Broccoli-Soybean-Mangrove Food Bar as an Emergency Food for Older People during Natural Disaster
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
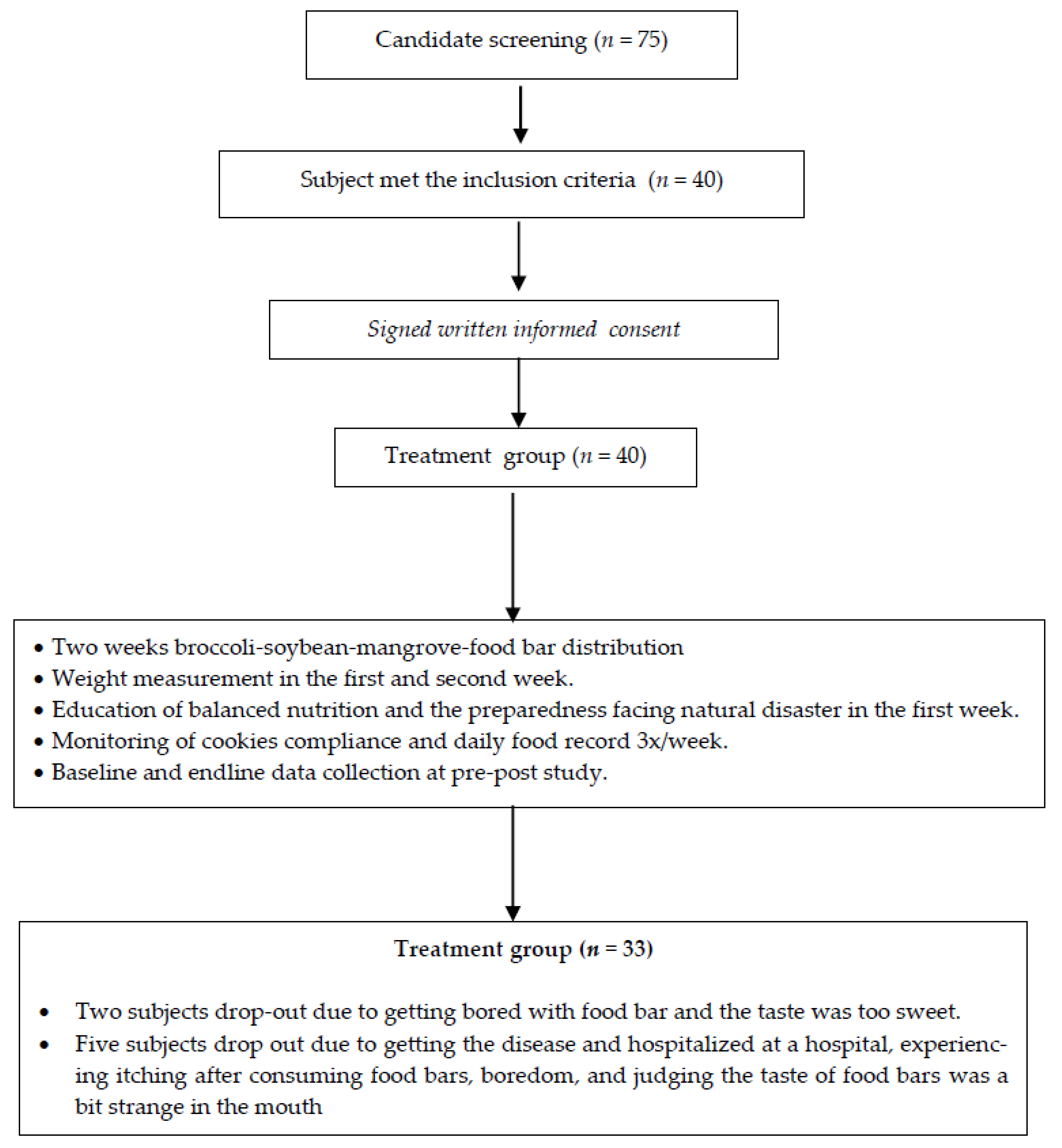
2.2. Population and Sample
2.3. Subject Recruitment
2.4. Instrument
2.5. Food Bar Cooking Process
- Beat melted butter and white sugar with a mixer until smooth/homogenous. Put all the eggs and the mangrove, broccoli, and soybean flour into the dough.
- Stir the dough with the wish tool until blended and put the chocolate paste or other flavor into the dough. Then, stir homogenously with a wish or spatula tool.
- Prepare a square baking sheet with white parchment paper, then spread with butter until blended.
- Pour the dough into the pan and baked it in the oven for 30 min at a temperature of 180 °C. Continue baking again at 180 °C for 20 min to get a really dry quality food bar. One of the criteria for a food bar is that it must be completely dry for long-term storage as an emergency food [13].
2.6. Nutrition Intervention and Follow-Up
2.7. Data Analysis
3. Results
3.1. Hedonic and Hedonic Quality Test
3.2. Sociodemography Characteristic and Nutritional Status, Independence Level, and Cognitive Profiles
3.3. Weight Change, Dietary Intakes, and Natural Disaster Preparedness Knowledge
3.3.1. Weight Changes and Dietary Intakes
3.3.2. Natural Disaster Preparedness Knowledge
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Kompas.com. Natural Disaster in Indonesia Increased in 2019. Available online: https://nasional.kompas.com/read/2019/03/29/17293031/bnpb-bencana-alam-di-indonesia-meningkat-pada-tahun-2019 (accessed on 3 October 2020).
- Berita Satu. In the Early 2020, 86 Person Died Caused by Flood. Available online: https://www.beritasatu.com/nasional/599646/awal-2020-86-orang-tewas-akibat-banjir (accessed on 5 October 2020).
- WHO. Older Person in Emergencies: An Active Ageing Perspective; WHO: Geneva, Switzerland, 2008; pp. 31–33. [Google Scholar]
- IASC. Nutrition Cluster: A Toolkit for Addressing Nutrition in Emergency Situations. Available online: https://motherchildnutrition.org/resources/pdf/mcn-iasc-toolkit-nutrition-in-emergency-situations.pdf (accessed on 1 October 2020).
- HelpAge International. Nutrition Interventions for Older People in Emergencies; HelpAge International: London, UK, 2013; pp. 6–8. [Google Scholar]
- Merck Manual, Consumer Version. Available online: http://www.merckmanuals.com/home/disorders-of-utrition/undernutrition/undernutrition (accessed on 25 January 2017).
- Jane, T. Opportunities to Improve Nutrition for Older Adults and Reduce Risk of Poor Health Outcomes; Administration for Community Living, Center for Policy and Evaluation: Washington, DC, USA, 2017.
- Nieuwenhuizen, W.F.; Hugo, W.; Paul, R.; Marion, M.H. Older Adults and Patients in Need of Nutritional Support: Review of Current Treatment Options and Factors Influencing Nutritional Intake. Clin. Nutr. 2010, 29, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Campbell, A.D.; Godfryd, A.; Buys, D.; Locher, J. Does Participation in Home-delivered Meals Programs Improve Outcomes for Older Adults? Results of a Systematic Review. J. Nutr. Gerontol. Geriatr. 2015, 34, 124–167. [Google Scholar] [CrossRef]
- Zhu, H.; Ruopeng, N. Impact of Home-delivered Meal Programs on Diet and Nutrition among Older Adults: A Review. Nutr. Health 2013, 22, 89–103. [Google Scholar] [CrossRef] [PubMed]
- Silver, H.J. Oral Strategies to Supplement Older Adults’ Dietary Intakes: Comparing the Evidence. Nutr. Rev. 2009, 67, 21–31. [Google Scholar] [CrossRef]
- Fatmah. Effect of Tempeh-dates Biscuits Supplementation for Undernourished Older Adults. J. Int. Dent. Med. Res. 2019, 12, 232–237. [Google Scholar]
- Elvira, S. Emergency Food Development; Scription; Bogor Agricultural University: Bogor, Indonesia, 2014. [Google Scholar]
- Raden, B.K.A.; Siswanti, S.; Edhi, N. Food Emergency Formulation in the Form of Food Bar Based on the White Millet Flour (Panicum milliaceum L.) and Red Bean Flour (Phaseolus vulgaris L.). Agritech 2016, 36, 23–29. [Google Scholar]
- UNHCR; UNICEF; WFP; WHO. Food Nutrition Needs in Emergencies; WHO: Geneva, Switzerland, 2002; pp. 23–24. [Google Scholar]
- Ratna, S.; Ratnawaty, F.; Andi, S. Effect of Lindur Mangrove Fruit Flour (Bruguiera gymnorrhiza) Substitution on the Quality of Wet Noodles. J. Pendidik. Teknol. Pertan. 2020, 6, 75–88. [Google Scholar]
- Hardi, B.P. Utilization of Mangrove Flour in Making Cookies; Bogor Agricultural University: Bogor, Indonesia, 2014. [Google Scholar]
- The Indonesian Ministry of Health (MOH). The Indonesian Food Composition Table 2017; The Indonesian MOH: Jakarta, Indonesia, 2018.
- The Indonesian Ministry of Health. The Rule of Minister of Heath of the Republic of Indonesia No. 75 Year 2013; The Indonesian MOH: Jakarta, Indonesia, 2013.
- IOM (Institute of Medicine). Estimated Mean per Capita Energy Requirements for Planning Energy Food and Rations; National Academy Press: Washington, DC, USA, 1995. [Google Scholar]
- IOM (Institute of Medicine). High Energy, Nutrient-Dense Emergency Relief Food Product; National Academy Press: Washington, DC, USA, 2002. [Google Scholar]
- Ariawan, I. Size and Sample Method in the Health Research; Faculty of Public Health Universitas Indonesia: Depok, Indonesia, 2011. [Google Scholar]
- Leslie, W.S.; Woodward, M.; Lean ME, J.; Theobald, H.; Watson, L.; Hankey, C.R. Improving the Dietary Intake of Undernourished Older People in Residential Care Homes using an Energy-enriching Food Approach: A Cluster Randomised Controlled Study. J. Nutr. Hum. Diet. 2012, 26, 387–394. [Google Scholar] [CrossRef]
- Rémond, D.; Shahar, D.R.; Gille, D.; Pinto, P.; Kachal, J.; Peyron, M.A.; Dos Santos, C.N.; Walther, B.; Bordoni, A.; Dupont, D.; et al. Understanding the Gastrointestinal Tract of the Elderly to Develop Dietary Solutions that Prevent Malnutrition). Oncotarget 2015, 6, 13858–13898. [Google Scholar] [CrossRef]
- Madsen, J.L.; Jesperr, G. Effects of Ageing on Gastrointestinal Motor Function. Age Ageing 2004, 33, 154–159. [Google Scholar] [CrossRef]
- Guigoz, Y.; Vellas, B. Nutritional Assessment in Older Adults: MNA® 25 Years of a Screening Tool & a Reference Standard for Care and Research; What Next? J. Nutr. Health Aging 2021. [Google Scholar] [CrossRef]
- Balai Besar Industri Agro Laboratory. Nutrient Content of Food Bars; Balai Besar Industri Agro (BBIA): Bogor, Indonesia, 2020. [Google Scholar]
- Szabo, P.B. Sensory Evaluation in Food Industry. Available online: https://u-szeged.hu/download.php?docID=55794 (accessed on 16 December 2020).
- Yoon, H.J.; Lee, S.K. Effect of Home-visit Nutrition Education for the Elderly with High Fasting Blood Glucose Levels. Korean J. Community Nutr. 2006, 11, 346–360. [Google Scholar]
- Kim, H.B.; Mi-Ju, K.; Yoonna, L. The Effect of a Nutritional Education Program on the Nutritional Status of Elderly Patients in a Long-term Care Hospital in Jeollanamdo Province: Health Behavior, Dietary Behavior, Nutrition Risk Level and Nutrient Intake. Nutr. Res. Pract. 2012, 6, 35–44. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Donald, K.G.; Payette, H.; Boutier, V. Randomized Clinical Trial of Nutritional Supplementation Shows Little Effect on Functional Status among Free-living Frail Elderly. J. Nutr. 1995, 125, 2965–2971. [Google Scholar]
- Damayanthi, H.D.W.T.; Moy, F.M.; Abdullah, K.L.; Dharmaratne, S.D. Prevalence of Malnutrition and Associated Factors among Community-dwelling Older Persons in Sri Lanka: A cross-Sectional Study. BMC Geriatr. 2019, 18, 199. [Google Scholar] [CrossRef]
- Gunaid, A.A. Obesity, Overweight and Underweight among Adults in an Urban Community in Yemen. East. Mediterr. Health J. 2012, 18, 1187–1193. [Google Scholar] [CrossRef] [PubMed]
- Wa, O.S.A.; Akbar, A. Older People Nutritional Status Assessment based on the BMI and MNA. J. Ilm. Kesehat. Diagn. 2018, 12, 287–290. [Google Scholar]
- Buys, D.R.; Roth, D.L.; Ritchie, C.S.; Sawyer, P.; Allman, R.M.; Funkhouser, E.M.; Hovater, M.; Locher, J.L. Nutritional Risk and Body Mass Index Predict Hospitalization, Nursing Home Admissions, and Mortality Community-dwelling Older Adults: Results from the UAB Study of Aging with 8.5 Years of Follow-up. J. Gerontol. A Bio. Sci. Med. Sci. 2014, 69, 1146–1153. [Google Scholar] [CrossRef]
- Elman, B. Older People Malnutrition Prevalence using MNA Tool at Community Health Center. Herb. Med. J. 2019, 2, 5–9. [Google Scholar]
- Kutikuppala, A.; Neeta, M.; Ghnana, P.T.L. Nutritional Status of Elderly People using Mini Nutritional Assessment Tool in an Urban Slum of Hyderabad. Int. J. Med. Sci. Public Health 2019, 7, 885–888. [Google Scholar] [CrossRef]
- Anna, K.; Jolanta, W.; Barbara, G.; Tomas, G. Nutritional and Functional Status in Newly Hospitalized Older Patients who are not Underweight. J. Nutr. Gerontol. Geriatr. 2017, 36, 111–120. [Google Scholar]
- Li-Chin, L.; Alan, C.T. Mini-Nutritional-Assessment (MNA) without Body Mass Index (BMI) Predicts Functional Disability in Elderly Taiwanese. Arch. Gerontol. Geriatr. 2015, 54, e405–e410. [Google Scholar]
- Remya, R.; Jenyz, M.M.; Saju, J.R.; Vidhu, M.J. Nutritional Status and Cognitive Impairment in Elderly Population in a Rural Area of Thrissur District, Kerala. Int. J. Community Med. Public Health 2018, 5, 1218–1223. [Google Scholar]
- Hou, Q.; Guan, Y.; Yu, W.; Liu, X.; Wu, L.; Xiao, M.; Lü, Y. Associations between Obesity and Cognitive Impairment in the Chinese Elderly: An Observational Study. Clin. Interv. Aging 2019, 14, 367–373. [Google Scholar] [CrossRef] [PubMed]



| Level of Likeness | Broccoli Soybean Mangrove Food Bar | |||||||
|---|---|---|---|---|---|---|---|---|
| Aroma | Texture | Taste | Color | |||||
| n | % | n | % | n | % | n | % | |
| Dislike extremely | 2 | 7.1 | 0 | 0.0 | 2 | 7.1 | 0 | 0.0 |
| Dislike | 11 | 39.3 | 1 | 3.6 | 5 | 17.9 | 4 | 14.3 |
| Like | 13 | 46.4 | 25 | 89.3 | 18 | 64.3 | 20 | 71.4 |
| Like extremely | 1 | 3.6 | 2 | 7.1 | 2 | 7.1 | 3 | 10.7 |
| Attribute | Broccoli Soybean Mangrove Food Bar | |
|---|---|---|
| n | % | |
| Aroma: | ||
| It was very bad | 4 | 14.3 |
| It was a little nice | 11 | 39.3 |
| Good | 11 | 39.3 |
| Very good | 2 | 7.1 |
| Texture: | ||
| It was not very crunchy | 2 | 7.1 |
| It was a bit crunchy | 12 | 42.9 |
| It was crunchy | 13 | 46.4 |
| It was very crunchy | 1 | 3.6 |
| Taste: | ||
| It was not very sweet | 2 | 7.1 |
| It was a little sweet | 8 | 28.6 |
| It was sweet | 16 | 57.1 |
| It was very sweet | 2 | 7.1 |
| Color: | ||
| It was not attractive | 2 | 7.1 |
| It was a bit attractive | 5 | 17.9 |
| It was attractive | 20 | 71.4 |
| It was very attractive | 1 | 3.6 |
| Indicator | n | % | Mean ± SD |
|---|---|---|---|
| Sex | |||
| Male | 6 | 18.2 | |
| Female | 27 | 81.8 | |
| Marital status | |||
| Married | 13 | 39.4 | |
| Widow/widower | 20 | 60.6 | |
| Age (y.o) | 70.4 ± 7.8 | ||
| 60–70 | 14 | 42.4 | |
| 71–80 | 16 | 48.5 | |
| ≥81 | 3 | 9.1 | |
| Final education level | |||
| Low | 29 | 87.9 | |
| Moderate | 4 | 12.1 | |
| Staying at home | |||
| Alone | 3 | 9.1 | |
| Husband/wife/4/12.1 | |||
| Children/grandchild/son-in-law | 23 | 69.7 | |
| Another family member | 3 | 9.1 | |
| Body Mass Index/BMI (kg/m2) | 19.6 ± 3.5 | ||
| Underweight (<18.5 kg/m2) | 15 | 45.5 | |
| Normal (18.5–24.9 kg/m2) | 18 | 54.5 | |
| Overweight (25.0–29.9 kg/m2) | 0 | 0.0 | |
| Obesity (≥30.0 kg/m2) | 0 | 0.0 | |
| MUAC (Mid Upper Arm Circumference) (cm) | 22.5 ± 2.8 | ||
| MNA (Mini Nutritional Assessment) | 21.2 ± 3.9 | ||
| At risk malnourished | 25 | 75.8 | |
| Normal | 8 | 24.2 | |
| MMSE (Mini Mental State Examination) | 21.1 ± 6.4 | ||
| Cognitive impairment | 8 | 24.2 | |
| Probably cognitive impairment | 11 | 33.3 | |
| Normal | 14 | 42.5 | |
| BADL (Basic Activity Daily Living) | 19.8 ± 0.9 | ||
| Light dependence | 3 | 9.1 | |
| Independently | 30 | 90.9 | |
| IADL (Instrumental Activity Daily Living) | 5.1 ± 2.3 | ||
| Need help all the time | 2 | 6.1 | |
| Need help now and then | 3 | 9.1 | |
| Independently | 28 | 84.8 |
| Nutritional Status at Pre-Study | In the First Week | In the Second Week | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Loose (Person) | Stay (Person) | Gain (Person) | Loose (Person) | Stay (Person) | Gain (Person) | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Underweight | 6 | 50.0 | 0 | 0.0 | 9 | 50.0 | 3 | 33.3 | 2 | 50.0 | 10 | 50.0 |
| Normal | 6 | 50.0 | 3 | 100.0 | 9 | 50.0 | 6 | 66.7 | 2 | 50.0 | 10 | 50.0 |
| Total | 12 | 100.0 | 3 | 100.0 | 18 | 100.0 | 9 | 100.0 | 4 | 100.0 | 20 | 100.0 |
| Mean (kg) | −0.30 | 0.0 | 0.34 | −0.29 | 0.0 | 0.50 | ||||||
| Minimum (kg) | −0.80 | 0.0 | 0.10 | −1.20 | 0.0 | 0.10 | ||||||
| Maximum (kg) | −0.10 | 0.0 | 0.90 | −0.10 | 0.0 | 1.20 | ||||||
| Nutritional Status at Pre-Study | Energy Intake | Carbohydrate Intake | Protein Intake | Fat Intake | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (kcal) | (gr) | (gr) | (gr) | |||||||||||||
| Loose | Gain | Loose | Gain | Loose | Gain | Loose | Gain | |||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Underweight | 5 | 71.4 | 10 | 38.5 | 4 | 66.7 | 11 | 40.0 | 8 | 66.7 | 7 | 33.3 | 5 | 62.5 | 10 | 40.0 |
| Normal | 2 | 28.6 | 16 | 61.5 | 2 | 33.3 | 16 | 59.3 | 4 | 33.3 | 14 | 66.7 | 3 | 37.5 | 15 | 60.0 |
| Total | 7 | 100.0 | 26 | 100.0 | 6 | 100.0 | 27 | 100.0 | 12 | 100.0 | 11 | 100.0 | 8 | 100.0 | 25 | 100.0 |
| Measurement | Mean | SD | 95% CI | p |
|---|---|---|---|---|
| Body weight (baseline vs. week 1) | 41.6 | 8.3 | 26.8–64.2 | >0.01 |
| Body weight (week 1 vs. week II) | 41.7 | 8.2 | 26.9–64.2 | <0.01 |
| Body weight (baseline vs. weeks I) | 41.8 | 8.2 | 26.7–64.4 | <0.01 |
| Energy (kcal) | 2291.9 | 210.0 | 217.4–366.4 | <0.01 |
| Protein (g) | 6.1 | 13.3 | 1.33–10.8 | <0.01 |
| Fat (g) | 15.6 | 14.6 | 10.4–20.8 | <0.01 |
| Carbohydrate (g) | 31.1 | 46.9 | 14.5–47.8 | <0.01 |
| Nutrition and natural disaster preparedness knowledge of older people (baseline-week II) | 11.8 | 21.7 | 4.1–19.5 | <0.01 |
| Mean (SD) Macronutrient Intake | Mean Macronutrient Intakes as Percentage of RDA | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nutrient | Baseline | At the Second Week | Baseline | At the Second Week | ||||||||
| Mean | DS | Mean | DS | Mean | DS | Mean | DS | Male | Female | Male | Female | |
| Energy (kcal) | 828.60 | 317.56 | 52.67 | 15.62 | 1271.90 | 296.04 | 69.33 | 14.19 | 46.03 | 52.67 | 70.66 | 69.33 |
| Protein (g) | 29.90 | 11.40 | 47.81 | 20.25 | 37.68 | 10.13 | 57.62 | 17.73 | 46.74 | 47.81 | 58.88 | 57.62 |
| Fat (g) | 27.95 | 9.39 | 63.47 | 28.66 | 45.05 | 10.57 | 97.32 | 21.67 | 55.90 | 63.47 | 90.10 | 97.32 |
| Carbohydrate (g) | 129.67 | 80.90 | 52.77 | 19.52 | 180.68 | 50.52 | 64.38 | 11.68 | 47.15 | 52.77 | 65.70 | 64.38 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fatmah, F.; Utomo, S.W.; Lestari, F. Broccoli-Soybean-Mangrove Food Bar as an Emergency Food for Older People during Natural Disaster. Int. J. Environ. Res. Public Health 2021, 18, 3686. https://doi.org/10.3390/ijerph18073686
Fatmah F, Utomo SW, Lestari F. Broccoli-Soybean-Mangrove Food Bar as an Emergency Food for Older People during Natural Disaster. International Journal of Environmental Research and Public Health. 2021; 18(7):3686. https://doi.org/10.3390/ijerph18073686
Chicago/Turabian StyleFatmah, Fatmah, Suyud Warno Utomo, and Fatma Lestari. 2021. "Broccoli-Soybean-Mangrove Food Bar as an Emergency Food for Older People during Natural Disaster" International Journal of Environmental Research and Public Health 18, no. 7: 3686. https://doi.org/10.3390/ijerph18073686
APA StyleFatmah, F., Utomo, S. W., & Lestari, F. (2021). Broccoli-Soybean-Mangrove Food Bar as an Emergency Food for Older People during Natural Disaster. International Journal of Environmental Research and Public Health, 18(7), 3686. https://doi.org/10.3390/ijerph18073686







