Validity and Reliability of Self-Assessment Tool for Risk Prioritization Following Exposure to Tuberculosis in a Hospital Setting
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population and Sample
2.2.1. Study Population for Examining Content Validity
2.2.2. The Study Population of Reliability Assessment
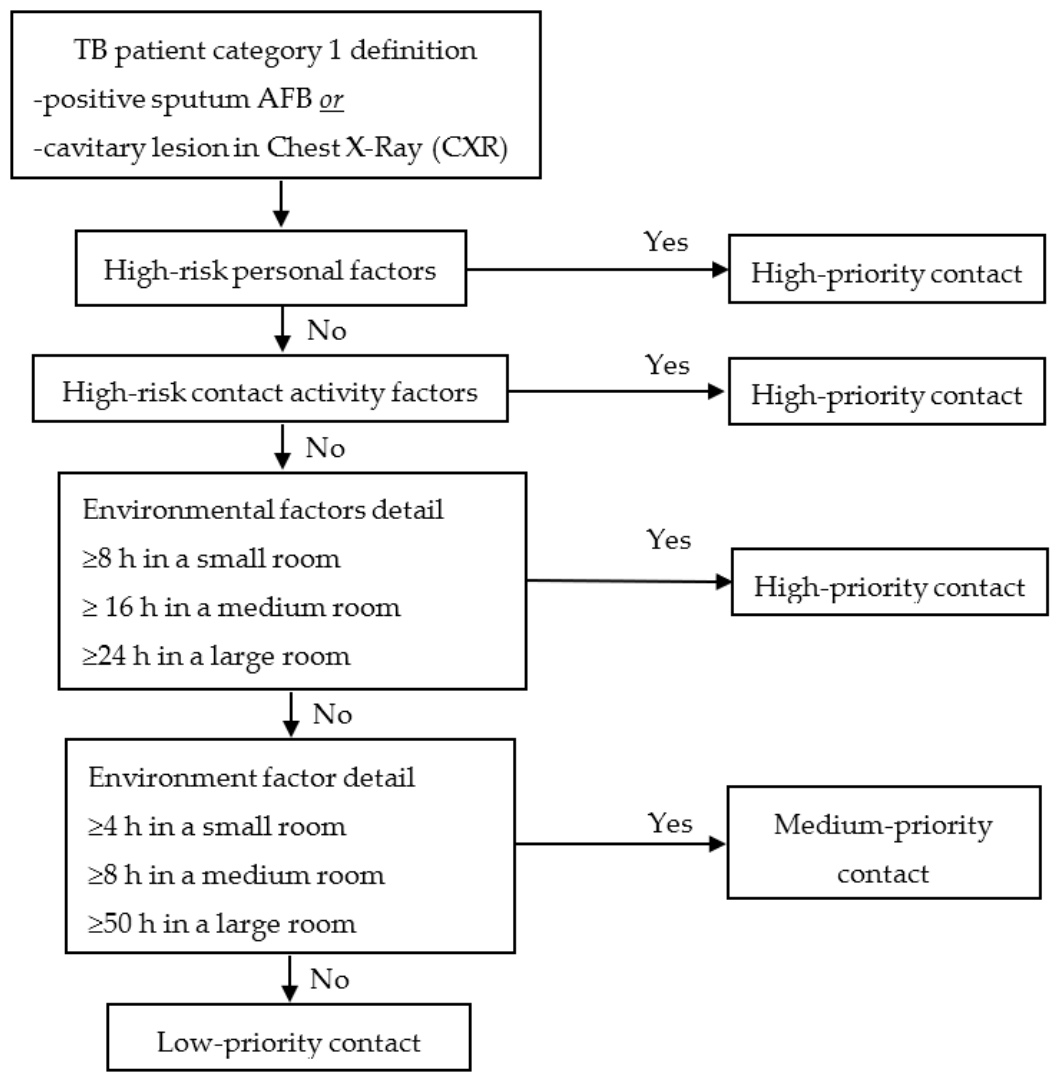
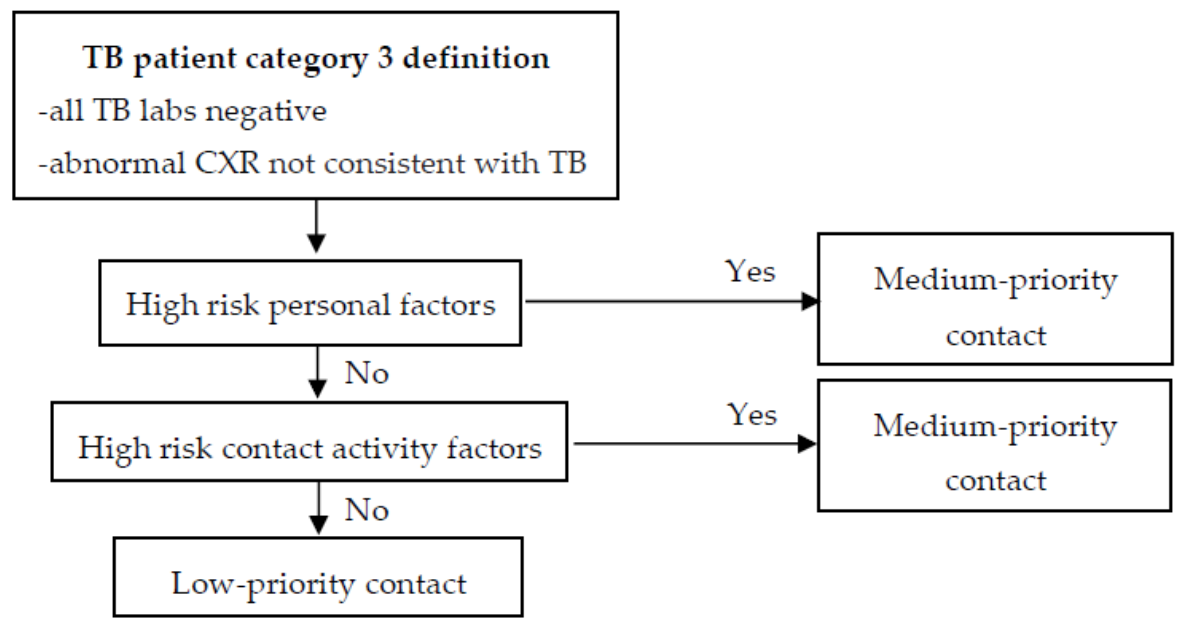
2.3. MSA and PSA
2.4. Study Tool
2.5. Analysis
2.5.1. Content Validity of MSA
2.5.2. Reliability of MSA and PSA
2.6. Ethics
3. Results
3.1. Demographic Data
3.2. Content Validity Assessment of MSA
3.3. Reliability Assessment of MSA and PSA
4. Discussion
4.1. Validity Assessment
4.2. Reliability Assessment
4.2.1. Discussion of Contact Priority Results
4.2.2. Discussion of Personal Factor Results
4.2.3. Discussion of Contact Activity Factor Results
4.2.4. Discussion of Environment Factor Results
4.3. Application
4.4. Limitation and Suggestion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Subject ID…………………..(Identify Index Case: Category 1 ☐ 2 ☐ 3 ☐) Contact Prioritize……….. | |
|---|---|
| Identify Personal Data | |
| |
| Diabetes mellitus End-stage renal disease, with dialysis HIV Malignancy/cancer | Systematic lupus erythematosus Chronic obstructive pulmonary disease (COPD) Bronchiectasis Silicosis |
| ☐ Yes ☐ No | |
| |
| Smoking (not quit) Alcohol abuse (have not quit) Old tuberculosis Body mass index <18.5 kg/m2 (now) | Gastrectomy Jejunoileal bypass surgery Renal transplant |
| ☐ Yes ☐ No | |
| |
| Please identify prescription………………………………………………………………………… | |
| Identify the contact activity with the TB patient and the contact duration of each activity. | |
| ☐ bronchoscopy……………….......……minute(s) ☐ ET-tube intubation …………..……minute(s) ☐ suction………………….…..….……minute(s) ☐ aerosolized medication……….……minute(s) ☐ oxygen therapy ≥3 LPM………..…minute(s) ☐ chest percussion…………….......……minute(s) ☐ sputum collection …………….……minute(s) ☐ airway assist using ambu-bag………minute(s) ☐ chest compression (CPR) …….....…minute(s) ☐ sputum examination…………...……minute(s) ☐ setting a positive pressure ventilator…minute(s) | ☐ setting a high-frequency ventilator…minute(s) ☐ autopsy…………………..…………minute(s) ☐ carry sputum……………….………minute(s) ☐ oral medication………….…………minute(s) ☐ IV medication…………….…………minute(s) ☐ venous puncture………….……..…minute(s) ☐ cleaning the room…………….……minute(s) ☐ bathing in bed………………….……minute(s) ☐ transferring the patient….......….……minute(s) ☐ vital sign assessment……….………minute(s) ☐ talking to the patient……………minute(s) |
| Identify the contact workplace | |
| ☐ Isolated room, ☐ Sputum examination room, ☐ Examination room, ☐ Individual room, ☐ Operation room, ☐ Bronchoscopy room, ☐ X-ray room | ☐ Ward ☐ Intensive care unit (ICU, SICU, CICU, PICU) ☐ Emergency room ☐ OPD station ☐ Recovery room ☐ Hall ☐ Large conference room |
| Subject ID…………………..(Identify Index Case: Category 1 ☐ 2 ☐ 3 ☐) Contact Prioritize……….. | |||
|---|---|---|---|
| Identify Personal Data | |||
| |||
| Diabetes mellitus HIV Chronic renal failure | |||
| ☐ Yes ☐ No | |||
| Identify the contact activity with the TB patient and the contact duration of each activity. | |||
| ☐ bronchoscopy ☐ ET-tube intubation ☐ suction | ☐ chest compression (CPR) ☐ sputum induction | ||
| Identify the contact duration, contact workplace | |||
| How long was your contact activity with the TB patient? | |||
| ☐ ≤4 h ☐ 4–8 h | ☐ 8–16 h ☐ 16–24 h | ☐ 24–50 h ☐ ≥50 h | |
| Where was the contact place? | |||
| ☐ Operation room ☐ Bronchoscopy room ☐ Isolated room ☐ Individual room | ☐ Recovery room ☐ Resuscitation room ☐ Hall ☐ Large conference room | ||
| Personal factors | These Underlying Diseases Are a Risk of Active TB. | Expert Opinion | |||
| Strongly Agree | Agree | Disagree | Strongly Disagree | ||
| HIV | 1 2 3 4 5 6 7 | ||||
| Diabetes mellitus (DM) | 1 2 3 4 5 6 7 | ||||
| End stage renal disease (ESRD) with dialysis | 1 2 3 4 | 5 6 7 | |||
| Chronic obstructive pulmonary disease (COPD) | 1 3 4 5 | 2 6 7 | |||
| Bronchiectasis | 1 | 2 3 4 5 7 | 6 | ||
| Any malignancy/cancer | 1 2 4 | 3 5 6 7 | |||
| Systematic lupus erythematosus (SLE) | 1 2 3 5 7 | 4 6 | |||
| Silicosis | 1 2 3 4 5 6 7 | ||||
| These health statuses are a risk of active TB. | Expert opinion | ||||
| Strongly agree | Agree | Disagree | Strongly disagree | ||
| smoking | 1 2 3 7 | 4 5 6 | |||
| Alcohol abuse | 1 | 2 3 4 5 6 7 | |||
| Old pulmonary TB | 1 2 3 4 7 | 5 6 | |||
| BMI < 18.5 kg/m2 | 1 2 3 4 6 7 | 5 | |||
| Gastrectomy | 1 | 2 3 4 5 6 7 | |||
| Jejunoileal bypass surgery | 1 2 3 4 5 6 7 | ||||
| Renal transplant | 1 2 3 | 4 5 6 7 | |||
| These medications are a risk of active TB | Expert opinion | ||||
| Strongly agree | Agree | Disagree | Strongly disagree | ||
| Corticosteroids ≥15 mg daily for >4 weeks | 1 2 3 4 5 6 7 | ||||
| Multiple cancer chemotherapy agents | 1 2 3 4 5 6 7 | ||||
| Antirejection drugs for organ transplants | 1 2 3 4 5 6 7 | ||||
| Tumor necrosis factor alpha antagonists | 1 2 3 4 5 6 7 | ||||
| Contact activities | These contact activities are at high-risk of latent TB infection | Expert opinion | |||
| Strongly agree | Agree | Disagree | Strongly disagree | ||
| Bronchoscopy | 1 2 3 4 5 6 7 | ||||
| ET-tube intubation | 1 2 3 4 5 6 7 | ||||
| Suction | 1 2 3 4 5 6 7 | ||||
| Autopsy pulmonary TB patient | 1 2 3 4 5 6 | 7 | |||
| Aerosolized medication | 1 3 4 7 | 2 5 6 | |||
| Oxygen therapy ≥3 LPM | 1 3 | 2 4 5 6 7 | |||
| Chest percussion | 1 2 3 4 5 6 7 | ||||
| Sputum collection | 1 2 3 4 5 6 7 | ||||
| Carry sputum (bring sputum container to lab) | 1 2 3 4 5 7 | 6 | |||
| Airway assist using ambu-bag | 1 3 4 | 2 5 6 7 | |||
| Chest compression (CPR) | 1 2 3 4 5 6 7 | ||||
| Sputum examination in laboratory | 5 6 | 1 2 3 4 7 | |||
| Setting a positive pressure ventilator | 1 2 3 4 5 6 7 | ||||
| Setting a high-frequency ventilator | 1 2 3 4 5 6 7 | ||||
| These contact activities are at low risk of latent TB infection | Expert opinion | ||||
| Strongly agree | Agree | Disagree | Strongly disagree | ||
| Oral medication | 1 2 3 4 5 6 7 | ||||
| IV medication | 1 2 3 4 5 6 7 | ||||
| Venous puncture | 1 2 3 4 5 6 7 | ||||
| Cleaning room | 1 2 4 | 3 5 6 | 7 | ||
| Bathing patient in bed | 1 2 3 4 | 5 7 | 6 | ||
| Transferring patient | 1 2 3 4 | 6 7 | 5 | ||
| Vital sign assessment | 1 2 3 4 | 6 7 | 5 | ||
| Talking to the patient | 1 2 3 4 5 6 | 7 | |||
| Environment factors | These rooms are of small size, which carries a high risk of LTBI. | Expert opinion | |||
| Strongly agree | Agree | Disagree | Strongly disagree | ||
| Isolated room | 1 2 3 4 5 6 7 | ||||
| Examination room | 1 2 3 4 | 5 7 | 6 | ||
| Individual room | 1 2 3 | 4 5 7 | 6 | ||
| Bronchoscopy room | 5 6 7 | 1 2 3 | 4 | ||
| Sputum examination room | 5 6 7 | 1 2 3 4 | |||
| Operation room | 1 2 3 4 5 7 | 6 | |||
| X-ray room | 1 2 3 4 5 7 | 6 | |||
| These rooms are of medium size, which carries a medium risk of LTBI | Experts opinion | ||||
| Strongly agree | Agree | Disagree | Strongly disagree | ||
| Intensive care unit (ICU, SICU, CCU) | 1 2 3 4 5 6 7 | ||||
| Ward | 1 2 3 4 5 6 | 7 | |||
| Emergency room | 1 2 3 4 5 6 | 7 | |||
| OPD station | 5 6 7 | 2 3 4 | 1 | ||
| Recovery room | 6 7 | 1 2 4 5 | 3 | ||
| These rooms are of large size, which carries a low risk of LTBI | Experts opinion | ||||
| Strongly agree | agree | disagree | Strongly disagree | ||
| Hall | 1 2 3 4 5 6 7 | ||||
| Large conference room | 1 2 3 4 5 6 7 | ||||
| MSA | Experts | Number of Agreement (%) | PSA | Experts | Number of Agreement (%) |
|---|---|---|---|---|---|
| High | High | 44 (40.7) | High | High | 34 (31.5) |
| High | Medium | 0 | High | Medium | 2 (1.9) |
| High | Low | 6 (5.6) | High | Low | 8 (7.4) |
| Medium | High | 0 | Medium | High | 4 (3.7) |
| Medium | Medium | 4 (3.7) | Medium | Medium | 2 (1.9) |
| Medium | Low | 2 (1.9) | Medium | Low | 1 (0.9) |
| Low | High | 2 (1.9) | Low | High | 8 (7.4) |
| Low | Medium | 2 (1.9) | Low | Medium | 2 (1.9) |
| Low | Low | 48 (44.4) | Low | Low | 47 (43.5) |
| Total agreement | 96 (88.9) | Total agreement | 83 (76.8) | ||
| Kappa (95% CI) | 0.80 (95% CI: 0.70, 0.90) | Kappa (95% CI) | 0.58 (95% CI: 0.44, 0.72) | ||
| Expert | TI | ||||
|---|---|---|---|---|---|
| High | Medium | Low | |||
| MSA | High | 44 | 0 | 6 | 50 |
| Medium | 0 | 4 | 2 | 8 | |
| Low | 2 | 2 | 48 | 52 | |
| Ui | 46 | 8 | 56 | ||
References
- World Health Organization. Global Tuberculosis Report 2018; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Stop TB Partnership. The Paradigm Shift 2016–2020—Global Plan to end TB (Document); World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Uden, L.; Barber, E.; Ford, N.; Cooke, G.S. Risk of tuberculosis infection and disease for health care workers: An updated meta-analysis. Open Forum Infect. Dis. 2017, 4, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Scano, F.; Cadman, H. WHO Policy on TB Infection Control in Health-Care Facilities, Congregate Settings, and Households; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Jong Lee, K.; Ae Kang, Y.; Mi Kim, Y.; Cho, S.N.; Wook Moon, J.; Suk Park, M.; Kyu Kim, S.; Chang, J.; Sam Kim, Y. Screening for latent tuberculosis infection in South Korean healthcare workers using a tuberculin skin test and whole blood interferon-gamma assay. Scand. J. Infect. Dis. 2010, 42, 672–678. [Google Scholar] [CrossRef] [PubMed]
- Paton, N.I.; Borand, L.; Benedicto, J.; Kyi, M.M.; Mahmud, A.M.; Norazmi, M.N.; Sharma, N.; Chuchottaworn, C.; Huang, Y.W.; Kaswandani, N.; et al. Diagnosis and management of latent tuberculosis infection in Asia: Review of current status and challenges. Int. J. Infect. Dis. 2019, 87, 21–29. [Google Scholar] [CrossRef] [Green Version]
- Centers for Disease Control and Prevention. TB Screening and Testing of Health Care Personnel. Available online: https://kku.world/qnl09 (accessed on 13 June 2019).
- Ogunremi, T.; Menzies, D.; Embil, J. Prevention and control of tuberculosis transmission in health care and other settings. In Canadian Tuberculosis Standards; Menzies, D., Ed.; Public Health Agency of Canada: Winnipeg, MB, Canada, 2014; pp. 361–404. [Google Scholar]
- Mullie, G.A.; Schwartzman, K.; Zwerling, A.; N′Diaye, D.S. Revisiting annual screening for latent tuberculosis infection in healthcare workers: A cost-effectiveness analysis. BMC Med. 2017, 15, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Panthong, J.; Chaiear, C.; Jonkumcho, W.; Janpho, P. In a hospital setting, is there any benefit in prioritizing risk following exposure to tuberculosis-a preliminary report. J. Med. Assoc. Thai. 2019, 102, S27–S32. [Google Scholar]
- National Tuberculosis Controllers Association. Centers for disease control and prevention guidelines for the investigation of contacts of persons with infectious tuberculosis. Recommendations from the National Tuberculosis Controllers Association and CDC. MMWR Recomm. Rep. 2005, 54, 1–47. [Google Scholar]
- O′Malley, M.; Brown, A.G.; Colmers, J.M. Maryland TB Guidelines for Prevention and Treatment of Tuberculosis; Maryland Department of Health and Mental Hygiene: Baltimore, MD, USA, 2007.
- Cantor, A.B. Sample-size calculations for Cohen′s kappa. Psychol. Methods 1996, 1, 150–153. [Google Scholar] [CrossRef]
- Apriani, L.; McAllister, S.; Sharples, K.; Alisjahbana, B.; Ruslami, R.; Hill, P.C.; Menzies, D. Latent tuberculosis infection in healthcare workers in low and middle-income countries: An updated systematic review. Eur. Respir. J. 2019, 53, 1801789. [Google Scholar] [CrossRef]
- Casas, I.; Esteve, M.; Guerola, R.; García-Olivé, I.; Roldán-Merino, J.; Martinez-Rivera, C.; Ruiz-Manzano, J. Incidence of tuberculosis infection among healthcare workers: Risk factors and 20-year evolution. Respir. Med. 2013, 107, 601–607. [Google Scholar] [CrossRef] [Green Version]
- Mathew, A.; David, T.; Thomas, K.; Kuruvilla, P.J.; Balaji, V.; Jesudason, M.V.; Samuel, P. Risk factors for tuberculosis among health care workers in South India: A nested case–control study. J. Clin. Epidemiol. 2013, 66, 67–74. [Google Scholar] [CrossRef]
- Rafiza, S.; Rampal, K.G.; Tahir, A. Prevalence and risk factors of latent tuberculosis infection among health care workers in Malaysia. BMC Infect. Dis. 2011, 11, 19. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Latent Tuberculosis Infection: Updated and Consolidated Guidelines for Programmatic Management; WHO: Geneva, Switzerland, 2018; ISBN 978-92-4-155023-9. [Google Scholar]
- Polit, D.F.; Beck, C.T. The content validity index: Are you sure you know what’s being reported? Critique and recommendations. Res. Nurs. Health 2006, 29, 489–497. [Google Scholar] [CrossRef] [Green Version]
- McHugh, M.L. Interrater reliability: The Kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Davies, A.; Thomson, G.; Walker, J.; Bennett, A. A review of the risks and disease transmission associated with aerosol generating medical procedures. J. Infect. Prev. 2009, 10, 122–126. [Google Scholar] [CrossRef]
- Jackson, T.; Deibert, D.; Wyatt, G.; Durand-Moreau, Q.; Adisesh, A.; Khunti, K.; Khunti, S.; Smith, S.; Chan, X.H.S.; Ross, L.; et al. Classification of aerosol-generating procedures: A rapid systematic review. BMJ Open Respir. Res. 2020, 7, e000730. [Google Scholar] [CrossRef]
- Chanpho, P.; Chaiear, N.; Kamsa-Ard, S. Factors associated with latent tuberculosis infection among the hospital employees in a tertiary hospital of Northeastern Thailand. Int. J. Environ. Res. Public Health 2020, 17, 6876. [Google Scholar] [CrossRef]
- Lee, J.Y. Tuberculosis infection control in health-care facilities: Environmental control and personal protection. Tuberc. Respir. Dis. 2016, 79, 234–240. [Google Scholar] [CrossRef]
- Mendes, M.A.; Gaio, R.; Reis, R.; Duarte, R. Contact screening in tuberculosis: Can we identify those with higher risk? Eur. Respir. J. 2013, 41, 758–760. [Google Scholar] [CrossRef] [Green Version]
- Zhou, F.; Zhang, L.; Gao, L.; Hao, Y.; Zhao, X.; Liu, J.; Lu, J.; Li, X.; Yang, Y.; Chen, J.; et al. Latent tuberculosis infection and occupational protection among health care workers in two types of public hospitals in China. PLoS ONE 2014, 9, e104673. [Google Scholar] [CrossRef] [Green Version]
- Sawanyawisuth, K.; Chaiear, N.; Sawanyawisuth, K.; Limpawattana, P.; Bourpoern, J.; Reechaipichitkul, W. Can job titles be predictors for recent onset latent tuberculosis in health care workers? Asian Biomed. Res. Rev. News 2012, 6, 534–539. [Google Scholar]
- Trakultaweesuk, P.; Niyompattama, A.; Boonbamroe, S.; Chaiear, N. Tuberculosis among hospital staffs in a tertiary care hospital Northeastern Thailand. Srinagarind. Med. J. 2017, 32, 204–213. [Google Scholar]
- Xie, Z.; Zhou, N.; Chi, Y.; Huang, G.; Wang, J.; Gao, H.; Xie, N.; Ma, Q.; Yang, N.; Duan, Z.; et al. Nosocomial tuberculosis transmission from 2006 to 2018 in Beijing Chest Hospital, China. Antimicrob. Resist. Infect. Control. 2020, 9, 165. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Number (n) | Percentage |
|---|---|---|
| Sex | ||
| Female | 93 | 86.11 |
| Male | 15 | 13.89 |
| Total | 108 | 100 |
| Job title | ||
| Nurses | 55 | 50.93 |
| Nurses’ assistants | 22 | 20.37 |
| Medical technicians | 16 | 14.81 |
| Healthcare assistants | 8 | 7.41 |
| Technicians | 5 | 4.63 |
| Ward workers | 1 | 0.93 |
| Physiotherapists | 1 | 0.93 |
| Total | 108 | 100 |
| Contact workplace | ||
| Inpatient department | 48 | 44.44 |
| Intensive care unit | 25 | 23.15 |
| Laboratory unit | 21 | 19.44 |
| Outpatient department | 11 | 10.19 |
| Operative unit | 3 | 2.78 |
| Total | 108 | 100 |
| Factors | Priorities | Items | I-CVI | S-CVI/Ave | |
|---|---|---|---|---|---|
| Personal | Underlying disease | High risk of aTB | HIV, DM, ESRD with dialysis, silicosis, COPD, cancer, SLE | 1 | 0.99 |
| bronchiectasis | 0.86 | ||||
| Health status | High risk of aTB | smoking, alcohol abuse, old pulmonary TB, gastrectomy, jejunoileal bypass surgery, renal transplant, | 1 | ||
| BMI < 18.5 kg/m2 | 0.86 | ||||
| Medication | High risk of aTB | corticosteroids ≥15 mg daily for >4 weeks, multiple cancer chemotherapy agents, antirejection drugs for organ transplants, tumor necrosis factor alpha antagonists | 1 | ||
| Contact activity | High risk of LTBI | bronchoscopy, ET-tube intubation, suction, aerosolized medication, oxygen therapy ≥3 LPM, chest percussion, sputum collection, airway assist using ambu-bag, chest compression, sputum examination, setting a positive pressure ventilator, setting a high-frequency ventilator | 1 | 0.96 | |
| autopsy, carry sputum | 0.86 | ||||
| Low risk of LTBI | oral medication, IV medication, venous puncture | 1 | |||
| cleaning room, bathing in bed, transferring patient, vital sign assessment, talking to patients | 0.86 | ||||
| Environment | Room size | Small size | isolated room, sputum examination room | 1 | 0.91 |
| examination room, individual room, operation room, bronchoscopy room, X-ray room | 0.86 | ||||
| Medium size | intensive care unit (ICU, SICU, CCU) | 1 | |||
| ward, emergency room, OPD station, recovery room | 0.86 | ||||
| Large size | hall, large conference room | 1 | |||
| Contact Priority | MSA | Expert | Agreement | PSA | Expert | Agreement |
|---|---|---|---|---|---|---|
| High | 50 | 46 | 44 | 44 | 46 | 34 |
| Moderate | 6 | 6 | 4 | 7 | 6 | 2 |
| Low | 52 | 56 | 48 | 57 | 56 | 47 |
| Total | 108 | 96 | 108 | 83 | ||
| Kappa (95% CI) | 0.80 (95% CI: 0.70, 0.90) | 0.58 (95% CI: 0.44, 0.72) | ||||
| Factors | Priorities | MSA | Expert | Agreement | PSA | Expert | Agreement | |
|---|---|---|---|---|---|---|---|---|
| Personal | Underlying disease | High risk of aTB | 8 | 8 | 7 | 5 | 8 | 4 |
| Low risk of aTB | 100 | 100 | 99 | 103 | 100 | 99 | ||
| Total (n) | 108 | 106 | 108 | 103 | ||||
| Kappa (95% CI) | 0.87 (95% CI: 0.77, 0.96) | 0.59 (95% CI: 0.43, 0.76) | ||||||
| Health status | High risk of aTB | 11 | 7 | 6 | non | 7 | - | |
| Low risk of aTB | 97 | 101 | 96 | non | 101 | - | ||
| Total (n) | 108 | 102 | 108 | - | ||||
| Kappa (95% CI) | 0.64 (95% CI: 0.37, 0.91) | - | ||||||
| Medication | High risk of aTB | 1 | 1 | 1 | non | 1 | - | |
| Low risk of aTB | 107 | 107 | 107 | non | 107 | - | ||
| Total (n) | 108 | 108 | 108 | - | ||||
| Kappa (95% CI) | 1 | - | ||||||
| Contact activity | High risk of LTBI | 42 | 30 | 30 | 33 | 30 | 28 | |
| Low risk of LTBI | 66 | 78 | 66 | 75 | 78 | 73 | ||
| Total (n) | 108 | 96 | 108 | 101 | ||||
| Kappa (95% CI) | 0.75 (95% CI: 0.62, 0.88) | 0.84 (95% CI: 0.73, 0.95) | ||||||
| Environment | Contact duration | ≤4 h | 67 | 72 | 59 | 49 | 72 | 45 |
| 4–8 h | 9 | 15 | 5 | 17 | 15 | 4 | ||
| 8–16 h | 16 | 12 | 8 | 8 | 12 | 3 | ||
| 16–24 h | 8 | 3 | 3 | 8 | 3 | 1 | ||
| 24–50 h | 5 | 1 | 1 | 16 | 1 | 0 | ||
| ≥50 h | 3 | 5 | 2 | 10 | 5 | 0 | ||
| Total (n) | 108 | 78 | 108 | 53 | ||||
| Kappa (95% CI) | 0.50 (95% CI: 0.36, 0.64) | 0.23 (95% CI: 0.13, 0.33) | ||||||
| Room size | Small size | 42 | 45 | 39 | 36 | 45 | 31 | |
| Medium size | 51 | 43 | 38 | 51 | 43 | 33 | ||
| Large size | 15 | 20 | 11 | 21 | 20 | 14 | ||
| Total (n) | 108 | 88 | 108 | 78 | ||||
| Kappa (95% CI) | 0.70 (95% CI: 0.59, 0.81) | 0.56 (95% CI: 0.43, 0.69) | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sirinapakul, P.; Chaiear, N.; Krisorn, P. Validity and Reliability of Self-Assessment Tool for Risk Prioritization Following Exposure to Tuberculosis in a Hospital Setting. Int. J. Environ. Res. Public Health 2021, 18, 3981. https://doi.org/10.3390/ijerph18083981
Sirinapakul P, Chaiear N, Krisorn P. Validity and Reliability of Self-Assessment Tool for Risk Prioritization Following Exposure to Tuberculosis in a Hospital Setting. International Journal of Environmental Research and Public Health. 2021; 18(8):3981. https://doi.org/10.3390/ijerph18083981
Chicago/Turabian StyleSirinapakul, Piyapong, Naesinee Chaiear, and Phanumas Krisorn. 2021. "Validity and Reliability of Self-Assessment Tool for Risk Prioritization Following Exposure to Tuberculosis in a Hospital Setting" International Journal of Environmental Research and Public Health 18, no. 8: 3981. https://doi.org/10.3390/ijerph18083981
APA StyleSirinapakul, P., Chaiear, N., & Krisorn, P. (2021). Validity and Reliability of Self-Assessment Tool for Risk Prioritization Following Exposure to Tuberculosis in a Hospital Setting. International Journal of Environmental Research and Public Health, 18(8), 3981. https://doi.org/10.3390/ijerph18083981







