Epilepsy as a Comorbidity in Polymyositis and Dermatomyositis—A Cross-Sectional Study
Abstract
1. Introduction
2. Material and Methods
2.1. Ethical Statement
2.2. Study Design
2.3. Measures
2.4. Statistical Analysis
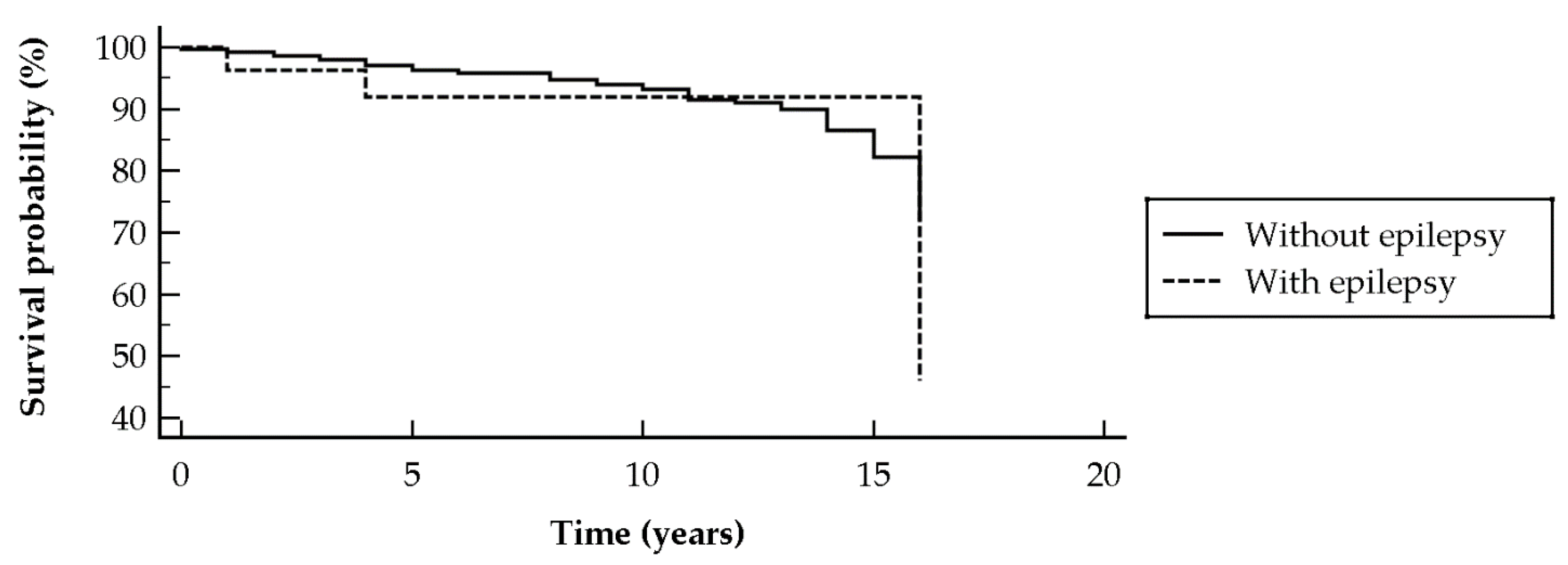
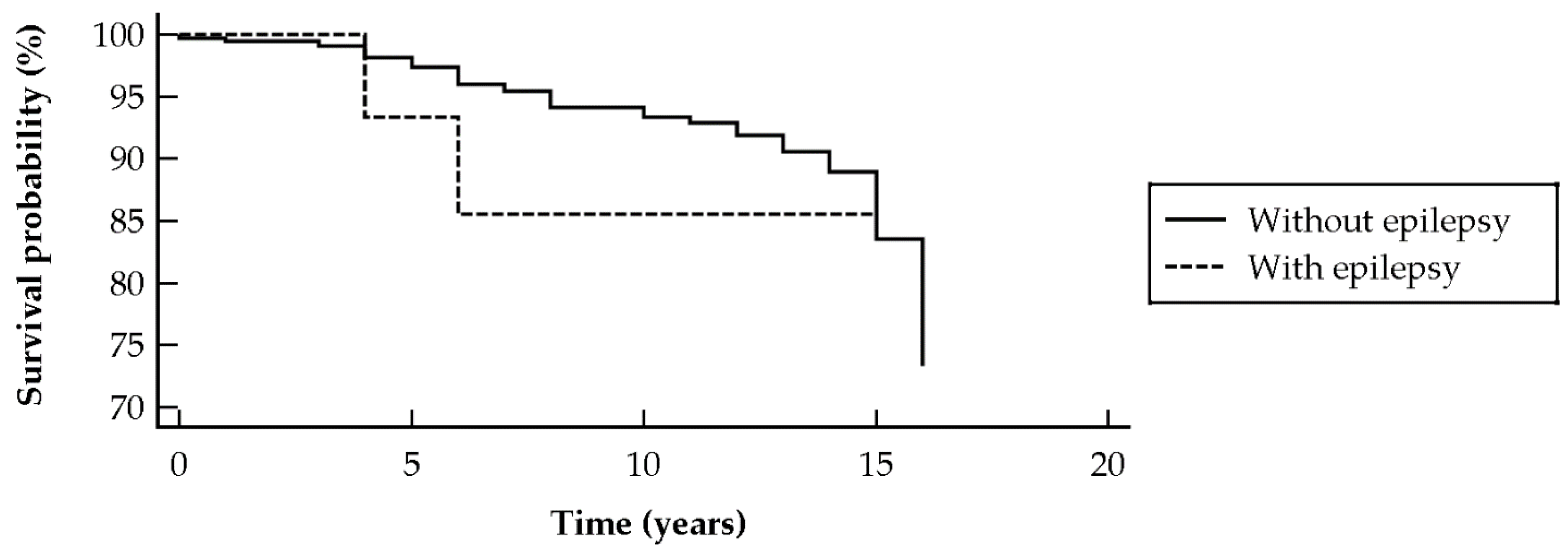
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DM | dermatomyositis |
| PM | polymyositis |
| ANA | antinuclear antibody; |
| Anti-SSA | anti-Sjögren’s syndrome-related antigen A |
| Anti-SSB | anti-Sjögren’s syndrome-related antigen B |
| Anti-RNP | anti-ribonucleoprotein |
| BMI | body mass index |
| CK | creatine kinase |
| SLE | systemic lupus erythematosus |
| SES | socioeconomic status |
| RA | rheumatoid arthritis |
References
- Dalakas, M. Polymyositis, dermatomyositis and inclusion-body myositis. N. Engl. J. Med. 1991, 325, 1487–1498. [Google Scholar] [CrossRef]
- Dalakas, M.; Hohlfeld, R. Polymyositis and dermatomyositis. Lancet 2003, 362, 971–982. [Google Scholar] [CrossRef]
- Manger, B.; Schett, G. Paraneoplastic syndromes in rheumatology. Nat. Rev. Rheumatol. 2014, 10, 662–670. [Google Scholar] [CrossRef] [PubMed]
- Baer, A.N. Paraneoplastic Muscle Disease. Rheum. Dis. Clin. N. Am. 2011, 37, 185–200. [Google Scholar] [CrossRef]
- Lin, Y.N.; Lin, C.L.; Chang, K.C.; Kao, C.H. Increased subsequent risk of acute coronary syndrome for patients with dermatomyo-sitis/polymyositis: A nationwide population-based retrospective cohort study. Scand. J. Rheumatol. 2015, 44, 42–47. [Google Scholar] [CrossRef]
- Silverberg, J.I.; Kwa, L.; Kwa, M.C.; Laumann, A.E.; Ardalan, K. Cardiovascular and cerebrovascular comorbidities of juvenile dermatomyositis in US children: An analysis of the National Inpatient Sample. Rheumatology 2018, 57, 694–702. [Google Scholar] [CrossRef] [PubMed]
- Nouh, A.; Carbunar, O.; Ruland, S. Neurology of Rheumatologic Disorders. Curr. Neurol. Neurosci. Rep. 2014, 14, 1–13. [Google Scholar] [CrossRef]
- Kronzer, V.L.; Crowson, C.S.; Sparks, J.A.; Myasoedova, E.; Davis, J.M., 3rd. Comorbidities as Risk Factors for Rheumatoid Arthritis and Their Accrual After Diagnosis. Mayo Clin. Proc. 2019, 94, 2488–2498. [Google Scholar] [CrossRef] [PubMed]
- Appenzeller, S.; Cendes, F.; Costallat, L.T. Epileptic seizures in systemic lupus erythematosus. Neurology 2004, 63, 1808–1812. [Google Scholar] [CrossRef] [PubMed]
- Delalande, S.; De Seze, J.; Fauchais, A.L.; Hachulla, E.; Stojkovic, T.; Ferriby, D.; Dubucquoi, S.; Pruvo, J.P.; Vermersch, P.; Hatron, P.Y. Neurologic manifestations in primary Sjögren syndrome: A study of 82 patients. Medicine 2004, 83, 280–291. [Google Scholar] [CrossRef] [PubMed]
- Ramanan, A.V.; Sawhney, S.; Murray, K.J. Central nervous system complications in two cases of juvenile onset dermatomyositis. Rheumatology 2001, 40, 1293–1298. [Google Scholar] [CrossRef] [PubMed]
- Elst, E.F.; Kamphuis, S.S.M.; Prakken, B.J.; Wulffraat, N.M.; Van Der Net, J.; Peters, A.C.B.; Kuis, W. Case report: Severe central nervous system involvement in juvenile dermatomyositis. J. Rheumatol. 2003, 30, 2059–2063. [Google Scholar] [PubMed]
- Li, G.; Bauer, S.; Nowak, M.; Norwood, B.; Tackenberg, B.; Rosenow, F.; Knake, S.; Oertel, W.H.; Hamer, H.M. Cytokines and epilepsy. Seizure 2011, 20, 249–256. [Google Scholar] [CrossRef] [PubMed]
- El-Hodhod, M.A.; Tomoum, H.Y.; Al-Aziz, M.M.A.; Samaan, S.M. Serum Fas and Bcl-2 in patients with epilepsy. Acta Neurol. Scand. 2006, 113, 315–321. [Google Scholar] [CrossRef]
- Yang, M.; Cen, X.; Xie, Q.; Zuo, C.; Shi, G.; Yin, G. Serum Interleukin-6 Expression Level and Its Clinical Significance in Patients with Dermatomyositis. Clin. Dev. Immunol. 2013, 2013, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, T.; Tomita, Y.; Son, K.; Nishinarita, S.; Sawada, S.; Horie, T. Elevation of serum soluble tumour necrosis factor receptors in patients with polymyositis and dermatomyositis. Clin. Rheumatol. 2000, 19, 352–359. [Google Scholar] [CrossRef]
- Şahin, M.; Aydintug, O.; Tunc, S.; Tutkak, H.; Naziroglu, M.; Aydıntug, O.; Nazıroğlu, M. Serum soluble Fas levels in patients with autoimmune rheumatic diseases. Clin. Biochem. 2007, 40, 6–10. [Google Scholar] [CrossRef]
- Brigo, F.; Igwe, S.C.; Erro, R.; Bongiovanni, L.G.; Marangi, A.; Nardone, R.; Tinazzi, M.; Trinka, E. Postictal serum creatine kinase for the differential diagnosis of epileptic seizures and psychogenic non-epileptic seizures: A systematic review. J. Neurol. 2015, 262, 251–257. [Google Scholar] [CrossRef]
- Nass, R.D.; Sassen, R.; Elger, C.E.; Surges, R. The role of postictal laboratory blood analyses in the diagnosis and prognosis of seizures. Seizure 2017, 47, 51–65. [Google Scholar] [CrossRef]
- Satoh, M.; Tanaka, S.; Ceribelli, A.; Calise, S.J.; Chan, E.K.L. A Comprehensive Overview on Myositis-Specific Antibodies: New and Old Biomarkers in Idiopathic Inflammatory Myopathy. Clin. Rev. Allergy Immunol. 2017, 52, 1–19. [Google Scholar] [CrossRef]
- Cohen, A.D.; Dreiher, J.; Regev-Rosenberg, S.; Yakovson, O.; Lieberman, N.; Goldfracht, M.; Balicer, R.D. The quality indigators program in Clalit Health Services: The first decade. Harefuah 2010, 149, 265. [Google Scholar]
- Bengtsson, C.; Nordmark, B.; Klareskog, L.; Lundberg, I.; Alfredsson, L. Socioeconomic status and the risk of developing rheumatoid arthritis: Results from the Swedish EIRA study. Ann. Rheum. Dis. 2005, 64, 1588–1594. [Google Scholar] [CrossRef]
- Calixto, O.-J.; Anaya, J.-M. Socioeconomic status. The relationship with health and autoimmune diseases. Autoimmun. Rev. 2014, 13, 641–654. [Google Scholar] [CrossRef] [PubMed]
- Findlay, A.R.; Goyal, N.A.; Mozaffar, T. An overview of polymyositis and dermatomyositis. Muscle Nerve 2015, 51, 638–656. [Google Scholar] [CrossRef] [PubMed]
- Vulliemoz, S.; Lurati-Ruiz, F.; Borruat, F.X.; Delavelle, J.; Koralnik, I.J.; Kuntzer, T.; Bogousslavsky, J.; Picard, F.; Landis, T.; Du Pasquier, R.A. Favourable outcome of progressive multifocal leucoencephalopathy in two patients with dermatomyositis. J. Neurol. Neurosurg. Psychiatry 2006, 77, 1079–1082. [Google Scholar] [CrossRef] [PubMed]
- Jimenez, C.; Rowe, P.C.; Keene, D. Cardiac and Central Nervous System Vasculitis in a Child with Dermatomyositis. J. Child. Neurol. 1994, 9, 297–300. [Google Scholar] [CrossRef]
- Regan, M.; Haque, U.; Pomper, M.; Pardo, C.; Stone, J. Central nervous system vasculitis as a complication of refractory dermatomyositis. J. Rheumatol. 2001, 28, 207–211. [Google Scholar] [PubMed]
- Michael, J.R.; Mitch, W.E. Reversible renal failure and myositis caused by phenytoin hypersensitivity. JAMA 1976, 236, 2773–2775. [Google Scholar] [CrossRef]
- Dimachkie, M.M.; Vriesendorp, F.J.; Heck, K.A. Phenytoin-induced dermatomyositis: Case report and literature review. J. Child. Neurol. 1998, 13, 577–580. [Google Scholar] [CrossRef]
- Coupal, T.M.; Chang, D.R.; Pennycooke, K.; Ouellette, H.A.; Munk, P.L. Radiologic Findings in Gabapentin-Induced Myositis. J. Radiol. Case Rep. 2017, 11, 30–37. [Google Scholar] [CrossRef]
- Vezzani, A.; Fujinami, R.S.; White, H.S.; Preux, P.-M.; Blümcke, I.; Sander, J.W.; Löscher, W. Infections, inflammation and epilepsy. Acta Neuropathol. 2016, 131, 211–234. [Google Scholar] [CrossRef] [PubMed]
- Crum-Cianflone, N.F. Bacterial, Fungal, Parasitic, and Viral Myositis. Clin. Microbiol. Rev. 2008, 21, 473–494. [Google Scholar] [CrossRef] [PubMed]
- Zampieri, S.; Ghirardello, A.; Iaccarino, L.; Briani, C.; Sarzi-Puttini, P.; Atzeni, F.; Arienti, S.; Todesco, S.; Doria, A. Polymyositis–dermatomyositis and infections. Autoimmunity 2006, 39, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Serafini, A.; Lukas, R.V.; VanHaerents, S.; Warnke, P.; Tao, J.X.; Rose, S.; Wu, S. Paraneoplastic epilepsy. Epilepsy Behav. 2016, 61, 51–58. [Google Scholar] [CrossRef]
- Britton, J. Autoimmune epilepsy. Neurocutan. Syndromes 2016, 133, 219–245. [Google Scholar] [CrossRef]
- Manganotti, P.; Furlanis, G.; Ajčević, M.; Moras, C.; Bonzi, L.; Pesavento, V.; Stella, A.B. Intravenous immunoglobulin response in new-onset refractory status epilepticus (NORSE) COVID-19 adult patients. J. Neurol. 2021, 1–5. [Google Scholar] [CrossRef]
- Mak, A.; Kow, N.Y. The Pathology of T Cells in Systemic Lupus Erythematosus. J. Immunol. Res. 2014, 2014, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Levy, Y.; Sherer, Y.; George, J.; Rovensky, J.; Lukac, J.; Rauova, L.; Poprac, P.; Langevitz, P.; Fabbrizzi, F.; Shoenfeld, Y. Intravenous immunoglobulin treatment of lupus nephritis. Semin. Arthritis Rheum. 2000, 29, 321–327. [Google Scholar] [CrossRef]
- Nevalainen, O.; Raitanen, J.; Ansakorpi, H.; Artama, M.; Isojärvi, J.; Auvinen, A. Long-term mortality risk by cause of death in newly diagnosed patients with epilepsy in Finland: A nationwide register-based study. Eur. J. Epidemiol. 2013, 28, 981–990. [Google Scholar] [CrossRef]
- Chamorro-Muñoz, M.I.; García-Martín, G.; Pérez-Errazquin, F.; Romero-Acebal, M.; García-Rodríguez, A.; Gutiérrez-Bedmar, M. Epidemiological study of mortality in epilepsy in a Spanish population. Seizure 2017, 46, 19–23. [Google Scholar] [CrossRef]
| Parameters | Entire Population (n = 12,278) | Controls (n = 10,193) | Cases (n = 2085) | Significance | ||
|---|---|---|---|---|---|---|
| Dermatomyositis/Polymyositis (n = 2085) | Dermatomyositis (n = 1475) | Polymyositis (n = 610) | ||||
| Age | 47.81 ± 22.51 | 47.75 ± 22.50 | 48.10 ± 22.56 | 43.68 ± 22.79 | 58.79 ± 17.97 | NS |
| Gender | NS | |||||
| Male | 5042 (41.1%) | 4186 (41.1%) | 856 (41.1%) | 639 (43.3%) | 217 (35.6%) | |
| Female | 7236 (58.9%) | 6007 (58.9%) | 1229 (58.9%) | 836 (56.7%) | 393 (64.4%) | |
| BMI | 26.89 ± 8.20 | 26.93 ± 8.58 | 26.73 ± 6.07 | 26.19 ± 6.03 | 27.88 ± 6.01 | NS |
| SES | NS | |||||
| Low | 5147 (42.1%) | 4277 (42.2%) | 870 (41.9%) | 614 (41.9%) | 256 (42.2%) | |
| Medium | 4454 (36.5%) | 3694 (36.4%) | 760 (36.6%) | 524 (35.7%) | 236 (38.9%) | |
| High | 2616 (21.4%) | 2172 (21.4%) | 444 (21.4%) | 329 (22.4%) | 115 (18.9%) | |
| Smoking | 3695 (30.1%) | 3079 (30.2%) | 616 (29.5%) | 402 (27.3%) | 214 (35.1%) | NS |
| Epilepsy | 189 (1.5%) | 141 (1.4%) | 48 (2.3%) | 28 (1.9%) | 20 (3.3%) | 0.0005 |
| All-cause mortality rate | 466 (3.8%) | 307 (3.0%) | 159 (7.6%) | 115 (7.8%) | 44 (7.2%) | <0.0001 |
| Variable | Coefficient | Standard Error | Wald | p-Value | Odds Ratio | 95% CI |
|---|---|---|---|---|---|---|
| Age | 0.01 | 0.00 | 5.67 | 0.0173 | 1.01 | 1.00 to 1.02 |
| Female vs. male | −0.11 | 0.16 | 0.43 | 0.5137 | 0.90 | 0.66 to 1.23 |
| BMI | 0.00 | 0.01 | 0.02 | 0.8916 | 1.00 | 0.98 to 1.02 |
| Current smoker | −0.02 | 0.17 | 0.01 | 0.9205 | 0.98 | 0.71 to 1.36 |
| SES | ||||||
| Medium | −0.03 | 0.17 | 0.04 | 0.8482 | 0.97 | 0.69 to 1.35 |
| High | −0.25 | 0.21 | 1.40 | 0.2374 | 0.78 | 0.51 to 1.18 |
| Dermatomyositis | 0.41 | 0.21 | 3.69 | 0.0547 | 1.51 | 0.99 to 2.30 |
| Polymyositis | 0.79 | 0.25 | 10.26 | 0.0014 | 2.20 | 1.36 to 3.55 |
| PM/DM | 0.55 | 0.17 | 10.36 | 0.0013 | 1.74 | 1.24 to 2.44 |
| Constant | −4.60 | 0.33 | 192.89 | <0.0001 |
| Variable | Coefficient | Standard Error | Wald | p-Value | Odds Ratio | 95% CI |
|---|---|---|---|---|---|---|
| Anti-SSA | ||||||
| PM/DM | −0.28 | 0.52 | 0.29 | 0.5929 | 0.76 | 0.28 to 2.09 |
| Dermatomyositis | 0.58 | 1.02 | 0.33 | 0.5672 | 1.79 | 0.24 to 13.13 |
| Polymyositis | 1.39 | 1.25 | 1.25 | 0.2639 | 4.03 | 0.35 to 46.49 |
| Anti-SSB | ||||||
| PM/DM | 18.58 | 7396.16 | 0.00 | 0.9980 | 0.00 | |
| Dermatomyositis | 17.56 | 7079.91 | 0.00 | 0.9980 | 0.00 | |
| Polymyositis | 17.59 | 6104.15 | 0.00 | 0.9977 | 0.00 | |
| ANA | ||||||
| PM/DM | 0.27 | 0.36 | 0.54 | 0.4628 | 1.30 | 0.64 to 2.65 |
| Dermatomyositis | −0.01 | 0.51 | 0.00 | 0.9899 | 0.99 | 0.37 to 2.68 |
| Polymyositis | 0.51 | 0.56 | 0.82 | 0.3648 | 1.66 | 0.56 to 4.94 |
| Anti-Jo1 | ||||||
| PM/DM | 0.15 | 0.57 | 0.07 | 0.7962 | 1.16 | 0.38 to 3.57 |
| Dermatomyositis | −19.90 | 9318.37 | 0.00 | 0.9983 | 0.00 | |
| Polymyositis | 0.84 | 0.65 | 1.66 | 0.1972 | 2.31 | 0.65 to 8.20 |
| Anti-RNP | ||||||
| PM/DM | −19.65 | 8059.58 | 0.00 | 0.9981 | 0.00 | |
| Dermatomyositis | −18.78 | 6255.66 | 0.00 | 0.9976 | 0.00 | |
| Polymyositis | −18.38 | 7951.13 | 0.00 | 0.9982 | 0.00 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nissan, E.; Watad, A.; Cohen, A.D.; Sharif, K.; Nissan, J.; Amital, H.; Shovman, O.; Bragazzi, N.L. Epilepsy as a Comorbidity in Polymyositis and Dermatomyositis—A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 3983. https://doi.org/10.3390/ijerph18083983
Nissan E, Watad A, Cohen AD, Sharif K, Nissan J, Amital H, Shovman O, Bragazzi NL. Epilepsy as a Comorbidity in Polymyositis and Dermatomyositis—A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2021; 18(8):3983. https://doi.org/10.3390/ijerph18083983
Chicago/Turabian StyleNissan, Ella, Abdulla Watad, Arnon D. Cohen, Kassem Sharif, Johnatan Nissan, Howard Amital, Ora Shovman, and Nicola Luigi Bragazzi. 2021. "Epilepsy as a Comorbidity in Polymyositis and Dermatomyositis—A Cross-Sectional Study" International Journal of Environmental Research and Public Health 18, no. 8: 3983. https://doi.org/10.3390/ijerph18083983
APA StyleNissan, E., Watad, A., Cohen, A. D., Sharif, K., Nissan, J., Amital, H., Shovman, O., & Bragazzi, N. L. (2021). Epilepsy as a Comorbidity in Polymyositis and Dermatomyositis—A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 18(8), 3983. https://doi.org/10.3390/ijerph18083983








