Patterns of Psychological Responses among the Public during the Early Phase of COVID-19: A Cross-Regional Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Measures
- the Brief Illness Perception Questionnaire (IPQ) items assessing the perceived consequences (“How much does COVID-19 affects your life?”), timeline (“How long do you think COVID-19 will continue?”), concern (“How much does COVID-19 worry you?”) and emotional responses toward COVID-19 (“How much does the pandemic COVID-19 affect you emotionally (e.g., makes you sad, angry, scared, worried”)? (4 items, 10-point Likert scale) [27];
- the measures assessing the perceived susceptibility (3 items, 6-point Likert scale) and severity of COVID-19 (3 items, 6-point Likert scale) in line with the principles of the Health Belief Model [28];
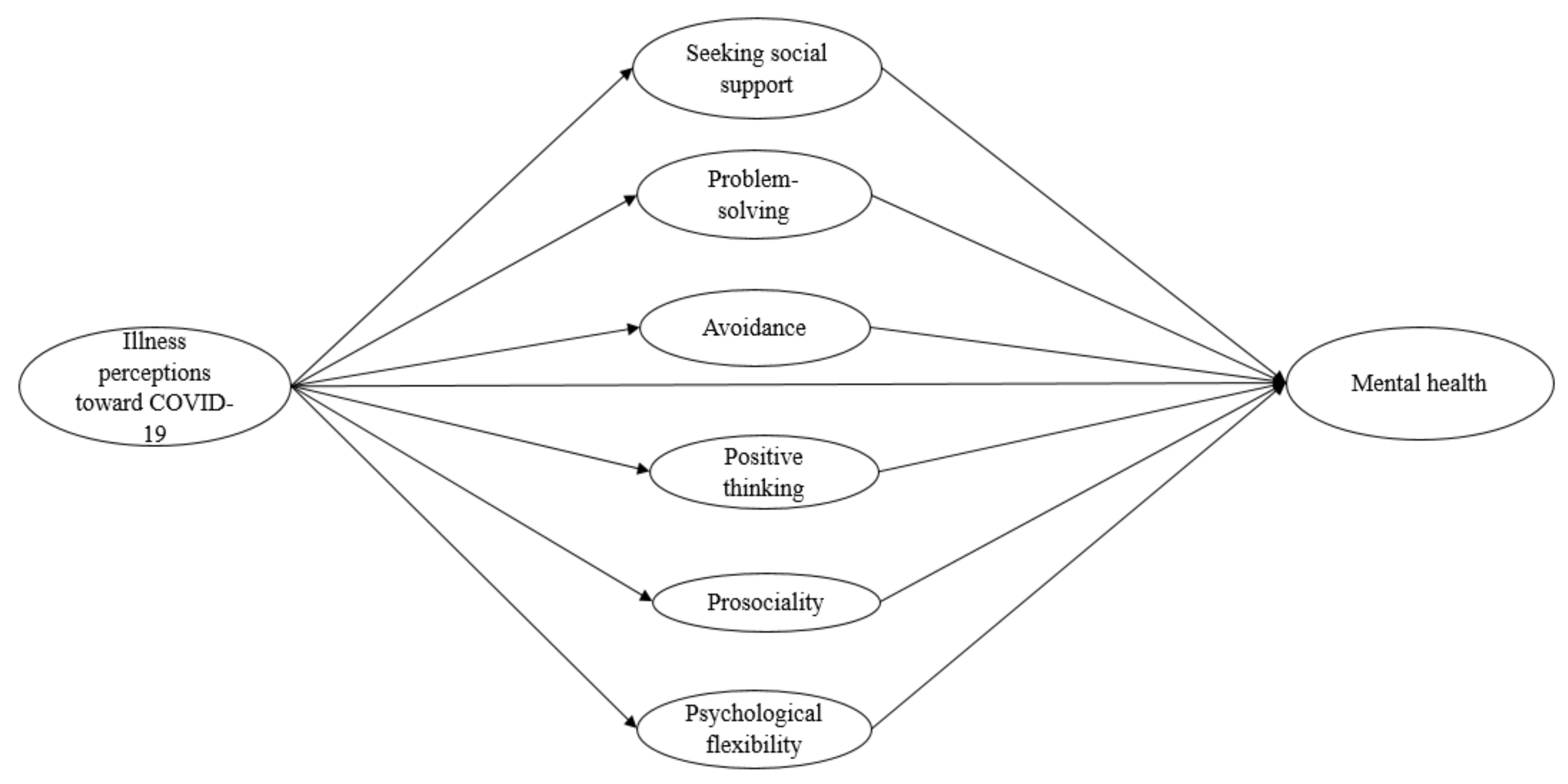
- the Brief Coping Orientation to Problems Experienced (Brief COPE) inventory composing of 28 items assessing a total of 14 coping strategies, which could be consolidated into four coping dimensions: seeking social support (venting, use of emotional support, use of instrumental support, religious belief); problem-solving (active coping, planning); avoidance (behavioral disengagement, self-distraction, substance use, denial, self-blaming) and positive thinking (humor, positive reframing, acceptance) [29,30,31];
- the Prosocialness Scale evaluating the level of prosocial behaviors, including sharing, helping, taking care of, and feeling empathic with others, which were carried out by the participant during the COVID-19 pandemic (6 items, 5-point Likert scale) [34].
2.3. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.2. Model Testing and Multiple-Group Structural Equation Model Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arora, T.; Grey, I.; Östlundh, L.; Lam, K.B.H.; Omar, O.M.; Arnone, D. The prevalence of psychological consequences of COVID-19: A systematic review and meta-analysis of observational studies. J. Health Psychol. 2020, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Jia, X.; Shi, H.; Niu, J.; Yin, X.; Xie, J.; Wang, X. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021, 281, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Asmundson, G.J.G.; Paluszek, M.M.; Landry, C.A.; Rachor, G.S.; McKay, D.; Taylor, S. Do pre-existing anxiety-related and mood disorders differentially impact COVID-19 stress responses and coping? J. Anxiety Disord. 2020, 74, 102271. [Google Scholar] [CrossRef] [PubMed]
- Krishnamoorthy, Y.; Nagarajan, R.; Saya, G.K.; Menon, V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2020, 293, 113382. [Google Scholar] [CrossRef]
- Cénat, J.M.; Blais-Rochette, C.; Kokou-Kpolou, C.K.; Noorishad, P.-G.; Mukunzi, J.N.; McIntee, S.-E.; Dalexis, R.D.; Goulet, M.-A.; Labelle, P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2021, 295, 113599. [Google Scholar] [CrossRef]
- Salari, N.; Khazaie, H.; Hosseinian-Far, A.; Khaledi-Paveh, B.; Kazeminia, M.; Mohammadi, M.; Shohaimi, S.; Daneshkhah, A.; Eskandari, S. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: A systematic review and meta-regression. Hum. Resour. Health 2020, 18, 100. [Google Scholar] [CrossRef]
- Muller, A.E.; Hafstad, E.V.; Himmels, J.P.W.; Smedslund, G.; Flottorp, S.; Stensland, S.Ø.; Stroobants, S.; Van de Velde, S.; Vist, G.E. The mental health impact of the Covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Res. 2020, 293, 113441. [Google Scholar] [CrossRef]
- Huberfeld, N.; Gordon, S.H.; Jones, D.K. Federalism complicates the response to the COVID-19 health and economic crisis: What can be done? J. Health Polit. Policy Law 2020, 45, 951–965. [Google Scholar] [CrossRef]
- Gordon, S.H.; Huberfeld, N.; Jones, D.K. What federalism means for the US response to coronavirus disease 2019. JAMA Health Forum 2020, 1, e200510. [Google Scholar] [CrossRef]
- Desson, Z.; Lambertz, L.; Peters, J.W.; Falkenbach, M.; Kauer, L. Europe’s Covid-19 outliers: German, Austrian and Swiss policy responses during the early stages of the 2020 pandemic. Health Policy Technol. 2020, 9, 405–418. [Google Scholar] [CrossRef]
- Han, E.; Tan, M.M.J.; Turk, E.; Sridhar, D.; Leung, G.M.; Shibuya, K.; Asgari, N.; Oh, J.; García-Basteiro, A.L.; Hanefeld, J.; et al. Lessons learnt from easing COVID-19 restrictions: An analysis of countries and regions in Asia Pacific and Europe. Lancet 2020, 396, 1525–1534. [Google Scholar] [CrossRef]
- Tso, R.V.; Cowling, B.J. Importance of Face Masks for COVID-19: A call for effective public education. Clin. Infec. Dis. 2020, 71, 2195–2198. [Google Scholar] [CrossRef]
- Allel, K.; Tapia-Muñoz, T.; Morris, W. Country-level factors associated with the early spread of COVID-19 cases at 5, 10 and 15 days since the onset. Glob. Public Health 2020, 15, 1589–1602. [Google Scholar] [CrossRef]
- Hagger, M.S.; Orbell, S. The common sense model of illness self-regulation: A conceptual review and proposed extended model. Health Psychol. Rev. 2021, 1–31. [Google Scholar] [CrossRef]
- Hagger, M.S.; Koch, S.; Chatzisarantis, N.L.D.; Orbell, S. The common sense model of self-regulation: Meta-analysis and test of a process model. Psychol. Bull. 2017, 143, 1117–1154. [Google Scholar] [CrossRef]
- Kashdan, T.B.; Rottenberg, J. Psychological flexibility as a fundamental aspect of health. Clin. Psychol. Rev. 2010, 30, 865–878. [Google Scholar] [CrossRef]
- Caprara, G.V.; Alessandri, G.; Eisenberg, N. Prosociality: The contribution of traits, values, and self-efficacy beliefs. J. Pers. Soc. Psychol. 2012, 102, 1289–1303. [Google Scholar] [CrossRef]
- Chong, Y.Y.; Chien, W.; Cheng, H.Y.; Kassianos, A.; Gloster, A.; Karekla, M. Can psychological flexibility and prosociality mitigate illness perceptions toward COVID-19 on mental health? A cross-sectional study among Hong Kong adults. Glob. Health 2021, 17, 43. [Google Scholar] [CrossRef]
- Adamson, M.M.; Phillips, A.; Seenivasan, S.; Martinez, J.; Grewal, H.; Kang, X.; Coetzee, J.; Luttenbacher, I.; Jester, A.; Harris, O.A.; et al. International prevalence and correlates of psychological stress during the global COVID-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 9248. [Google Scholar] [CrossRef]
- Faulkner, J.; O’Brien, W.J.; McGrane, B.; Wadsworth, D.; Batten, J.; Askew, C.D.; Badenhorst, C.; Byrd, E.; Coulter, M.; Draper, N.; et al. Physical activity, mental health and well-being of adults during initial COVID-19 containment strategies: A multi-country cross-sectional analysis. J. Sci. Med. Sport 2021, 24, 320–326. [Google Scholar] [CrossRef]
- Généreux, M.; Schluter, P.J.; Hung, K.K.C.; Wong, C.S.; Mok, C.P.Y.; O’sullivan, T.; David, M.D.; Carignan, M.-E.; Blouin-Genest, G.; Champagne-Poirier, O.; et al. One virus, four continents, eight countries: An interdisciplinary and international study on the psychosocial impacts of the covid-19 pandemic among adults. Int. J. Environ. Res. Public Health 2020, 17, 8390. [Google Scholar] [CrossRef] [PubMed]
- Bartoszek, A.; Walkowiak, D.; Bartoszek, A.; Kardas, G. Mental well-being (depression, loneliness, insomnia, daily life fatigue) during COVID-19 related home-confinement—A study from Poland. Int. J. Environ. Res. Public Health 2020, 17, 7417. [Google Scholar] [CrossRef] [PubMed]
- Gloster, A.T.; Lamnisos, D.; Lubenko, J.; Presti, G.; Squatrito, V.; Constantinou, M.; Nicolaou, C.; Papacostas, S.; Aydin, G.; Chong, Y.Y.; et al. Impact of COVID-19 pandemic on mental health: An international study. PLoS ONE 2020, 15, e0244809. [Google Scholar] [CrossRef] [PubMed]
- Chong, Y.Y.; Chien, W.T.; Cheng, H.Y.; Chow, K.M.; Kassianos, A.P.; Karekla, M.; Gloster, A. The role of illness perceptions, coping, and self-efficacy on adherence to precautionary measures for COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 6540. [Google Scholar] [CrossRef] [PubMed]
- Lamers, S.M.A.; Westerhof, G.J.; Bohlmeijer, E.T.; Ten Klooster, P.M.; Keyes, C.L.M. Evaluating the psychometric properties of the Mental Health Continuum-Short Form (MHC-SF). J. Clin. Psychol. 2011, 67, 99–110. [Google Scholar] [CrossRef]
- Guo, C.; Tomson, G.; Guo, J.; Li, X.; Keller, C.; Söderqvist, F. Psychometric evaluation of the Mental Health Continuum-Short Form (MHC-SF) in Chinese adolescents—A methodological study. Health Qual. Life Outcomes 2015, 13, 198. [Google Scholar] [CrossRef] [PubMed]
- Broadbent, E.; Wilkes, C.; Koschwanez, H.; Weinman, J.; Norton, S.; Petrie, K.J. A systematic review and meta-analysis of the Brief Illness Perception Questionnaire. Health Psychol. 2015, 30, 1361–1385. [Google Scholar] [CrossRef]
- Rosenstock, I.M.; Strecher, V.J.; Becker, M.H. Social learning theory and the health belief model. Health Educ. Q. 1988, 15, 175–183. [Google Scholar] [CrossRef]
- Baumstarck, K.; Alessandrini, M.; Hamidou, Z.; Auquier, P.; Leroy, T.; Boyer, L. Assessment of coping: A new French four-factor structure of the brief COPE inventory. Health Qual. Life Outcomes 2017, 15, 8. [Google Scholar] [CrossRef]
- Chew, Q.H.; Chia, F.L.-A.; Ng, W.K.; Lee, W.C.I.; Tan, P.L.L.; Wong, C.S.; Puah, S.H.; Shelat, V.G.; Seah, E.-J.D.; Huey, C.W.T.; et al. Perceived stress, stigma, traumatic stress levels and coping responses amongst residents in training across multiple specialties during COVID-19 pandemic—A longitudinal study. Int. J. Environ. Res. Public Health 2020, 17, 6572. [Google Scholar] [CrossRef]
- Marguerite, S.; Laurent, B.; Marine, A.; Tanguy, L.; Karine, B.; Pascal, A.; Xavier, Z. Actor-partner interdependence analysis in depressed patient-caregiver dyads: Influence of emotional intelligence and coping strategies on anxiety and depression. Psychiatry Res. 2017, 258, 396–401. [Google Scholar] [CrossRef] [PubMed]
- Hayes, S.C. Acceptance and Commitment Therapy: The Process and Practice of Mindful Change, 2nd ed.; Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- Villanueva, J.; Meyer, A.H.; Rinner, M.T.B.; Firsching, V.J.; Benoy, C.; Brogli, S.; Walter, M.; Bader, K.; Gloster, A.T. “Choose change”: Design and methods of an acceptance and commitment therapy effectiveness trial for transdiagnostic treatment-resistant patients. BMC Psychiatry 2019, 19, 173. [Google Scholar] [CrossRef] [PubMed]
- Caprara, G.V.; Steca, P.; Zelli, A.; Capanna, C. A new scale for measuring adults’ prosocialness. Eur. J. Psychol. Assess. 2005, 21, 77–89. [Google Scholar] [CrossRef]
- Hale, T.; Petherick, A.; Phillips, T.; Webster, S. Variation in government responses to COVID-19. In Blavatnik School of Government Working Paper; University of Oxford: Oxford, UK, 2020; Volume 31, p. 2020-11. [Google Scholar]
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects 2019, Volume II: Demographic Profiles (ST/ESA/SER.A/427). 2019. Available online: https://population.un.org/wpp/Publications/Files/WPP2019_Volume-II-Demographic-Profiles.pdf (accessed on 20 March 2021).
- Pakenham, K.I.; Landi, G.; Boccolini, G.; Furlani, A.; Grandi, S.; Tossani, E. The moderating roles of psychological flexibility and inflexibility on the mental health impacts of COVID-19 pandemic and lockdown in Italy. J. Contextual Behav. Sci. 2020, 17, 109–118. [Google Scholar] [CrossRef]
- Dawson, D.L.; Golijani-Moghaddam, N. COVID-19: Psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. J. Contextual Behav. Sci. 2020, 17, 126–134. [Google Scholar] [CrossRef]
- McCracken, L.M.; Badinlou, F.; Buhrman, M.; Brocki, K.C. The role of psychological flexibility in the context of COVID-19: Associations with depression, anxiety, and insomnia. J. Contextual Behav. Sci. 2021, 19, 28–35. [Google Scholar] [CrossRef]
- Kroska, E.B.; Roche, A.I.; Adamowicz, J.L.; Stegall, M.S. Psychological flexibility in the context of COVID-19 adversity: Associations with distress. J. Contextual Behav. Sci. 2020, 18, 28–33. [Google Scholar] [CrossRef]
- Peltz, J.S.; Daks, J.S.; Rogge, R.D. Mediators of the association between COVID-19-related stressors and parents’ psychological flexibility and inflexibility: The roles of perceived sleep quality and energy. J. Contextual Behav. Sci. 2020, 17, 168–176. [Google Scholar] [CrossRef]
- Crasta, D.; Daks, J.S.; Rogge, R.D. Modeling suicide risk among parents during the COVID-19 pandemic: Psychological inflexibility exacerbates the impact of COVID-19 stressors on interpersonal risk factors for suicide. J. Contextual Behav. Sci. 2020, 18, 117–127. [Google Scholar] [CrossRef]
- Wielgus, B.; Urban, W.; Patriak, A.; Cichocki, Ł. Examining the associations between psychological flexibility, mindfulness, psychosomatic functioning, and anxiety during the COVID-19 pandemic: A path analysis. Int. J. Environ. Res. Public Health 2020, 17, 8764. [Google Scholar] [CrossRef]
- Daks, J.S.; Peltz, J.S.; Rogge, R.D. Psychological flexibility and inflexibility as sources of resiliency and risk during a pandemic: Modeling the cascade of COVID-19 stress on family systems with a contextual behavioral science lens. J. Contextual Behav. Sci. 2020, 18, 16–27. [Google Scholar] [CrossRef]
- Gloster, A.T.; Karekla, M. A multi-level, multi-method approach to testing and refining intervention targets. In Beyond the DSM; Hayes, S., Hofmann, S., Eds.; New Harbinger: Oakland, CA, USA, 2020. [Google Scholar]
- Ngan, H.Y.; Chong, Y.Y.; Chien, W.T. Effects of mindfulness- and acceptance-based interventions on diabetes distress and glycaemic level in people with type 2 diabetes: Systematic review and meta-analysis. Diabet. Med. 2021, e14525. [Google Scholar] [CrossRef]
- Li, H.; Wong, C.L.; Jin, X.; Chen, J.; Chong, Y.Y.; Bai, Y. Effects of Acceptance and Commitment Therapy on health-related outcomes for patients with advanced cancer: A systematic review. Int. J. Nurs. Stud. 2021, 115, 103876. [Google Scholar] [CrossRef]
- Gloster, A.T.; Walder, N.; Levin, M.E.; Twohig, M.P.; Karekla, M. The empirical status of acceptance and commitment therapy: A review of meta-analyses. J. Contextual Behav. Sci. 2020, 18, 181–192. [Google Scholar] [CrossRef]
- French, K.; Golijani-Moghaddam, N.; Schröder, T. What is the evidence for the efficacy of self-help acceptance and commitment therapy? A systematic review and meta-analysis. J. Contextual Behav. Sci. 2017, 6, 360–374. [Google Scholar] [CrossRef]
- Chong, Y.Y.; Cheng, H.Y.; Chan, H.Y.L.; Chien, W.T.; Wong, S.Y.S. COVID-19 pandemic, infodemic and the role of eHealth literacy. Int. J. Nurs. Stud. 2020, 108, 103644. [Google Scholar] [CrossRef]
- Biglan, A.; Johansson, M.; Van Ryzin, M.; Embry, D. Scaling up and scaling out: Consilience and the evolution of more nurturing societies. Clin. Psychol. Rev. 2020, 81, 101893. [Google Scholar] [CrossRef]
- Grey, I.; Arora, T.; Thomas, J.; Saneh, A.; Tohme, P.; Abi-Habib, R. The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry Res. 2020, 293, 113452. [Google Scholar] [CrossRef]
- Ye, Z.; Yang, X.; Zeng, C.; Wang, Y.; Shen, Z.; Li, X.; Lin, D. Resilience, social support, and coping as mediators between COVID-19-related stressful experiences and acute stress disorder among college students in China. Appl. Psychol. Health Well-Being 2020, 12, 1074–1094. [Google Scholar] [CrossRef]
- Saltzman, L.Y.; Hansel, T.C.; Bordnick, P.S. Loneliness, isolation, and social support factors in post-COVID-19 mental health. Psychol. Trauma 2020, 12, S55–S57. [Google Scholar] [CrossRef]
- Taylor, S.E. Social support: A review. In The Oxford Handbook of Health Psychology; Friedman, H.S., Ed.; Oxford University Press: Oxford, UK; New York, NY, USA, 2011. [Google Scholar]
- Bonavita, S.; Sparaco, M.; Russo, A.; Borriello, G.; Lavorgna, L. Perceived stress and social support in a large population of people with multiple sclerosis recruited online through the COVID-19 pandemic. Eur. J. Neurol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Luo, S.; Mu, W.; Li, Y.; Ye, L.; Zheng, X.; Xu, B.; Ding, Y.; Ling, P.; Zhou, M.; et al. Effects of sources of social support and resilience on the mental health of different age groups during the COVID-19 pandemic. BMC Psychiatry 2021, 21, 16. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.; Chen, C.-N.; Alegría, M. Contextualizing social support: Pathways to help seeking in Latinos, Asian Americans, and whites. J. Soc. Clin. Psychol. 2014, 33, 1–24. [Google Scholar] [CrossRef]
- Gloster, A.T.; Rinner, M.T.B.; Meyer, A.H. Increasing prosocial behavior and decreasing selfishness in the lab and everyday life. Sci. Rep. 2020, 10, 21220. [Google Scholar] [CrossRef]
- Laguna, M.; Mazur, Z.; Kędra, M.; Ostrowski, K. Interventions stimulating prosocial helping behavior: A systematic review. J. Appl. Soc. Psychol. 2020, 50, 676–696. [Google Scholar] [CrossRef]
- Raposa, E.B.; Laws, H.B.; Ansell, E.B. Prosocial behavior mitigates the negative effects of stress in everyday life. Clin. Psychol. Sci. 2016, 4, 691–698. [Google Scholar] [CrossRef]
- Preston, S.D. The origins of altruism in offspring care. Psychol. Bull. 2013, 139, 1305–1341. [Google Scholar] [CrossRef]
- Gilbert, P. Affiliative and prosocial motives and emotions in mental health. Dialogues Clin. Neurosci. 2015, 17, 381–389. [Google Scholar]
- Heffner, J.; Vives, M.-L.; FeldmanHall, O. Emotional responses to prosocial messages increase willingness to self-isolate during the COVID-19 pandemic. Personal. Individ. Differ. 2021, 170, 110420. [Google Scholar] [CrossRef]
- Szmyd, B.; Bartoszek, A.; Karuga, F.F.; Staniecka, K.; Błaszczyk, M.; Radek, M. Medical students and SARS-CoV-2 vaccination: Attitude and behaviors. Vaccines 2021, 9, 128. [Google Scholar] [CrossRef]
- Szmyd, B.; Karuga, F.F.; Bartoszek, A.; Staniecka, K.; Siwecka, N.; Bartoszek, A.; Błaszczyk, M.; Radek, M. Attitude and behaviors towards SARS-CoV-2 vaccination among healthcare workers: A cross-sectional study from Poland. Vaccines 2021, 9, 218. [Google Scholar] [CrossRef]
- Skinner, E.A.; Edge, K.; Altman, J.; Sherwood, H. Searching for the structure of coping: A review and critique of category systems for classifying ways of coping. Psychol. Bull. 2003, 129, 216–269. [Google Scholar] [CrossRef]
- Babore, A.; Lombardi, L.; Viceconti, M.L.; Pignataro, S.; Marino, V.; Crudele, M.; Candelori, C.; Bramanti, S.M.; Trumello, C. Psychological effects of the COVID-2019 pandemic: Perceived stress and coping strategies among healthcare professionals. Psychiatry Res. 2020, 293, 113366. [Google Scholar] [CrossRef]
- Agha, S. Mental well-being and association of the four factors coping structure model: A perspective of people living in lockdown during COVID-19. Ethics Med. Public Health 2021, 16, 100605. [Google Scholar] [CrossRef]
- Korkmaz, S.; Kazgan, A.; Çekiç, S.; Tartar, A.S.; Balcı, H.N.; Atmaca, M. The anxiety levels, quality of sleep and life and problem-solving skills in healthcare workers employed in COVID-19 services. J. Clin. Neurosci. 2020, 80, 131–136. [Google Scholar] [CrossRef]
- World Health Organization. The WHO Special Initiative for Mental Health (2019–2023): Universal Health Coverage for Mental Health. Available online: https://apps.who.int/iris/bitstream/handle/10665/310981/WHO-MSD-19.1-eng.pdf?sequence=1&isAllowed=y (accessed on 4 April 2021).
- Rosenberg, S.; Mendoza, J.; Tabatabaei-Jafari, H.; Salvador-Carulla, L. International experiences of the active period of COVID-19—Mental health care. Health Policy Technol. 2020, 9, 503–509. [Google Scholar] [CrossRef]
| Variables | All Regions a (n = 9130) | Eastern Asia—HK Only (n = 514) | Western Asia (n = 1657) | N. & S. America b (n = 753) | Northern Europe (n = 1956) | Western Europe (n = 1507) | Southern Europe (n = 1996) | Eastern Europe (n = 747) | χ2 (df) | p-Value |
|---|---|---|---|---|---|---|---|---|---|---|
| Gender, n (%) | ||||||||||
| Male | 2015 | 133 | 438 | 147 | 287 | 339 | 451 | 220 | 120.89 (12) | <0.001 |
| (22.1) | (25.9) | (26.4) | (19.5) | (14.7) | (22.5) | (22.6) | (29.5) | |||
| Female | 7084 | 380 | 1215 | 602 | 1656 | 1164 | 1540 | 527 | ||
| (77.6) | (73.9) | (73.3) | (79.9) | (84.7) | (77.2) | (77.2) | (70.5) | |||
| Non-binary | 31 | 1 | 4 | 4 | 13 | 4 | 5 | 0 | ||
| (0.3) | (0.2) | (0.2) | (0.5) | (0.7) | (0.3) | (0.3) | (0.0) | |||
| Age, n (%) | ||||||||||
| Young adults (18–30 years) | 3532 (38.7) | 259 (50.4) | 882 (53.2) | 362 (48.1) | 545 (27.9) | 533 (35.4) | 604 (30.3) | 347 (46.5) | 443.93 (12) | <0.001 |
| Middle-aged (31–59 years) | 5017 (55.0) | 245 (47.7) | 727 (43.9) | 324 (43.0) | 1235 (63.1) | 874 (58.0) | 1233 (61.8) | 379 (50.7) | ||
| Older adults (≥60 years) | 581 (6.4) | 10 (1.9) | 48 (2.9) | 67 (8.9) | 176 (9.0) | 100 (6.6) | 159 (8.0) | 21 (2.8) | ||
| Employment status, n (%) | ||||||||||
| Full-time | 4904 (53.7) | 326 (63.4) | 808 (48.8) | 359 (47.7) | 1288 (62.8) | 610 (40.5) | 1118 (56.0) | 455 (60.9) | 806.24 (18) | <0.001 |
| Part-time | 1599 (17.5) | 72 (14.0) | 189 (11.4) | 115 (15.3) | 266 (13.6) | 557 (37.0) | 323 (16,2) | 77 (10.3) | ||
| Unemployed | 2028 (22.2) | 103 (20.0) | 583 (35.2) | 222 (29.5) | 267 (13.7) | 256 (17.0) | 428 (21.4) | 169 (22.6) | ||
| Others (retired/on leave) | 599 (6.6) | 13 (2.5) | 77 (4.6) | 57 (7.6) | 1956 (10.0) | 84 (5.6) | 127 (6.4) | 46 (6.2) | ||
| Working as health care professionals b, n (%) | ||||||||||
| Yes | 1478 (16.5) | 59 (11.7) | 168 (10.8) | 57 (7.7) | 204 (10.6) | 473 (31.6) | 388 (19.7) | 129 (17.4) | 400.24 (6) | <0.001 |
| No | 7472 (83.5) | 444 (88.3) | 1393 (89.2) | 686 (92.3) | 1728 (89.4) | 1022 (68.4) | 1586 (80.3) | 613 (82.6) | ||
| Educational level, n (%) | ||||||||||
| Higher school or below | 1135 (12.4) | 44 (8.6) | 351 (21.2) | 71 (9.4) | 235 (12.0) | 98 (6.5) | 164 (8.2) | 172 (23.0) | 797.19 (30) | <0.001 |
| College/university students | 1175 (12.9) | 49 (9.5) | 201 (12.1) | 134 (17.8) | 212 (10.8) | 242 (16.1) | 278 (13.9) | 59 (7.9) | ||
| Graduated from university | 2655 (29.1) | 239 (46.5) | 564 (34.0) | 222 (29.5) | 524 (26.8) | 235 (15.6) | 622 (31.2) | 249 (33.3) | ||
| Master or postgraduate | 3162 (34.6) | 150 (29.2) | 386 (23.3) | 247 (32.8) | 721 (36.9) | 688 (45.7) | 751 (37.6) | 219 (29.3) | ||
| Doctorate | 764 (8.4) | 32 (6.2) | 132 (8.0) | 59 (7.8) | 240 (12.3) | 153 (10.2) | 115 (5.8) | 33 (4.4) | ||
| Others | 239 (2.6) | 0 (0.0) | 23 (1.4) | 20 (2.7) | 24 (1.2) | 91 (6.0) | 66 (3.3) | 15 (2.0) | ||
| Marital status, n (%) | ||||||||||
| Single | 2823 (30.9) | 233 (45.3) | 705 (42.5) | 279 (37.1) | 417 (21.3) | 390 (25.9) | 584 (29.3) | 215 (28.8) | 441.82 (18) | <0.001 |
| In a relationship/ engaged | 2329 (25.5) | 108 (21.0) | 267 (16.1) | 154 (20.5) | 555 (28.4) | 522 (34.6) | 483 (24.2) | 240 (32.1) | ||
| Married | 3297 (36.1) | 163 (31.7) | 618 (37.3) | 26 (34.7) | 758 (38.8) | 499 (33.1) | 761 (38.1) | 237 (31.7) | ||
| Others (divorced/widowed/separated) | 681 (7.5) | 10 (1.9) | 67 (4.0) | 59 (7.8) | 226 (11.6) | 96 (6.4) | 168 (8.4) | 55 (7.4) | ||
| Having children, n (%) | ||||||||||
| Yes | 3730 (40.9) | 121 (23.5) | 587 (35.4) | 287 (38.1) | 997 (51.0) | 652 (43.3) | 835 (41.8) | 251 (33.6) | 189.86 (6) | <0.001 |
| No | 5400 (59.1) | 393 (76.5) | 1070 (64.6) | 466 (61.9) | 959 (49.0) | 855 (56.7) | 1161 (58.2) | 496 (66.4) | ||
| Living situation, n (%) | ||||||||||
| Live alone | 1341 (14.7) | 38 (7.4) | 186 (11.2) | 79 (10.5) | 351 (17.9) | 270 (17.9) | 291 (14.6) | 126 (16.9) | 1076.23 (24) | <0.001 |
| Live with both parents | 1904 (20.9) | 231 (44.9) | 644 (38.9) | 181 (24.0) | 145 (7.4) | 134 (7.4) | 426 (21.3) | 143 (19.1) | ||
| Living with one of the parents | 465 (5.1) | 34 (6.6) | 85 (5.1) | 86 (11.4) | 94 (4.8) | 44 (2.9) | 83 (4.2) | 39 (5.2) | ||
| Live with own family | 4928 (54.0) | 179 (34.8) | 695 (41.9) | 365 (48.5) | 1270 (64.9) | 901 (59.8) | 1128 (56.5) | 390 (52.2) | ||
| Live with friends/roommates | 492 (5.4) | 32 (6.2) | 47 (2.8) | 42 (5.6) | 96 (4.9) | 158 (10.5) | 68 (3.4) | 49 (6.6) | ||
| Since the social isolation measures began, how frequent you needed to leave your house? n (%) | ||||||||||
| No, I stayed at home | 4304 (47.1) | 173 (33.7) | 803 (48.5) | 504 (66.9) | 889 (45.4) | 310 (20.6) | 1187 (59.5) | 438 (58.6) | 977.70 (18) | <0.001 |
| Once only | 695 (7.6) | 49 (9.5) | 199 (12.0) | 49 (6.5) | 144 (7.4) | 69 (4.6) | 128 (6.4) | 57 (7.6) | ||
| A couple of times | 2186 (23.9) | 150 (29.2) | 409 (24.7) | 130 (17.3) | 450 (23.0) | 563 (37.4) | 386 (19.3) | 98 (13.1) | ||
| More than three times per week | 1945 (21.3) | 142 (27.6) | 246 (14.8) | 70 (9.3) | 473 (24.2) | 565 (37.5) | 295 (14.8) | 154 (20.6) | ||
| Since the social isolation measures began, have your financial situation changed? n (%) | ||||||||||
| Have got better | 787 (8.6) | 38 (7.4) | 177 (10.7) | 54 (7.2) | 165 (8.4) | 150 (10.0) | 143 (7.2) | 60 (8.0) | 173.08 (12) | <0.001 |
| Stay the same | 5290 (57.9) | 322 (62.6) | 961 (58.0) | 377 (50.1) | 1254 (64.1) | 903 (59.9) | 1001 (50.2) | 472 (63.2) | ||
| Have got worse | 3053 (33.4) | 154 (30.0 | 519 (31.3) | 322 (42.8) | 537 (27.5) | 454 (30.1) | 852 (42.7) | 215 (28.8) | ||
| Have you been infected by COVID-19 c? n (%) | ||||||||||
| Yes | 133 (1.5) | 1 (0.2) | 65 (3.9) | 7 (0.9) | 33 (1.7) | 10 (0.7) | 13 (0.7) | 4 (0.5) | 332.59 (12) | <0.001 |
| No | 8041 (88.1) | 507 (98.6) | 1513 (91.3) | 671 (89.1) | 1639 (83.8) | 1254 (83.2) | 1836 (92.0) | 621 (83.1) | ||
| I am not sure or have had symptoms but not diagnosed | 956 (10.5) | 6 (1.2) | 79 (4.8) | 75 (10.0) | 284 (14.5) | 243 (16.1) | 147 (7.4) | 122 (16.3) | ||
| Have your partner being infected by COVID-19 c,d? n (%) | ||||||||||
| Yes | 68 (0.8) | 1 (0.2) | 15 (0.9) | 1 (0.1) | 29 (1.5) | 9 (0.6) | 10 (0.5) | 3 (0.4) | 188.62 (12) | <0.001 |
| No | 8351 (92.4) | 475 (98.5) | 1590 (96.5) | 704 (93.0) | 1733 (89.2) | 1320 (88.4) | 1877 (94.5) | 652 (88.3) | ||
| I am not sure or have had symptoms but not diagnosed | 622 (6.9) | 6 (1.2) | 42 (2.6) | 45 (6.0) | 181 (9.3) | 165 (11.0) | 100 (5.0) | 83 (11.2) | ||
| Have your significant others being infected by COVID-19 c,d? n (%) | ||||||||||
| Yes | 519 (5.7) | 3 (0.6) | 65 (3.9) | 27 (3.6) | 98 (5.0) | 146 (9.7) | 150 (7.5) | 30 (4.0) | 262.11 (12) | <0.001 |
| No | 7856 (86.1) | 506 (98.4) | 1526 (92.1) | 651 (86.5) | 1655 (84.6) | 1182 (78.4) | 1717 (86.1) | 619 (82.9) | ||
| I am not sure or my significant others have had symptoms but not diagnosed | 754 (8.3) | 5 (1.0) | 66 (4.0) | 75 (10.0) | 203 (10.4) | 179 (11.9) | 128 (6.4) | 98 (13.1) | ||
| COVID-19 Government Response Stringency Index (OxCGRT Indicators) | ||||||||||
| Mean (SD) score across studied countries across study period | 70.92 (6.71) | 59.34 (8.71) | 76.83 (12.14) | 79.76 (7.83) | 67.63 (18.62) | 70.32 (14.42) | 73.35 (13.61) | 67.81 (12.42) | ||
| All Regions a (n = 9130) | Eastern Asia—HK Only (n = 514) | Western Asia (n = 1657) | N. & S. America b (n = 753) | Northern Europe (n = 1956) | Western Europe (n= 1507) | Southern Europe (n = 1996) | Eastern Europe (n = 747) | F (df) | p-Value | |
|---|---|---|---|---|---|---|---|---|---|---|
| Variables (Possible Range) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
| Mental health | ||||||||||
| Total score (0–70) | 41.07 (13.87) | 34.23 (12.54) | 40.57 (14.21) | 42.44 (14.89) | 41.29 (13.97) | 43.28 (12.98) | 42.31 (13.13) | 37.18 (14.09) | 42.47 (6) | <0.001 |
| Emotional (0–15) | 10.15 (3.34) | 8.73 (3.06) | 9.60 (3.50) | 10.57 (3.43) | 10.42 (3.24) | 10.94 (3.06) | 10.23 (3.25) | 9.46 (3.51) | 47.98 (6) | <0.001 |
| Social (0–25) | 11.37 (5.99) | 8.35 (5.05) | 11.29 (6.23) | 11.78 (6.24) | 11.79 (5.99) | 12.12 (5.81) | 11.56 (5.87) | 10.08 (5.70) | 34.86 (6) | <0.001 |
| Psychological (0–30) | 19.55 (6.56) | 17.15 (6.46) | 19.69 (6.54) | 20.09 (6.88) | 19.08 (6.81) | 20.23 (6.12) | 20.51 (6.13) | 17.65 (6.83) | 35.24 (6) | <0.001 |
| Illness perceptions toward COVID-19 | ||||||||||
| Consequence (1–10) | 7.40 (2.24) | 6.84 (1.88) | 7.96 (2.12) | 7.25 (2.17) | 7.48 (2.21) | 6.49 (2.36) | 7.83 (2.07) | 7.15 (2.37) | 82.86 (6) | <0.001 |
| Timeline (1–10) | 6.57 (1.81) | 7.09 (1.64) | 7.06 (2.00) | 6.78 (1.66) | 6.03 (1.72) | 6.34 (1.59) | 6.86 (1.78) | 6.03 (1.80) | 85.57 (6) | <0.001 |
| Concern (1–10) | 6.72 (2.41) | 6.63 (2.03) | 7.30 (2.33) | 7.50 (2.15) | 6.65 (2.37) | 5.42 (2.39) | 7.36 (2.13) | 5.80 (2.56) | 160.04 (6) | <0.001 |
| Emotional responses (1–10) | 6.39 (2.51) | 6.28 (2.09) | 6.97 (2.51) | 6.84 (2.45) | 6.38 (2.53) | 5.64 (2.49) | 6.49 (2.41) | 5.99 (2.60) | 46.95 (6) | <0.001 |
| Perceived susceptibility (3–18) | 8.74 (3.56) | 9.23 (2.99) | 9.82 (3.62) | 9.11 (3.63) | 9.25 (3.48) | 7.35 (3.27) | 8.29 (3.42) | 8.35 (3.66) | 85.04 (6) | <0.001 |
| Perceived severity (3–18) | 12.42 (3.70) | 14.55 (3.02) | 11.90 (3.94) | 13.56 (3.52) | 12.83 (3.54) | 11.12 (3.28) | 12.86 (3.64) | 11.37 (3.77) | 101.43 (6) | <0.001 |
| Seeking social support | ||||||||||
| Venting (2–8) | 4.76 (1.56) | 5.23 (1.45) | 4.93 (1.67) | 4.41 (1.47) | 4.46 (1.35) | 5.06 (1.67) | 4.52 (1.42) | 5.18 (1.73) | 57.49 (6) | <0.001 |
| Use of emotional support (2–8) | 4.72 (1.74) | 4.75 (1.60) | 4.66 (1.71) | 4.43 (1.95) | 4.83 (1.56) | 4.76 (1.78) | 4.56 (1.74) | 5.26 (1.93) | 20.66(6) | <0.001 |
| Use of instrumental support (2–8) | 4.38 (1.69) | 5.28 (1.52) | 4.88 (1.95) | 4.00 (1.76) | 4.34 (1.42) | 4.15 (1.58) | 4.08 (1.60) | 4.44 (1.72) | 73.93 (6) | <0.001 |
| Religious belief (2–8) | 3.84 (1.95) | 4.06 (1.92) | 4.69 (2.17) | 4.19 (2.14) | 3.56 (1.76) | 3.27 (1.69) | 3.61 (1.76) | 3.90 (1.98) | 96.39 (6) | <0.001 |
| Problem-solving | ||||||||||
| Active coping (2–8) | 5.65 (1.55) | 5.78 (1.44) | 6.11 (1.45) | 5.32 (1.60) | 5.51 (1.45) | 5.27 (1.59) | 5.72 (1.53) | 5.82 (1.68) | 52.84 (6) | <0.001 |
| Planning (2–8) | 5.57 (1.54) | 5.90 (1.34) | 5.54 (1.48) | 5.28 (1.64) | 5.66 (1.44) | 5.39 (1.64) | 5.61 (1.56) | 5.80 (1.61) | 16.53 (6) | <0.001 |
| Avoidance | ||||||||||
| Behavioral disengagement (2–8) | 2.86 (1.23) | 3.40 (1.26) | 2.99 (1.33) | 2.73 (1.25) | 3.06 (1.24) | 2.62 (1.13) | 2.69 (1.10) | 2.73 (1.21) | 48.51 (6) | <0.001 |
| Self-distraction (2–8) | 5.51 (1.61) | 5.19 (1.54) | 5.87 (1.47) | 5.87 (1.49) | 5.16 (1.55) | 5.36 (1.76) | 5.47 (1.59) | 5.83 (1.67) | 47.65 (6) | <0.001 |
| Substance use (2–8) | 2.60 (1.22) | 2.69 (1.34) | 2.37 (1.00) | 2.66 (1.41) | 2.82 (1.26) | 2.64 (1.24) | 2.37 (0.97) | 3.00 (1.58) | 49.09 (6) | <0.001 |
| Denial (2–8) | 2.93 (1.32) | 2.84 (1.16) | 3.83 (1.50) | 2.60 (1.14) | 2.81 (1.15) | 2.45 (0.95) | 2.83 (1.25) | 2.91 (1.44) | 199.51 (6) | <0.001 |
| Self-blaming (2–8) | 3.46 (1.45) | 4.34 (1.49) | 4.11 (1.47) | 3.45 (1.70) | 3.64 (1.39) | 2.83 (1.17) | 3.06 (1.24) | 3.24 (1.31) | 188.61 (6) | <0.001 |
| Positive thinking | ||||||||||
| Humor (2–8) | 4.57 (1.73) | 4.04 (1.54) | 4.80 (1.74) | 4.05 (1.87) | 4.56 (1.60) | 5.11 (1.75) | 4.18 (1.54) | 4.92 (1.93) | 73.36 (6) | <0.001 |
| Positive reframing (2–8) | 5.78 (1.62) | 5.50 (1.45) | 6.15 (1.56) | 5.31 (1.73) | 5.68 (1.52) | 6.10 (1.62) | 5.53 (1.63) | 5.93 (1.64) | 48.8 9 (6) | <0.001 |
| Acceptance (2–8) | 6.55 (1.35) | 6.17 (1.34) | 6.17 (1.34) | 6.51 (1.37) | 6.72 (1.13) | 6.85 (1.36) | 6.61 (1.27) | 6.90 (1.36) | 87.54 (6) | <0.001 |
| Psychological flexibility | ||||||||||
| Total score (6–30) | 21.83 (4.09) | 19.43 (4.02) | 21.15 (4.02) | 21.41 (4.58) | 22.09 (3.85) | 22.89 (3.97) | 22.22 (3.89) | 21.58 (4.16) | 62.57 (6) | <0.001 |
| Prosociality | ||||||||||
| Total score (6–30) | 22.85 (4.19) | 20.72 (3.93) | 24.38 (3.94) | 23.33 (4.25) | 21.04 (4.29) | 23.04 (3.66) | 23.75 (3.76) | 22.34 (4.31) | 152.61 (6) | <0.001 |
| All Regions a (n= 9130) | Eastern Asia, HK Only (n = 514) | Western Asia (n = 1657) | N. & S. America b (n = 753) | Northern Europe (n = 1956) | Western Europe (n = 1507) | Southern Europe (n = 1996) | Eastern Europe (n = 747) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Β c (SE) | p-Value | β (SE) | p-Value | β (SE) | p-value | β (SE) | p-Value | β (SE) | p-Value | β (SE) | p-Value | β (SE) | p-Value | |
| Direct effects from illness perceptions toward COVID-19 (i.e., unstandardized path coefficient) | ||||||||||||||
| Seeking social support | 0.12 (0.03) | <0.001 | 0.15 (0.02) | <0.001 | 0.10 (0.02) | <0.001 | 0.11 (0.01) | <0.001 | 0.20 (0.02) | <0.001 | 0.12 (0.01) | <0.001 | 0.21 (0.02) | <0.001 |
| Problem-solving | −0.04 (0.03) | 0.22 | 0.02 (0.02) | 0.24 | 0.09 (0.02) | <0.001 | 0.04 (0.01) | <0.001 | 0.10 (0.02) | <0.001 | 0.12 (0.01) | <0.001 | 0.11 (0.03) | <0.001 |
| Avoidance | 0.10 (0.03) | <0.001 | 0.13 (0.01) | <0.001 | 0.17 (0.02) | <0.001 | 0.15 (0.01) | <0.001 | 0.14 (0.01) | <0.001 | 0.12 (0.01) | <0.001 | 0.15 (0.02) | <0.001 |
| Positive thinking | −0.02 (0.01) | 0.19 | −0.03 (0.01) | <0.001 | −0.03 (0.01) | 0.01 | −0.05 (0.01) | <0.001 | −0.11 (0.01) | <0.001 | −0.05 (0.01) | <0.001 | −0.02 (0.01) | 0.033 |
| Prosociality | 0.05 (0.02) | 0.035 | −0.01 (0.01) | 0.29 | −0.03 (0.01) | 0.016 | 0.01 (0.01) | 0.57 | 0.01 (0.01) | 0.09 | 0.01 (0.01) | 0.81 | 0.02 (0.01) | <0.001 |
| PF c | −0.12 (0.02) | <0.001 | −0.10 (0.01) | <0.001 | −0.14 (0.02) | <0.001 | −0.12 (0.01) | <0.001 | −0.09 (0.01) | <0.001 | −0.10 (0.01) | <0.001 | −0.13 (0.02) | <0.001 |
| Direct effects on mental health (i.e., unstandardized path coefficient) | ||||||||||||||
| Seeking social support | 0.19 (0.16) | 0.043 | 0.41 (0.12) | <0.001 | −0.09 (0.14) | 0.51 | 0.58 (0.10) | <0.001 | 0.41 (0.08) | <0.001 | 1.10 (0.20) | <0.001 | 0.38 (0.14) | 0.004 |
| Problem-solving | −0.57 (.66) | 0.39 | 0.08 (0.11) | 0.49 | 0.18 (0.50) | 0.72 | −0.84 (0.28) | 0.008 | −0.21 (0.11) | 0.06 | −0.40 (0.29) | 0.17 | −0.06 (0.33) | 0.86 |
| Avoidance | −0.68 (0.26) | 0.010 | −0.41 (0.20) | 0.041 | −0.74 (0.34) | 0.03 | −0.72 (0.25) | 0.003 | −10.02 (0.34) | 0.003 | −30.07 (0.60) | <0.001 | −0.60 (0.48) | 0.21 |
| Positive thinking | 2.83 (2.14) | 0.19 | 0.57 (0.20) | 0.005 | 0.70 (2.14) | 0.76 | 1.99 (0.80) | 0.013 | 0.67 (0.20) | <0.001 | 1.69 (0.46) | <0.001 | 1.75 (1.40) | 0.21 |
| Prosociality | 0.48 (0.22) | 0.029 | .66 (0.13) | <0.001 | 0.36 (0.17) | 0.030 | 0.16 (0.10) | 0.12 | 0.30 (0.11) | 0.023 | 0.59 (0.14) | <0.001 | 0.41 (0.16) | 0.01 |
| PF d | 1.30 (0.28) | <0.001 | 2.43 (0.18) | <0.001 | 2.35 (0.38) | <0.001 | 2.45 (0.26) | <0.001 | 2.53 (0.26) | <0.001 | 1.15 (0.35) | 0.001 | 2.58 (0.29) | <0.001 |
| IP e | −0.09 (0.06) | 0.13 | −0.01 (0.03) | 0.89 | 0.07 (0.10) | 0.44 | 0.10 (0.06) | 0.10 | 0.11 (0.04) | 0.009 | 0.10 (0.07) | 0.20 | −0.04 (0.07) | 0.55 |
| Indirect effects | ||||||||||||||
| IP➔SS f➔MH g | 0.03 (0.02) | 0.06 | 0.06 (0.02) | 0.002 | −0.01 (0.01) | 0.53 | 0.07 (0.01) | <0.001 | 0.07 (0.02) | <0.001 | 0.12 (0.03) | <0.001 | 0.08 (0.03) | 0.005 |
| IP➔PS h➔MH | 0.02 (0.03) | 0.47 | 0.01 (0.01) | 0.56 | 0.02 (0.05) | 0.72 | −0.04 (0.01) | 0.009 | −0.02 (0.01) | 0.12 | −0.08 (0.03) | 0.16 | −0.01 (0.03) | 0.72 |
| IP➔Avoidance ➔MH | −0.07 (0.03) | 0.04 | −0.05 (0.03) | 0.042 | −0.13 (0.06) | 0.035 | −0.14 (0.04) | 0.002 | −0.12 (0.04) | 0.004 | −0.32 (0.07) | <0.001 | −0.13 (0.07) | 0.07 |
| IP➔PT i➔MH | −0.06 (0.05) | 0.30 | −0.02 (0.01) | 0.038 | −0.01 (0.06) | 0.75 | −0.11 (0.04) | 0.01 | −0.07 (0.03) | 0.015 | −0.11 (0.03) | 0.011 | −0.05 (0.03) | 0.14 |
| IP➔Prosociaity➔MH | 0.05 (0.01) | 0.016 | −0.01 (0.01) | 0.33 | −0.01 (0.01) | 0.08 | 0.00 (0.00) | 0.39 | 0.00 (0.00) | 0.39 | −0.01 (0.01) | 0.33 | 0.10 (0.03) | 0.008 |
| IP➔PF➔ MH | −0.15 (0.07) | 0.021 | −0.24 (0.03) | 0.002 | −0.33 (0.12) | 0.02 | −0.29 (0.05) | 0.002 | −0.25 (0.04) | 0.001 | −0.16 (0.05) | 0.008 | −0.25 (0.05) | 0.004 |
| Total variance (R2) | 0.64 | 0.56 | 0.67 | 0.72 | 0.66 | 0.73 | 0.72 | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chong, Y.Y.; Chien, W.T.; Cheng, H.Y.; Lamnisos, D.; Ļubenko, J.; Presti, G.; Squatrito, V.; Constantinou, M.; Nicolaou, C.; Papacostas, S.; et al. Patterns of Psychological Responses among the Public during the Early Phase of COVID-19: A Cross-Regional Analysis. Int. J. Environ. Res. Public Health 2021, 18, 4143. https://doi.org/10.3390/ijerph18084143
Chong YY, Chien WT, Cheng HY, Lamnisos D, Ļubenko J, Presti G, Squatrito V, Constantinou M, Nicolaou C, Papacostas S, et al. Patterns of Psychological Responses among the Public during the Early Phase of COVID-19: A Cross-Regional Analysis. International Journal of Environmental Research and Public Health. 2021; 18(8):4143. https://doi.org/10.3390/ijerph18084143
Chicago/Turabian StyleChong, Yuen Yu, Wai Tong Chien, Ho Yu Cheng, Demetris Lamnisos, Jeļena Ļubenko, Giovambattista Presti, Valeria Squatrito, Marios Constantinou, Christiana Nicolaou, Savvas Papacostas, and et al. 2021. "Patterns of Psychological Responses among the Public during the Early Phase of COVID-19: A Cross-Regional Analysis" International Journal of Environmental Research and Public Health 18, no. 8: 4143. https://doi.org/10.3390/ijerph18084143
APA StyleChong, Y. Y., Chien, W. T., Cheng, H. Y., Lamnisos, D., Ļubenko, J., Presti, G., Squatrito, V., Constantinou, M., Nicolaou, C., Papacostas, S., Aydin, G., Ruiz, F. J., Garcia-Martin, M. B., Obando-Posada, D. P., Segura-Vargas, M. A., Vasiliou, V. S., McHugh, L., Höfer, S., Baban, A., ... Kassianos, A. P. (2021). Patterns of Psychological Responses among the Public during the Early Phase of COVID-19: A Cross-Regional Analysis. International Journal of Environmental Research and Public Health, 18(8), 4143. https://doi.org/10.3390/ijerph18084143













