How Public Trust in Health Care Can Shape Patient Overconsumption in Health Systems? The Missing Links
Abstract
1. Introduction
2. Literature Review
2.1. Overconsumption of Health Care and Patient Moral Hazard
2.2. Patient Satisfaction and Patient Adherence
2.3. Trust in Health Care
3. Materials and Methods
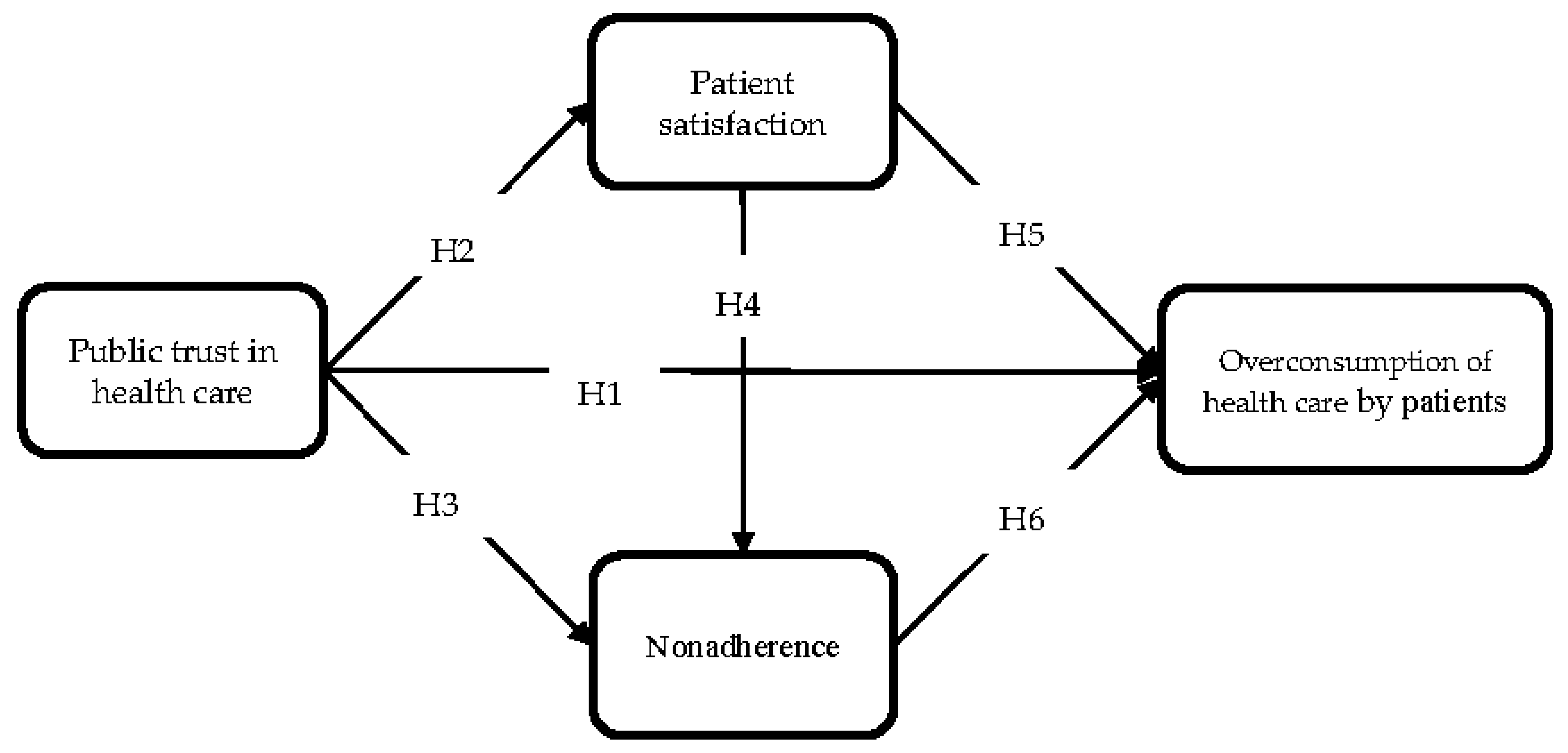
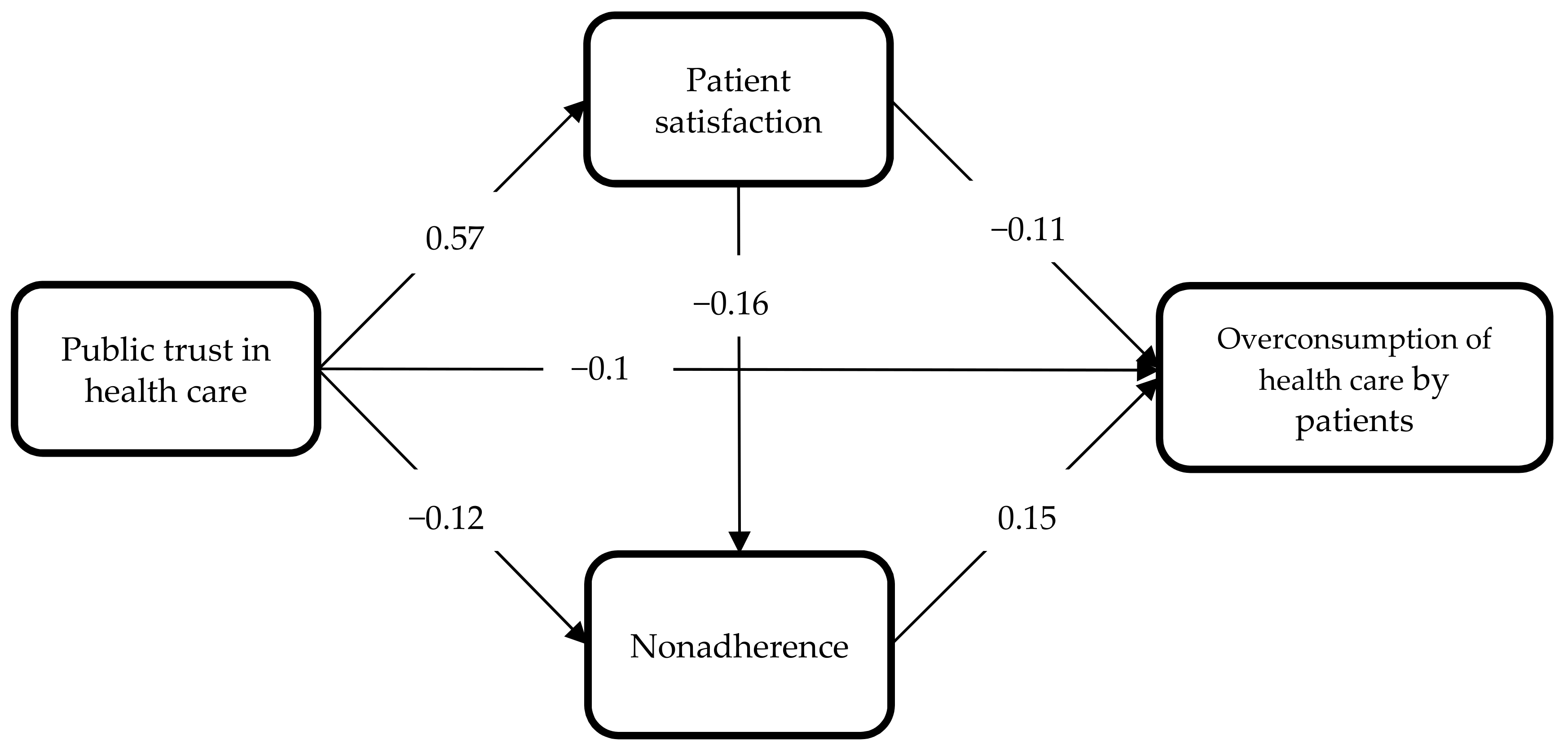
3.1. Research Model and Hypotheses
3.2. Variables and Scale Development
3.3. Sample and Method
4. Results
5. Discussion
- It is an attempt at taking a new and two-dimensional look at overconsumption of health care. On the one hand, overuse is a macroeconomic problem, and it has been the subject of extensive research. On the other hand, it can be viewed as patient behavior that is subject to modification through appropriate management by the service provider (patient satisfaction) and by the health system (public trust in health care).
- It identifies factors influencing overconsumption of health care, both on the macro (trust in the health system) and micro (patient satisfaction, non-adherence) scales. It also points to the mediating role of patient satisfaction and emphasizes the importance of patient non-adherence in stimulating overuse of medical services.
- It focuses on Poland, a country in transition, where no research into the degree of overuse has been conducted before. Interestingly, Poland’s health system has been undergoing major transformations, and patients are not yet treated as clients.
- Finally, it improves the understanding of how public trust operates within both macro- and micro-relationships in the health system, which may provide an insight into interpersonal trust. This research is sufficiently novel in that few studies have emphasized the role of patient satisfaction and patient non-adherence in shaping overconsumption of health care before.
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dexnell, P.; Farid, F.Y. Public trust in the healthcare system in a developing country. Int. J. Health Plan. Manag. 2016, 31, 227–241. [Google Scholar] [CrossRef]
- Gilson, L. Trust and the development of health care as a social institution. Soc. Sci. Med. 2003, 56, 1453–1468. [Google Scholar] [CrossRef]
- Pearson, S.D.; Raeke, L.H. Patients’ trust in physicians: Many theories, few measure, and little data. J. Gen. Intern. Med. 2000, 15, 509–513. [Google Scholar] [CrossRef]
- Rowe, R.; Calnan, M. Trust relations in health care—The new agenda. Eur. J. Public Health 2006, 16, 4–6. [Google Scholar] [CrossRef]
- Dugan, E.; Trachtenberg, F.; Hall, M.A. Development of abbreviated measures to assess patient trust in a physician, a health insurer, and the medical profession. BMC Health Serv. Res. 2005, 5, 64. [Google Scholar] [CrossRef]
- Dagger, T.S.; O’Brien, T.K. Does experience matter? Differences in relationship benefits, satisfaction, trust, commitment and loyalty for novice and experienced service users. Eur. J. Mark. 2010, 44, 1528–1552. [Google Scholar] [CrossRef]
- Ehsan, U.; Ashill, N. Drivers of patients’ trusts in doctors: A study of private healthcare in Pakistan. Int. J. Healthc. Manag. 2014, 7, 237–246. [Google Scholar] [CrossRef]
- Gaur, S.S.; Xu, Y.; Quazi, A.; Nandi, S. Relational impact of service providers’ interaction behavior in healthcare. Manag. Serv. Qual. 2011, 21, 67–87. [Google Scholar] [CrossRef]
- Thom, D.H.; Kravitz, R.L.; Bell, R.A.; Krupat, E.; Azari, R. Patient trust in the physician: Relation to patient requests and request fulfillment. Fam. Pract. 2002, 19, 476–483. [Google Scholar] [CrossRef]
- van der Schee, E.V.D.; Braun, B.; Calnan, M.; Schnee, M.; Groenewegen, P.P. Public trust in health care: A comparison of Germany, The Netherlands, and England and Wales. Health Policy 2007, 81, 56–67. [Google Scholar] [CrossRef]
- Straten, G.F.M.; Friele, R.D.; Groenewegen, P.P. Public trust in Dutch health care. Soc. Sci. Med. 2002, 55, 227–234. [Google Scholar] [CrossRef]
- Lee, Y.Y.; Ng, C.T.; Aishah, M.G.S.; Ngiam, J.Z.; Tai, B.C.; Lim, M.K.; Hughes, K. Public trust in primary care doctors, the medical profession and the healthcare system among Redhill residents in Singapore. Ann. Acad. Med. Singap. 2007, 36, 655–661. [Google Scholar]
- Chassin, M.R.; Galvin, R.W. The urgent need to improve health care quality. Institute of Medicine National Roundtable on Health Care Quality. JAMA 1998, 280, 1000–1005. [Google Scholar] [CrossRef] [PubMed]
- Morgan, D.J.; Brownlee, S.; Leppin, A.L.; Kressin, N.; Dhruva, S.S.; Levin, L.; Landon, B.; Zezza, M.; Schmidt, H.; Saini, V.; et al. Setting a research agenda for medical overuse. BMJ 2015, 351, h4534. [Google Scholar] [CrossRef]
- Brownlee, S.; Chalkidou, K.; Doust, J.; Elshaug, A.G.; Glasziou, P.; Heath, I.; Nagpal, S.; Saini, V.; Srivastava, D.; Chalmers, K.; et al. Evidence for overuse of medical services around the world. Lancet 2017, 390, 156–168. [Google Scholar] [CrossRef]
- Berwick, D.M.; Hackbarth, A.D. Eliminating waste in US health care. JAMA 2012, 307, 1513–1516. [Google Scholar] [PubMed]
- Korenstein, D.; Falk, R.; Howell, E.A.; Bishop, T.; Keyhani, S. Overuse of health care services in the United States: An understudied problem. Arch. Intern. Med. 2012, 172, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Marshall, J.M. Moral hazard. Am. Econ. Rev. 1976, 66, 880–890. [Google Scholar]
- Zweifel, P.; Manning, W.G. Moral hazard and consumer incentives in health care. In Handbook of Health Economics; Culyer, A.J., Newhouse, J.P., Eds.; Elsevier: New York, NY, USA, 2000; pp. 409–459. [Google Scholar]
- Reichmann, G.; Sommersguter-Reichmann, M. Co-payments in the Austrian social health insurance system. Analysing patient behaviour and patients’ views on the effects of co-payments. Health Policy 2004, 67, 75–91. [Google Scholar] [CrossRef]
- Folland, S.; Goodman, A.C.; Satno, M. The Economics of Health and Health Care, 4th ed.; Pearson/Prentice Hall: Hoboken, NJ, USA, 2004. [Google Scholar]
- Stanciole, A.E. Health insurance and lifestyle choices: Identifying ex ante moral hazard in the US market. Geneva Pap. 2008, 33, 627–644. [Google Scholar] [CrossRef]
- Cutler, D.; Zeckhauser, R.J. The Anatomy of Health Insurance. In Handbook of Health Economics; Culyer, A.J., Newhouse, J.P., Eds.; Elsevier: New York, NY, USA, 2000. [Google Scholar]
- Osterkamp, R. Public health insurance Pareto-efficient allocative improvements through differentiated copayment rates. Eur. J. Health Econ. 2003, 4, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Blomqvist, A.; Johansson, P.O. Economic efficiency and mixed public/private insurance. J. Public Econ. 1997, 66, 505–516. [Google Scholar] [CrossRef]
- Powell, D.; Goldman, D. Disentangling moral hazard and adverse selection in private health insurance. J. Econ. 2021, 222, 141–160. [Google Scholar] [CrossRef] [PubMed]
- Konetzka, R.T.; He, D.; Dong, J.; Nyman, J. Moral hazard and long-term care insurance. Geneva Pap. Risk Insur. Issues Pract. 2019, 44, 231–251. [Google Scholar] [CrossRef]
- Cronin, C.J. Insurance-induced moral hazard: A dynamic model of within-year medical care decision making under uncertainty. Int. Econ. Rev. 2019, 60, 187–218. [Google Scholar] [CrossRef]
- Ziethaml, V.A.; Berry, L.L.; Parasuraman, A. The behavioral consequences of service quality. J. Mark. 1996, 60, 31–46. [Google Scholar] [CrossRef]
- Gustafsson, A.; Johnson, M.D.; Roos, I. The effects of customer satisfaction, relationship commitment dimensions, and triggers on customer retention. J. Mark. 2005, 69, 210–218. [Google Scholar] [CrossRef]
- Hojat, M.; Louis, D.Z.; Maxwell, K.; Markham, F.W.; Wender, R.C.; Gonnella, J.S. A brief instrument to measure patients’ overall satisfaction with primary care physicians. Fam. Med. Kans. City 2011, 43, 412–417. [Google Scholar]
- Hall, J.A.; Dornan, M.C. Meta-analysis of satisfaction with medical care: Description of research domain and analysis of overall satisfaction levels. Soc. Sci. Med. 1988, 27, 637–644. [Google Scholar] [CrossRef]
- Hall, M.A.; Zheng, B.; Dugan, E.; Camacho, F.; Kidd, K.E.; Mishra, A.; Balkrishnan, R. Measuring patients’ trust in their primary care providers. Med. Care Res. Rev. 2002, 59, 293–318. [Google Scholar] [CrossRef]
- Buller, M.K.; Buller, D.B. Physicians’ communication style and patient satisfaction. J. Health Soc. Behav. 1987, 28, 375–388. [Google Scholar] [CrossRef]
- Street, R.L.; Gordon, H., Jr.; Haidet, P. Physicians’ communication and perceptions of patients: Is it how they look, how they talk, or is it just the doctor? Soc. Sci. Med. 2007, 65, 586–598. [Google Scholar] [CrossRef] [PubMed]
- Chua, S.S.; Lai, P.S.M.; Tan, C.H.; Chan, S.P.; Chung, W.W.; Morisky, D.E. The development and validation of the Malaysian medication adherence scale (MALMAS) among patients with 2 type diabetes in Malaysia. Int. J. Pharm. Sci. 2013, 5, 790–794. [Google Scholar]
- Vermeire, E.; Hearnshaw, H.; van Royen, P.; Denekens, J. Patient adherence to treatment: Three decades of research. A comprehensive review. J. Clin. Pharm. Ther. 2001, 26, 331–342. [Google Scholar] [CrossRef]
- Bondesson, Å.; Hellström, L.; Eriksson, T.; Höglund, P. A structured questionnaire to assess patient compliance and beliefs about medicines taking into account the ordered categorical structure of data. J. Eval. Clin. Pract. 2009, 15, 713–723. [Google Scholar] [CrossRef]
- Kripalani, S.; Risser, J.; Gatti, M.E.; Jacobson, T.A. Development and evaluation of the adherence to refills and medications scale (ARMS) among low-literacy patients with chronic disease. Value Health 2009, 12, 118–123. [Google Scholar] [CrossRef]
- Dowell, J.; Hudson, H. A qualitative study of medication taking behaviour in primary care. Fam. Pract. 1997, 14, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Aikens, J.E.; Nease, D.E., Jr.; Nau, D.P.; Klinkman, M.S.; Schwenk, T.L. Adherence to maintenance-phase antidepressant medication as a function of patient beliefs about medication. Ann. Fam. Med. 2005, 3, 23–30. [Google Scholar] [CrossRef]
- Babbie, E. Podstawy Badań Społecznych; PWN: Warsaw, Poland, 2008; p. 150. [Google Scholar]
- Coleman, J.S. Foundations of Social Theory; Harvard University Press: Cambridge, MA, USA, 1990. [Google Scholar]
- Weber, J.M.; Malhotra, D.; Murnighan, J.K. Normal acts of irrational trust: Motivated attributions and the trust development process. Res. Organ. Behav. 2004, 26, 75–101. [Google Scholar] [CrossRef]
- Hardin, R. Trust in government. In Trust and Governance; Braithwaite, V., Levi, M., Eds.; Russell Sage Foundation: New York, NY, USA, 1988. [Google Scholar]
- Putnam, R.D.; Robert, D. Bowling Alone: America’s Declining Social Capital. J. Democr. 1995, 6, 65–78. [Google Scholar] [CrossRef]
- Inglehart, R. Trust, well-being and democracy. In Democracy and Trust; Warren, M.E., Ed.; Cambridge University Press: Cambridge, MA, USA, 1999. [Google Scholar]
- Organisation for Economic Co-Operation and Development. Trust and Public Policy: How Better Governance Can Help Rebuild Public Trust; OECD Public Governance Reviews, OECD Publishing: Paris, France, 2017. [Google Scholar] [CrossRef]
- Lewicki, R.J.; McAllister, D.J.; Bies, R.J. Trust and distrust: New relationships and realities. Acad. Manag. Rev. 1998, 23, 438–458. [Google Scholar] [CrossRef]
- Jabłoński, A.; Jabłoński, M. Trust as a key factor in shaping the social business model of water supply companies. Sustainability 2019, 11, 5805. [Google Scholar] [CrossRef]
- Hall, M.A.; Camacho, F.; Dugan, E.; Balkrishnan, R. Trust in the medical profession: Conceptual and measurement issues. Health Serv. Res. 2002, 37, 1419–1439. [Google Scholar] [CrossRef] [PubMed]
- Huang, E.C.; Pu, C.; Chou, Y.J.; Huang, N. Public trust in physicians-health care commodification as a possible deteriorating factor: Cross-sectional analysis of 23 countries. Inquiry 2018, 55, 1–11. [Google Scholar] [CrossRef]
- Davies, H.T.O.; Rundall, T.G. Managing patient trust in managed care. Milbank Q. 2000, 78, 609–624. [Google Scholar] [CrossRef]
- Meyer, S.; Ward, P.; Coveney, J.; Rogers, W. Trust in the health system: An analysis and extension of the social theories of Giddens and Luhmann. Health Sociol. Rev. 2008, 17, 177–186. [Google Scholar] [CrossRef]
- Gupta, S.; Brenner, A.T.; Ratanawongsa, N.; Inadomi, J.M. Patient trust in physician influences colorectal cancer screening in low-income patients. Am. J. Prev. Med. 2014, 47, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.Y.; Lin, J.L. How much does trust really matter? A study of the longitudinal effects of trust and decision-making preferences on diabetic patient outcomes. Patient Educ. Couns. 2011, 85, 406–412. [Google Scholar] [CrossRef]
- Jones, D.E.; Carson, K.A.; Bleich, S.N.; Cooper, L.A. Patient trust in physicians and adoption of lifestyle behaviors to control high blood pressure. Patient Educ. Couns. 2012, 89, 57–62. [Google Scholar] [CrossRef]
- Tboni, D.H.; Hall, M.A.; Pawlson, L.G. Measuring patients’ trust in physicians when assessing quality of care. Health Aff. 2004, 23, 124–132. [Google Scholar]
- Thiede, M. Information and access to health care: Is there a role for trust? Soc. Sci. Med. 2005, 61, 1452–1462. [Google Scholar] [CrossRef]
- Kato, K.; O’Malley, K.J. Relationships between the eligibility process, trust in the U.S. health care system, and patient satisfaction with the Houston Veterans Affairs Medical Center. Mil. Med. 2007, 172, 819–823. [Google Scholar] [CrossRef]
- Hall, M.A.; Dugan, E.; Zheng, B.; Mishra, A.K. Trust in physicians and medical institutions: What is it, can it be measured, and does it matter? Milbank Q. 2001, 79, 613–639. [Google Scholar] [CrossRef] [PubMed]
- Montague, E.N.H.; Winchester, W.W.; Kleiner, B.M. Trust in medical technology by patients and healthcare providers in obstetric work systems. Behav. Inf. Technol. 2010, 29, 541–554. [Google Scholar] [CrossRef] [PubMed]
- Egede, L.E.; Ellis, C. Development and testing of the multidimensional trust in health care systems scale. J. Gen. Intern. Med. 2008, 23, 808–815. [Google Scholar] [CrossRef] [PubMed]
- van der Schee, E.; Groenewegen, P.P.; Friele, R.D. Public trust in health care: A performance indicator? J. Health Organ. Manag. 2006, 20, 468–476. [Google Scholar] [CrossRef] [PubMed]
- Boulware, L.E.; Cooper, L.A.; Ratner, L.E.; LaVeist, T.A.; Powe, N.R. Race and trust in the health care system. Public Health Rep. 2003, 118, 358–365. [Google Scholar] [CrossRef]
- Musa, D.; Schulz, R.; Harris, R.; Silverman, M.; Thomas, S.B. Trust in the health care system and use of preventive health services by older black and white adults. Am. J. Public Health 2009, 99, 1293–1299. [Google Scholar] [CrossRef] [PubMed]
- Krot, K.; Sousa, J.P. Factors impacting on patient compliance with medical advice: Empirical study. Eng. Manag. Prod. Serv. 2017, 9, 73–81. [Google Scholar] [CrossRef]
- Mechanic, D.; Schlesinger, M. The impact of managed care on patients’ trust in medical care and their physicians. JAMA 1996, 275, 1693–1697. [Google Scholar] [CrossRef]
- Gray, B. Trust and trustworthy care in the managed care era. Health Aff. 1997, 16, 34–49. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Zhao, H.; Cleary, P.D. International variations in trust in health care systems. Int. J. Health Plan. Manag. 2019, 34, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Gabay, G.; Moore, D. Antecedents of patient trust in health care insurers. Serv. Mark. Q. 2015, 36, 77–93. [Google Scholar] [CrossRef]
- Mollborn, S.; Stepanikova, I.; Cook, K.S. Delayed care and unmet needs among health care system users: When does fiduciary trust in a physician matter? Health Serv. Res. 2005, 40, 1898–1917. [Google Scholar] [CrossRef]
- Elleuch, A. Patient satisfaction in Japan. Int. J. Health Care Qual. Assur. 2008, 21, 692–705. [Google Scholar] [CrossRef] [PubMed]
- Trumble, S.C.; O’Brien, M.L.; O’Brien, M.; Hartwig, B. Communication skills training for doctors increases patient satisfaction. Clin. Gov. Int. J. 2006, 11, 299–307. [Google Scholar] [CrossRef]
- Joreskog, K.; Sorbom, D. LISREL 8: User’s Reference Guide; Scientific Software International Inc.: Chicago, IL, USA, 1996. [Google Scholar]
- Rodríguez, N.G.; Pérez, M.J.S.; Trespalacios, G.J.A. Interfunctional trust as a determining factor of a new product performance. Eur. J. Mark. 2007, 41, 678–702. [Google Scholar] [CrossRef]
- Bentler, P.M. EQS 6 Structural Equations Program Manual; Multivariate Software, Inc.: Encino, CA, USA, 2006; Available online: http://www.econ.upf.edu/~satorra/CourseSEMVienna2010/EQSManual.pdf (accessed on 15 March 2021).
| Concept | Meaning | Source |
|---|---|---|
| Overuse | A situation when health care service is provided under circumstances in which its potential for harm exceeds the possible benefit | [13] |
| Moral hazard | Excessive expenditure due to eligibility for insurance benefits | [18] |
| Patient satisfaction | A patients’ overall evaluation of the performance of a service offering after experiencing it | [30] |
| Patient adherence | The extent to which a person’s behavior (such as taking medication, modifying lifestyle, following a diet) corresponds with agreed recommendations from a health care professional | [36] |
| Interpersonal trust | Characterizes a relationship between two individuals, such as a specific doctor–patient relationship. | [51] |
| Public/system trust | Characterizes attitudes toward collective entities or social organizations. | [10] |
| Variable | Source | Cronbach Alpha |
|---|---|---|
| Public trust in health care (5 items) | [63,64] | 0.68 |
| Patient satisfaction (8 items) | [64,73,74] | 0.86 |
| Patient non-adherence (3 itmes) | [39] | 0.64 |
| Income | Sex | ||||
|---|---|---|---|---|---|
| N | % | N. | % | ||
| up to PLN 1.000 * | 84 | 9.3 | female | 572 | 58.2 |
| from PLN 1.001 to 1.400 | 95 | 10.5 | male | 411 | 41.8 |
| from PLN 1.401 to 1.800 | 108 | 12.0 | Age | ||
| from PLN 1.801 to 2.000 | 113 | 12.5 | 18–24 | 103 | 10.5 |
| from PLN 2.001 to 2.500 | 76 | 8.4 | 25–34 | 182 | 18.5 |
| from PLN 2.501 to 3.000 | 120 | 13.3 | 35–44 | 163 | 16.6 |
| from PLN 3.001 to 5.000 | 139 | 15.4 | 45–59 | 252 | 25.6 |
| over PLN 5.000 | 118 | 13.1 | over 60 | 283 | 28.8 |
| hard to say | 49 | 5.4 | |||
| Place of residence | Level of education | ||||
| village | 356 | 36.2 | elementary | 148 | 15.0 |
| up to 100 thous. | 335 | 34.1 | basic vocational | 213 | 21.7 |
| 100–499 thous. | 164 | 16.7 | secondary | 345 | 35.2 |
| 500+ thous. | 127 | 13.0 | college/university | 276 | 28.1 |
| Mean | SD | Patient Satisfaction | Patient Non-Adherence | Public Trust in Health Care | |
|---|---|---|---|---|---|
| Correlation Coefficient | |||||
| Patient satisfaction | 3.62 | 0.77 | |||
| Patient non-adherence | 2.31 | 1.02 | −0.19 | ||
| Public trust in health care | 2.97 | 0.76 | 0.47 | −0.14 | |
| Overconsumption of health care by patients | 3.54 | 1.22 | −0.19 | 0.16 | −0.15 |
| Index | Score |
|---|---|
| CMIN/DF | 1.78 |
| GFI | 0.97 |
| CFI | 0.97 |
| RMSA | 0.028 |
| Holter | 691 |
| Estimate | p Value | ||||
|---|---|---|---|---|---|
| H1: Overconsumption of health care by patients | ← | Public trust in health system | −0.10 | 0.002 | Supported |
| H2: Patient satisfaction | ← | Public trust in health system | 0.57 | 0.000 | Supported |
| H3: Patient non-adherence | ← | Public trust in health system | −0.12 | 0.05 | Supported |
| H4: Patient non-adherence | ← | Patient satisfaction | −0.16 | 0.003 | Supported |
| H5: Overconsumption of health care by patients | ← | Patient satisfaction | −0.11 | 0.000 | Supported |
| H6: Overconsumption of health care by patients | ← | Patient non-adherence | 0.15 | 0.001 | Supported |
| Public Trust in Health Care | Patient Satisfaction | Patient Non-Adherence | |
|---|---|---|---|
| Standardized total effects | |||
| Public trust in health care | - | - | - |
| Patient satisfaction | 0.57 | - | - |
| Patient non-adherence | −0.21 | −0.16 | - |
| Overconsumption of health care by patients | −0.19 | −0.13 | 0.14 |
| Standardized direct effects | |||
| Public trust in health care | - | - | - |
| Patient satisfaction | 0.57 | - | - |
| Patient non-adherence | −0.12 | −0.16 | - |
| Overconsumption of health care by patients | −0.10 | −0.11 | 0.14 |
| Standardized indirect effects | |||
| Public trust in health care | - | - | - |
| Patient satisfaction | - | - | - |
| Patient non-adherence | −0.09 | - | - |
| Overconsumption of health care by patients | −0.09 | −0.02 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krot, K.; Rudawska, I. How Public Trust in Health Care Can Shape Patient Overconsumption in Health Systems? The Missing Links. Int. J. Environ. Res. Public Health 2021, 18, 3860. https://doi.org/10.3390/ijerph18083860
Krot K, Rudawska I. How Public Trust in Health Care Can Shape Patient Overconsumption in Health Systems? The Missing Links. International Journal of Environmental Research and Public Health. 2021; 18(8):3860. https://doi.org/10.3390/ijerph18083860
Chicago/Turabian StyleKrot, Katarzyna, and Iga Rudawska. 2021. "How Public Trust in Health Care Can Shape Patient Overconsumption in Health Systems? The Missing Links" International Journal of Environmental Research and Public Health 18, no. 8: 3860. https://doi.org/10.3390/ijerph18083860
APA StyleKrot, K., & Rudawska, I. (2021). How Public Trust in Health Care Can Shape Patient Overconsumption in Health Systems? The Missing Links. International Journal of Environmental Research and Public Health, 18(8), 3860. https://doi.org/10.3390/ijerph18083860







