The Moyamoya Health Behavior Scale for Adolescent Patients: Measurement Tool Development and Psychometric Evaluation
Abstract
:1. Introduction
2. Materials and Methods
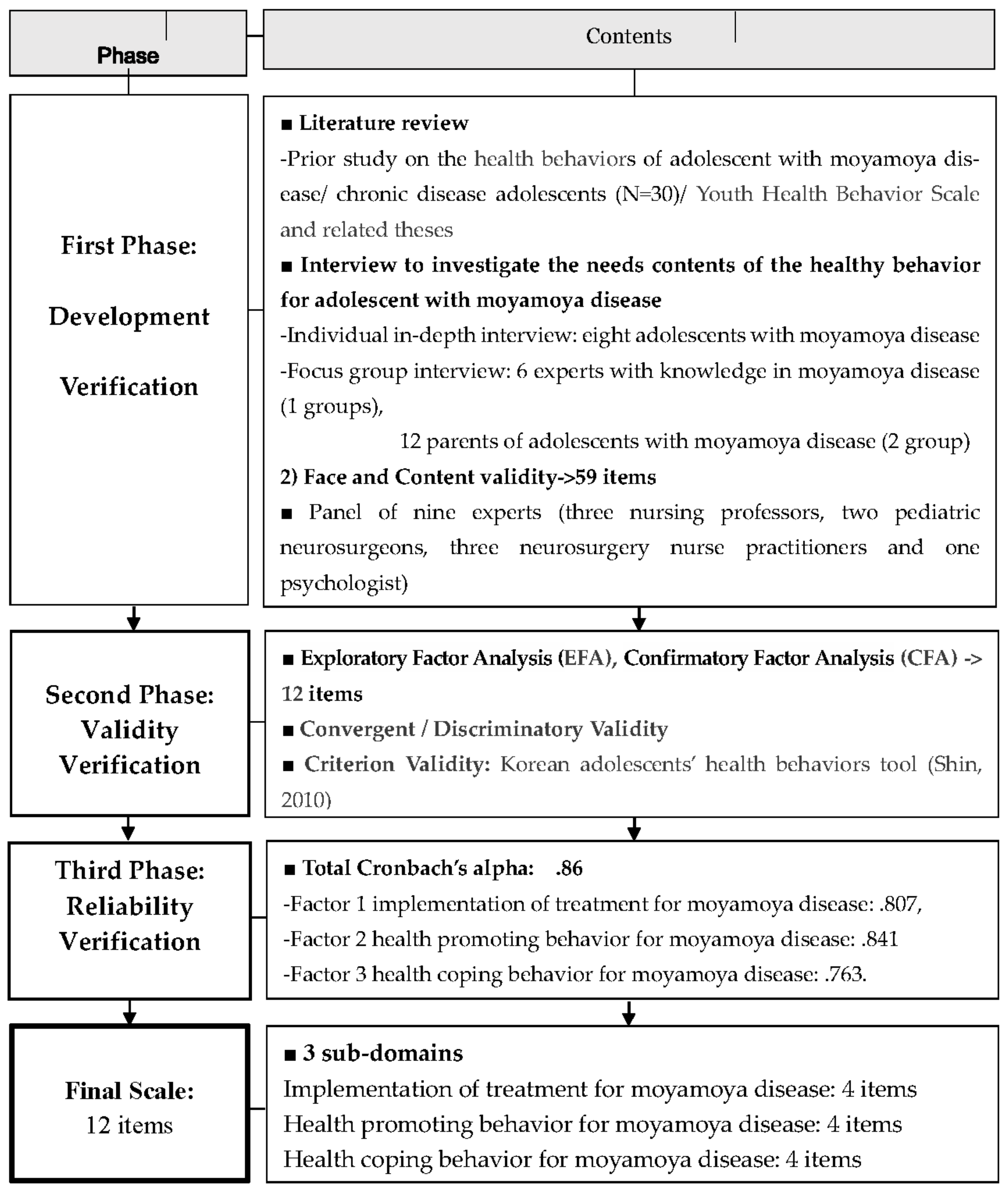
2.1. Research Design
2.2. Development Verification of the Moyamoya-HB Scale
2.2.1. Item Generation Stage: Identification of Preliminary Questions
Review of Literature and Consideration of Existing Tools
In-Depth Interviews for Initial Questions
2.2.2. Content Validity Testing: Face and Content Validity
2.2.3. Item Analysis
2.3. Tests of Validity
2.3.1. EFA and CFA
2.3.2. Convergent/Discriminatory Validity
2.3.3. Criterion Validity
2.4. Test of Reliability
2.5. Ethical Considerations
2.6. Data Analysis
3. Results
3.1. Item Generation
3.2. Content and Face Validity
3.3. General Characteristics of Participants
3.4. Item Analysis
3.5. Validity Verification
3.5.1. Exploratory Factor Analysis (EFA)
3.5.2. Confirmatory Factor Analysis (CFA)
3.5.3. Concurrent Validity
3.5.4. Convergent Validity and Discriminant Validity
3.6. Reliability Verification
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, J.S. Moyamoya disease: Epidemiology, clinical features, and diagnosis. J. Stroke 2016, 18, 2–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bang, O.; Fujimura, M.; Kim, S.K. The Pathophysiology of Moyamoya Disease: An Update. J. Stroke 2016, 18, 12–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suzuki, J.; Takaku, A. Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch. Neurol. 1969, 20, 288–299. [Google Scholar] [CrossRef] [PubMed]
- Uchino, K.; Johnston, S.C.; Becker, K.J.; Tirschwell, D.L. Moyamoya disease in Washington state and California. Neurology 2005, 65, 956–958. [Google Scholar] [CrossRef]
- Fujimura, M.; Tominaga, T. Lessons learned from moyamoya disease: Outcome of direct/indirect revascularization surgery for 150 affected hemispheres. Neurol. Med. Chir. 2012, 52, 327–332. [Google Scholar] [CrossRef] [Green Version]
- Hwang, Y.S. Clinical Features of Moyamoya Disease: An Overview. In Moyamoya Disease Update; Springer: New York, NY, USA, 2010; pp. 107–109. [Google Scholar]
- Guzman, R.; Lee, M.; Achrol, A.; Bell-Stephens, T.; Kelly, M.; Do, H.M.; Marks, M.P.; Steinberh, G.K. Clinical outcome after 450 revascularization procedures for moyamoya disease. Clinical article. J. Neurosurg. 2009, 111, 927–935. [Google Scholar] [CrossRef]
- Liu, X.; Zhang, D.; Shuo, W.; Zhao, Y.; Wang, R.; Zhao, J. Long term outcome after conservative and surgical treatment of haemorrhagic moyamoya disease. J. Neurol. Neurosurg. Psychiatry 2013, 84, 258–265. [Google Scholar]
- Takanashi, J.I. Moyamoya disease in children. Brain Dev. 2011, 33, 229–234. [Google Scholar] [CrossRef]
- Chamlin, S.L.; Chren, M.M. Quality of life outcomes and measurement in childhood atopic dermatitis. Immunol. Allergy Clin. N. Am. 2010, 30, 281–288. [Google Scholar] [CrossRef] [Green Version]
- Yeom, I.S.; Kim, D.S.; Lee, E.Y.; Kim, H.S. The Intellectual and Psychological Characteristics of Children with Moyamoya Disease. Child Health Nurs. Res. 2015, 21, 123–130. [Google Scholar] [CrossRef]
- Bersano, A.; Guey, S.; Bedini, G.; Nava, S.; Hervé, D.; Vajkoczy, P.; Klijn, C. Research Progresses in Understanding the Pathophysiology of Moyamoya Disease. Cerebrovasc. Dis. 2016, 41, 105–118. [Google Scholar] [CrossRef] [Green Version]
- Hertza, J.; Loughan, A.; Perna, R. Moyamoya disease: Review of literature. Appl. Neuropsychol. 2014, 21, 21–27. [Google Scholar] [CrossRef]
- Yasuyuki, K.; Koji, I.; Norio, N.; Hiroharu, K.; Kenji, F.; Jun, M.; Kazuhito, F.; Hidehiro, I.; Nobuo, H. Cerebral blood flow and metabolism of hyperperfusion after cerebral revascularization in patients with moyamoya disease. J. Cereb. Blood Flow Metab. 2012, 32, 2066–2075. [Google Scholar]
- Kim, D.K.; Chang, S.A.; Park, T.K. Moyamoya disease: Cardiologist’s Perspectives. J. Lipid Atheroscler. 2016, 5, 115–120. [Google Scholar] [CrossRef] [Green Version]
- Abbott, A.L.; Silvestrini, M.; Topakian, R.; Golledge, J.; Brunser, A.M.; de Borst, G.J.; Harbaugh, R.E.; Doubal, F.N.; Rundek, T.; Thapar, A.; et al. Optimizing the Definitions of Stroke, Transient Ischemic Attack, and Infarction for Research and Application in Clinical Practice. Front. Neurol. 2017, 8, 537. [Google Scholar] [CrossRef] [Green Version]
- Currie, C.; Roberts, C.; Morgan, A.; Smith, R.; Settertobulte, W.; Samdal, O. Health Behaviour in School-Aged Children (HBSC) Study; International Report from the 2001/2002 Survey; WHO: Copenhagen, Denmark, 2004. [Google Scholar]
- Doremus-Fitzwater, T.L.; Varlinskaya, E.I.; Spear, L.P. Motivation systems in adolescence: Possible implications for age differences in substance above and other risk taking behaviors. Brain Cognition. 2010, 72, 114–123. [Google Scholar] [CrossRef] [Green Version]
- Ernst, M.; Romeo, R.D.; Andersen, S.L. Neurobiology of the development of motivated behaviors in adolescence: A window into a neural systems model. Pharmacol. Biochem. Behav. 2009, 93, 199–211. [Google Scholar] [CrossRef]
- Hwang, H.; Kim, Y. A systematic review of studies on happiness determinants among domestic adolescents. Korean J. Youth Stud. 2017, 24, 1–28. [Google Scholar] [CrossRef]
- Shim, K.W.; Park, E.K.; Kim, J.S.; Kim, D.S. Cognitive Outcome of Pediatric Moyamoya Disease. J. Korean Neurosurg. Soc. 2015, 57, 440–444. [Google Scholar] [CrossRef]
- Kann, L.; Brener, N.D.; Warren, C.W.; Collins, J.L.; Giovino, G.A. An assessment of the effect of data collection setting on the prevalence of health risk behaviors among adolescents. J. Adolesc. Health 2002, 31, 327–335. [Google Scholar] [CrossRef]
- Kwon, S.J. A study on the correlation between health behaviors of adolescents and social factors. J. Korean Soc. Sch. Health 1996, 9, 69–75. [Google Scholar]
- DeVellis, R. Scale Development: Theory and Applications, 4th ed.; Sage Publishing: Thousand Oaks, CA, USA, 2016; pp. 111–147. [Google Scholar]
- Shin, Y.H. Development and Psychometric Evaluation of a Scale to Measure Health Behaviors of Adolescents. J. Korean Acad. Nurs. 2010, 40, 820–830. [Google Scholar] [CrossRef] [PubMed]
- Lincoln, Y.S.; Guba, E.G. Naturalistic Inquiry; Sage Publishing: Beverly Hills, CA, USA, 1985. [Google Scholar]
- Zamanzadeh, V.; Ghahramanian, A.; Rassouli, M.; Abbaszadeh, A.; Alavi-Majd, H.; Nikanfar, A.-R. Design and implementation content validity Study: Development of an instrument for measuring patient-centered communication. J. Caring Sci. 2015, 4, 165–178. [Google Scholar] [CrossRef] [PubMed]
- Pett, M.A.; Lackey, N.R.; Sullivan, J.J. Making Sense of Factor Analysis: The Use of Factor Analysis for Instrument Development in Health Care Research; Sage Publishing: Beverly Hills, CA, USA, 2003. [Google Scholar]
- Downe-Wamboldt, B. Content analysis: Method, applications, and issues. Health Care Women Int. 1992, 2, 313–321. [Google Scholar] [CrossRef]
- Kang, H. A guide on the use of factor analysis in the assessment of construct validity. J. Korean Acad. Nurs. 2013, 43, 587–594. [Google Scholar] [CrossRef] [Green Version]
- Ware, J.E., Jr.; Gandekm, B.; Kosinski, M.; Aaronson, N.K.; Apolone, G.; Cech, P.; Brazier, J.; Bullinger, M.; Kaasa, S.; Leplege, A.; et al. The equivalence of SF-36 summary health scores estimated using standard and country-specific algorithms in 10 countries: Results from the IQOLA Project. International Quality of Life Assessment. J. Clin. Epidemiol. 1998, 51, 1167–1170. [Google Scholar] [CrossRef]
- Erdfelder, E.; Faul, F.; Buchner, A. GPOWER: A general power analysis program. Behav. Res. Methods Instrum. Comput. 1996, 28, 1–11. [Google Scholar] [CrossRef]
- Dracup, K.A.; Meleis, A.I. Compliance: An interactionist approach. Nurs. Res. 1982, 31, 31–36. [Google Scholar] [CrossRef]
- Min, H.S.; Lee, E.J. A study of the relationship between compliance with therapeutic regimens and physiological parameters of hemodialysis patients. J. Korean Acad. Nurs. 2006, 36, 64–73. [Google Scholar] [CrossRef]
- Lynn, M.R. Determination and quantification of content validity. Nurs. Res. 1986, 35, 382–385. [Google Scholar] [CrossRef]
- Lee, J.G. SAS and Statistical Data Analysis; Hakjisa Corp.: Seoul, Korea, 2001. [Google Scholar]
- Kim, B.J.; Chae, S.I. Statistic Analysis Using SPSS PC+; Bobmunsa Co.: Seoul, Korea, 1988. [Google Scholar]
- Lee, E.O.; Lim, N.Y.; Park, H.A.; Lee, I.S.; Kim, J.I.; Bae, J.I.; Kim, H.S. Nursing Research and Statistics; Soomoonsa: Paju, Korea, 2009; pp. 770–789. [Google Scholar]
- Woo, J.P. AMOS and SPSS; Hanarea Academy: Seoul, Korea, 2016; pp. 564–567. [Google Scholar]
- Anderson, J.; Gerbing, D. Structural equation modeling in practice: A review and recommended two-step approach. Psychol. Bull. 1988, 103, 411–423. [Google Scholar] [CrossRef]
- Agras, W.S. Understanding compliance with the medical regimen: The scope of the problem and a theoretical perspective. Arthritis Care Res. 1989, 2, S2–S7. [Google Scholar] [CrossRef]
- Cox, K.; Stevenson, F.; Britten, N.; Dundar, Y. A Systematic Review of Communication between Patients and Health Providers about Medicine-Taking and Prescribing; GKT Concordance Unit, Kings College: Hong Kong, China, 2003. [Google Scholar]
- Noble, L.M. Doctor–patient communication and adherence to treatment. In Adherence to Treatment in Medical Conditions; Myers, L.B., Midence, K., Eds.; Harwood Academic Publishers: New York, NY, USA, 1998; pp. 51–82. [Google Scholar]
- Horn, P.; Bueltmann, E.; Buch, C.V.; Schmiedek, P. Arterio-embolic ischemic stroke in children with moyamoya disease. Child Nerv. Syst. 2005, 21, 104–107. [Google Scholar] [CrossRef]
- Kim, Y.S. The relationship of knowledge, attitudes about cancer and health behavior for cancer prevention in high school students. J Korean Acad. Child Health Nurs. 2010, 16, 102–111. [Google Scholar] [CrossRef]
- Oh, C.K.; Bae, A.J. The Relationship between Active Stress Coping and Internet Addiction: The Mediating Effects of Emotion Regulation and Impulsivity. Korean J. Youth Stud. 2019, 26, 401–424. [Google Scholar] [CrossRef]
- Byun, Y.S.; Lee, H.Y. A study on health risk behaviors in adolescents. J. Korean Acad. Fundam. Nurs. 2005, 12, 413–420. [Google Scholar]
- Takase, M.; Teraoka, S. Development of the holistic nursing competence scale. Nurs Health Sci. 2011, 13, 396–403. [Google Scholar] [CrossRef]
- Fabiane, F.R.M.; Julianan, F.F.M.; Clara, M.N.; Ana, C.S.A.; Maria, E.C.F. Scale development: Ten main limitations and recommendations to improve future research practices. Psicol. Reflex. Cirt. 2017, 30, 1–20. [Google Scholar]

| Variable | Category | Number of Patients (%) | Mean (±SD) | p-Value * |
|---|---|---|---|---|
| Sex | Male | 71 (59.17) | 0.02 * | |
| Female | 49 (40.83) | |||
| Age | 15.00 (±1.60) | |||
| Follow-up (month) | 35.64 (±30.94) | |||
| Suzuki stage | 3.18 (±0.54) | |||
| Diagnostic path | Clinical symptoms | 114 (95.00) | 0.19 | |
| Medical checkup | 6 (5.00) | |||
| During examination for other diseases | 0 (0.00) | |||
| Disease severity | Very serious | 6 (5.00) | 0.03 * | |
| Serious | 34 (28.33) | |||
| Average | 56 (46.67) | |||
| Not so serious | 24 (20.00) | |||
| Not at all serious | 0 (0.00) | |||
| Influence on normal life | None | 10 (8.33) | 0.04 * | |
| Slight | 74 (61.67) | |||
| Some | 13 (10.83) | |||
| Moderate | 23 (19.17) | |||
| Severe | 0 (0.00) | |||
| Frequency of symptom (last month) | Never | 6 (5.00) | 0.03 * | |
| Rarely | 44 (36.67) | |||
| Sometimes | 32 (26.67) | |||
| Very Often | 32 (26.67) | |||
| Constant | 6 (5.00) | |||
| Cerebral hemorrhage/cerebral infarction (history) | Infarction | 27 (22.50) | 0.04 * | |
| Hemorrhage | 0 (0.00) | |||
| Both | 0 (0.00) | |||
| Neither | 93 (77.50) | |||
| Seizure | Yes | 113 (94.17) | <0.05 * | |
| No | 7 (5.83) | |||
| Experienced TIA | Yes | 119 (99.17) | <0.05 * | |
| No | 1 (0.83) | |||
| TIA more than once a month | Yes | 91 (75.83) | 0.03 * | |
| No | 29 (24.17) | |||
| Surgery (EDAS) | No | 2 (1.67) | 0.04 * | |
| Both | 86 (71.67) | |||
| One | 32 (26.67) |
| Factors | Item Card No. | Communalities | Factor Loading | ||
|---|---|---|---|---|---|
| Factor 1 | Factor 2 | Factor 3 | |||
| Factor 1 (Implementation of treatment for moyamoya disease) | health08 | 0.660 | 0.656 | 0.405 | −0.256 |
| health38 | 0.809 | 0.838 | 0.139 | 0.296 | |
| health55 | 0.698 | 0.803 | 0.122 | 0.195 | |
| health56 | 0.687 | 0.774 | −0.062 | 0.290 | |
| Factor 2 (Health promoting behavior for moyamoya disease) | health03 | 0.613 | 0.308 | 0.673 | 0.257 |
| health15 | 0.799 | 0.058 | 0.861 | 0.232 | |
| health16 | 0.781 | −0.027 | 0.859 | 0.205 | |
| health42 | 0.564 | 0.147 | 0.721 | 0.151 | |
| Factor 3 (Health coping behavior for moyamoya disease) | health19 | 0.725 | 0.308 | 0.361 | 0.707 |
| health47 | 0.561 | 0.205 | 0.081 | 0.716 | |
| health51 | 0.713 | −0.028 | 0.241 | 0.809 | |
| health57 | 0.667 | 0.315 | 0.308 | 0.688 | |
| Explained variance | 8.276 | 2.733 | 2.944 | 2.599 | |
| Explained (%) | 68.974 | 22.778 | 24.535 | 21.661 | |
| Theoretical Variables | Measurement Variables | Estimated λ | Standard Error | Standardized Estimate | C.R. | p | SMC | AVE | Construct Reliability | Chronbach’s Alpha | * SMC (** CC) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Factor 1 (Treatment Instructions for Moyamoya Disease) | Item08 | 1.000 | - | 0.494 | - | - | 0.244 | 0.510 | 0.798 | 0.807 | Factor 1 & Factor 2 0.102 (0.320) |
| Item 38 | 2.033 | 0.354 | 0.946 | 5.742 *** | <0.001 | 0.895 | |||||
| Item 55 | 1.417 | 0.273 | 0.750 | 5.199 *** | <0.001 | 0.563 | |||||
| Item 56 | 1.162 | 0.231 | 0.707 | 5.032 *** | <0.001 | 0.500 | |||||
| Factor 2 (Moyamoya Health Promotion Acts) | Item 03 | 1.000 | - | 0.654 | - | - | 0.428 | 0.544 | 0.824 | 0.841 | Factor 2 & Factor 3 0.371 (0.609) |
| Item 15 | 2.172 | 0.275 | 0.905 | 7.893 *** | <0.001 | 0.820 | |||||
| Item 16 | 1.720 | 0.233 | 0.834 | 7.392 *** | <0.001 | 0.696 | |||||
| Item 42 | 1.426 | 0.228 | 0.651 | 6.266 *** | <0.001 | 0.424 | |||||
| Factor 3 (Health coping behavior for moyamoya disease) | Item 19 | 1.000 | - | 0.863 | - | - | 0.745 | 0.543 | 0.763 | 0.800 | Factor 1 & Factor 3 0.371 (0.609) |
| Item 47 | 0.594 | 0.090 | 0.587 | 6.590 *** | <0.001 | 0.345 | |||||
| Item 51 | 1.134 | 0.159 | 0.628 | 7.144 *** | <0.001 | 0.394 | |||||
| Item 57 | 1.095 | 0.109 | 0.831 | 10.07 5 *** | <0.001 | 0.690 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oh, W.-o.; Yeom, I.; Lim, S.-H.; Kim, D.-S.; Shim, K.-w. The Moyamoya Health Behavior Scale for Adolescent Patients: Measurement Tool Development and Psychometric Evaluation. Int. J. Environ. Res. Public Health 2021, 18, 4064. https://doi.org/10.3390/ijerph18084064
Oh W-o, Yeom I, Lim S-H, Kim D-S, Shim K-w. The Moyamoya Health Behavior Scale for Adolescent Patients: Measurement Tool Development and Psychometric Evaluation. International Journal of Environmental Research and Public Health. 2021; 18(8):4064. https://doi.org/10.3390/ijerph18084064
Chicago/Turabian StyleOh, Won-oak, Insun Yeom, Sung-Hyun Lim, Dong-Seok Kim, and Kyu-won Shim. 2021. "The Moyamoya Health Behavior Scale for Adolescent Patients: Measurement Tool Development and Psychometric Evaluation" International Journal of Environmental Research and Public Health 18, no. 8: 4064. https://doi.org/10.3390/ijerph18084064






