Blood Donations and Transfusions during the COVID-19 Pandemic in Spain: Impact According to Autonomous Communities and Hospitals
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants/Scope of the Study
2.3. Period Studied
2.4. Study Variables
2.5. Data Collection
2.6. Statistical Analysis
3. Results
3.1. Activity in Spain
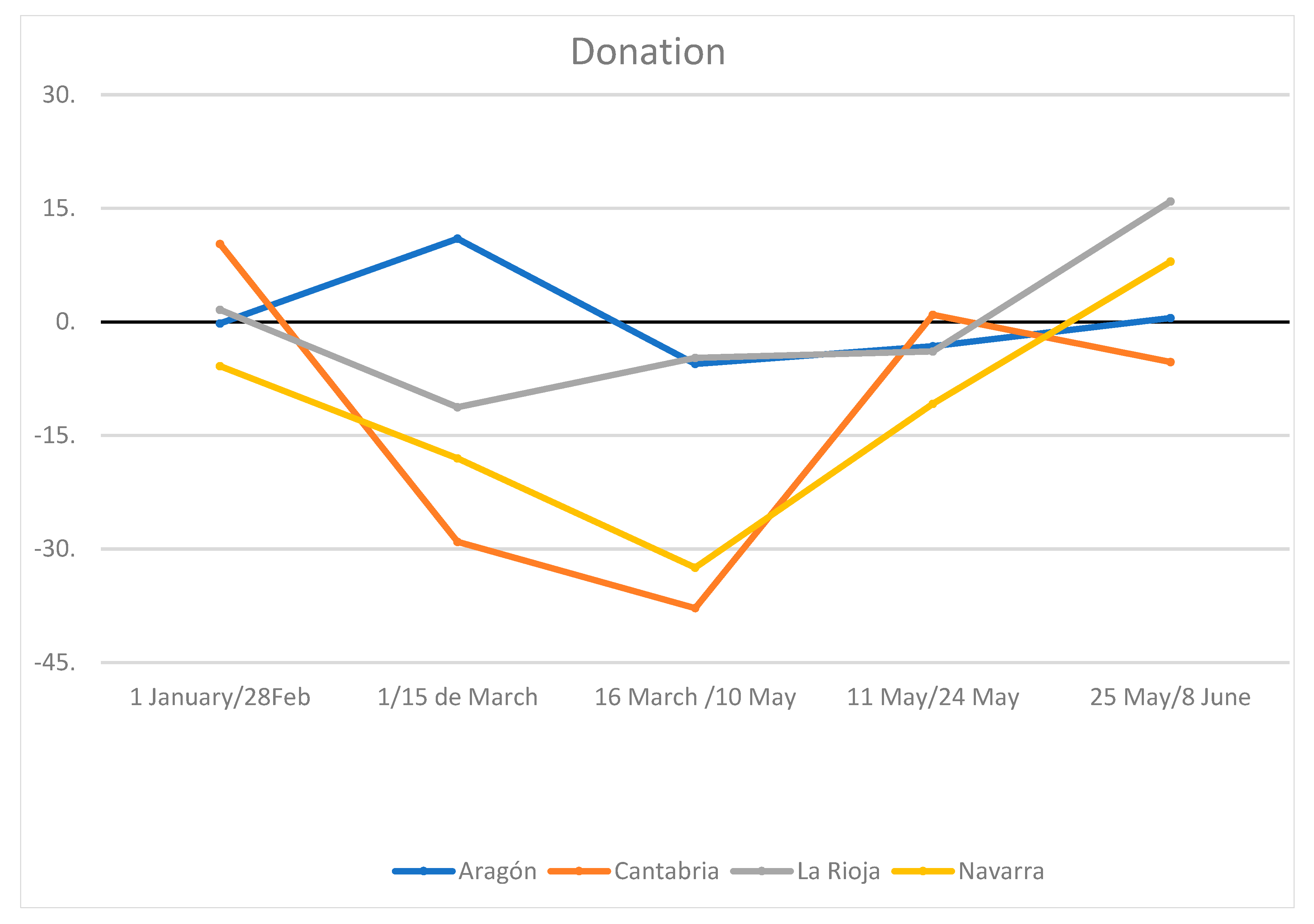
3.2. Donations
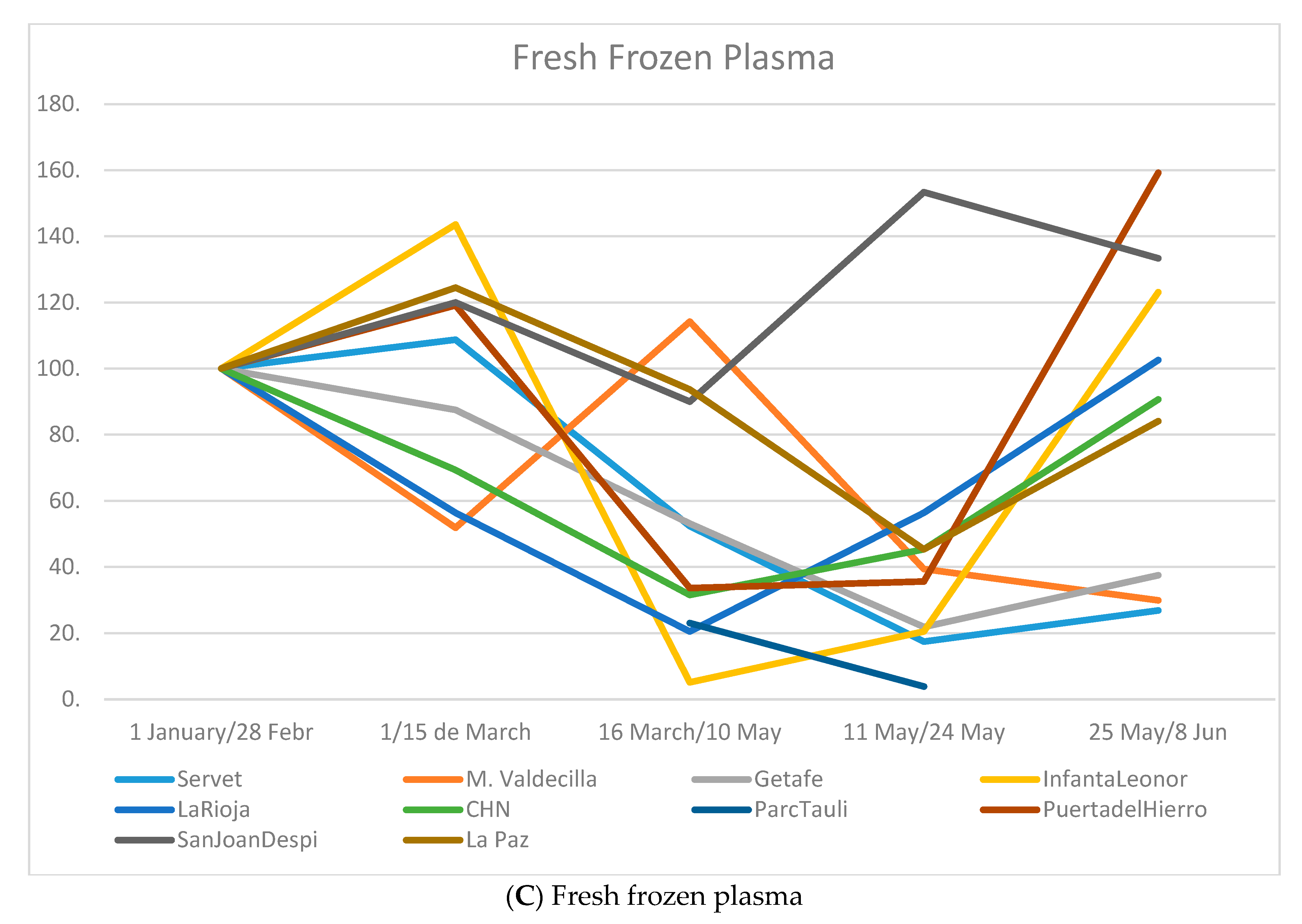
3.3. Distribution
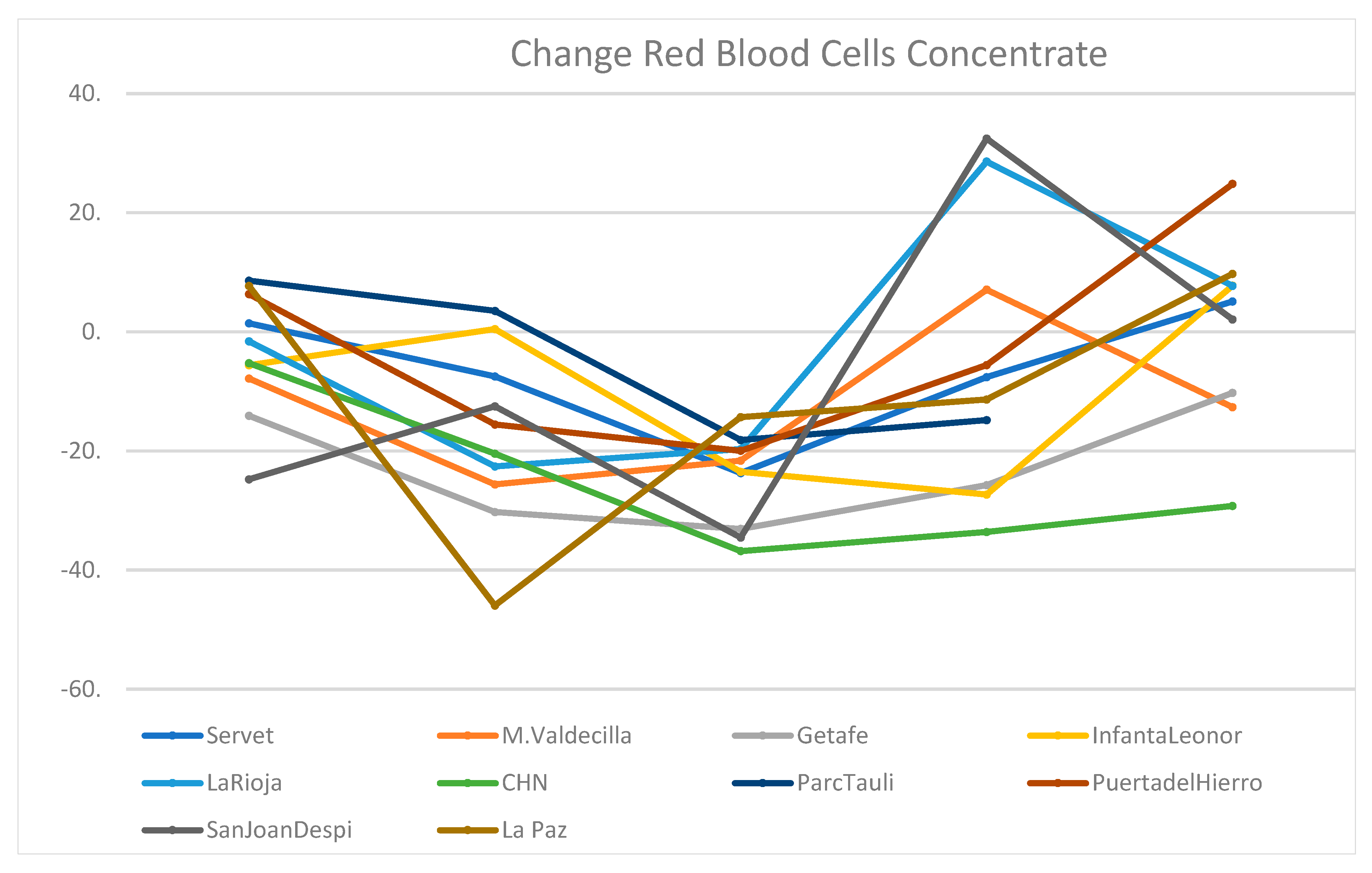
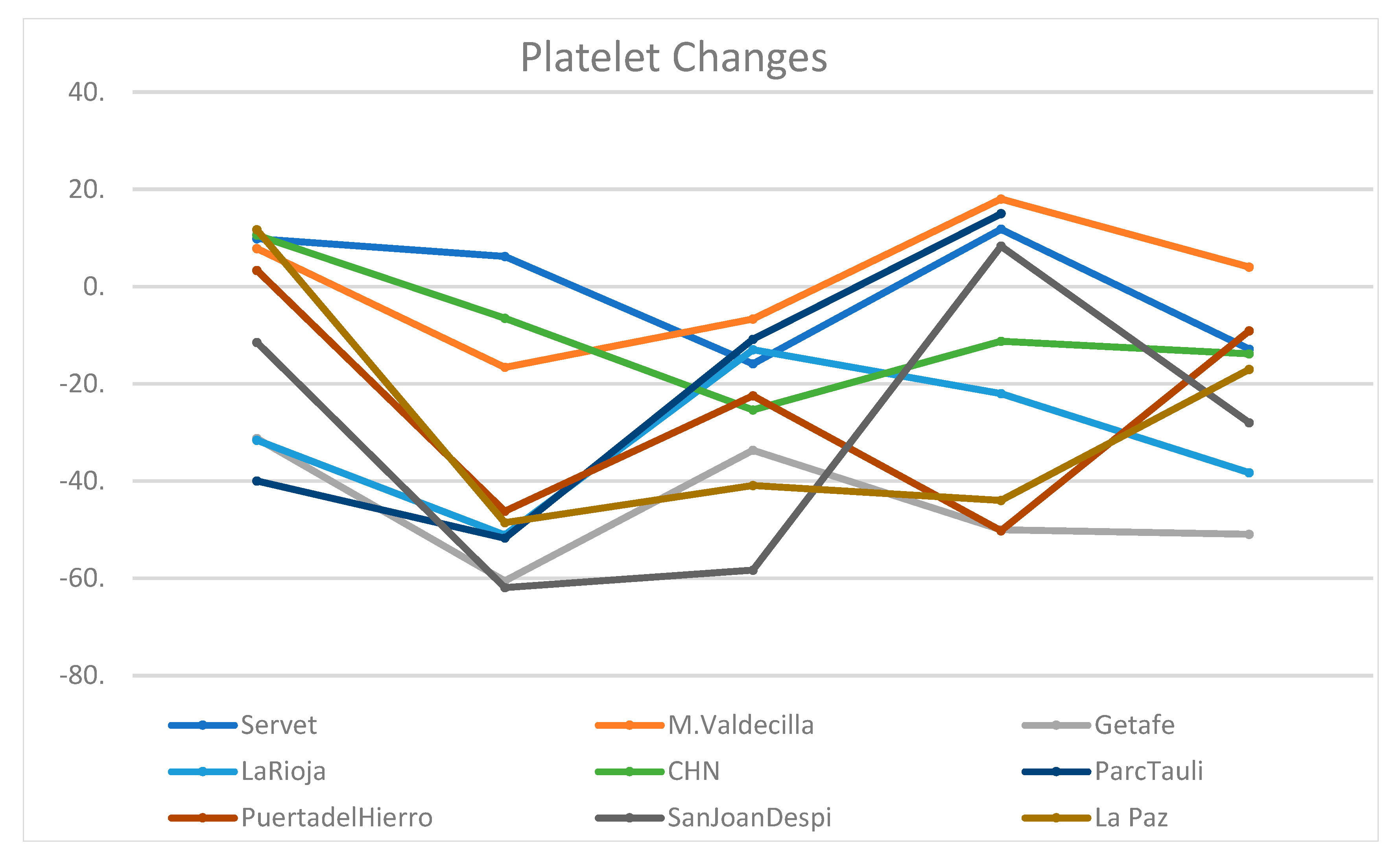
3.4. Consumption of Blood Components
3.5. Shortage
3.6. Hemovigilance
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| 1 January–28 February | 1–15 March | 16–10 May | 11–24 May | 25 May–8 June | 11 May–8 June | 16 March–8 June | ||
|---|---|---|---|---|---|---|---|---|
| Navarra | 2020 | 3573.0. | 803.0 | 2372.0 | 744.0 | 719.0 | 3835.0 | 1463.0 |
| Mean 18–19 | 3740.0 | 931 | 3393 | 851 | 938 | 5182 | 1789 | |
| Difference (%) | −4.5 | −13.8 | −30.1 | −12.6 | −23.6 | −26.0 | −18.2 | |
| La Rioja | 2020 | 1521.0 | 305 | 1157 | 371 | 397 | 1925 | 768 |
| Mean 18–19 | 1545.5 | 394 | 1440 | 288.5 | 368.5 | 2097 | 657 | |
| Difference (%) | −1.6 | −22.6 | −19.7 | 28.6 | 7.7 | −8.2 | +16.9 | |
| Cantabria | 2020 | 3445.0 | 718 | 2259 | 794 | 638 | 3691 | 1432 |
| Mean 18–19 | 3425.0 | 892.5 | 2948 | 775 | 793 | 4516 | 1568 | |
| Difference (%) | 0.6 | −19.5 | −23.4 | 2.4 | −19.6 | −18.3 | −8.7 | |
| Total | Average percentage change | −1.8 (−8.1, 4.7) | −18.6 (−29.7, −7.5) | −24.4 (−37.5, −11.3) | 6.2 (−45.6, 57.9) | −11.7 (−53.8, 30.4) | −17.5 (−39.7, 4.7) | −3.3 (−48.4, 41.8) |
| p-value | 0.339 | 0.019 | 0.015 | 0.660 | 0.354 | 0.077 | 0.781 |
| 1 January–28 February | 1–15 March | 16–10 May | 11–24 May | 25 May–8 June | 11 May–8 June | 16 March–8 June | ||
|---|---|---|---|---|---|---|---|---|
| Navarra | 2020 | 809.0 | 186 | 560 | 195 | 182 | 377 | 937 |
| Mean 18–19 | 630.0 | 126 | 568.5 | 156 | 170 | 326 | 894.5 | |
| Difference (%) | 28.4 | 47.6 | −1.5 | +25.0 | +7.1 | +15.6 | +4.7 | |
| La Rioja | 2020 | 92.0 | 22 | 124 | 23 | 25 | 48 | 172 |
| Mean 18–19 | 134.5 | 45 | 142.5 | 29.5 | 40.5 | 70 | 212.5 | |
| Difference (%) | −31.6 | −51.1 | −13.0 | −22.0 | −38.3 | −31.4 | −19.1 | |
| Cantabria | 2020 | 568.0 | 117 | 443 | 118 | 129 | 247 | 690 |
| Mean 18–19 | 564.5 | 132.5 | 503 | 121.5 | 131.5 | 253 | 756 | |
| Difference (%) | 0.6 | −11.7 | −11.9 | −2.9 | −1.9 | −2.4 | −8.7 | |
| Total | Average percentage change | −0.9 (−75.5, 73.8) | −5.1 (−128−5, 118.4) | −8.8 (−24.6, 7.0) | 0.03 (−58.7, 58.8) | −11.0 (−70.7, 48.6) | −6.1 (−65.0, 52.8) | −7.7 (−37.3, 21.9) |
| p-value | 0.965 | 0.876 | 0.138 | 0.999 | 0.509 | 0.701 | 0.378 |
| 1 January–28 February | 1–15 March | 16–10 May | 11–24 May | 25 May–8 June | 11 May–8 June | 16 March–8 June | ||
|---|---|---|---|---|---|---|---|---|
| Navarra | 2020 | 364 | 54 | 179 | 40 | 83 | 123 | 302 |
| Mean 18–19 | 577 | 114 | 410.5 | 112 | 94 | 206 | 616.5 | |
| Difference (%) | −37.0 | −52.6 | −56.4 | −64.3 | −11.7 | −40.3 | −51.0 | |
| La Rioja | 2020 | 78 | 11 | 16 | 22 | 20 | 42 | 58 |
| Mean 18–19 | 111 | 50.5 | 309 | 28 | 91 | 119 | 428 | |
| Difference (%) | −29.7 | −78.2 | −94.8 | −21.4 | −78.0 | −64.7 | −86.5 | |
| Cantabria | 2020 | 285 | 48 | 322 | 39 | 30 | 69 | 413 |
| Mean 18–19 | 331 | 458.5 | 249.5 | 70 | 81.5 | 151.5 | 401 | |
| Difference (%) | −13.9 | −1.0 | 29.1 | −44.3 | −63.2 | −54.5 | +3.0 | |
| Total | Average percentage change | −27.9 (−56.2, 2.4) | −44.0 (−141.6, 53.7) | −40.7 (−198.2, 116.8) | −43.3 (−96.6, 9.9) | −51.0 (−137.4, 35.5) | −53.3 (−83.8, −22.7) | −44.8 (−156.8, 67.1) |
| p-value | 0.059 | 0.192 | 0.382 | 0.073 | 0.127 | 0.017 | 0.227 |
Appendix B

References
- Arcot, P.J.; Kumar, K.; Mukhopadhyay, T.; Subramanian, A. Potential challenges faced by blood bank services during COVID-19 pandemic and their mitigative measures: The Indian scenario. Transfus. Apher. Sci. 2020, 59, 102877. [Google Scholar] [CrossRef]
- Stanworth, S.J.; New, H.V.; O Apelseth, T.; Brunskill, S.; Cardigan, R.; Doree, C.; Germain, M.; Goldman, M.; Massey, E.; Prati, D.; et al. Effects of the COVID-19 pandemic on supply and use of blood for transfusion. Lancet Haematol. 2020, 7, e756–e764. [Google Scholar] [CrossRef]
- Cai, X.; Ren, M.; Chen, F.; Li, L.; Lei, H.; Wang, X. Blood transfusion during the COVID-19 outbreak. Blood Transfus. 2020, 18, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Ou-Yang, J.; Li, S.; Bei, C.; He, B.; Chen, J.; Liang, H.; Fu, Y. Blood donor recruitment in Guangzhou, China, during the 2019 novel coronavirus (COVID-19) epidemic. Transfusion 2020, 60, 2597–2610. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Han, W.; Pan, L.; Wang, C.; Liu, Y.; Hu, W.; Zhou, H.; Zheng, X. Impact of COVID-19 on blood centres in Zhejiang province China. Vox Sang. 2020, 115, 502–506. [Google Scholar] [CrossRef] [PubMed]
- Raturi, M.; Kusum, A. The blood supply management amid the COVID-19 outbreak. Transfus. Clin. Biol. 2020, 27, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Yahia, A.I.O. Management of blood supply and demand during the COVID-19 pandemic in King Abdullah Hospital, Bisha, Saudi Arabia. Transfus. Apher. Sci. 2020, 59, 102836. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, S.; Yazdi, S.M.T.; Eshghi, P.; Norooznezhad, A.H. Coronavirus disease 2019 (COVID-19) and decrease in blood donation: Experience of Iranian Blood Transfusion Organization (IBTO). Vox Sang. 2020, 115, 595–596. [Google Scholar] [CrossRef] [PubMed]
- Grandone, E.; Mastroianno, M.; Caroli, A.; Ostuni, A. Blood supply and transfusion support in southern Italy: Findings during the first four weeks of the SARS-CoV-2 pandemic. Blood Transfus. 2020, 18, 230–232. [Google Scholar] [CrossRef] [PubMed]
- Pagano, M.B.; Hess, J.R.; Tsang, H.C.; Staley, E.; Gernsheimer, T.; Sen, N.; Clark, C.; Nester, T.; Bailey, C.; Alcorn, K. Prepare to adapt: Blood supply and transfusion support during the first 2 weeks of the 2019 novel coronavirus (COVID-19) pandemic affecting Washington State. Transfusion 2020, 60, 908–911. [Google Scholar] [CrossRef] [PubMed]
- Sistema de Información del Sistema Nacional para la Seguridad Transfusional (SISNST). Transfusión y Coronavirus. Infección por Nuevo Coronavirus (COVID-19). Acuerdos del Comité Científico de Seguridad Transfusional (CCST). Unidad de Hemoterapia. Subdirección General de Promoción de la Salud y Vigilancia en Salud Pública. Dirección General de Salud Pública, Calidad e Innovación. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/medicinaTransfusional/acuerdos/docs/COVID-19_Tranfusion_nuevo_Coronavirus.pdf (accessed on 1 October 2020).
- Asociación Española de Cirujanos. Recomendaciones Generales de Actuación y Organización Básica a Servicios de Cirugía en Zonas con Alta Afectación por la Pandemia por COVID-19 (SARS COV-2). Available online: https://www.aecirujanos.es/files/noticias/152/documentos/Recomendaciones_Servicio_Alta(1).pdf (accessed on 15 October 2020).
- Domínguez-Gil, B.; Coll, E.; Ferrer-Fàbrega, J.; Briceño, J.; Ríos, A. Drástico impacto de la epidemia de COVID-19 sobre la actividad de donación y trasplante en España. Cirugía Española 2020, 98, 412–414. [Google Scholar] [CrossRef] [PubMed]
- Sistema de Información del Sistema Nacional para la Seguridad Transfusional (SISNST). Actividad Centros y Servicios Transfusión, Informe 2018. Unidad de Hemoterapia, Subdirección General de Promoción de la Salud y Vigilancia en Salud Pública. Dirección General de Salud Pública, Calidad e Innovación. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/medicinaTransfusional/indicadores/docs/Informe_Actividad2018.pdf (accessed on 18 January 2020).
- COVIDSurg Collaborative; Nepogodiev, D.; Bhangu, A. Elective surgery cancellations due to the COVID-19 pandemic: Global predictive modelling to inform surgical recovery plans. Br. J. Surg. 2020, 107, 1440–1449. [Google Scholar] [CrossRef] [PubMed]
- Doughty, H.; Green, L.; Callum, J.; Murphy, M.F. National Blood Transfusion Committee Triage tool for the rationing of blood for massively bleeding patients during a severe national blood shortage: Guidance from the National Blood Transfusion Committee. Br. J. Haematol. 2020, 191, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Marcos, S.Z.; Martí, I.P.; Caamaño, M.L.A.; Garraza, J.M.D.M.; Guillén, M.L.A.; Rodríguez, E.M.; Azparren, A.A.; López, A.T.; Jiménez, A.G.; Erce, J.A.G. Efecto de la aplicación del programa Patient blood management en el abordaje de las artroplastias de cadera y rodilla programada. Med. Clín. 2020, 155, 425–433. [Google Scholar] [CrossRef]
- Ripollés-Melchor, J.; Abad-Motos, A.; Díez-Remesal, Y.; Aseguinolaza-Pagola, M.; Padin-Barreiro, L.; Sánchez-Martín, R.; Logroño-Egea, M.; Catalá-Bauset, J.C.; García-Orallo, S.; Bisbe, E.; et al. Association between Use of Enhanced Recovery after Surgery Protocol and Postoperative Complications in Total Hip and Knee Arthroplasty in the Postoperative Outcomes within Enhanced Recovery after Surgery Protocol in Elective Total Hip and Knee Arthroplasty Study (POWER2). JAMA Surg. 2020, 155, e196024. [Google Scholar] [CrossRef] [PubMed]
- Encuesta Nacional Sobre ERAS Tras la Pandemia COVID19. 2020. Available online: https://docs.google.com/forms/d/e/1FAIpQLSe-3hKDPzDrPkXoJKScCwJWcldMjY376WcS1HxolXE61hdimQ/closedform (accessed on 1 October 2020).
- Bisbe, E.; Garcia-Casanovas, A.; Illa, C.; Varela, J.; Basora, M.; Barquero, M.; Colomina, M.J.; González, L.; Hofmann, A.; Rodríguez, L.E.F.; et al. Maturity Assessment model for Patient Blood Management to assist hospitals in improving patients’ safety and outcomes. The MAPBM project. Blood Transfus. 2020. [Google Scholar] [CrossRef]
- World Health Organization. Action Framework to Advance Universal Access to Safe, Effective and Quality-Assured Blood Products 2020–2023. Available online: https://www.who.int/publications/i/item/action-framework-to-advance-uas-bloodprods-978-92-4-000038-4 (accessed on 7 October 2020).
- Shander, A.; Goobie, S.M.; Warner, M.A.; Aapro, M.; Bisbe, E.; Perez-Calatayud, A.A.; Callum, J.; Cushing, M.M.; Dyer, W.B.; Erhard, J.; et al. International Foundation of Patient Blood Management (IFPBM) and Society for the Advancement of Blood Management (SABM) Work Group. Essential Role of Patient Blood Management in a Pandemic: A Call for Action. Anesth. Analg. 2020, 131, 74–85. [Google Scholar] [CrossRef] [PubMed]
- Baron, D.M.; Franchini, M.; Goobie, S.M.; Javidroozi, M.; Klein, A.A.; Lasocki, S.; Liumbruno, G.M.; Muñoz, M.; Shander, A.; Spahn, D.R.; et al. Patient blood management during the COVID-19 pandemic: A narrative review. Anaesthesia 2020, 75, 1105–1113. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Rodríguez, J.M.; Erce, J.A.G.; Sebastián, A.A. «Regreso al futuro»: Tras la pandemia debemos intensificar la recuperación. Cirugía Española 2021, 99, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Ripolles-Melchor, J.; Jericó-Alba, C.; Quintana-Díaz, M.; García-Erce, J.A. Del ahorro de sangre al patient blood management. Med. Clín. 2018, 151, 368–373. [Google Scholar] [CrossRef] [PubMed]

| 9–15 March | 16–22 March | 23–29 March | 30 March–3 April | 6–12 April | 13–19 April | 20–26 April | 27 April–3 May | 4–10 May | 11–17 May | 18–24 May | 25–31 May | 1–7 June | 8–14 June | 15–21 June | 22–28 June | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Week | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 |
| Donation | 33,760 | 30,151 | 22,595 | 21,899 | 20,496 | 22,395 | 26,541 | 24,688 | 27,480 | 32,997 | 32,748 | 32,174 | 31,562 | 32,589 | 35,239 | 28,085 |
| Difference | 2880 | −729 | −8285 | −8981 | −10,384 | −8485 | −4339 | −6192 | −3400 | 2117 | 1868 | 1294 | 682 | 1709 | 4359 | −2795 |
| (%) | 9.3 | −2.4 | −26.8 | −29.1 | −33.6 | −27.5 | −14.1 | −20.1 | −11.0 | +6.9 | +6.1 | +4.2 | +2.2 | +5.5 | +14.1 | −9.1 |
| Region | January and February | 1–15 March | 16 March–10 May | 11–24 May | 25 May–8 June | 11 May–8 June | 16 March–8 June | |
|---|---|---|---|---|---|---|---|---|
| Navarra | 2020 | 3581 | 800 | 2294 | 773 | 983 | 1756 | 4050 |
| Mean 18–19 | 3803.5 | 976 | 3396.5 | 867 | 910.5 | 1777.5 | 5174 | |
| Difference (%) | −5.8 | −18.0 | −32.5 | −10.8 | 8.0 | 0.1 | −21.7 | |
| Aragón | 2020 | 7155 | 1816 | 5536 | 1668 | 1889 | 3557 | 9093 |
| Mean 18–19 | 7170 | 1636 | 5861.5 | 1723.5 | 1879.5 | 3603 | 9464.5 | |
| Difference (%) | −0.21 | 11.0 | −5.6 | −3.2 | −0.5 | −1.3 | −3.9 | |
| La Rioja | 2020 | 1663 | 397 | 1522 | 394 | 470 | 864 | 2386 |
| Mean 18–19 | 1637 | 447.5 | 1598 | 410 | 405.5 | 815.5 | 2413.5 | |
| Difference (%) | 1.6 | −11.3 | −4.8 | −3.9 | +15.9 | +5.9 | −1.1 | |
| Cantabria | 2020 | 4139 | 642 | 2018 | 818 | 793 | 1611 | 3629 |
| Mean 18–19 | 3752.5 | 905 | 3245 | 810.5 | 837.5 | 1648 | 4893 | |
| Difference (%) | 10.3 | −29.1 | −37.8 | +0.9 | −5.3 | −2.2 | −25.8 | |
| Total | Average percentage change | 1.5 (−9.2, 12.1) | −11.8 (−38.7, 15.1) | −20.1 (−47.9, 7.6) | −4.3 (−12.0, 3.5) | 4.8 (−9.9, 19.4) | 0.6 (−5.2, 6.4) | −13.1 (−32.9, 6.7) |
| p-value | 0.693 | 0.256 | 0.104 | 0.179 | 0.377 | 0.754 | 0.125 |
| 1 January–28 February | 1–15 March | 16 March–10 May | 11–24 May | 25 May–8 June | ||
|---|---|---|---|---|---|---|
| Red Blood Cells | Average (%) | −3.6 (−11.0, 3.9) | −17.6 (−28.2, −7.1) | −24.5 (−30.0, −19.1) | −5.8 (−21.9, 10.3) | 0.6 (−11.5, 12.7) |
| p-value | 0.307 | 0.004 | <0.001 | 0.437 | 0.915 | |
| Platelets | Average (%) | 2.4 (−25.9, 29.8) | −2.65 (−83.2, 77.9) | −25.3 (−36.5, −14.1) | −16.9 (−37.5, 3.7) | −22.9 (−36.4, −9.4) |
| p-value | 0.846 | 0.942 | 0.001 | 0.097 | 0.005 | |
| Plasma | Average (%) | −15.6 (−53.7, 22.5) | 16.0 (−59.4, 91.3) | −45.3 (−76.7, −14.6) | −9.1 (−49.1, 30.8) | −32.9 (−74.1, 8.3) |
| p-value | 0.379 | 0.638 | 0.009 | 0.618 | 0.103 |
| 1 January–28 February | 1–15 de March | 16 March–10 May | 11–24 May | 25 May–8 June | ||
|---|---|---|---|---|---|---|
| Navarra | 2020 | 2410.0 | 554.0 | 1502.0 | 717.0 | 510.0 |
| Mean 18–19 | 2543.5 | 696.5 | 2405.5 | 1080.0 | 720.5 | |
| Difference (%) | −5.25 | −20.46 | −36.91 | −33.61 | −29.22 | |
| Aragón | 2020 | 2399.00 | 581.00 | 1673.00 | 498.00 | 597.00 |
| Mean 18–19 | 2365.00 | 628.00 | 2193.00 | 539.00 | 568.00 | |
| Difference (%) | 1.44 | −7.48 | −23.71 | −7.61 | 5.11 | |
| La Rioja | 2020 | 1521.00 | 305.00 | 1157.00 | 371.00 | 397.00 |
| Mean 18–19 | 1545.50 | 394.00 | 1440.50 | 288.50 | 368.50 | |
| Difference (%) | −1.59 | −22.59 | −19.68 | 28.60 | 7.73 | |
| Valdecilla | 2020 | 2303.0 | 463.0 | 1642.0 | 597.0 | 507.0 |
| Mean 18–19 | 2499.0 | 622.5 | 2095.0 | 557.5 | 580.5 | |
| Difference (%) | −7.84 | −25.62 | −21.62 | 7.09 | −12.66 | |
| Parc Tauli | 2020 | 1086 | 249.00 | 773.00 | 224.00 | |
| Mean 18–19 | 1000 | 240.50 | 944.50 | 263.00 | ||
| Difference (%) | 8.6 | 3.53 | −18.16 | −14.83 | ||
| San Joan Despi | 2020 | 626 | 175.00 | 489.00 | 202.00 | 171.0 |
| Mean 18–19 | 832.0 | 200.00 | 747.00 | 152.50 | 167.5 | |
| Difference (%) | −24.76 | −12.50 | −34.54 | 32.46 | 2.09 | |
| La Paz | 2020 | 3604.0 | 714.00 | 2634.00 | 667.00 | 794.0 |
| Mean 18–19 | 3346.0 | 1321.00 | 3074.50 | 752.50 | 723.5 | |
| Difference (%) | 7.71 | −45.95 | −14.33 | −11.36 | 9.74 | |
| Getafe | 2020 | 878.0 | 197.0 | 620.0 | 192.0 | 193.0 |
| Mean 18–19 | 1022.0 | 282.5 | 926.5 | 258.5 | 215.0 | |
| Difference (%) | −14.09 | −30.27 | −33.08 | −25.73 | −10.23 | |
| Puerta del Hierro | 2020 | 2327.0 | 483.0 | 1539.0 | 499.0 | 598.0 |
| Mean 18–19 | 2188.5 | 572.0 | 1923.0 | 528.5 | 479.0 | |
| Difference (%) | 6.33 | −15.56 | −19.97 | −5.58 | 24.84 | |
| Infanta Leonor | 2020 | 881.0 | 209.0 | 547.0 | 145.0 | 201.0 |
| Mean 18–19 | 933.5 | 208.0 | 715.0 | 199.5 | 186.5 | |
| Difference (%) | −5.62 | 0.48 | −23.50 | −27.32 | 7.77 | |
| Total | Average percentage change | −3.6 (−11.0, 3.9) | −17.6 (−28.2, −7.1) | −24.5 (−30.0, −19.1) | −5.8 (−21.9, 10.3) | 0.6 (−11.5, 12.7) |
| p-value | 0.307 | 0.004 | <0.001 | 0.437 | 0.915 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Erce, J.A.; Romón-Alonso, Í.; Jericó, C.; Domingo-Morera, J.M.; Arroyo-Rodríguez, J.L.; Sola-Lapeña, C.; Bueno-Cabrera, J.L.; Juárez-Vela, R.; Zalba-Marcos, S.; Abad-Motos, A.; et al. Blood Donations and Transfusions during the COVID-19 Pandemic in Spain: Impact According to Autonomous Communities and Hospitals. Int. J. Environ. Res. Public Health 2021, 18, 3480. https://doi.org/10.3390/ijerph18073480
García-Erce JA, Romón-Alonso Í, Jericó C, Domingo-Morera JM, Arroyo-Rodríguez JL, Sola-Lapeña C, Bueno-Cabrera JL, Juárez-Vela R, Zalba-Marcos S, Abad-Motos A, et al. Blood Donations and Transfusions during the COVID-19 Pandemic in Spain: Impact According to Autonomous Communities and Hospitals. International Journal of Environmental Research and Public Health. 2021; 18(7):3480. https://doi.org/10.3390/ijerph18073480
Chicago/Turabian StyleGarcía-Erce, José Antonio, Íñigo Romón-Alonso, Carlos Jericó, José María Domingo-Morera, José Luis Arroyo-Rodríguez, Carlos Sola-Lapeña, José Luis Bueno-Cabrera, Raúl Juárez-Vela, Saioa Zalba-Marcos, Ane Abad-Motos, and et al. 2021. "Blood Donations and Transfusions during the COVID-19 Pandemic in Spain: Impact According to Autonomous Communities and Hospitals" International Journal of Environmental Research and Public Health 18, no. 7: 3480. https://doi.org/10.3390/ijerph18073480
APA StyleGarcía-Erce, J. A., Romón-Alonso, Í., Jericó, C., Domingo-Morera, J. M., Arroyo-Rodríguez, J. L., Sola-Lapeña, C., Bueno-Cabrera, J. L., Juárez-Vela, R., Zalba-Marcos, S., Abad-Motos, A., Gea-Caballero, V., Santolalla-Arnedo, I., & Quintana-Díaz, M. (2021). Blood Donations and Transfusions during the COVID-19 Pandemic in Spain: Impact According to Autonomous Communities and Hospitals. International Journal of Environmental Research and Public Health, 18(7), 3480. https://doi.org/10.3390/ijerph18073480








