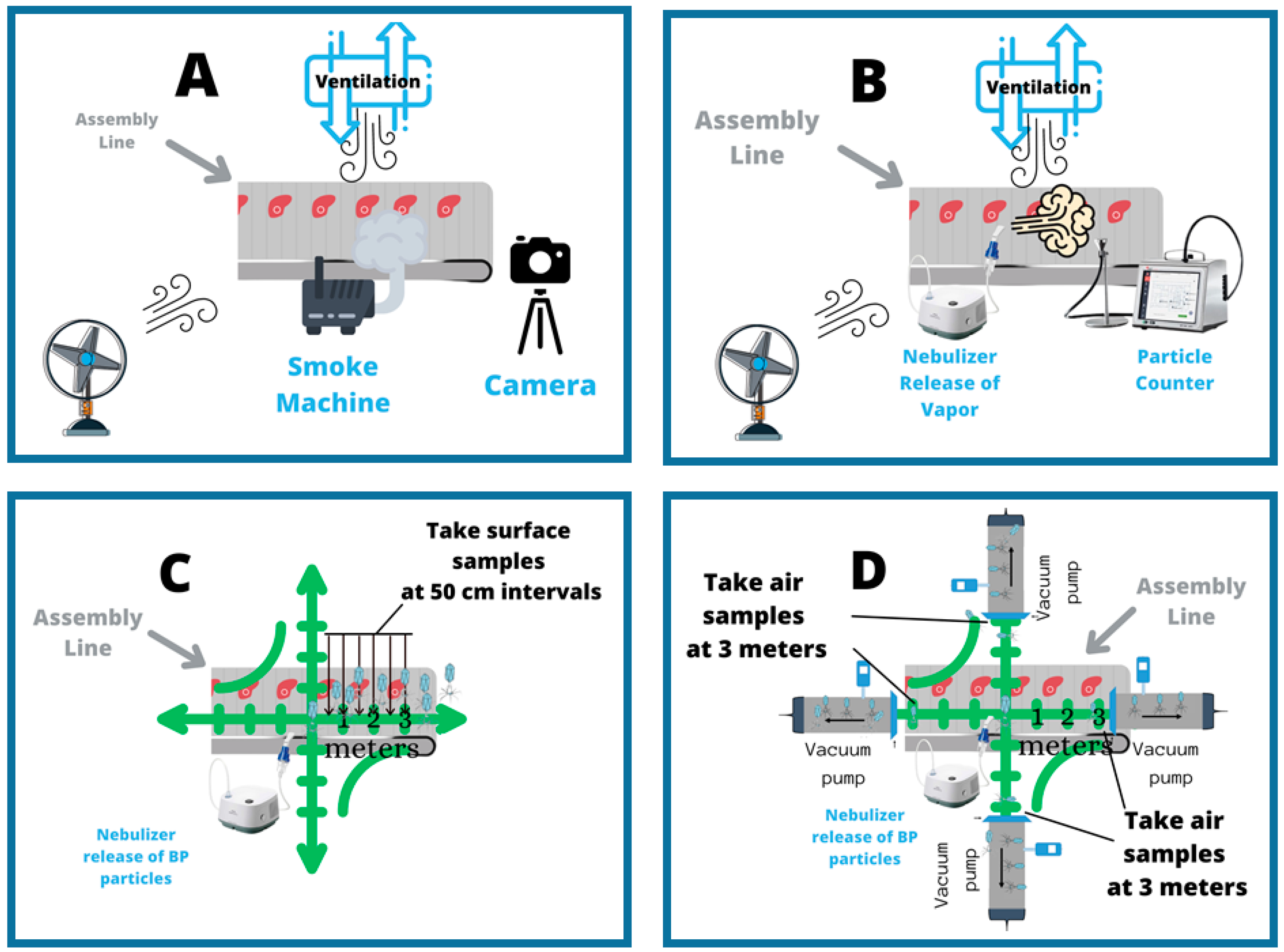
2. An Airborne Virus Model of Food Safety
3. Proposal for an AVT Model Facility
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Crews, J. Tyson Confirms Hundreds of COVID-19 Cases at Missouri Chicken Plant. Meat + Poultry. 29 June 2020. Available online: https://www.meatpoultry.com/articles/23379-tyson-confirms-hundreds-of-covid-19-cases-at-missouri-chicken-plant (accessed on 11 February 2021).
- Taylor, C.A.; Boulos, C.; Almond, D. Livestock plants and COVID-19 transmission. Proc. Natl. Acad. Sci. USA 2020, 117, 31706–31715. [Google Scholar] [CrossRef] [PubMed]
- Masotti, F.; Cattaneo, S.; Stuknytė, M.; Pica, V.; De Noni, I. Transmission routes, preventive measures and control strategies of SARS-CoV-2 in the food factory. Crit. Rev. Food Sci. Nutr. 2021. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, R.D.S. COVID-19 Meat Plant Closures. Meat + Poultry. 2020. Available online: https://www.meatpoultry.com/articles/22993-covid-19-meat-plant-map (accessed on 11 February 2021).
- Leclerc, Q.J.; Fuller, N.M.; Knight, L.E.; Funk, S.; Knight, G.M. What settings have been linked to SARS-CoV-2 transmission clusters? US Natl. Libr. Med. 2020, 5, 83. [Google Scholar] [CrossRef]
- Cheboi, P.K.; Siddiqui, S.A.; Onyando, J.; Kiptum, C.K.; Heinz, V. Effect of Ploughing Techniques on Water Use and Yield of Rice in Maugo Small-Holder Irrigation Scheme, Kenya. AgriEngineering 2021, 3, 110–117. [Google Scholar] [CrossRef]
- Salins, S.S.; Siddiqui, S.A.; Reddy, S.V.K.; Kumar, S. Parametric Analysis for Varying Packing Materials & Water Temper-atures in a Humidifier. Int. Conf. Fluid Flow Heat Mass Transf. 2020, 196-1–196–11. [Google Scholar] [CrossRef]
- Shoup, M. Frontline Food Industry Workers Prioritized for Next Phase of COVID-19 Vaccination, 21st of December 2020. Available online: https://www.foodnavigator-usa.com/article/2020/12/21/frontline-food-industry-workers-prioritized-for-next-phase-of-covid-19-vaccination (accessed on 11 February 2021).
- MacDonald, J.O.; Kenneth, K.E.; Handy, C.R. Consolidation in U.S. Meatpacking; Food and Rural Economics Division, Economic Research Service, U.S. Department of Agriculture: Washington, DC, USA, 2020.
- Fremstad, S.R.H.J.; Brown, H. Meatpacking Workers are a Diverse Group Who Need Better Protections Center for Economic and Policy Research. 2020. Available online: https://cepr.net/meatpacking-workers-are-a-diverse-group-who-need-better-protections/ (accessed on 12 February 2021).
- Yao, M.; Zhang, L.; Ma, J.; Zhou, L. On airborne transmission and control of SARS-CoV-2. Sci. Total Environ. 2020, 731. [Google Scholar] [CrossRef] [PubMed]
- Mayer, J. How Trump is Helping Tycoons Exploit the Pandemic. 2020. Available online: https://www.newyorker.com/magazine/2020/07/20/how-trump-is-helping-tycoons-exploit-the-pandemic (accessed on 11 February 2021).
- Durand-Moreau, Q.A.A.; Mackenzie, G.; Bowley, J.; Straube, S.; Chan, X.H.; Zelyas, N.; Greenhalgh, T. COVID-19 in Meat and Poultry Facilities: A Rapid Review and Lay Media Analysis 2020. Available online: https://www.cebm.net/covid-19/what-explains-the-high-rate-of-sars-cov-2-transmission-in-meat-and-poultry-facilities-2/ (accessed on 12 February 2021).
- WHO. The Best Time to Prevent the Next Pandemic Is Now: Countries Join Voices for Better Emergency Preparedness; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/news/item/01-10-2020-the-best-time-to-prevent-the-next-pandemic-is-now-countries-join-voices-for-better-emergency-preparedness (accessed on 21 February 2021).
- Centers for Disease Control and Prevention. Interim Guidance from CDC and the Occupational Safety and Health Administration (OSHA): Meat and Poultry Processing Workers and Employers. Available online: https://www.cdc.gov/coronavirus/2019-ncov/community/organizations/meat-poultry-processing-workers-employers.html (accessed on 18 May 2020).
- Nagdalian, A.A.; Rzhepakovsky, I.V.; Siddiqui, S.A.; Piskov, S.I.; Oboturova, N.P.; Timchenko, L.D.; Lodygin, A.D.; Blinov, A.V.; Ibrahim, S.A. Analysis of the Content of Mechanically Separated Poultry Meat in Sausage Using Computing Microtomography. J. Food Compos. Anal. 2021, 100, 103918. [Google Scholar] [CrossRef]
- Pimentel, D.; Whitecraft, M.; Scott, Z.R.; Zhao, L.; Satkiewicz, P.; Scott, T.J.; Phillips, J.; Szimak, D.; Singh, G.; Gonzalez, D.O.; et al. Will Limited Land, Water, and Energy Control Human Population Numbers in the Future? Hum. Ecol. 2010, 38, 599–611. [Google Scholar] [CrossRef]
- GPMB. The World at Risk: Annual Report on Global Preparedness for Health Emergencies; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Repko, M.; The Meat Supply Chain is Broken. Here’s Why Shortages are likely to Last during the Coronavirus Pandemic. CNBC. 7 May 2020. Available online: https://www.cnbc.com/2020/05/07/heres-why-meat-shortages-are-likely-to-last-during-the-pandemic.html (accessed on 31 December 2020).
- Skerritt, J.; Shanker, D.; Hirtzer, M. Meat Shortages Reopen Costly Path to Smaller U.S. Plants. Bloom. Bus. 2020. Available online: https://www.bloomberg.com/news/articles/2020-06-26/meat-shortages-reopen-costly-path-to-small-u-s-slaughterhouses (accessed on 31 December 2020).
- Huff, A.G.; Beyeler, W.E.; Kelley, N.S.; McNitt, J.A. How resilient is the United States’ food system to pandemics? J. Environ. Stud. Sci. 2015, 5, 337–347. [Google Scholar] [CrossRef]
- Günther, T.; Czech-Sioli, M.; Indenbirken, D.; Robitaille, A.; Tenhaken, P.; Exner, M.; Ottinger, M.; Fischer, N.; Grundhoff, A.; Brinkmann, M.M. SARS-CoV-2 outbreak investigation in a German meat processing plant. EMBO Mol. Med. 2020, 12, e13296. [Google Scholar] [CrossRef]
- Siddiqui, S.A.; Ahmad, A. Implementation of Thin-Walled Approximation to Evaluate Properties of Complex Steel Sec-tions Using C++. SN Comput. Sci. 2020, 1, 342. [Google Scholar] [CrossRef]
- Siddiqui, S.A.; Ahmad, A. Implementation of Newton’s Algorithm Using FORTRAN. SN Comput. Sci. 2020, 1, 348. [Google Scholar] [CrossRef]
- Swanson, A.Y.-B.D. Trump Declares Meat Supply ‘Critical,’ Aiming to Reopen Plants. The New York Times. 28 April 2020. Available online: https://www.nytimes.com/2020/04/28/business/economy/coronavirus-trump-meat-food-supply.html (accessed on 11 February 2021).
- Abott, C. CORONAVIRUS OUTBREAKS AT TWO CALIFORNIA CHICKEN PLANTS. Successful Farming. 8 December 2020. Available online: https://www.agriculture.com/news/business/coronavirus-outbreaks-at-two-california-chicken-plants (accessed on 11 February 2021).
- Baka, A.; Cenciarelli, O.; Kinross, P.; Penttinen, P.; Plachouras, D.; Semenza, J.; Suetens, C.; Weist, K. Heating, Ventilation and Air-Conditioning Systems in the Context of COVID-19; ECDC: Stolkholm, Sweden, 2020; Available online: https://www.ecdc.europa.eu/en/publications-data/heating-ventilation-air-conditioning-systems-covid-19 (accessed on 13 March 2021).
- EC (2004) Regulation (EC) No 852/2004 of the European Parliament and of the Council. Off. J. Eur. Union. 2004. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32004R0852&from=EN (accessed on 11 February 2021).
- Waltenburg, M. Coronavirus Disease among Workers in Food Processing, Food Manufacturing, and Agriculture Workplaces Center for Disease Control-Dispatch. 2020. Available online: https://wwwnc.cdc.gov/eid/article/27/1/20-3821_article (accessed on 31 December 2020).
- Gibb, R.; Redding, D.W.; Chin, K.Q.; Donnelly, C.A.; Blackburn, T.M.; Newbold, T.; Jones, K.E. Zoonotic host diversity increases in human-dominated ecosystems. Nature 2020, 584, 398–402. [Google Scholar] [CrossRef] [PubMed]
- Dyal, J. COVID-19 among Workers in Meat and Poultry Processing Facilities―19 States, April 2020. In Morbidity and Mortality Weekly Report (MMWR); Center for Disease Control: Atlenta, GA, USA, 2020. [Google Scholar]
- Sampath, S.S.; M, C.P.S.; Shetty, S. DETERMINATION OF POWER INHYDROELECTRIC PLANT DRIVEN BY HYDRAM: A PERPETUAL MOTION MACHINE TYPE 1. Int. J. Multidiscip. Res. Modern Educ. 2015, I, 115–122. [Google Scholar]
- Suranjan Salins, S.; Anusha Siddiqui, S.; Reddy, S.V.K.; Kumar, S. Experimental Investigation on the Performance Parameters of a Helical Coil Dehumidifier Test Rig. Energy Sources, Part A Recover. Util. Environ. Eff. 2021, 43, 35–53. [Google Scholar] [CrossRef]
- Bischoff, W.; Russell, G.; Willard, E.; Stehle, J. Impact of a novel mobile high-efficiency particulate air–ultraviolet air recirculation system on the bacterial air burden during routine care. Am. J. Infect. Control 2019, 47, 1025–1027. [Google Scholar] [CrossRef] [PubMed]
- Bischoff, W.E.; Swett, K.; Leng, I.; Peters, T.R. Exposure to Influenza Virus Aerosols During Routine Patient Care. J. Infect. Dis. 2013, 207, 1037–1046. [Google Scholar] [CrossRef] [PubMed]
- WHO. Recommendation to Member States to Improve Hand Hygiene Practices Widely to Help Prevent the Transmission of the COVID-19. World Health Organization: Geneva, Switzerland, 2020. Available online: https://www.who.int/docs/default-source/inaugural-who-partners-forum/who-interim-recommendation-on-obligatory-hand-hygiene-against-transmission-of-covid-19.pdf (accessed on 31 December 2020).
- Eykelbosh, A. Physical Barriers for COVID-19 Infection Prevention and Control in Commercial Settings; National Collaborating Center for Environmental Health: Vancouver, BC, Canada, 2020. [Google Scholar]
- Han, J.; Zhang, X.; He, S.; Jia, P. Can the coronavirus disease be transmitted from food? A review of evidence, risks, policies and knowledge gaps. Environ. Chem. Lett. 2020, 19, 5–16. [Google Scholar] [CrossRef] [PubMed]
- KSU. Grant Supports Research to Mitigate COVID-19 in Meat and Poultry Processing Facilities K-State News. 11 September 2020. Available online: https://www.k-state.edu/media/newsreleases/2020-09/covid-meat-processing91420.html (accessed on 11 January 2021).
- Nelson, C.C.; Baker, M.G.; Peckham, T.K.; Seixas, N.S. Estimating the burden of United States workers exposed to infection or disease: A key factor in containing risk of COVID-19 infection. PLoS ONE 2020, 15, e0232452. [Google Scholar]
- Zuber, S.; Brüssow, H. COVID 19: Challenges for virologists in the food industry. Microb. Biotechnol. 2020, 13, 1689–1701. [Google Scholar] [CrossRef] [PubMed]
- Samara, F.; Badran, R.; Dalibalta, S. Are Disinfectants for the Prevention and Control of COVID-19 Safe? Health Secur. 2020, 18, 496–498. [Google Scholar] [CrossRef]
- Zhao, L.; Qi, Y.; Luzzatto-Fegiz, P.; Cui, Y.; Zhu, Y. COVID-19: Effects of Environmental Conditions on the Propagation of Respiratory Droplets. Nano Lett. 2020, 20, 7744–7750. [Google Scholar] [CrossRef]
- Inagaki, H.; Saito, A.; Sugiyama, H.; Okabayashi, T.; Fujimoto, S. Rapid inactivation of SARS-CoV-2 with deep-UV LED irradiation. Emerg. Microbes Infect. 2020, 9, 1744–1747. [Google Scholar] [CrossRef] [PubMed]
- Fernstrom, A.; Goldblatt, M. Aerobiology and Its Role in the Transmission of Infectious Diseases. J. Pathog. 2013, 2013, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Pottage, T.; Richardson, C.; Parks, S.; Walker, J.T.; Bennett, A.M. Evaluation of hydrogen peroxide gaseous disinfection systems to decontaminate viruses. J. Hosp. Infect. 2007, 74, 55–61. [Google Scholar] [CrossRef] [PubMed]
- WHO. Considerations for Public Health and Social Measures in the Workplace in the Context of COVID-19; World Health Organization: Geneva, Switzerland, 2020; Available online: https://apps.who.int/iris/handle/10665/332050 (accessed on 13 March 2021).
- Siddiqui, S.A.; Ahmad, A. Dynamic Analysis of an Observation Tower Subjected to Wind Loads Using ANSYS. In Proceedings of the 2nd International Conference on Computation, Automation and Knowledge Management (ICCAKM), Dubai, UAE, 19–21 January 2021; pp. 6–11. [Google Scholar] [CrossRef]
- Siddiqui, S.; Sampath, S.S.; M, C.P.S. Determination of Endurance limit and stresses in grooved mild steel. In Proceedings of the 9th International Conference on Latest Trends in Engineering and Technology (ICLTET’2016), Abu Dhabi, UAE, 13–14 October 2016; IIENG: Abu Dhabi, UAE, 2016; pp. 10–15. [Google Scholar]

| Installation | Country | Locality | Date Published/Accessed | Total Number of Cases Per Cluster | Final Attack Rate |
|---|---|---|---|---|---|
| Cedar Meats Australia | Australia | Melbourne | 22 May 2020 | 67 | |
| Vegetable processing plant | Canada | Oppenheimer Group, Coquitlam, B.C. | 16 May 2020 | 3 | |
| Poultry | Canada | Coquitlam | 29 April 2020 | 50 | |
| Poultry plant | Canada | United Poultry, Canada | 08 May 2020 | 35 | |
| Westfleisch meat processing plant | Germany | North Rhine-Westphalia, Coesfeld | 08 May 2020 | 151 | |
| Meat processing plant | Germany | North Rhine-Westphalia, Oer-Erkenschwick | 08 May 2020 | 33 | 0.026 |
| Westcrown | Germany | Dissen | 21 May 2020 | 146 | |
| Fish factory | Ghana | Tema | 11 May 2020 | 534 | |
| Meat processing plant | Netherlands | Vion, Groenlo, The Netherlands | 22 May 2020 | 45 | |
| Meat processing plants | USA | South Dakota | 19 April 2020 | 518 | |
| Meat processing plants | USA | Iowa | 19 April 2020 | 84 | |
| Meat processing plants | USA | Iowa | 19 April 2020 | 177 | |
| Meat processing plant | Germany | Rheda-Wiedenbrück/Gütersloh | 20 June 2020 | 1029 | 0.158 |
| Chicken factory | UK | 2 Sisters in Llangefni, Anglesey | 25 June 2020 | 200 | 0.357 |
| Pladis biscuit factory | UK | Leicester | 25 June 2020 | 5 | |
| Kober meat factory | UK | Kirklees | 25 June 2020 | 165 | |
| Kepak meat factory | UK | Merthyr Tydfil | 25 June 2020 | 34 | |
| Rowan Foods meat factory | UK | Wrexham | 25 June 2020 | 70 | |
| Princes canned produce factory | UK | Wisbech | 25 June 2020 | 14 | 0.034 |
| Walkers crisps factory | UK | Leicester | 01 July 2020 | 28 | 0.02 |
| Tyson Poultry Processing | USA | Wilkes, North Carolina | 20 July 2020 | 570 | 0.254 |
| Risk Factor | Range Identified as High Risk | Sources |
|---|---|---|
| shift length | 8–12 h | [13] |
| prolonged close proximity | <6 feet, >15 min | [13] |
| not maintaining face covering | [13] | |
| shared work spaces | [13] | |
| shared transportation | [19] | |
| facility size | [26] | |
| assembly line speeds | High | [2] |
| relative humidity | 90–95% | [29] |
| airflow | recirculated and unfiltered, low exchange | [30] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zimmerman, T.; Siddiqui, S.A.; Bischoff, W.; Ibrahim, S.A. Tackling Airborne Virus Threats in the Food Industry: A Proactive Approach. Int. J. Environ. Res. Public Health 2021, 18, 4335. https://doi.org/10.3390/ijerph18084335
Zimmerman T, Siddiqui SA, Bischoff W, Ibrahim SA. Tackling Airborne Virus Threats in the Food Industry: A Proactive Approach. International Journal of Environmental Research and Public Health. 2021; 18(8):4335. https://doi.org/10.3390/ijerph18084335
Chicago/Turabian StyleZimmerman, Tahl, Shahida Anusha Siddiqui, Werner Bischoff, and Salam A. Ibrahim. 2021. "Tackling Airborne Virus Threats in the Food Industry: A Proactive Approach" International Journal of Environmental Research and Public Health 18, no. 8: 4335. https://doi.org/10.3390/ijerph18084335
APA StyleZimmerman, T., Siddiqui, S. A., Bischoff, W., & Ibrahim, S. A. (2021). Tackling Airborne Virus Threats in the Food Industry: A Proactive Approach. International Journal of Environmental Research and Public Health, 18(8), 4335. https://doi.org/10.3390/ijerph18084335







