Exploring Quality of Life, Stress, and Risk Factors Associated with Irritable Bowel Syndrome for Female University Students in Taiwan
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Participants and Setting
2.3. Data Collection and Ethecial Consideration
2.4. Instruments
2.4.1. The Demographic Characteristics Questionnaire
2.4.2. The Chinese Version of the Rome III Criteria for Functional Gastrointestinal Disorder Questionnaire
2.4.3. The IBS Symptom Severity Scale (IBS-SSS)
2.4.4. The Perceived Stress Scale (PSS)
2.4.5. The World Health Organization Quality of Life-BREF Questionnaire (WHOQOL-BREF)
2.5. Statistical Analysis
3. Results
3.1. Participants’ Demographic Characteristics
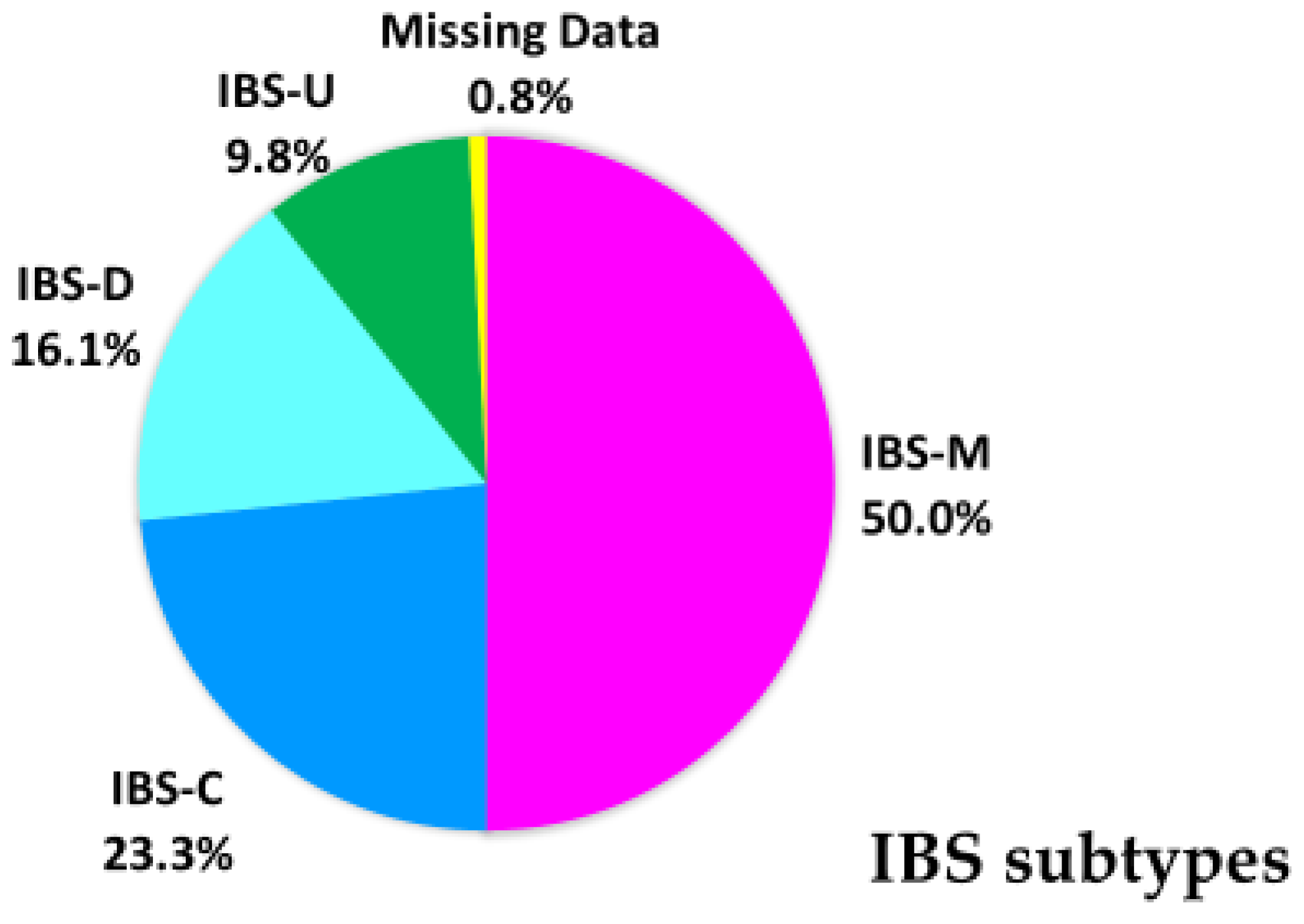
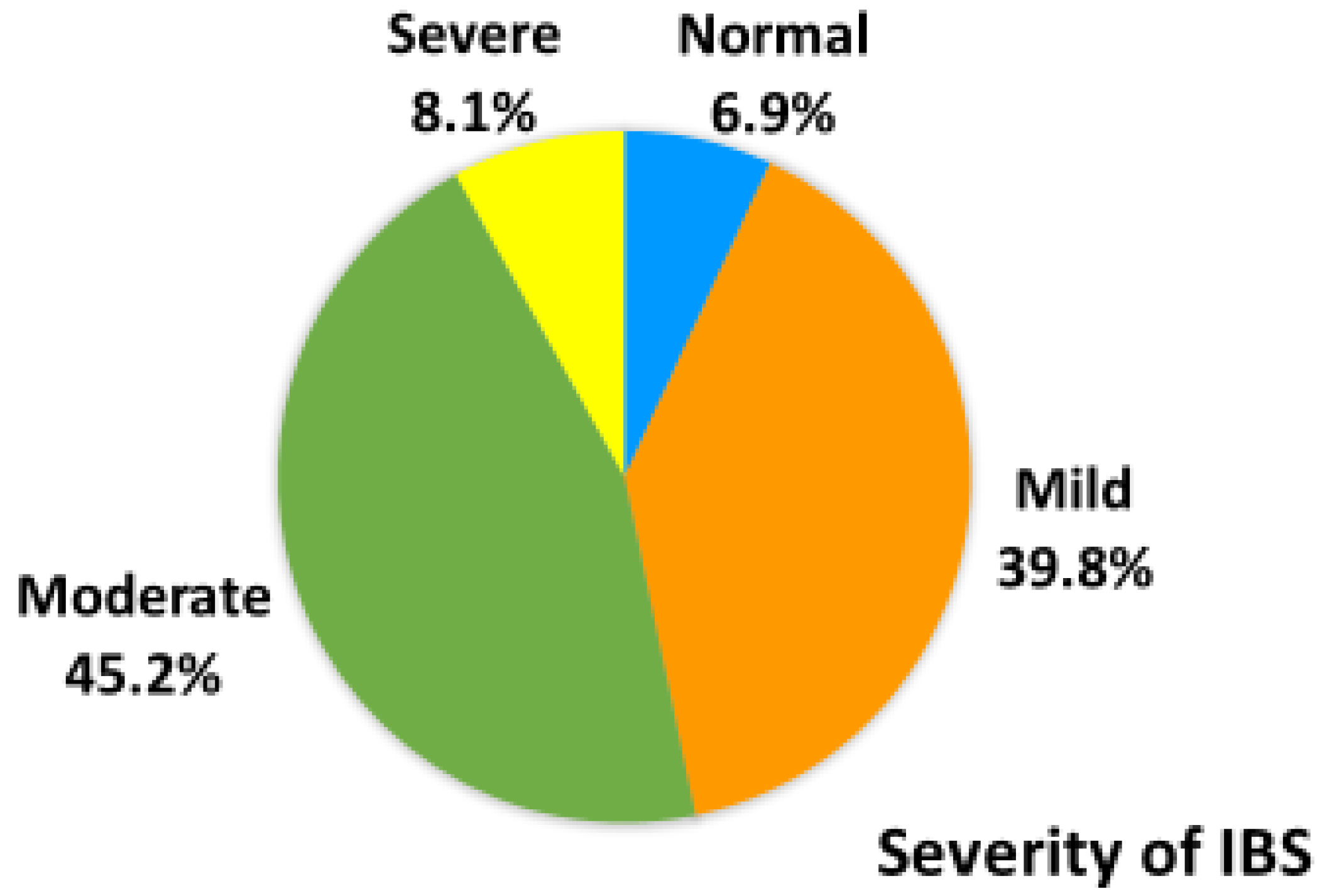
3.2. Prevalence of IBS and Severity of IBS
3.3. Demographic Characteristics of Female Students with or without Irritable Bowel Syndrome
3.4. The Levels of Stress and QOL between Female Students with and without IBS
3.5. The Risk Factors for IBS of Female Students
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Enck, P.; Aziz, Q.; Barbara, G.; Farmer, A.D.; Fukudo, S.; Mayer, E.A.; Niesler, B.; Quigley, E.M.M.; Rajilić-Stojanović, M.; Schemann, M.; et al. Irritable bowel syndrome. Nat. Rev. Dis. Prim. 2016, 2, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Lovell, R.M.; Ford, A.C. Global Prevalence of and Risk Factors for Irritable Bowel Syndrome: A Meta-analysis. Clin. Gastroenterol. Hepatol. 2012, 10, 712–721.e4. [Google Scholar] [CrossRef]
- Sperber, A.D.; Dumitrascu, D.; Fukudo, S.; Gerson, C.; Ghoshal, U.C.; Gwee, K.A.; Hungin, A.P.S.; Kang, J.-Y.; Minhu, C.; Schmulson, M.; et al. The global prevalence of IBS in adults remains elusive due to the heterogeneity of studies: A Rome Foundation working team literature review. Gut 2017, 66, 1075–1082. [Google Scholar] [CrossRef]
- Lu, C.-L.; Chen, C.-Y.; Lang, H.-C.; Luo, J.-C.; Wang, S.-S.; Chang, F.-Y.; Lee, S.-D. Current patterns of irritable bowel syndrome in Taiwan: The Rome II questionnaire on a Chinese population. Aliment. Pharmacol. Ther. 2003, 18, 1159–1169. [Google Scholar] [CrossRef] [PubMed]
- American College of Gastroenterology IBS Task Force; Brandt, L.J.; Chey, W.D.; E. Foxx-Orenstein, A.; Quigley, E.M.M.; Schiller, L.R.; Schoenfeld, P.S.; Spiegel, B.M.; Talley, N.J.; Moayyedi, P. An Evidence-Based Position Statement on the Management of Irritable Bowel Syndrome. Am. J. Gastroenterol. 2008, 104, S1–S35. [Google Scholar] [CrossRef]
- Frändemark, Å; Törnblom, H.; Jakobsson, S.; Simrén, M. Work Productivity and Activity Impairment in Irritable Bowel Syndrome (IBS): A Multifaceted Problem. Am. J. Gastroenterol. 2018, 113, 1540–1549. [Google Scholar] [CrossRef]
- Balmus, I.M. Perceived Stress and Gastrointestinal Habits in College Students. ACTA Endocrinol. 2019, 15, 274–275. [Google Scholar] [CrossRef]
- Shen, L.; Kong, H.; Hou, X. Prevalence of irritable bowel syndrome and its relationship with psychological stress status in Chinese university students. J. Gastroenterol. Hepatol. 2009, 24, 1885–1890. [Google Scholar] [CrossRef]
- Ford, A.C.; Forman, D.; Bailey, A.G.; Axon, A.T.R.; Moayyedi, P. Irritable Bowel Syndrome: A 10-Yr Natural History of Symptoms and Factors That Influence Consultation Behavior. Am. J. Gastroenterol. 2008, 103, 1229–1239. [Google Scholar] [CrossRef]
- Gralnek, I.M.; Hays, R.D.; Kilbourne, A.; Naliboff, B.; Mayer, E.A. The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology 2000, 119, 654–660. [Google Scholar] [CrossRef]
- Kanuri, N.; Cassell, B.; Bruce, S.E.; White, K.S.; Gott, B.M.; Gyawali, C.P.; Sayuk, G.S. The impact of abuse and mood on bowel symptoms and health-related quality of life in irritable bowel syndrome (IBS). Neurogastroenterol. Motil. 2016, 28, 1508–1517. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.-Y.; Zuo, X.-L.; Li, C.-Q.; Yu, Y.-B.; Zhao, Q.-J.; Li, Y.-Q. Prevalence of irritable bowel syndrome in Chinese college and university students assessed using Rome III criteria. World J. Gastroenterol. 2010, 16, 4221–4226. [Google Scholar] [CrossRef] [PubMed]
- Dai, N.; Cong, Y.; Yuan, H. Prevalence of irritable bowel syndrome among undergraduates in Southeast China. Dig. Liver Dis. 2008, 40, 418–424. [Google Scholar] [CrossRef] [PubMed]
- Sugaya, N.; Nomura, S. Relationship between cognitive appraisals of symptoms and negative mood for subtypes of irritable bowel syndrome. Biopsychosoc. Med. 2008, 2, 9. [Google Scholar] [CrossRef]
- Tayama, J.; Nakaya, N.; Hamaguchi, T.; Tomiie, T.; Shinozaki, M.; Saigo, T.; Shirabe, S.; Fukudo, S. Effects of personality traits on the manifestations of irritable bowel syndrome. Biopsychosoc. Med. 2012, 6, 20. [Google Scholar] [CrossRef] [PubMed]
- Jane, Z.-Y.; Chang, C.-C.; Lin, H.-K.; Liu, Y.-C.; Chen, W.-L. The Association Between the Exacerbation of Irritable Bowel Syndrome and Menstrual Symptoms in Young Taiwanese Women. Gastroenterol. Nurs. 2011, 34, 277–286. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regres-sion analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Liu, L.; Xiao, Q.-F.; Zhang, Y.-L.; Yao, S.-K. A cross-sectional study of irritable bowel syndrome in nurses in China: Prevalence and associated psychological and lifestyle factors. J. Zhejiang Univ. Sci. B 2014, 15, 590–597. [Google Scholar] [CrossRef]
- Longstreth, G.F.; Thompson, W.G.; Chey, W.D.; Houghton, L.A.; Mearin, F.; Spiller, R.C. Functional Bowel Disorders. Gastroenterology 2006, 130, 1480–1491. [Google Scholar] [CrossRef] [PubMed]
- Francis, C.Y.; Morris, J.; Whorwell, P.J. The irritable bowel severity scoring system: A simple method of monitoring irritable bowel syndrome and its progress. Aliment. Pharmacol. Ther. 1997, 11, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Chu, L.C.; Kao, S.R. The moderation of meditation experience and emotional intelligence on the relationship between perceived stress and negative mental health. Chin. J. Psychol. 2005, 47, 157–179. [Google Scholar] [CrossRef]
- The Whoqol Group Development of the World Health Organization WHOQOL-BREF Quality of Life Assessment. Psychol. Med. 1998, 28, 551–558. [CrossRef] [PubMed]
- Yao, G.; Chung, C.-W.; Yu, C.-F.; Wang, J.-D. Development and verification of validity and reliability of the WHOQOL-BREF Taiwan version. J. Formos. Med. Assoc. 2002, 101, 342–351. [Google Scholar] [PubMed]
- Wang, Y.; Jin, F.; Chi, B.; Duan, S.; Zhang, Q.; Liu, Y.; Hao, W.; Sun, J. Gender differences in irritable bowel syndrome among medical students at Inner Mongolia Medical University, China: A cross-sectional study. Psychol. Health Med. 2016, 21, 964–974. [Google Scholar] [CrossRef] [PubMed]
- AlButaysh, O.F.; AlQuraini, A.A.; Almukhaitah, A.A.; Alahmdi, Y.M.; Alharbi, F.S. Epidemiology of irritable bowel syndrome and its associated factors in Saudi undergraduate students. Saudi J. Gastroenterol. 2020, 26, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, N.K.R.; Battarjee, W.F.; Almehmadi, S.A. Prevalence and predictors of irritable bowel syndrome among medical students and interns in King Abdulaziz University, Jeddah. Libyan J. Med. 2013, 8, 21287. [Google Scholar] [CrossRef]
- Govindaraja, C.; Chandramouli, A.; Winn, T.; Min, A.; JaiPrakash, H.; Patil, A.; Kale, S.; Sornam, S. Prevalence of Irritable Bowel Syndrome and Its Imprint on the Quality of Life of Undergraduate Students at a Malaysian Medical University. J. Adv. Med. Med. Res. 2018, 26, 1–13. [Google Scholar] [CrossRef]
- Singh, R.K.; Chang, H.-W.; Yan, D.; Lee, K.M.; Ucmak, D.; Wong, K.; Abrouk, M.; Farahnik, B.; Nakamura, M.; Zhu, T.H.; et al. Influence of diet on the gut microbiome and implications for human health. J. Transl. Med. 2017, 15, 1–17. [Google Scholar] [CrossRef]
- O’Mahony, S.M.; Marchesi, J.R.; Scully, P.; Codling, C.; Ceolho, A.-M.; Quigley, E.M.; Cryan, J.F.; Dinan, T.G. Early Life Stress Alters Behavior, Immunity, and Microbiota in Rats: Implications for Irritable Bowel Syndrome and Psychiatric Illnesses. Biol. Psychiatry 2009, 65, 263–267. [Google Scholar] [CrossRef]
- Maxwell, P.; Rink, E.; Kumar, D.; Mendall, M. Antibiotics increase functional abdominal symptoms. Am. J. Gastroenterol. 2002, 97, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.-L.; Cho, C.-Y.; Hsu, C.-L.; Chen, C.-J.; Chang, L.-Y.; Lee, Y.-S.; Soong, W.-J.; Jeng, M.-J.; Wu, K.-G. Recent trends in antibiotic prescriptions for acute respiratory tract infections in pediatric ambulatory care in Taiwan, 2000–2009: A nationwide population-based study. J. Microbiol. Immunol. Infect. 2016, 49, 554–560. [Google Scholar] [CrossRef] [PubMed]
- Mulak, A.; Taché, Y. Sex difference in irritable bowel syndrome: Do gonadal hormones play a role? Gastroenterol. Pol. Organ Pol. Tow. Gastroenterol. 2010, 17, 89–97. [Google Scholar]
- Olafsdottir, L.B.; Gudjonsson, H.; Jonsdottir, H.H.; Björnsson, E.; Thjodleifsson, B. Natural History of Irritable Bowel Syndrome in Women and Dysmenorrhea: A 10-Year Follow-Up Study. Gastroenterol. Res. Pract. 2012, 2012, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Holtmann, G.J.; Ford, A.C.; Talley, N.J. Pathophysiology of irritable bowel syndrome. Lancet Gastroenterol. Hepatol. 2016, 1, 133–146. [Google Scholar] [CrossRef]
- Gubbels, J.; Van Der Put, C.E.; Assink, M. Risk Factors for School Absenteeism and Dropout: A Meta-Analytic Review. J. Youth Adolesc. 2019, 48, 1637–1667. [Google Scholar] [CrossRef]
- Crespo, N.; Palomo, M.T.; Mendez, M. Causes of Absenteeism in University Students and Its Effects in the Academic Performance. Available online: https://www.researchgate.net/publication/287302518 (accessed on 1 February 2021).
- Zahedi, M.J.; Behrouz, V.; Azimi, M. Low fermentable oligo-di-mono-saccharides and polyols dietversusgeneral dietary advice in patients with diarrhea-predominant irritable bowel syndrome: A randomized controlled trial. J. Gastroenterol. Hepatol. 2018, 33, 1192–1199. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.S.C.; Yu, S.; Fedewa, A. Systematic review: Dietary fibre and FODMAP-restricted diet in the management of constipation and irritable bowel syndrome. Aliment. Pharmacol. Ther. 2015, 41, 1256–1270. [Google Scholar] [CrossRef] [PubMed]
- Lacy, B.E.; Weiser, K.; Noddin, L.; Robertson, D.J.; Crowell, M.D.; Parratt-Engstrom, C.; Grau, M.V. Irritable bowel syndrome: Patients’ attitudes, concerns and level of knowledge. Aliment. Pharmacol. Ther. 2007, 25, 1329–1341. [Google Scholar] [CrossRef]
- Soltani, S.; Keshteli, A.H.; Esmaillzadeh, A.; Adibi, P. Food Item Avoidance of Patients with Irritable Bowel Syndrome Com-pared with Healthy People. Arch. Iran Med. 2019, 22, 369–375. [Google Scholar] [PubMed]
- Generation NHI, National Health Insurance Administration, Ministry of Health and Welfare. 2012. Available online: http://www.nhi.gov.tw/ (accessed on 6 December 2014).
- Moloney, R.D.; Johnson, A.C.; O’Mahony, S.M.; Dinan, T.G.; Meerveld, B.G.-V.; Cryan, J.F. Stress and the Microbiota-Gut-Brain Axis in Visceral Pain: Relevance to Irritable Bowel Syndrome. CNS Neurosci. Ther. 2016, 22, 102–117. [Google Scholar] [CrossRef] [PubMed]
- Okami, Y.; Kato, T.; Nin, G.; Harada, K.; Aoi, W.; Wada, S.; Higashi, A.; Okuyama, Y.; Takakuwa, S.; Ichikawa, H.; et al. Lifestyle and psychological factors related to irritable bowel syndrome in nursing and medical school students. J. Gastroenterol. 2011, 46, 1403–1410. [Google Scholar] [CrossRef] [PubMed]
- Qin, H.-Y.; Cheng, C.-W.; Tang, X.-D.; Bian, Z.-X. Impact of psychological stress on irritable bowel syndrome. World J. Gastroenterol. 2014, 20, 14126–14131. [Google Scholar] [CrossRef] [PubMed]
- Tayama, J.; Nakaya, N.; Hamaguchi, T.; Saigo, T.; Takeoka, A.; Sone, T.; Fukudo, S.; Shirabe, S. Maladjustment to Academic Life and Employment Anxiety in University Students with Irritable Bowel Syndrome. PLoS ONE 2015, 10, e0129345. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.H.; Huang, Y.C. College Students’ Capacity to be Alone with Life Stress and Their Personal Variables-Taking Central Taiwan as an Example. J. Educ. Natl. Chang. Univ. Educ. 2009, 16, 75–102. [Google Scholar] [CrossRef]
- Aselton, P. Sources of Stress and Coping in American College Students Who Have Been Diagnosed with Depression. J. Child. Adolesc. Psychiatr. Nurs. 2012, 25, 119–123. [Google Scholar] [CrossRef]
- Lin, K.P.; Hu, P.Y. The Study of Consultation for Enterprise Stress Management Service. J. Occup. Saf. Health 2012, 20, 240–272. [Google Scholar] [CrossRef]
- Frank, L.; Kleinman, L.; Rentz, A.; Ciesla, G.; Kim, J.J.; Zacker, C. Health-related quality of life associated with irritable bowel syndrome: Comparison with other chronic diseases. Clin. Ther. 2002, 24, 675–689. [Google Scholar] [CrossRef]
- Siegrist, J. Impaired quality of life as a risk factor in cardiovascular disease. J. Chronic Dis. 1987, 40, 571–578. [Google Scholar] [CrossRef]
- Xie, G.; Zou, H.; Myint, P.K.; Shi, P.; Ren, F.; Gao, W.; Wu, Y. Baseline overall health-related quality of life predicts the 10-year incidence of cardiovascular events in a Chinese population. Qual. Life Res. 2015, 25, 363–371. [Google Scholar] [CrossRef]
- Lu, W.-C.; Tzeng, N.-S.; Kao, Y.-C.; Yeh, C.-B.; Kuo, T.B.J.; Chang, C.-C.; Chang, H.-A. Correlation between health-related quality of life in the physical domain and heart rate variability in asymptomatic adults. Health Qual. Life Outcomes 2016, 14, 149. [Google Scholar] [CrossRef]
- Zalewski, P.; Słomko, J.; Zawadka-Kunikowska, M. Autonomic dysfunction and chronic disease. Br. Med. Bull. 2018, 128, 61–74. [Google Scholar] [CrossRef]
- Raskov, H.; Burcharth, J.; Pommergaard, H.-C.; Rosenberg, J. Irritable bowel syndrome, the microbiota and the gut-brain axis. Gut Microbes 2016, 7, 365–383. [Google Scholar] [CrossRef]
- Lackner, J.M.; Gudleski, G.D.; Zack, M.M.; Katz, L.A.; Powell, C.; Krasner, S.; Holmes, E.; Dorscheimer, K. Measuring Health-Related Quality of Life in Patients with Irritable Bowel Syndrome: Can Less Be More? Psychosom. Med. 2006, 68, 312–320. [Google Scholar] [CrossRef] [PubMed]
- Schauer, B.; Grabe, H.J.; Ittermann, T.; Lerch, M.M.; Weiss, F.U.; Mönnikes, H.; Völzke, H.; Enck, P.; Schwille-Kiuntke, J. Irritable bowel syndrome, mental health, and quality of life: Data from a population-based survey in Germany (SHIP-Trend-0). Neurogastroenterol. Motil. 2018, 31, e13511. [Google Scholar] [CrossRef] [PubMed]
- Raisi, M.; Matini, M.; Moravveji, A.; Omidi, A.; Amini, J.; Jamali, R. Health related quality of life in irritable bowel syndrome patients, Kashan, Iran: A case control study. Adv. Biomed. Res. 2015, 4, 75. [Google Scholar] [CrossRef] [PubMed]
- Kopczyńska, M.; Mokros, Ł.; Pietras, T.; Małecka-Panas, E. Quality of life and depression in patients with irritable bowel syndrome. Gastroenterol. Rev. 2018, 13, 102–108. [Google Scholar] [CrossRef]
- Khan, Y.L.; Lodhi, S.K.; Bhatti, S.; Ali, W. Does Absenteeism Affect Academic Performance Among Undergraduate Medical Students? Evidence from “Rashid Latif Medical College (RLMC)”. Adv. Med. Educ. Pract. 2019, 10, 999–1008. [Google Scholar] [CrossRef]
| College | Department | Number (%) | IBS (%) |
|---|---|---|---|
| College of Medical Technology | Medical Laboratory Science & Biotechnology | 136 (7.2) | 16 (0.8) |
| Biological Science & Technology | 49 (2.6) | 5 (0.3) | |
| Optometry | 92 (4.9) | 9 (0.4) | |
| Pharmaceutical Science & Technology | 13 (0.7) | 3 (0.2) | |
| Cosmetics Application & Management | 152 (8.0) | 19 (1.0) | |
| Subtotal | 442 (23.4) | 52 (2.7) | |
| College of Nursing | Nursing | 491 (25.9) | 53 (2.8) |
| Long-Term Care | 81 (4.3) | 10 (0.5) | |
| Health Care Administration | 132 (7.0) | 11 (0.6) | |
| Digital Design & Information Management | 42 (2.2) | 2 (0.1) | |
| Subtotal | 746 (39.4) | 76 (4.0) | |
| College of Human Life Science | Occupational Safety & Health | 24 (1.3) | 3 (0.2) |
| Food Nutrition | 317 (16.7) | 30 (1.6) | |
| Early Childhood Caring & education | 95 (5.0) | 8 (0.4) | |
| Safety Health & Environmental Engineering | 18 (0.9) | 1 (0.1) | |
| Hotel & Restaurant Management | 199 (10.5) | 16 (0.8) | |
| Sport, Health, & Leisure | 53 (2.8) | 7 (0.3) | |
| Subtotal | 706 (37.2) | 65 (3.4) | |
| Total | 1894 (100) | 193 (10.1) |
| Variables | Total (N = 1894) M(SD)/n(%) | Non-IBS (N = 1701) M(SD)/n(%) | IBS (N = 193) M(SD)/n(%) | χ2/t | p Value |
|---|---|---|---|---|---|
| Age | 21.59 (1.40) | 21.58 (1.43) | 21.62 (1.05) | −0.342 | 0.728 |
| Body height (cm) | 159.77 (5.81) | 159.76 (5.87) | 159.84 (5.24) | −0.189 | 0.850 |
| Body weight (kg) | 54.36 (10.58) | 54.42 (10.74) | 53.85 (9.10) | 0.792 | 0.429 |
| Body mass index (kg/m2) | 21.29 (3.80) | 21.32 (3.84) | 21.08 (3.45) | 0.790 | 0.430 |
| Colleges | 1894 (100%) | 1701 (100%) | 193 (100%) | 1.943 | 0.378 |
| Medical Technology | 442 (23.4%) | 390 (23.4%) | 52 (26.9%) | ||
| Nursing | 746 (39.4%) | 670 (39.4%) | 76 (39.4%) | ||
| Human Life Science | 706 (37.2%) | 641 (37.2%) | 65 (33.7%) | ||
| Years of education | 1891 (100%) | 1698 (100%) | 193 (100%) | 0.968 | 0.616 |
| Sophomore | 517 (27.3%) | 470 (27.7%) | 47 (24.3%) | ||
| Junior | 708 (37.5%) | 633 (37.3%) | 75 (38.9%) | ||
| Senior | 666 (35.2%) | 595 (35.0%) | 71 (36.8%) | ||
| Living status | 1879 (100%) | 1687 (100%) | 192 (100%) | 2.519 | 0.142 |
| at home | 788 (41.9%) | 717 (42.5%) | 71 (37%) | ||
| rental house | 1091 (58.1%) | 970 (57.5%) | 121 (63%) | ||
| Working status | 1886 (100%) | 1693 (100%) | 193 (100%) | 0.367 | 0.545 |
| non-working | 1181 (62.6%) | 1064 (62.8%) | 117 (60.6%) | ||
| working | 705 (37.4%) | 629 (37.2%) | 76 (39.4%) | ||
| Relationship status | 1875 (100%) | 1683 (100%) | 192 (100%) | 0.818 | 0.366 |
| without | 1102 (58.8%) | 995 (59.1%) | 107 (55.7%) | ||
| with | 773 (41.2%) | 688 (40.9%) | 85 (44.3%) | ||
| Internship experience | 1890 (100%) | 1698 (100%) | 192 (100%) | 0.011 | 0.917 |
| without | 830 (43.9%) | 745 (43.9%) | 85 (44.3%) | ||
| with | 1060 (56.1%) | 953 (56.1%) | 107 (55.7%) | ||
| Current internship | 1792 (100%) | 1608 (100%) | 184 (100%) | 0.085 | 0.771 |
| without | 1665 (92.9%) | 1495 (93.0%) | 170 (92.4%) | ||
| with | 127 (7.1%) | 113 (7.0%) | 14 (7.6%) | ||
| Exercise habits | 1889 (100%) | 1697 (100%) | 192 (100%) | 0.706 | 0.401 |
| without (<3 days/week) | 676 (35.8%) | 602 (35.5%) | 74 (38.5%) | ||
| with (≦3 days/week) | 1213 (64.2%) | 1095 (64.5%) | 118 (61.5%) | ||
| Dysmenorrhea | 1886 (100%) | 1694 (100%) | 192 (100%) | 61.120 | <0.001 ** |
| no | 1349 (71.6%) | 1258 (74.3%) | 91 (47.4%) | ||
| yes | 537 (28.4%) | 436 (25.7%) | 101 (52.6%) | ||
| Food avoidance | 1857 (100%) | 1670 (100%) | 187 (100%) | 79.818 | <0.001 ** |
| no | 1370 (73.8%) | 1283 (76.8%) | 87 (46.5%) | ||
| yes | 487 (26.2%) | 387 (23.2%) | 100 (53.5%) | ||
| Regular medication (gastrointestinal medication and traditional Chinese medicine) | 1876 (100%) | 1683 (100%) | 193 (100%) | 22.360 | <0.001 ** |
| no | 1581 (84.3%) | 1441 (85.6%) | 140 (72.5%) | ||
| yes | 295 (15.7%) | 242 (14.4%) | 53 (27.5%) | ||
| Academic performance | 1882 (100%) | 1690 (100%) | 192 (100%) | 0.002 | 0.963 |
| low grade (<80) | 938 (49.8%) | 842 (49.8%) | 96 (50.0%) | ||
| high grade (≧80) | 944 (50.2%) | 848 (50.2%) | 96 (50.0%) | ||
| Class absenteeism | 1880 (100%) | 1688 (100%) | 192 (100%) | 22.259 | <0.001 ** |
| ≦3 days/semester | 1333 (71%) | 1225 (72.6%) | 108 (56.2%) | ||
| >3 days/semester | 547 (29%) | 463 (27.4%) | 84 (43.8%) |
| Variables | Non-IBS (n = 1701) M(SD) | IBS (n = 193) M(SD) | t | p Value |
|---|---|---|---|---|
| Stress | 26.06 (6.45) | 28.87 (6.80) | −5.66 | <0.001 ** |
| WHOQOL | ||||
| Overall QOL | 3.42 (0.72) | 3.19 (0.64) | 4.73 | <0.001 ** |
| Overall Health | 3.27 (0.79) | 2.80 (0.73) | 8.33 | <0.001 ** |
| QOL_Physical health | 14.46 (2.13) | 13.40 (2.31) | 6.47 | <0.001 ** |
| QOL_Psychological | 13.34 (2.56) | 12.37 (2.42) | 5.04 | <0.001 ** |
| QOL_Social Relationships | 13.83 (2.32) | 13.26 (2.30) | 3.19 | 0.001 * |
| QOL_Environment | 13.67 (2.25) | 13.02 (2.27) | 3.77 | <0.001 ** |
| Variables | β | S.E. | Wald | OR | p | 95% C.I. | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Dysmenorrhea (yes/no) | 0.925 | 0.171 | 29.286 | 2.522 | <0.001 ** | 1.804 | 3.526 |
| Class absenteeism (≦3 days/>3 days) | 0.571 | 0.172 | 11.034 | 1.771 | 0.001 * | 1.264 | 2.481 |
| Food avoidance (yes/ no) | 1.161 | 0.171 | 46.332 | 3.192 | <0.001 ** | 2.285 | 4.459 |
| Regular medication (yes/no) | 0.383 | 0.203 | 3.567 | 1.467 | 0.059 | 0.986 | 2.183 |
| Stress | 0.021 | 0.016 | 1.717 | 1.021 | 0.190 | 0.990 | 1.054 |
| QOL Physical health | −0.140 | 0.059 | 5.537 | 0.870 | 0.019 * | 0.774 | 0.977 |
| QOL Psycological health | −0.039 | 0.055 | 0.490 | 0.962 | 0.484 | 0.863 | 1.072 |
| QOL Social relationship | 0.023 | 0.052 | 0.193 | 1.023 | 0.660 | 0.923 | 1.134 |
| QOL Environment | 0.024 | 0.057 | 0.183 | 1.025 | 0.669 | 0.916 | 1.146 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, H.-H.; Hung, C.-H.; Kao, A.-W.; Hsieh, H.-F. Exploring Quality of Life, Stress, and Risk Factors Associated with Irritable Bowel Syndrome for Female University Students in Taiwan. Int. J. Environ. Res. Public Health 2021, 18, 3888. https://doi.org/10.3390/ijerph18083888
Chen H-H, Hung C-H, Kao A-W, Hsieh H-F. Exploring Quality of Life, Stress, and Risk Factors Associated with Irritable Bowel Syndrome for Female University Students in Taiwan. International Journal of Environmental Research and Public Health. 2021; 18(8):3888. https://doi.org/10.3390/ijerph18083888
Chicago/Turabian StyleChen, Huan-Hwa, Chich-Hsiu Hung, Ai-Wen Kao, and Hsiu-Fen Hsieh. 2021. "Exploring Quality of Life, Stress, and Risk Factors Associated with Irritable Bowel Syndrome for Female University Students in Taiwan" International Journal of Environmental Research and Public Health 18, no. 8: 3888. https://doi.org/10.3390/ijerph18083888
APA StyleChen, H.-H., Hung, C.-H., Kao, A.-W., & Hsieh, H.-F. (2021). Exploring Quality of Life, Stress, and Risk Factors Associated with Irritable Bowel Syndrome for Female University Students in Taiwan. International Journal of Environmental Research and Public Health, 18(8), 3888. https://doi.org/10.3390/ijerph18083888






