Health Literacy, Digital Health Literacy, and COVID-19 Pandemic Attitudes and Behaviors in U.S. College Students: Implications for Interventions
Abstract
1. Introduction
2. Materials and Methods
2.1. Sampling
2.2. Variables
2.2.1. Demographics
2.2.2. Health Literacy
2.2.3. Digital Health Literacy
2.2.4. Digital Health Information Sources
2.2.5. COVID-19 Attitudes and Behaviors
2.2.6. Social Network
2.3. Analysis
3. Results
3.1. Demographics
3.2. Health Literacy
3.3. Digital Health Literacy
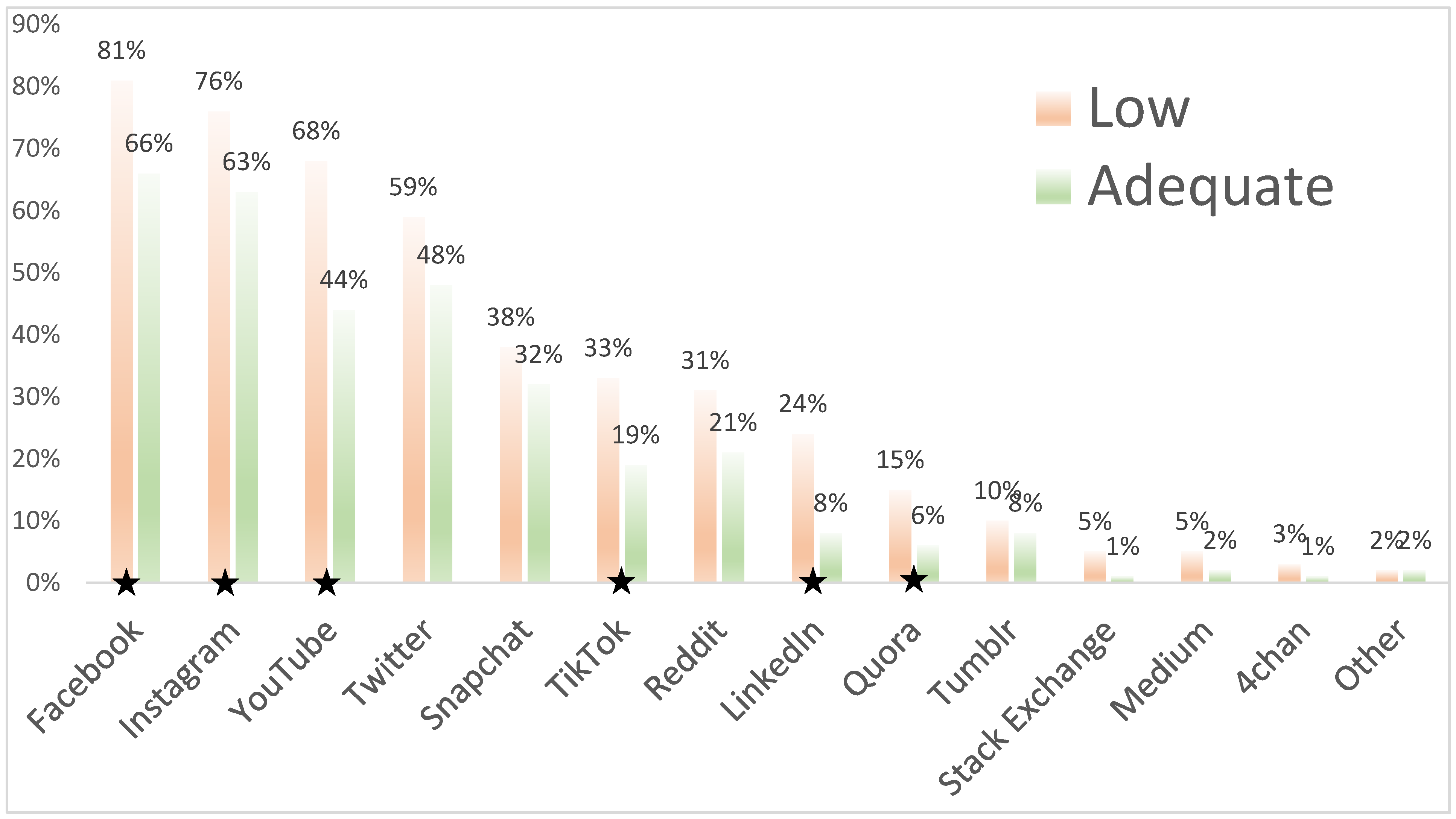
3.4. Digital Information Sources
3.5. Attitudes and Behaviors
3.6. Social Networks
3.7. Multivariable Models
4. Discussion
4.1. Implications
4.2. Limitations
4.3. Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Managing the COVID-19 Infodemic: Promoting Healthy Behaviours and Mitigating the Harm from Misinformation and Disinformation. Joint Statement by WHO, UN, UNICEF, UNDP, UNESCO, UNAIDS, ITU, UN Global Pulse, and IFRC. Available online: https://www.who.int/news/item/23-09-2020-managing-the-covid-19-infodemic-promoting-healthy-behaviours-and-mitigating-the-harm-from-misinformation-and-disinformation (accessed on 14 December 2020).
- Kearney, M.D.; Chiang, S.C.; Massey, P.M. The Twitter origins and evolution of the COVID-19 “plandemic” conspiracy theory. Harv. Kennedy Sch. Misinf. Rev. 2020, 1. [Google Scholar] [CrossRef]
- Duplaga, M. The Determinants of Conspiracy Beliefs Related to the COVID-19 Pandemic in a Nationally Representative Sample of Internet Users. Int. J. Environ. Res. Public Health 2020, 17, 7818. [Google Scholar] [CrossRef] [PubMed]
- Sentell, T.; Vamos, S.; Okan, O. Interdisciplinary Perspectives on Health Literacy Research Around the World: More Important Than Ever in a Time of COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 3010. [Google Scholar] [CrossRef]
- Paakkari, L.; Okan, O. COVID-19: Health literacy is an underestimated problem. Lancet Public Health 2020, 5, e249–e250. [Google Scholar] [CrossRef]
- Sørensen, K.; Messer, M.; Okan, O. COVID-19: A Guide to Good Practice on Keeping People Well Informed. Available online: https://theconversation.com/covid-19-a-guide-to-good-practice-on-keeping-people-well-informed-134046 (accessed on 1 March 2021).
- Berkman, N.D.; Davis, T.C.; McCormack, L. Health Literacy: What Is It? J. Health Commun. 2010, 15, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Norman, C.D.; Skinner, H.A. eHealth Literacy: Essential Skills for Consumer Health in a Networked World. J. Med. Internet Res. 2006, 8, e9. [Google Scholar] [CrossRef] [PubMed]
- Ortiz, D.N. Digital Health Literacy. In Proceedings of the First Meeting of the WHO GCM/NCD Working Group on Health Literacy for NCDs 2017, Geneva, Switzerland, 27–28 February 2017. [Google Scholar]
- Van der Vaart, R.; Drossaert, C. Development of the Digital Health Literacy Instrument: Measuring a Broad Spectrum of Health 1.0 and Health 2.0 Skills. J. Med. Internet Res. 2017, 19, e27. [Google Scholar] [CrossRef] [PubMed]
- Stellefson, M.; Hanik, B.; Chaney, B.; Chaney, D.; Tennant, B.; Chavarria, E.A. eHealth literacy among college students: A systematic review with implications for eHealth education. J. Med. Internet Res. 2011, 13, e102. [Google Scholar] [CrossRef]
- Escoffery, C.; Miner, K.R.; Adame, D.D.; Butler, S.; McCormick, L.; Mendell, E. Internet use for health information among college students. J. Am. Coll. Health 2005, 53, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Britt, R.K.; Collins, W.B.; Wilson, K.; Linnemeier, G.; Englebert, A.M. eHealth Literacy and Health Behaviors Affecting Modern College Students: A Pilot Study of Issues Identified by the American College Health Association. J. Med. Internet Res. 2017, 19, e392. [Google Scholar] [CrossRef]
- Horgan, Á.; Sweeney, J. University Students’ Online Habits and Their Use of the Internet for Health Information. CIN Comput. Inform. Nurs. 2012, 30, 402–408. [Google Scholar] [CrossRef]
- Levin-Zamir, D.; Bertschi, I. Media Health Literacy, eHealth Literacy, and the Role of the Social Environment in Context. Int. J. Environ. Res. Public Health 2018, 15, 1643. [Google Scholar] [CrossRef]
- Jackson, D.N.; Trivedi, N.; Baur, C. Re-prioritizing Digital Health and Health Literacy in Healthy People 2030 to Affect Health Equity. Health Commun. 2020, 1–8. [Google Scholar] [CrossRef]
- National Student Clearinghouse Research Center. Current Term Enrollment Estimates: Fall 2020; National Center for Education Statistics: Washington, DC, USA, 2020. [Google Scholar]
- Chesser, A.; Ham, A.D.; Woods, N.K. Assessment of COVID-19 Knowledge Among University Students: Implications for Future Risk Communication Strategies. Health Educ. Behav. 2020, 47, 540–543. [Google Scholar] [CrossRef]
- Dadaczynski, K.; Okan, O.; Messer, M.; Leung, A.Y.M.; Rosário, R.; Darlington, E.; Rathmann, K. Digital Health Literacy and Web-Based Information-Seeking Behaviors of University Students in Germany During the COVID-19 Pandemic: Cross-sectional Survey Study. J. Med. Internet Res. 2021, 23, e24097. [Google Scholar] [CrossRef] [PubMed]
- Dadaczynski, K.; Okan, O.; Rathmann, K. COVID-19 Health Literacy Survey: University Students (COVID-HL-Survey). Questionnaire and Scale Documentation; Bielefeld University, Interdisciplinary Centre for Health Literacy Research: Bielefeld, Germany; Fulda University of Applied Sciences, Public Health Centre: Fulda, Germany, 2020. [Google Scholar]
- Nguyen, H.T.; Do, B.N.; Pham, K.M.; Kim, G.B.; Dam, H.T.B.; Nguyen, T.T.; Nguyen, T.T.P.; Nguyen, Y.H.; Sørensen, K.; Pleasant, A.; et al. Fear of COVID-19 Scale—Associations of Its Scores with Health Literacy and Health-Related Behaviors among Medical Students. Int. J. Environ. Res. Public Health 2020, 17, 4164. [Google Scholar] [CrossRef] [PubMed]
- Cai, W.; Ivory, D.; Smith, M.; Lemonides, A.; Higgins, L. More Than 6600 Coronavirus Cases Have Been Linked to U.S. Colleges. Available online: https://web.archive.org/web/20200808053047/https://www.nytimes.com/interactive/2020/07/28/us/covid-19-colleges-universities.html (accessed on 1 August 2020).
- Schricker, J.; Rathmann, K.; Dadaczynski, K. Soziale Unterschiede in der Gesundheitskompetenz von Studierenden: Ergebnisse einer Online-Studie an der Technischen Universität Dortmund. Prävent. Gesundheitsförderung 2020, 15, 8–14. [Google Scholar] [CrossRef]
- Rababah, J.A.; Al-Hammouri, M.M.; Drew, B.L.; Aldalaykeh, M. Health literacy: Exploring disparities among college students. BMC Public Health 2019, 19, 1401. [Google Scholar] [CrossRef] [PubMed]
- Freeman, J.L.; Caldwell, P.H.Y.; Bennett, P.A.; Scott, K.M. How Adolescents Search for and Appraise Online Health Information: A Systematic Review. J. Pediatr. 2018, 195, 244–255.e1. [Google Scholar] [CrossRef]
- McKinnon, K.A.; Caldwell, P.H.Y.; Scott, K.M. How adolescent patients search for and appraise online health information: A pilot study. J. Paediatr. Child Health 2020, 56, 1270–1276. [Google Scholar] [CrossRef]
- Rosário, R.; Martins, M.R.O.; Augusto, C.; Silva, M.J.; Martins, S.; Duarte, A.; Fronteira, I.; Ramos, N.; Okan, O.; Dadaczynski, K. Associations between COVID-19-Related Digital Health Literacy and Online Information-Seeking Behavior among Portuguese University Students. Int. J. Environ. Res. Public Health 2020, 17, 8987. [Google Scholar] [CrossRef] [PubMed]
- Lennon, R.P.; Sakya, S.M.; Miller, E.L.; Snyder, B.; Yaman, T.; Zgierska, A.E.; Ruffin, M.T.; Van Scoy, L.J. Public Intent to Comply with COVID-19 Public Health Recommendations. HLRP Health Lit. Res. Pract. 2020, 4, e161–e165. [Google Scholar] [CrossRef]
- Lee, S.-Y.D.; Arozullah, A.M.; Cho, Y.I. Health literacy, social support, and health: A research agenda. Soc. Sci. Med. 2004, 58, 1309–1321. [Google Scholar] [CrossRef]
- Sentell, T.; Foss-Durant, A.; Patil, U.; Taira, D.; Paasche-Orlow, M.K.; Trinacty, C.M. Organizational Health Literacy: Opportunities for Patient-Centered Care in the Wake of COVID-19. Qual. Manag. Healthc. 2021, 30, 49–60. [Google Scholar] [CrossRef]
- Qualtrics. Qualtrics for Education. Available online: https://www.qualtrics.com/education/ (accessed on 14 August 2020).
- Espinosa, L.L.; Turk, J.M.; Taylor, M.; Chessman, H.M. Race and Ethnicity in Higher Education: A Status Report; American Council on Education: Washington, DC, USA, 2019; p. 34. [Google Scholar]
- The Atlantic Monthly Group. US Historical Data. Available online: https://covidtracking.com/data/national (accessed on 19 September 2020).
- Haeder, S.F.; Gollust, S.E. From Poor to Worse: Health Policy and Politics Scholars’ Assessment of the U.S. COVID-19 Response and Its Implications. World Med. Health Policy 2020, 12, 454–481. [Google Scholar] [CrossRef]
- Morris, N.S.; MacLean, C.D.; Chew, L.D.; Littenberg, B. The Single Item Literacy Screener: Evaluation of a brief instrument to identify limited reading ability. BMC Fam. Pract. 2006, 7, 21. [Google Scholar] [CrossRef] [PubMed]
- Chew, L.D.; Bradley, K.A.; Boyko, E.J. Brief questions to identify patients with inadequate health literacy. Fam. Med. 2004, 36, 588–594. [Google Scholar] [PubMed]
- Brice, J.H.; Foster, M.B.; Principe, S.; Moss, C.; Shofer, F.S.; Falk, R.J.; Ferris, M.E.; DeWalt, D.A. Single-item or two-item literacy screener to predict the S-TOFHLA among adult hemodialysis patients. Patient Educ. Couns. 2014, 94, 71–75. [Google Scholar] [CrossRef]
- Caplan, L.; Wolfe, F.; Michaud, K.; Quinzanos, I.; Hirsh, J.M. Strong Association of Health Literacy With Functional Status Among Rheumatoid Arthritis Patients: A Cross-Sectional Study. Arthritis Care Res. 2014, 66, 508–514. [Google Scholar] [CrossRef]
- Neter, E.; Brainin, E.; Baron-Epel, O. The dimensionality of health literacy and eHealth literacy. Eur. Health Psychol. 2015, 17, 275–280. [Google Scholar]
- Chou, W.-Y.S.; Oh, A.; Klein, W.M.P. Addressing Health-Related Misinformation on Social Media. JAMA 2018, 320, 2417–2418. [Google Scholar] [CrossRef]
- Van der Vaart, R.; van Deursen, A.J.; Drossaert, C.H.; Taal, E.; van Dijk, J.A.; van de Laar, M.A. Does the eHealth Literacy Scale (eHEALS) measure what it intends to measure? Validation of a Dutch version of the eHEALS in two adult populations. J. Med. Internet Res. 2011, 13, e86. [Google Scholar] [CrossRef] [PubMed]
- Sentell, T.; Agner, J.; Pitt, R.; Davis, J.; Guo, M.; McFarlane, E. Considering Health Literacy, Health Decision Making, and Health Communication in the Social Networks of Vulnerable New Mothers in Hawai‘i: A Pilot Feasibility Study. Int. J. Environ. Res. Public Health 2020, 17, 2356. [Google Scholar] [CrossRef]
- Sentell, T.; Agner, J.; Davis, J.; Mannem, S.; Seto, T.; Valente, T.; Vawer, M.; Taira, D. Social Networks in Patients Hospitalized with Preventable Conditions for Heart Disease and Diabetes in Hawai‘i by Health Literacy. Chronic Illn. 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Sentell, T.; Kennedy, F.; Seto, T.; Vawer, M.; Chiriboga, G.; Valdez, C.; Garrett, L.M.; Paloma, D.; Taira, D. Sharing the Patient Experience: A “Talk Story” Intervention for Heart Failure Management in Native Hawaiians. J. Patient Exp. 2020, 7, 399–407. [Google Scholar] [CrossRef]
- Maddock, J.E.; Moore, J.B. Should Public Health Literacy Be a Core Requirement for College Students? J. Public Health Manag. Pract. 2020, 26, 304–305. [Google Scholar] [CrossRef] [PubMed]
- Division of Population Health, National Center for Chronic Disease Prevention and Health Promotion National Health Education Standards. Available online: https://www.cdc.gov/healthyschools/sher/standards/index.htm (accessed on 21 December 2020).
- Zhu, C.; Xu, X.; Zhang, W.; Chen, J.; Evans, R. How Health Communication via Tik Tok Makes a Difference: A Content Analysis of Tik Tok Accounts Run by Chinese Provincial Health Committees. Int. J. Environ. Res. Public Health 2020, 17, 192. [Google Scholar] [CrossRef]
- Stellefson, M.; Paige, S.R.; Chaney, B.H.; Chaney, J.D. Social Media and Health Promotion. Int. J. Environ. Res. Public Health 2020, 17, 3323. [Google Scholar] [CrossRef]
- Papageorge, N.; Zahn, M.; Belot, M.; van den Broek-Altenburg, E.; Choi, S.; Jamison, J.; Tripodi, E. Socio-Demographic Factors Associated with Self-Protecting Behavior during the COVID-19 Pandemic; National Bureau of Economic Research: Cambridge, MA, USA, 2020; p. 52. [Google Scholar]
- Duplaga, M.; Sobecka, K.; Wójcik, S. The reliability and validity of the telephone-based and online polish ehealth literacy scale based on two nationally representative samples. Int. J. Environ. Res. Public Health 2019, 16, 3216. [Google Scholar] [CrossRef]
- Norman, C.D.; Skinner, H.A. eHEALS: The eHealth Literacy Scale. J. Med. Internet Res. 2006, 8, e27. [Google Scholar] [CrossRef]
- Pelikan, J.M.; Röthlin, F.; Ganahl, K. Measuring comprehensive health literacy in general populations: Validation of instrument, indices and scales of the HLS-EU study. In Proceedings of the 6th Annual Health Literacy Research Conference, Bethesda, MD, USA, 3–4 November 2014. [Google Scholar]
| Title | N | % |
|---|---|---|
| Gender | ||
| Female | 108 | 42% |
| Male | 140 | 55% |
| Other Identity | 8 | 3% |
| Ethnicity and Race | ||
| Non-Hispanic Black | 37 | 14% |
| Non-Hispanic Asian | 24 | 9% |
| Non-Hispanic White | 91 | 36% |
| Non-Hispanic Other | 6 | 2% |
| Hispanic | 98 | 38% |
| Political Affiliation | ||
| Republican | 71 | 28% |
| Democrat | 132 | 52% |
| Independent | 53 | 21% |
| Disability | 49 | 19% |
| First-Generation Student | 146 | 57% |
| Searched Internet for COVID-19 Information | ||
| Yes, for me | 92 | 36% |
| Yes, for others | 48 | 19% |
| Yes, for me and others | 106 | 41% |
| No | 10 | 4% |
| Health Literacy | ||
| Low | 130 | 51% |
| Adequate | 126 | 49% |
| M | SD | |
| Age | 23.9 | 4.3 |
| Semesters Enrolled | 4.7 | 3.7 |
| Health Discussion Partners | ||
| Own Health | 4.3 | 5.0 |
| Their Health | 4.5 | 5.8 |
| COVID-19 Digital Health Literacy (N = 246) | 2.99 | 0.51 |
| Search Information Subscale | 3.08 | 0.57 |
| Determine Reliability Subscale | 2.83 | 0.62 |
| Establish Relevance Subscale | 3.06 | 0.61 |
| Title | Total | Health Literacy (N = 256) | COVID-19 Digital Health Literacy (N = 246) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low | Adequate | Test | Test | |||||||||
| N | % | N | % | N | % | χ2 | P | SD | F | P | ||
| Total | 256 | 130 | 126 | ns | 2.99 | 0.51 | ||||||
| Pandemic Perception | 9.55 | 0.008 | 0.08 | 0.92 | ||||||||
| Overreaction | 73 | 29% | 41 | 32% | 32 | 25% | 3.01 | 0.53 | ||||
| Fair Reaction | 123 | 48% | 69 | 53% | 54 | 43% | 2.99 | 0.46 | ||||
| Underreaction | 60 | 23% | 20 | 15% | 40 | 32% | 2.98 | 0.59 | ||||
| Vaccination Likeliness | 0.55 | 0.46 | 5.39 | 0.02 | ||||||||
| Very Likely | 124 | 48% | 60 | 46% | 64 | 51% | 3.07 | 0.54 | ||||
| Somewhat/Not Likely | 132 | 52% | 70 | 54% | 62 | 49% | 2.92 | 0.47 | ||||
| Compliance | ||||||||||||
| Hand Washing | 9.76 | 0.002 | 17.08 | <0.001 | ||||||||
| Yes | 127 | 50% | 52 | 40% | 75 | 60% | 3.12 | 0.50 | ||||
| No | 129 | 50% | 78 | 60% | 51 | 41% | 2.86 | 0.49 | ||||
| Social Distancing | 2.60 | 0.11 | 8.71 | 0.003 | ||||||||
| Yes | 119 | 46% | 54 | 42% | 65 | 52% | 3.09 | 0.54 | ||||
| No | 137 | 54% | 76 | 58% | 61 | 48% | 2.90 | 0.46 | ||||
| Mask-Wearing | 12.12 | <0.001 | 9.53 | 0.002 | ||||||||
| Yes | 166 | 65% | 71 | 55% | 95 | 75% | 3.06 | 0.50 | ||||
| No | 90 | 35% | 59 | 45% | 31 | 25% | 2.86 | 0.50 | ||||
| Staying at Home | 2.59 | 0.11 | 10.33 | 0.001 | ||||||||
| Yes | 99 | 39% | 44 | 34% | 55 | 44% | 3.12 | 0.50 | ||||
| No | 157 | 61% | 86 | 66% | 71 | 56% | 2.91 | 0.50 | ||||
| Full Compliance | 6.94 | 0.008 | 17.50 | <0.001 | ||||||||
| Yes | 61 | 24% | 22 | 17% | 39 | 31% | 3.22 | 0.48 | ||||
| No | 195 | 76% | 108 | 83% | 87 | 69% | 2.92 | 0.50 | ||||
| Chance of Getting COVID-19 | 1.51 | 0.22 | 4.31 | 0.04 | ||||||||
| No or Low Chance | 110 | 43% | 51 | 39% | 59 | 47% | 3.07 | 0.53 | ||||
| Medium or High Chance | 146 | 57% | 79 | 61% | 67 | 53% | 2.93 | 0.48 | ||||
| COVID-19 Would Impact Life | 0.38 | 0.83 | 6.37 | 0.002 | ||||||||
| Not a big deal | 17 | 7% | 9 | 7% | 8 | 6% | 2.90 | 0.51 | ||||
| Make me a little sick | 121 | 47% | 59 | 45% | 62 | 49% | 2.88 | 0.50 | ||||
| Make me very sick | 118 | 46% | 62 | 48% | 56 | 44% | 3.11 | 0.49 | ||||
| Title | Pandemic Perception: Underreaction | Compliance with All Four Guidances | Very Likely to Vaccinate | Very Likely to Impact Life | High Chance of Getting COVID-19 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Low Health Literacy | 0.51 * | 0.24–1.04 | 0.046 ** | 0.23–0.92 | 0.88 | 0.50–1.56 | 1.07 | 0.61–1.89 | 1.47 | 0.84–2.60 |
| COVID-19 Digital Health Literacy | 0.80 | 0.37–1.71 | 4.96 ** | 2.39–10.26 | 1.82 ** | 1.04–3.19 | 2.61 ** | 1.48–4.60 | 0.58 ** | 0.33–0.99 |
| Gender | ||||||||||
| Male (vs. Female) | 0.73 | 0.35–1.54 | 0.74 | 0.35–1.53 | 1.21 | 0.66–2.22 | 1.45 | 0.79–2.66 | 1.08 | 0.59–1.98 |
| Other Gender | 5.09 | 0.73–35.38 | 6.11 | 0.67–55.45 | ||||||
| Race/Ethnicity | ||||||||||
| Hispanic | 1.13 | 0.47–2.68 | 1.27 | 0.58–2.79 | 0.77 | 0.40–1.48 | 1.00 | 0.52–1.92 | 1.08 | 0.56–2.07 |
| Non-Hispanic Asian | 2.81 * | 0.94–8.36 | 1.21 | 0.36–4.03 | 2.02 | 0.73–5.59 | 1.01 | 0.37–2.72 | 0.64 | 0.24–1.72 |
| Non-Hispanic Black | 0.40 | 0.11–1.49 | 0.91 | 0.30–2.82 | 0.41 * | 0.16–1.05 | 1.31 | 0.54–3.20 | 1.21 | 0.49–2.96 |
| Non-Hispanic Other | 1.74 | 0.23–12.70 | 10.66 | 1.36–83.92 | 1.82 | 0.26–12.59 | 2.64 | 0.39–17.87 | 3.13 | 0.32–30.54 |
| Non-Hispanic White | ||||||||||
| First-Generation Student (vs. not) | 0.74 | 0.37–1.51 | 0.69 | 0.36–1.33 | 0.77 | 0.44–1.34 | 1.26 | 0.73–2.19 | 0.74 | 0.43–1.29 |
| Disability (vs. no) | 0.80 | 0.29–2.23 | 1.21 | 0.49–2.98 | 0.88 | 0.43–1.79 | 1.12 | 0.55–2.27 | 1.13 | 0.59–2.31 |
| Political Affiliation | ||||||||||
| Republican | 0.26 ** | 0.09–0.69 | 0.89 | 0.40–1.98 | 1.07 | 0.56–2.06 | 0.69 | 0.36–1.33 | 0.77 | 0.41–1.45 |
| Independent | 0.65 | 0.26–1.59 | 1.15 | 0.49–2.68 | 0.91 | 0.44–1.85 | 1.04 | 0.51–2.13 | 1.44 | 0.70–2.97 |
| Democrat | ||||||||||
| Social Network Size | 1.04 | 0.37–1.50 | 1.02 | 0.96–1.09 | 0.99 | 0.92–1.06 | 0.97 | 0.92–1.03 | 1.01 | 0.95–1.08 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patil, U.; Kostareva, U.; Hadley, M.; Manganello, J.A.; Okan, O.; Dadaczynski, K.; Massey, P.M.; Agner, J.; Sentell, T. Health Literacy, Digital Health Literacy, and COVID-19 Pandemic Attitudes and Behaviors in U.S. College Students: Implications for Interventions. Int. J. Environ. Res. Public Health 2021, 18, 3301. https://doi.org/10.3390/ijerph18063301
Patil U, Kostareva U, Hadley M, Manganello JA, Okan O, Dadaczynski K, Massey PM, Agner J, Sentell T. Health Literacy, Digital Health Literacy, and COVID-19 Pandemic Attitudes and Behaviors in U.S. College Students: Implications for Interventions. International Journal of Environmental Research and Public Health. 2021; 18(6):3301. https://doi.org/10.3390/ijerph18063301
Chicago/Turabian StylePatil, Uday, Uliana Kostareva, Molly Hadley, Jennifer A. Manganello, Orkan Okan, Kevin Dadaczynski, Philip M. Massey, Joy Agner, and Tetine Sentell. 2021. "Health Literacy, Digital Health Literacy, and COVID-19 Pandemic Attitudes and Behaviors in U.S. College Students: Implications for Interventions" International Journal of Environmental Research and Public Health 18, no. 6: 3301. https://doi.org/10.3390/ijerph18063301
APA StylePatil, U., Kostareva, U., Hadley, M., Manganello, J. A., Okan, O., Dadaczynski, K., Massey, P. M., Agner, J., & Sentell, T. (2021). Health Literacy, Digital Health Literacy, and COVID-19 Pandemic Attitudes and Behaviors in U.S. College Students: Implications for Interventions. International Journal of Environmental Research and Public Health, 18(6), 3301. https://doi.org/10.3390/ijerph18063301







