Effects of a Rehabilitation Programme Using a Nasal Inspiratory Restriction Device in COPD
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Size Calculation
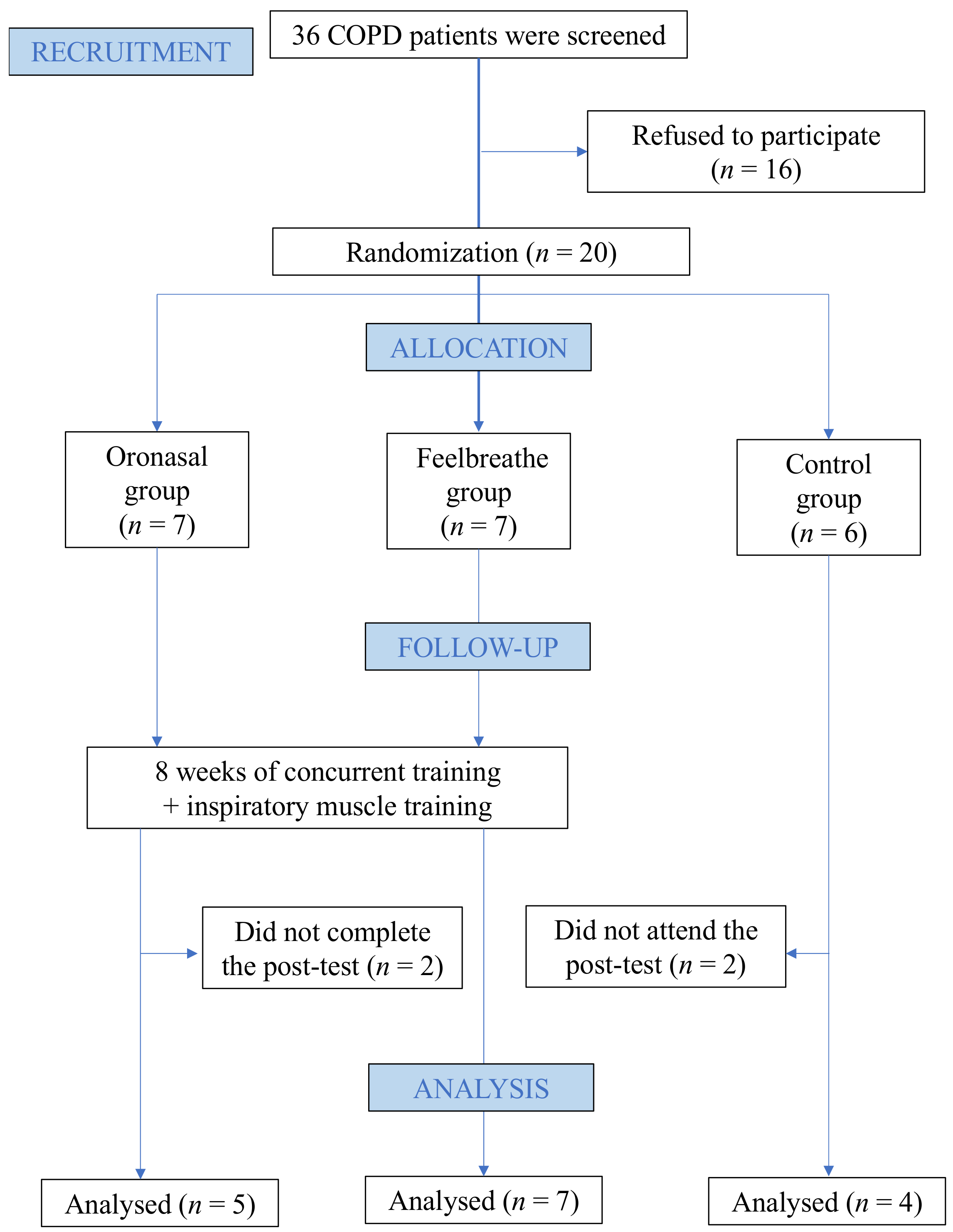
2.2. Design
2.3. Participants
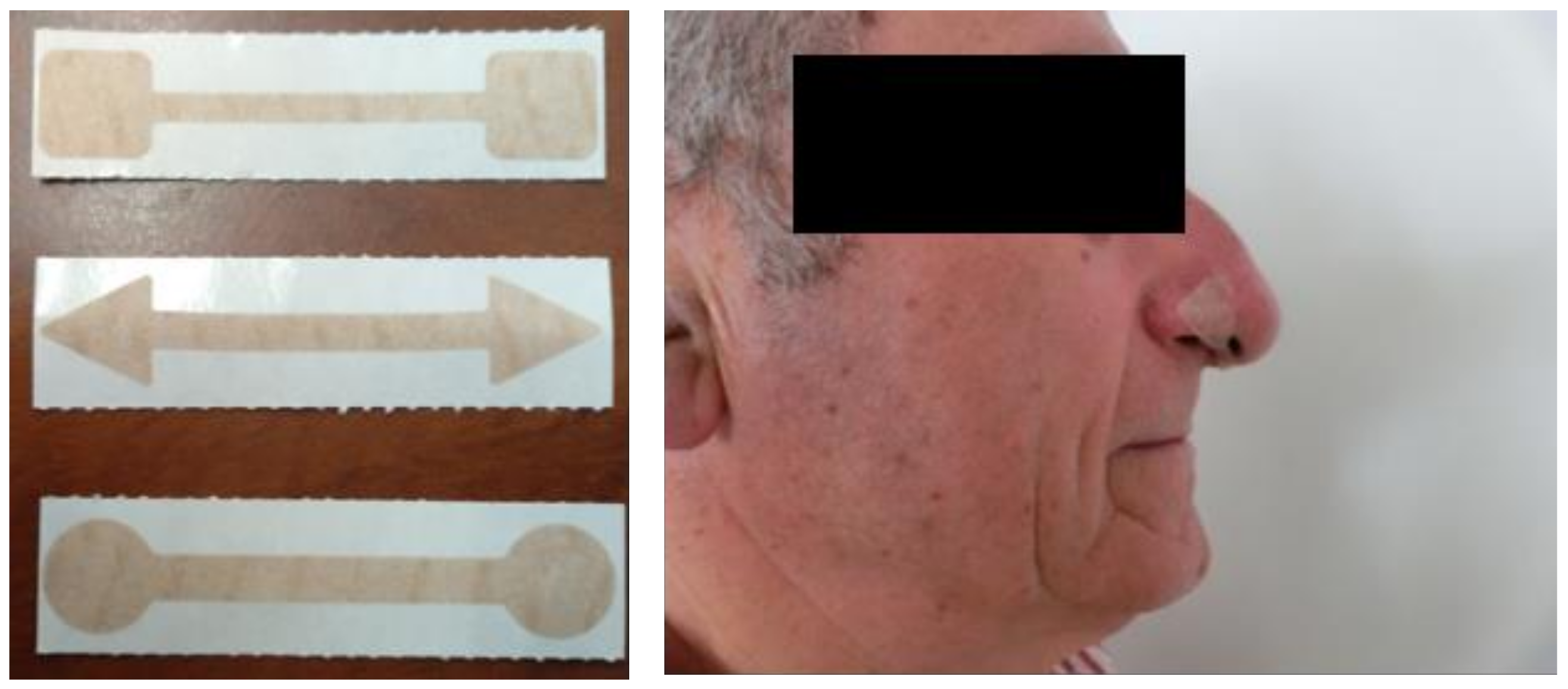
2.4. Training Programme
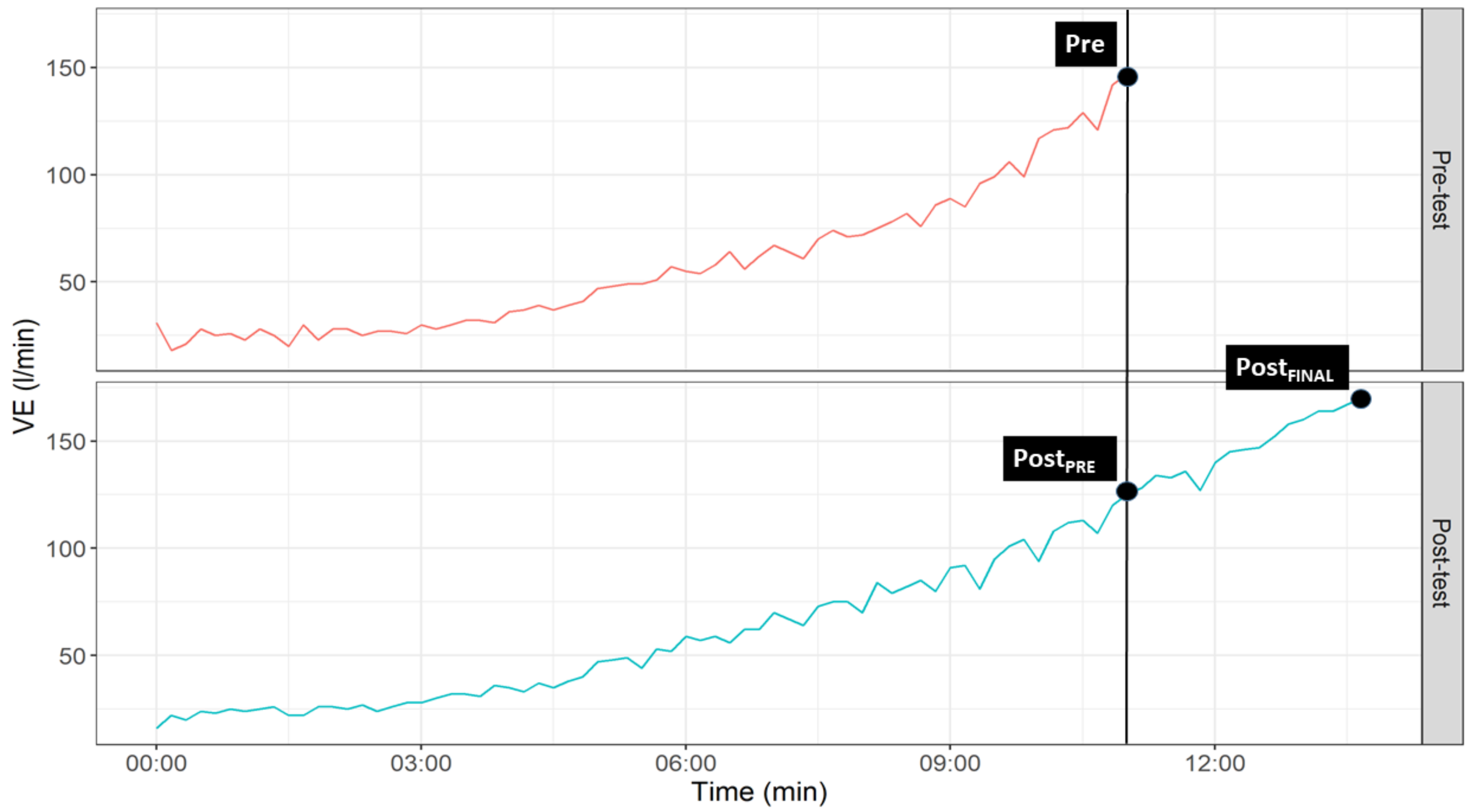
2.5. Cardiopulmonary Exercise Test
2.6. Statistical Analysis
3. Results
3.1. Descriptive Characteristics
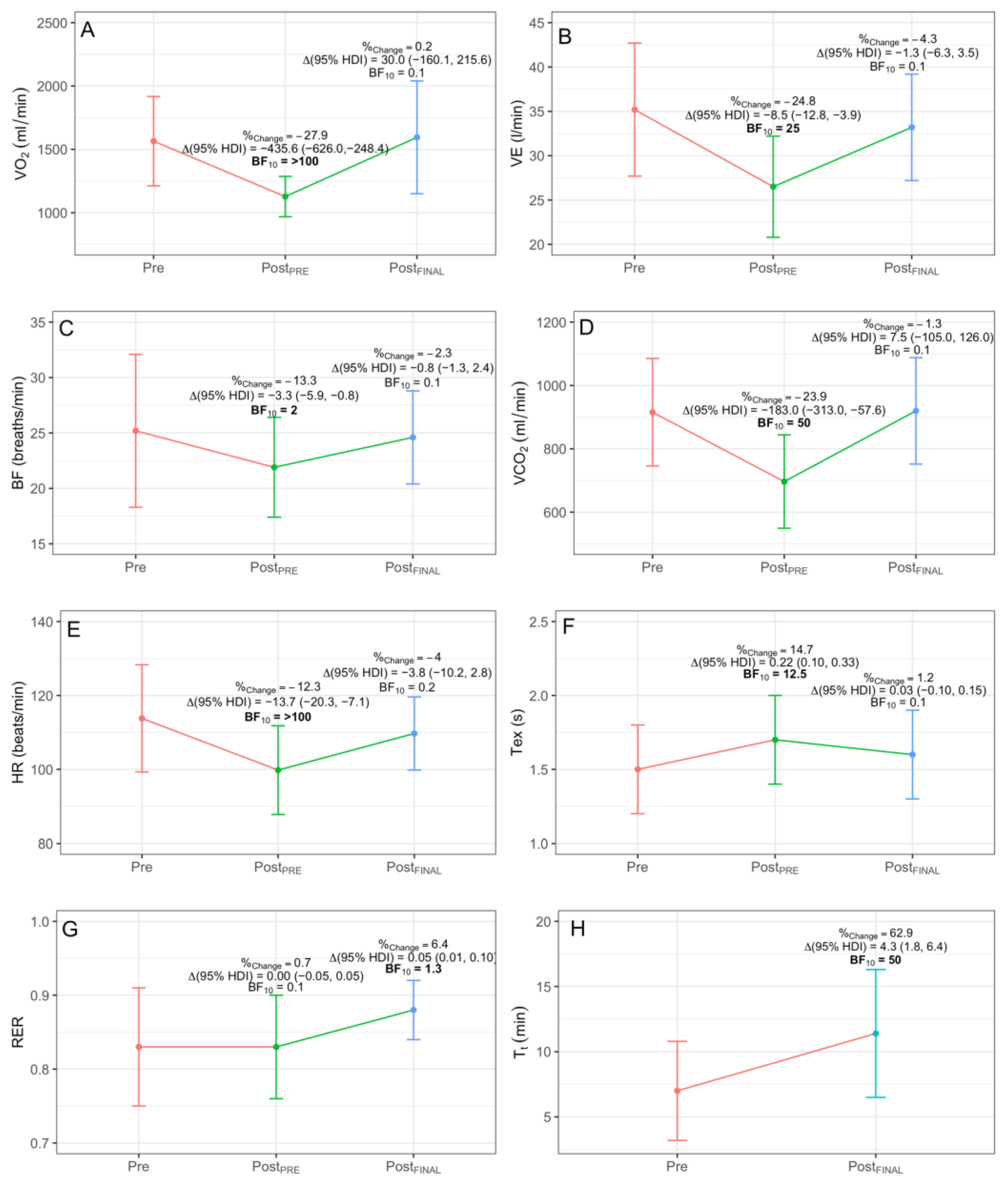
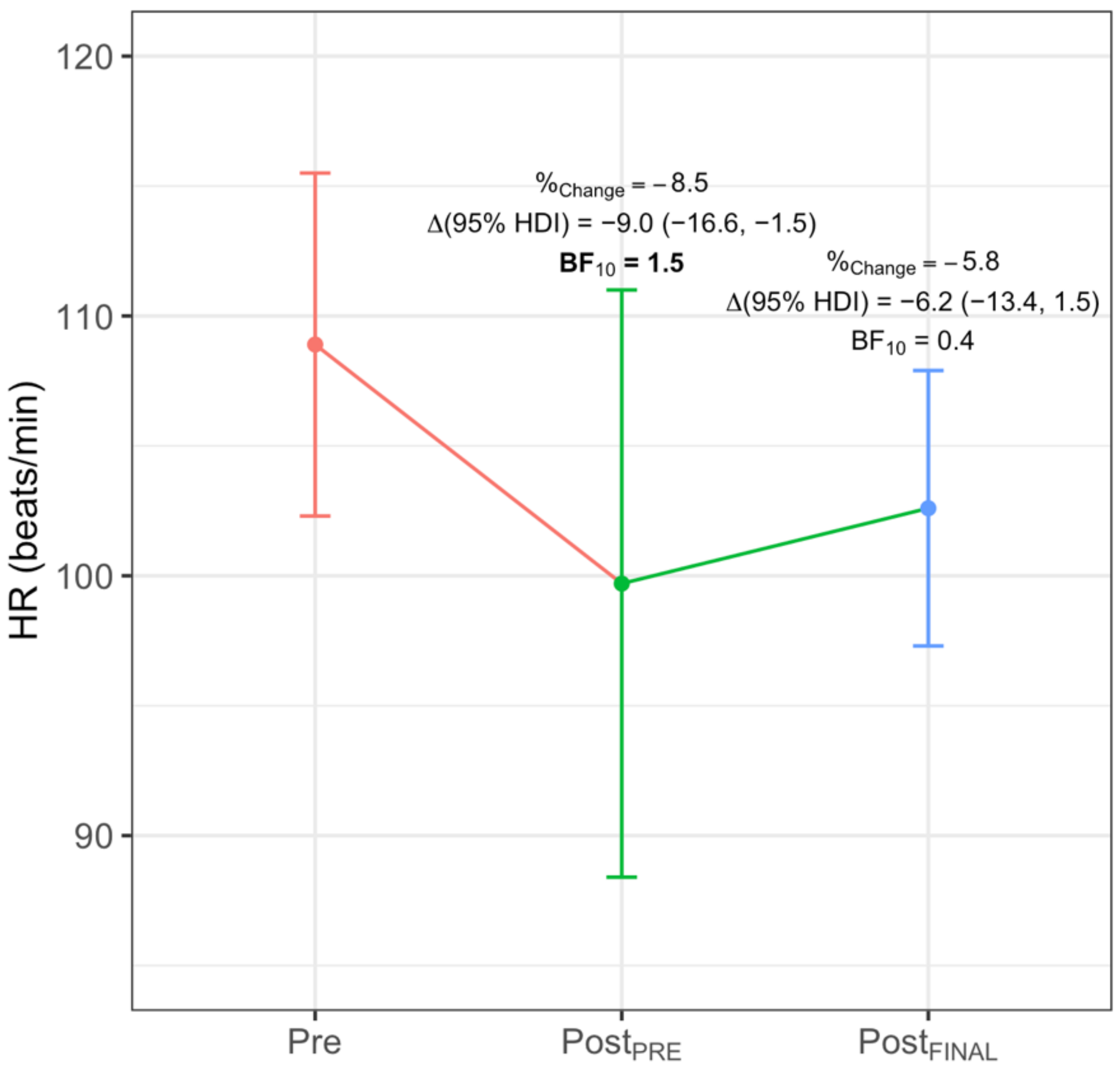
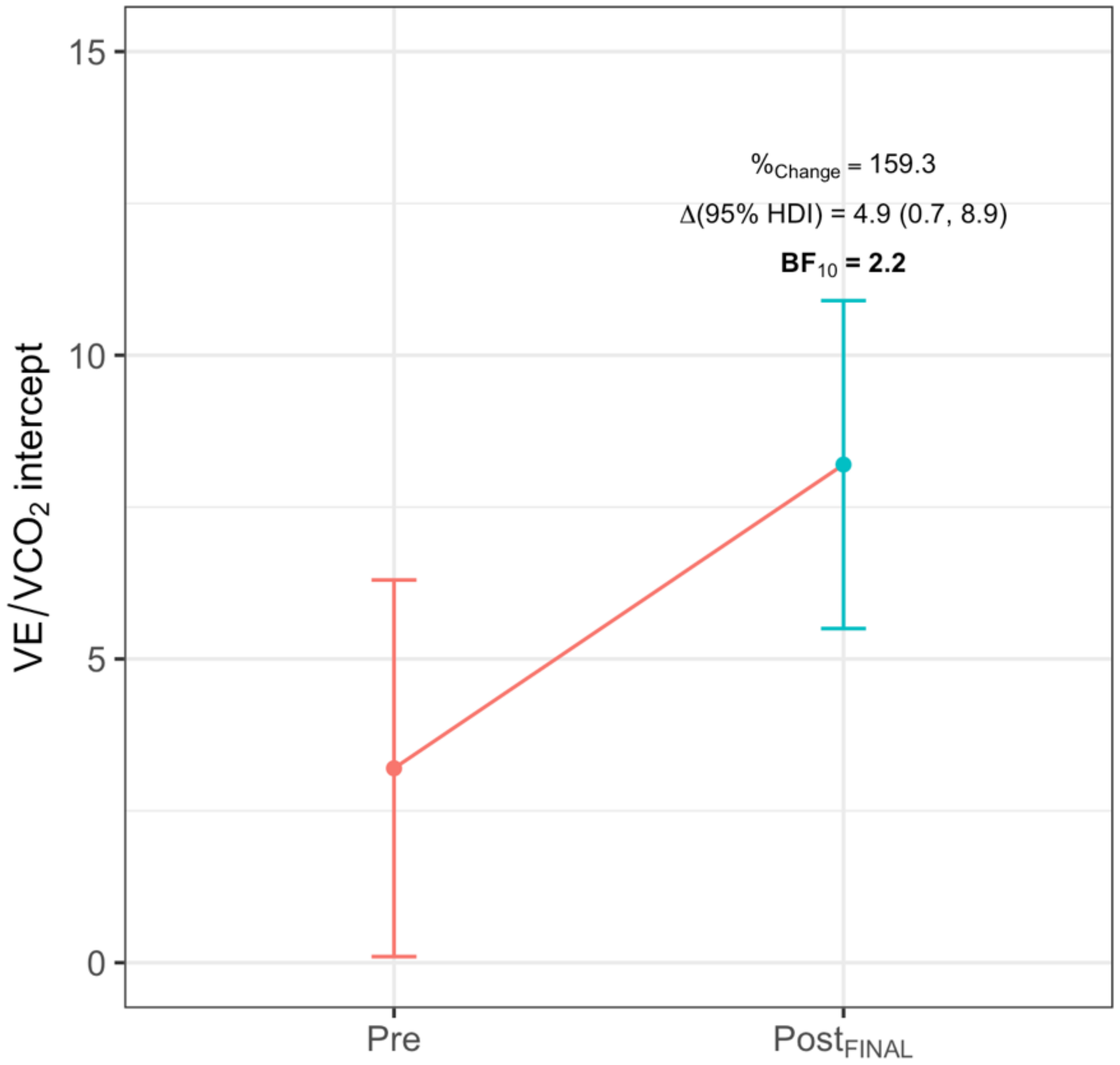
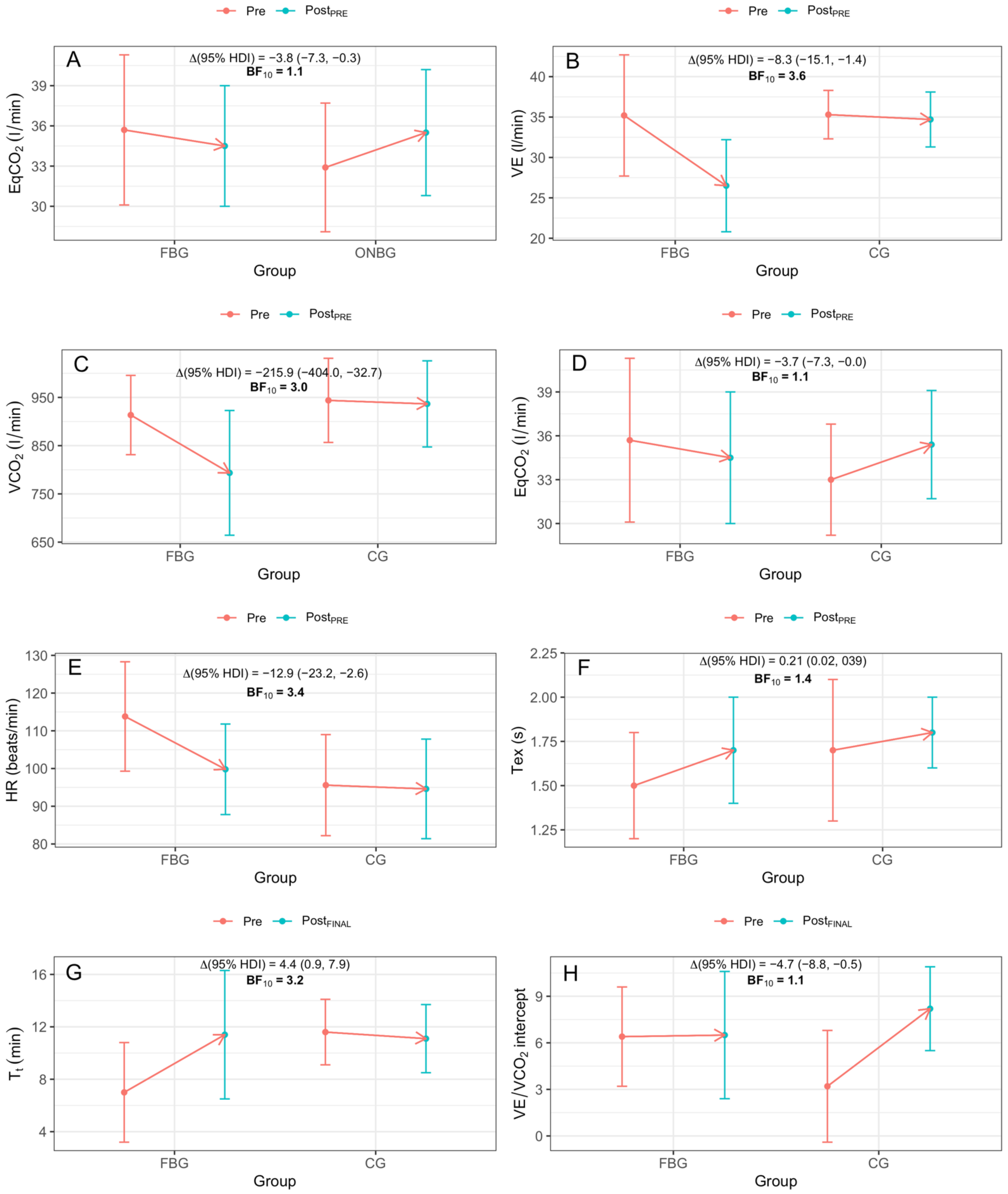
3.2. Intra-Group Differences
3.3. Inter-Group Differences
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Rabe, K.F.; Watz, H. Chronic Obstructive Pulmonary Disease. Lancet 2017, 389, 1931–1940. [Google Scholar] [CrossRef]
- Vogelmeier, C.F.; Criner, G.J.; Martinez, F.J.; Anzueto, A.; Barnes, P.J.; Bourbeau, J.; Celli, B.R.; Chen, R.; Decramer, M.; Fabbri, L.M.; et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report. GOLD Executive Summary. Am. J. Respir. Crit. Care Med. 2017, 195, 557–582. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, B.; Casey, D.; Devane, D.; Murphy, K.; Murphy, E.; Lacasse, Y. Pulmonary Rehabilitation for Chronic Obstructive Pulmonary Disease. Cochrane Database Syst. Rev. 2015, CD003793. [Google Scholar] [CrossRef] [PubMed]
- Garvey, C.; Bayles, M.P.; Hamm, L.F.; Hill, K.; Holland, A.; Limberg, T.M.; Spruit, M.A. Pulmonary Rehabilitation Exercise Prescription in Chronic Obstructive Pulmonary Disease: Review of Selected Guidelines: An Official Statement from the American Association of Cardiovascular and Pulmonary Rehabilitation. J. Cardiopulm. Rehabil. Prev. 2016, 36, 75–83. [Google Scholar] [CrossRef]
- Gosselink, R.; De Vos, J.; van den Heuvel, S.P.; Segers, J.; Decramer, M.; Kwakkel, G. Impact of Inspiratory Muscle Training in Patients with COPD: What Is the Evidence? Eur. Respir. J. 2011, 37, 416–425. [Google Scholar] [CrossRef] [PubMed]
- Beaumont, M.; Forget, P.; Couturaud, F.; Reychler, G. Effects of Inspiratory Muscle Training in COPD Patients: A Systematic Review and Meta-Analysis. Clin. Respir. J. 2018, 12, 2178–2188. [Google Scholar] [CrossRef] [PubMed]
- Beaumont, M.; Mialon, P.; Le Ber, C.; Le Mevel, P.; Péran, L.; Meurisse, O.; Morelot-Panzini, C.; Dion, A.; Couturaud, F. Effects of Inspiratory Muscle Training on Dyspnoea in Severe COPD Patients during Pulmonary Rehabilitation: Controlled Randomised Trial. Eur. Respir. J. 2018, 51. [Google Scholar] [CrossRef] [PubMed]
- Schultz, K.; Jelusic, D.; Wittmann, M.; Krämer, B.; Huber, V.; Fuchs, S.; Lehbert, N.; Wingart, S.; Stojanovic, D.; Göhl, O.; et al. Inspiratory Muscle Training Does Not Improve Clinical Outcomes in 3-Week COPD Rehabilitation: Results from a Randomised Controlled Trial. Eur. Respir. J. 2018, 51. [Google Scholar] [CrossRef]
- Wang, K.; Zeng, G.-Q.; Li, R.; Luo, Y.-W.; Wang, M.; Hu, Y.-H.; Xu, W.-H.; Zhou, L.-Q.; Chen, R.-C.; Chen, X. Cycle Ergometer and Inspiratory Muscle Training Offer Modest Benefit Compared with Cycle Ergometer Alone: A Comprehensive Assessment in Stable COPD Patients. Int. J. Chron. Obstruct. Pulmon. Dis. 2017, 12, 2655–2668. [Google Scholar] [CrossRef]
- Shei, R.-J. Recent Advancements in Our Understanding of the Ergogenic Effect of Respiratory Muscle Training in Healthy Humans: A Systematic Review. J. Strength Cond. Res. 2018, 32, 2665–2676. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Montesinos, J.L.; Arnedillo, A.; Vaz-Pardal, C.; Fernandez-Santos, J.R. Dispositivo Para El Entrenamiento de La Musculatura Nasal. Utility model U201930922, 6 August 2019. Available online: https://consultas2.oepm.es/InvenesWeb/detalle?referencia=PCT/ES2020/070364 (accessed on 10 December 2020).
- Gonzalez-Montesinos, J.L.; Arnedillo, A.; Fernandez-Santos, J.R.; Vaz-Pardal, C.; García, P.A.; Castro-Piñero, J.; Ponce-González, J.G. A New Nasal Restriction Device Called FeelBreathe(®) Improves Breathing Patterns in Chronic Obstructive Pulmonary Disease Patients during Exercise. Int. J. Environ. Res. Public Health 2020, 17, 4876. [Google Scholar] [CrossRef]
- Arnedillo, A.; Gonzalez-Montesinos, J.L.; Fernandez-Santos, J.R.; Vaz-Pardal, C.; España-Domínguez, C.; Ponce-González, J.G.; Cuenca-García, M. Effects of a Rehabilitation Programme with a Nasal Inspiratory Restriction Device on Exercise Capacity and Quality of Life in COPD. Int. J. Environ. Res. Public Health 2020, 17, 3669. [Google Scholar] [CrossRef] [PubMed]
- Boutou, A.K.; Zafeiridis, A.; Pitsiou, G.; Dipla, K.; Kioumis, I.; Stanopoulos, I. Cardiopulmonary Exercise Testing in Chronic Obstructive Pulmonary Disease: An Update on Its Clinical Value and Applications. Clin. Physiol. Funct. Imaging 2020, 40, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Stringer, W.; Marciniuk, D. The Role of Cardiopulmonary Exercise Testing (CPET) in Pulmonary Rehabilitation (PR) of Chronic Obstructive Pulmonary Disease (COPD) Patients. COPD 2018, 15, 621–631. [Google Scholar] [CrossRef] [PubMed]
- Palange, P.; Ward, S.A.; Carlsen, K.-H.; Casaburi, R.; Gallagher, C.G.; Gosselink, R.; O’Donnell, D.E.; Puente-Maestu, L.; Schols, A.M.; Singh, S.; et al. Recommendations on the Use of Exercise Testing in Clinical Practice. Eur. Respir. J. 2007, 29, 185–209. [Google Scholar] [CrossRef]
- Radtke, T.; Crook, S.; Kaltsakas, G.; Louvaris, Z.; Berton, D.; Urquhart, D.S.; Kampouras, A.; Rabinovich, R.A.; Verges, S.; Kontopidis, D.; et al. ERS Statement on Standardisation of Cardiopulmonary Exercise Testing in Chronic Lung Diseases. Eur. Respir. Rev. 2019, 28. [Google Scholar] [CrossRef] [PubMed]
- Uschner, D.; Schindler, D.; Hilgers, R.-D.; Heussen, N. RandomizeR: An R Package for the Assessment and Implementation of Randomization in Clinical Trials. J. Stat. Softw. 2018, 1. [Google Scholar] [CrossRef]
- Bestall, J.C.; Paul, E.A.; Garrod, R.; Garnham, R.; Jones, P.W.; Wedzicha, J.A. Usefulness of the Medical Research Council (MRC) Dyspnoea Scale as a Measure of Disability in Patients with Chronic Obstructive Pulmonary Disease. Thorax 1999, 54, 581–586. [Google Scholar] [CrossRef]
- Gloeckl, R.; Marinov, B.; Pitta, F. Practical Recommendations for Exercise Training in Patients with COPD. Eur. Respir. Rev. 2013, 22, 178–186. [Google Scholar] [CrossRef]
- Borg, G.A. Psychophysical Bases of Perceived Exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Hsia, D.; Casaburi, R.; Pradhan, A.; Torres, E.; Porszasz, J. Physiological Responses to Linear Treadmill and Cycle Ergometer Exercise in COPD. Eur. Respir. J. 2009, 34, 605–615. [Google Scholar] [CrossRef] [PubMed]
- Holm, S.M.; Rodgers, W.; Haennel, R.G.; MacDonald, G.F.; Bryan, T.L.; Bhutani, M.; Wong, E.; Stickland, M.K. Effect of Modality on Cardiopulmonary Exercise Testing in Male and Female COPD Patients. Respir. Physiol. Neurobiol. 2014, 192, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Neder, J.A.; Berton, D.C.; Arbex, F.F.; Alencar, M.C.; Rocha, A.; Sperandio, P.A.; Palange, P.; O’Donnell, D.E. Physiological and Clinical Relevance of Exercise Ventilatory Efficiency in COPD. Eur. Respir. J. 2017, 49. [Google Scholar] [CrossRef]
- Neder, J.A.; Alharbi, A.; Berton, D.C.; Alencar, M.C.N.; Arbex, F.F.; Hirai, D.M.; Webb, K.A.; O’Donnell, D.E. Exercise Ventilatory Inefficiency Adds to Lung Function in Predicting Mortality in COPD. COPD 2016, 13, 416–424. [Google Scholar] [CrossRef] [PubMed]
- Phillips, D.B.; Collins, S.É.; Stickland, M.K. Measurement and Interpretation of Exercise Ventilatory Efficiency. Front. Physiol. 2020, 11, 659. [Google Scholar] [CrossRef]
- Gelman, A.; Simpson, D.; Betancourt, M. The Prior Can Generally Only Be Understood in the Context of the Likelihood. Entropy 2017, 19, 555. [Google Scholar] [CrossRef]
- Bürkner, P.-C. Brms: An R Package for Bayesian Multilevel Models Using Stan. J. Stat. Softw. 2017, 1. [Google Scholar] [CrossRef]
- Wagenmakers, E.-J.; Lodewyckx, T.; Kuriyal, H.; Grasman, R. Bayesian Hypothesis Testing for Psychologists: A Tutorial on the Savage-Dickey Method. Cogn. Psychol. 2010, 60, 158–189. [Google Scholar] [CrossRef] [PubMed]
- Calvert, L.D.; Singh, S.J.; Morgan, M.D.; Steiner, M.C. Exercise Induced Skeletal Muscle Metabolic Stress Is Reduced after Pulmonary Rehabilitation in COPD. Respir. Med. 2011, 105, 363–370. [Google Scholar] [CrossRef]
- Maltais, F.; LeBlanc, P.; Simard, C.; Jobin, J.; Bérubé, C.; Bruneau, J.; Carrier, L.; Belleau, R. Skeletal Muscle Adaptation to Endurance Training in Patients with Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 1996, 154, 442–447. [Google Scholar] [CrossRef] [PubMed]
- Casaburi, R.; Patessio, A.; Ioli, F.; Zanaboni, S.; Donner, C.F.; Wasserman, K. Reductions in Exercise Lactic Acidosis and Ventilation as a Result of Exercise Training in Patients with Obstructive Lung Disease. Am. Rev. Respir. Dis. 1991, 143, 9–18. [Google Scholar] [CrossRef]
- Güell Rous, M.R.; Díaz Lobato, S.; Rodríguez Trigo, G.; Morante Vélez, F.; San Miguel, M.; Cejudo, P.; Ortega Ruiz, F.; Muñoz, A.; Galdiz Iturri, J.B.; García, A.; et al. Pulmonary rehabilitation. Sociedad Española de Neumología y Cirugía Torácica (SEPAR). Arch. Bronconeumol. 2014, 50, 332–344. [Google Scholar] [CrossRef] [PubMed]
- Shei, R.-J.; Mickleborough, T.D. Unresolved Questions That Need to Be Addressed in Order to Maximize the Efficacy of Inspiratory Muscle Training. Phys. Ther. Sport 2019, 35, 97–98. [Google Scholar] [CrossRef]
- Shei, R.-J. Training Load Influences the Response to Inspiratory Muscle Training. J. Sports Sci. Med. 2020, 19, 772–773. [Google Scholar] [PubMed]
- Karsten, M.; Ribeiro, G.S.; Esquivel, M.S.; Matte, D.L. Maximizing the Effectiveness of Inspiratory Muscle Training in Sports Performance: A Current Challenge. Phys. Ther. Sport 2019, 36, 68–69. [Google Scholar] [CrossRef] [PubMed]
| Variables | FBG (n = 7) | ONBG (n = 5) | CG (n = 4) | FBG vs. ONBG | BF10 | FBG vs. CG | BF10 | ONBG vs. CG | BF10 |
|---|---|---|---|---|---|---|---|---|---|
| Age (years) | 65.0 ± 8.0 | 72.0 ± 7.4 | 70.2 ± 5.9 | −4.8 (−14.8, 6.2) | 0.1 | −6.6 (−15.5, 3.6) | 0.3 | 1.7 (−10.0, 12.9) | 0.1 |
| BMI (m/kg2) | 28.4 ± 4.2 | 26.8 ± 2.5 | 25.9 ± 2.1 | 1.5 (−2.4, 5.4) | 0.3 | 2.3 (−2.0, 6.3) | 0.2 | 0.8 (−3.6, 5.5) | 0.2 |
| FEV1 (mL) | 1571 ± 334 | 1608 ± 344 | 1812 ± 706 | −23.5 (−557, 469) | 0.1 | −218 (−760, 349) | 0.1 | 194 (−441, 773) | 0.1 |
| FEV1 (% predicted) | 46.9 ± 10.6 | 51.2 ± 9.8 | 52.6 ± 19.9 | −3.7 (−18.4, 11.1) | 0.1 | −5.4 (−21.6, 10.8) | 0.1 | −1.8 (−19.8, 16.1) | 0.1 |
| FVC (mL) | 2869 ± 298 | 2580 ± 577 | 3270 ± 474 | 283 (−260, 801) | 0.3 | −382 (−929, 207) | 0.1 | −665 (−1317, −22.9) | >100 |
| FVC (% predicted) | 63.9 ± 8.3 | 59.2 ± 10.0 | 67.1 ± 13.8 | 4.5 (−7.4, 17.1) | 0.3 | −3.1 (−15.9, 10.1) | 0.1 | −7.6 (−21.5, 7.7) | 0.3 |
| FEV/FVC (%) | 54.1 ± 6.9 | 62.6 ± 5.6 | 54.2 ± 14.7 | −8.1 (−18.7, 2.8) | 0.2 | 0.0 (−11.4, 11.4) | 0.1 | 8.1 (−4.2, 20.8) | 0.3 |
| PImax (mmHg) | 93.3 ± 19.1 | 85.6 ± 23.9 | 102.0 ± 14.9 | 7.9 (−15.6, 31.1) | 0.1 | −7.6 (−34.3, 17.3) | 0.2 | −15.5 (−42.8, 12.5) | 0.2 |
| CAT (score) | 9.7 ± 6.5 | 10.0 ± 4.5 | 6.8 ± 4.4 | −0.3 (−6.8, 6.4) | 0.1 | 2.7 (−3.8, 9.7) | 0.2 | 3.0 (−4.5, 10) | 0.1 |
| mMRC (score|%) | P(Y|FB) | P(Y|ONB) | P(Y|CG) | ||||||
| 0 | 0 (0%) | 0 (0%) | 0 (0%) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | |||
| 1 | 0 (0%) | 0 (0%) | 0 (0%) | 0.0 (0.0, 0.1) | 0.0 (0.0, 0.2) | 0.0 (0.0, 0.2) | |||
| 2 | 6 (85%) | 5 (100%) | 4 (100%) | 0.9 (0.6, 0.1) | 0.9 (0.7, 1.0) | 0.9 (0.7, 1.0) | |||
| 3 | 1 (15%) | 0 (0%) | 0 (0%) | 0.1 (0.0, 0.4) | 0.0 (0.0, 0.2) | 0.0 (0.0, 0.3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gonzalez-Montesinos, J.L.; Fernandez-Santos, J.R.; Vaz-Pardal, C.; Ponce-Gonzalez, J.G.; Marin-Galindo, A.; Arnedillo, A. Effects of a Rehabilitation Programme Using a Nasal Inspiratory Restriction Device in COPD. Int. J. Environ. Res. Public Health 2021, 18, 4207. https://doi.org/10.3390/ijerph18084207
Gonzalez-Montesinos JL, Fernandez-Santos JR, Vaz-Pardal C, Ponce-Gonzalez JG, Marin-Galindo A, Arnedillo A. Effects of a Rehabilitation Programme Using a Nasal Inspiratory Restriction Device in COPD. International Journal of Environmental Research and Public Health. 2021; 18(8):4207. https://doi.org/10.3390/ijerph18084207
Chicago/Turabian StyleGonzalez-Montesinos, Jose L., Jorge R. Fernandez-Santos, Carmen Vaz-Pardal, Jesus G. Ponce-Gonzalez, Alberto Marin-Galindo, and Aurelio Arnedillo. 2021. "Effects of a Rehabilitation Programme Using a Nasal Inspiratory Restriction Device in COPD" International Journal of Environmental Research and Public Health 18, no. 8: 4207. https://doi.org/10.3390/ijerph18084207
APA StyleGonzalez-Montesinos, J. L., Fernandez-Santos, J. R., Vaz-Pardal, C., Ponce-Gonzalez, J. G., Marin-Galindo, A., & Arnedillo, A. (2021). Effects of a Rehabilitation Programme Using a Nasal Inspiratory Restriction Device in COPD. International Journal of Environmental Research and Public Health, 18(8), 4207. https://doi.org/10.3390/ijerph18084207








