Association between Kinesiophobia and Gait Asymmetry after ACL Reconstruction: Implications for Prevention of Reinjury
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Procedure
2.3. Data Analysis and Reduction
2.4. Statistical Analysis
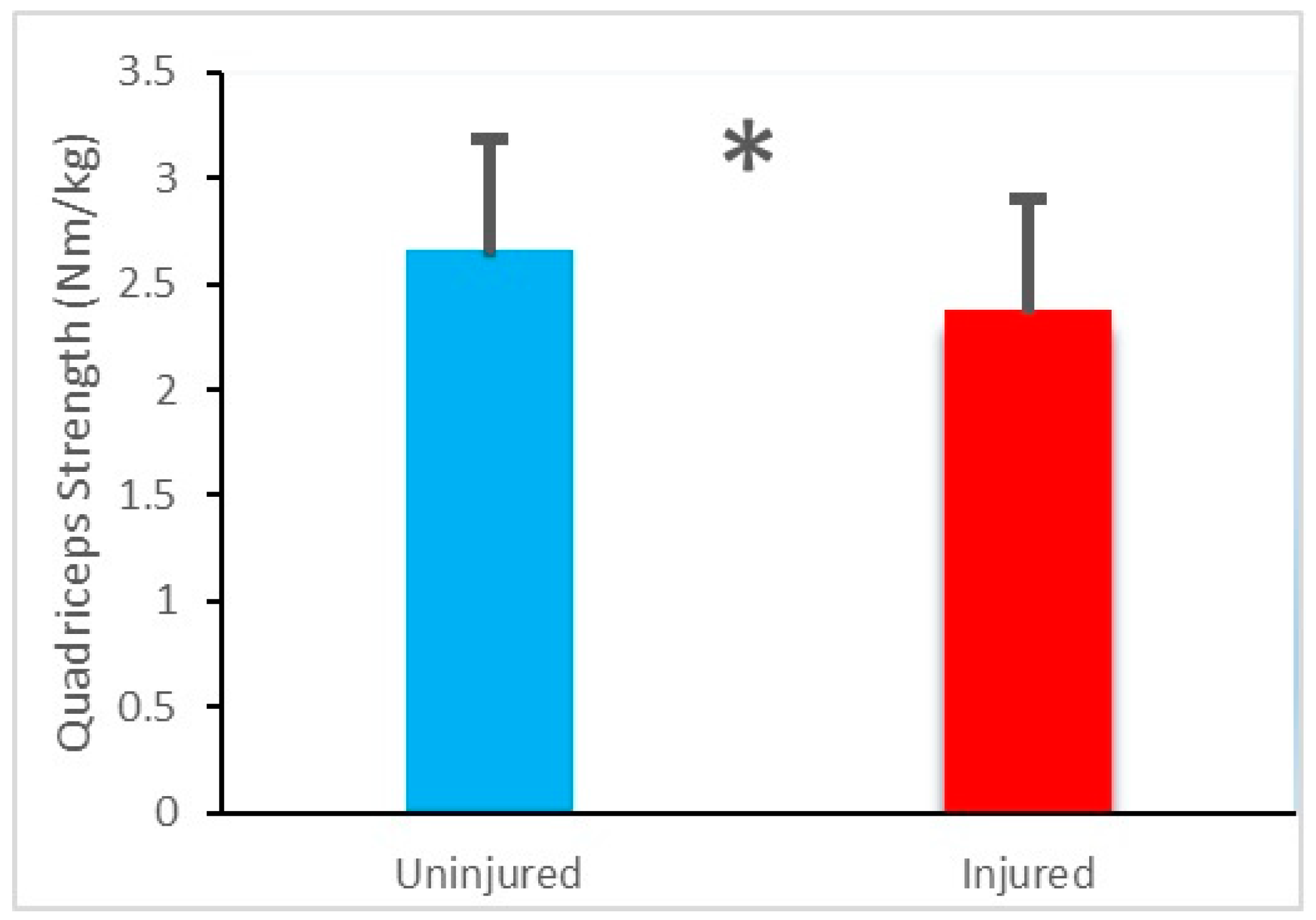
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wiggins, A.J.; Grandhi, R.K.; Schneider, D.K.; Stanfield, D.; Webster, K.E.; Myer, G.D. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Am. J. Sports Med. 2016, 44, 1861–1876. [Google Scholar] [CrossRef]
- Oiestad, B.E.; Holm, I.; Aune, A.K.; Gunderson, R.; Myklebust, G.; Engebretsen, L.; Fosdahl, M.A.; Risberg, M.A. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: A prospective study with 10 to 15 years of follow-up. Am. J. Sports Med. 2010, 38, 2201–2210. [Google Scholar] [CrossRef] [PubMed]
- Di Stasi, S.L.; Logerstedt, D.; Gardinier, E.S.; Snyder-Mackler, L. Gait patterns differ between ACL-reconstructed athletes who pass return-to-sport criteria and those who fail. Am. J. Sports Med. 2013, 41, 1310–1318. [Google Scholar] [CrossRef] [PubMed]
- Mantashloo, Z.; Letafatkar, A.; Moradi, M. Vertical ground reaction force and knee muscle activation asymmetries in patients with ACL reconstruction compared to healthy individuals. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 2009–2014. [Google Scholar] [CrossRef]
- Capin, J.J.; Zarzycki, R.; Arundale, A.; Cummer, K.; Snyder-Mackler, L. Report of the primary outcomes for gait mechanics in men of the ACL-SPORTS trial: Secondary prevention with and without perturbation training does not restore gait symmetry in men 1 or 2 years after ACL reconstruction. Clin. Orthop. Relat. Res. 2017, 475, 2513–2522. [Google Scholar] [CrossRef] [PubMed]
- Paterno, M.V.; Schmitt, L.C.; Ford, K.R.; Rauh, M.J.; Myer, G.D.; Huang, B.; Hewett, T.E. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am. J. Sports Med. 2010, 38, 1968–1978. [Google Scholar] [CrossRef]
- Butler, R.; Minick, K.; Ferber, R.; Underwood, F. Gait mechanics after ACL reconstruction: Implications for the early onset of knee osteoarthritis. Br. J. Sports Med. 2009, 43, 366–370. [Google Scholar] [CrossRef] [PubMed]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Heidt, R.S., Jr.; Colosimo, A.J.; McLean, S.G.; van den Bogert, A.J.; Paterno, M.V.; Succop, P. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am. J. Sports Med. 2005, 33, 492–501. [Google Scholar] [CrossRef]
- Barber-Westin, S.D.; Noyes, F.R. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthrosc. J. Arthrosc. Relat. Surg. 2011, 27, 1697–1705. [Google Scholar] [CrossRef] [PubMed]
- Carter, D.R.; Beaupré, G.S.; Wong, M.; Smith, R.L.; Andriacchi, T.P.; Schurman, D.J. The mechanobiology of articular cartilage development and degeneration. Clin. Orthop. Relat. Res. 2004, 427, 69–77. [Google Scholar] [CrossRef]
- Chmielewski, T.L. Asymmetrical lower extremity loading after ACL reconstruction: More than meets the eye. J. Orthop. Sports Phys. Ther. 2011, 41, 374–376. [Google Scholar] [CrossRef]
- Theologis, A.A.; Haughom, B.; Liang, F.; Zhang, Y.; Majumdar, S.; Link, T.M.; Ma, C.B.; Li, X. Comparison of T1rho relaxation times between ACL-reconstructed knees and contralateral uninjured knees. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 298–307. [Google Scholar] [CrossRef] [PubMed]
- Luc, B.; Gribble, P.A.; Pietrosimone, B.G. Osteoarthritis prevalence following anterior cruciate ligament reconstruction: A systematic review and numbers-needed-to-treat analysis. J. Athl. Train. 2014, 49, 806–819. [Google Scholar] [CrossRef] [PubMed]
- Wellsandt, E.; Gardinier, E.S.; Manal, K.; Axe, M.J.; Buchanan, T.S.; Snyder-Mackler, L. Decreased knee joint loading associated with early knee osteoarthritis after anterior cruciate ligament injury. Am. J. Sports Med. 2016, 44, 143–151. [Google Scholar] [CrossRef]
- Gokeler, A.; Bisschop, M.; Benjaminse, A.; Myer, G.D.; Eppinga, P.; Otten, E. Quadriceps function following ACL reconstruction and rehabilitation: Implications for optimisation of current practices. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1163–1174. [Google Scholar] [CrossRef]
- Palmieri-Smith, R.M.; Thomas, A.C.; Wojtys, E.M. Maximizing quadriceps strength after ACL reconstruction. Clin. Sports Med. 2008, 27, 405–424. [Google Scholar] [CrossRef]
- Lewek, M.; Rudolph, K.; Axe, M.; Snyder-Mackler, L. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin. Biomech. Bristol Avon 2002, 17, 56–63. [Google Scholar] [CrossRef]
- Snyder-Mackler, L.; Delitto, A.; Bailey, S.L.; Stralka, S.W. Strength of the quadriceps femoris muscle and functional recovery after reconstruction of the anterior cruciate ligament. A prospective, randomized clinical trial of electrical stimulation. J. Bone Jt. Surg. Am. 1995, 77, 1166–1173. [Google Scholar] [CrossRef]
- Roewer, B.D.; Di Stasi, S.L.; Snyder-Mackler, L. Quadriceps strength and weight acceptance strategies continue to improve two years after anterior cruciate ligament reconstruction. J. Biomech. 2011, 44, 1948–1953. [Google Scholar] [CrossRef]
- Zarzycki, R.; Failla, M.; Capin, J.J.; Snyder-Mackler, L. Psychological readiness to return to sport is associated with knee kinematic asymmetry during gait following anterior cruciate ligament reconstruction. J. Orthop. Sports Phys. Ther. 2018, 48, 968–973. [Google Scholar] [CrossRef]
- Chmielewski, T.L.; Jones, D.; Day, T.; Tillman, S.M.; Lentz, T.A.; George, S.Z. The association of pain and fear of movement/re-injury with function during anterior cruciate ligament reconstruction rehabilitation. J. Orthop. Sports Phys. Ther. 2008, 38, 746–753. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Whitehead, T.S.; Webster, K.E. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am. J. Sports Med. 2013, 41, 1549–1558. [Google Scholar] [CrossRef] [PubMed]
- Lentz, T.A.; Zeppieri, J.G.; George, S.Z.; Tillman, S.M.; Moser, M.W.; Farmer, K.W.; Chmielewski, T.L. Comparison of physical impairment, functional, and psychosocial measures based on fear of re-injury/lack of confidence and return-to-sport status after ACL reconstruction. Am. J. Sports Med. 2015, 43, 345–353. [Google Scholar] [CrossRef]
- Sonesson, S.; Kvist, J.; Ardern, C.; Österberg, A.; Silbernagel, K.G. Psychological factors are important to return to pre-injury sport activity after anterior cruciate ligament reconstruction: Expect and motivate to satisfy. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1375–1384. [Google Scholar] [CrossRef]
- Trigsted, S.M.; Cook, D.B.; Pickett, K.A.; Cadmus-Bertram, L.; Dunn, W.R.; Bell, D.R. Greater fear of re-injury is related to stiffened jump-landing biomechanics and muscle activation in women after ACL reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3682–3689. [Google Scholar] [CrossRef]
- Palomo-López, P.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; López-López, D.; Rodríguez-Sanz, D.; Romero-Morales, C.; Calvo-Lobo, C.; Mazoteras-Pardo, V. Kinesiophobia and pain intensity are increased by a greater hallux valgus deformity degree—Kinesiophobia and pain intensity in hallux valgus. Int. J. Environ. Res. Public Health 2020, 17, 626. [Google Scholar] [CrossRef]
- Chmielewski, T.L.; Zeppieri, G., Jr.; Lentz, T.A.; Tillman, S.M.; Moser, M.W.; Indelicato, P.A.; George, S.Z. Longitudinal changes in psychosocial factors and their association with knee pain and function after anterior cruciate ligament reconstruction. Phys. Ther. 2011, 91, 1355–1366. [Google Scholar] [CrossRef]
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Webster, K.E. A systematic review of the psychological factors associated with returning to sport following injury. Br. J. Sports Med. 2013, 47, 1120–1126. [Google Scholar] [CrossRef]
- Ardern, C.L. Anterior cruciate ligament reconstruction—Not exactly a one-way ticket back to the preinjury level: A review of contextual factors affecting return to sport after surgery. Sports Health 2015, 7, 224–230. [Google Scholar] [CrossRef]
- Tripp, D.A.; Stanish, W.; Ebel-Lam, A.; Brewer, B.W.; Birchard, J. Fear of reinjury, negative affect, and catastrophizing predicting return to sport in recreational athletes with anterior cruciate ligament injuries at 1 year postsurgery. Rehabil. Psychol. 2007, 52, 74–81. [Google Scholar] [CrossRef]
- Kvist, J.; Ek, A.; Sporrstedt, K.; Good, L. Fear of re-injury: A hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2005, 13, 393–397. [Google Scholar] [CrossRef] [PubMed]
- Paterno, M.V.; Flynn, K.; Thomas, S.; Schmitt, L.C. Self-reported fear predicts functional performance and second ACL injury after ACL reconstruction and return to sport: A pilot study. Sports Health 2018, 10, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Osterberg, A.; Tagesson, S.; Gauffin, H.; Webster, K.E.; Kvist, J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br. J. Sports Med. 2014, 48, 1613–1619. [Google Scholar] [CrossRef] [PubMed]
- Woby, S.R.; Roach, N.K.; Urmston, M.; Watson, P.J. Psychometric properties of the TSK-11: A shortened version of the Tampa Scale for Kinesiophobia. Pain 2005, 117, 137–144. [Google Scholar] [CrossRef]
- George, S.Z.; Lentz, T.A.; Zeppieri, G.; Lee, D.; Chmielewski, T.L. Analysis of shortened versions of the Tampa Scale for Kinesiophobia and Pain Catastrophizing Scale for patients following anterior cruciate ligament reconstruction. Clin. J. Pain 2012, 28, 73–80. [Google Scholar] [CrossRef]
- Stegeman, D.; Hermens, H. Standards for surface electromyography. In The European project Surface EMG for non-invasive assessment of muscles (SENIAM); Roessingh Research and Development: Enschede, The Netherlands, 2007; pp. 108–112. [Google Scholar]
- Robinson, R.; Herzog, W.; Nigg, B.M. Use of force platform variables to quantify the effects of chiropractic manipulation on gait symmetry. J. Manipulative Physiol. Ther. 1987, 10, 172–176. Available online: https://pubmed.ncbi.nlm.nih.gov/2958572 (accessed on 10 February 2021).
- Hopkins, J.T.; Ingersoll, C.D.; Cordova, M.L.; Edwards, J.E. Intrasession and intersession reliability of the soleus H-reflex in supine and standing positions. Electromyogr. Clin. Neurophysiol. 2000, 40, 89–94. Available online: https://pubmed.ncbi.nlm.nih.gov/10746184 (accessed on 10 February 2021).
- Bowersock, C.D.; Willy, R.W.; DeVita, P.; Willson, J.D. Reduced step length reduces knee joint contact forces during running following anterior cruciate ligament reconstruction but does not alter inter-limb asymmetry. Clin. Biomech. Bristol Avon 2017, 43, 79–85. [Google Scholar] [CrossRef]
- Mazet, A.; Morin, J.B.; Semay, B.; Philippot, R.; Edouard, P. Changes in running mechanical pattern after an anterior cruciate ligament plasty. Sci. Sports 2016, 31, 219–222. [Google Scholar] [CrossRef]
- Pamukoff, D.N.; Montgomery, M.M.; Choe, K.H.; Moffit, T.J.; Garcia, S.A.; Vakula, M.N. Bilateral alterations in running mechanics and quadriceps function following unilateral anterior cruciate ligament reconstruction. J. Orthop. Sports Phys. Ther. 2018, 48, 960–967. [Google Scholar] [CrossRef]
- Milandri, G.; Posthumus, M.; Small, T.; Bothma, A.; Merwe, W.V.D.; Kassanjee, R.; Sivarasu, S. Kinematic and kinetic gait deviations in males long after anterior cruciate ligament reconstruction. Clin. Biomech. Bristol Avon 2017, 49, 78–84. [Google Scholar] [CrossRef]
- Sanford, B.A.; Zucker-Levin, A.R.; Williams, J.L.; Mihalko, W.M.; Jacobs, E.L. Principal component analysis of knee kinematics and kinetics after anterior cruciate ligament reconstruction. Gait. Posture 2012, 36, 609–613. [Google Scholar] [CrossRef]
- Gao, B.; Zheng, N.N. Alterations in three-dimensional joint kinematics of anterior cruciate ligament-deficient and-reconstructed knees during walking. Clin. Biomech. Bristol Avon 2010, 25, 222–229. [Google Scholar] [CrossRef]
- Hart, J.M.; Ko, J.W.K.; Konold, T.; Pietrosimione, B. Sagittal plane knee joint moments following anterior cruciate ligament injury and reconstruction: A systematic review. Clin. Biomech. Bristol Avon 2010, 25, 277–283. [Google Scholar] [CrossRef]
- Paterno, M.V.; Ford, K.R.; Myer, G.D.; Heyl, R.; Hewett, T.E. Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin. J. Sport Med. 2007, 17, 258–262. [Google Scholar] [CrossRef]
- Alkjaer, T.; Simonsen, E.B.; Jorgensen, U.; Dyhre-Poulsen, P. Evaluation of the walking pattern in two types of patients with anterior cruciate ligament deficiency: Copers and non-copers. Eur. J. Appl. Physiol. 2003, 89, 301–308. [Google Scholar] [CrossRef]
- Rudolph, K.S.; Axe, M.J.; Buchanan, T.S.; Scholz, J.P.; Snyder-Mackler, L. Dynamic stability in the anterior cruciate ligament deficient knee. Knee Surg. Sports Traumatol. Arthrosc. 2001, 9, 62–71. [Google Scholar] [CrossRef]
- Hartigan, E.; Axe, M.J.; Snyder-Mackler, L. Perturbation training prior to ACL reconstruction improves gait asymmetries innon-copers. J. Orthop. Res. 2009, 27, 724–729. [Google Scholar] [CrossRef]
- Noehren, B.; Wilson, H.; Miller, C.; Lattermann, C. Long term gait deviations in anterior cruciate ligament reconstructed females. Med. Sci. Sports Exerc. 2013, 45, 1340–1347. [Google Scholar] [CrossRef]
- Baumgart, C.; Schubert, M.; Hoppe, M.W.; Gokeler, A.; Freiwald, J. Do ground reaction forces during unilateral and bilateral movements exhibit compensation strategies following ACL reconstruction? Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1385–1394. [Google Scholar] [CrossRef]
- Dai, B.; Butler, R.J.; Garrett, W.E.; Queen, R.M. Anterior cruciate ligament reconstruction in adolescent patients: Limb asymmetry and functional knee bracing. Am. J. Sports Med. 2012, 40, 2756–2763. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Nagao, M.; Arita, H.; Shiozawa, J.; Nishio, H.; Kobayashi, Y.; Kaneko, H.; Nagayama, M.; Saita, Y.; Ishijima, M.; et al. Reproducibility, responsiveness and validation of the Tampa Scale for Kinesiophobia in patients with ACL injuries. Health Qual. Life Outcomes 2019, 17, 1–8. [Google Scholar] [CrossRef] [PubMed]
- McCullough, K.A.; Phelps, K.D.; Spindler, K.P.; Matava, M.J.; Dunn, W.R.; Parker, R.D.; Reinke, E.K.; MOON Group. Return to high school-and college-level football after anterior cruciate ligament reconstruction: A multicenter orthopaedic outcomes network (MOON) cohort study. Am. J. Sports Med. 2012, 40, 2523–2529. [Google Scholar] [CrossRef] [PubMed]
- Vlaeyen, J.W.; Linton, S.J. Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain 2000, 85, 317–332. [Google Scholar] [CrossRef]
- Langford, J.L.; Webster, K.E.; Feller, J.A. A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. Br. J. Sports Med. 2009, 43, 377–381. [Google Scholar] [CrossRef]
- Olmedilla, A.; Rubio, V.J.; Ortega, E. Predicting and preventing sport injuries: The role of stress. In Sports Injuries: Prevention, Management and Risk Factors; Hopkins, G., Ed.; Nova Science Publishers: Hauppauge, NY, USA, 2015; pp. 87–104. [Google Scholar]
- Ivarsson, A.; Johnson, U.; Andersen, M.B.; Tranaeus, U.; Stenling, A.; Lindwall, M. Psychosocial factors and sport injuries: Meta-analyses for prediction and prevention. Sports Med. 2017, 47, 353–365. [Google Scholar] [CrossRef]
- Cupal, D.D.; Brewer, B.W. Effects of relaxation and guided imagery on knee strength, reinjury anxiety and pain following anterior cruciate ligament reconstruction. Rehab. Psychol. 2001, 46, 28–43. [Google Scholar] [CrossRef]
| Injured | Uninjured | ||
|---|---|---|---|
| vGRF (%BW) | First peak | 109.94 ± 9.36 | 102.51 ± 8.80 |
| Second peak | 97.63 ± 6.75 | 116.37 ± 10.45 | |
| Muscle activity in contact phase (%MVC) | Medial gastrocnemius | 13.42 ± 3.55 | 12.37 ± 3.18 |
| Rectus femoris | 34.78 ± 6.24 | 27.68 ± 5.02 | |
| Biceps femoris | 26.57 ± 4.27 | 22.24 ± 4.02 | |
| Muscle activity in midstance/propulsion phase (%MVC) | Medial gastrocnemius | 32.27 ± 5.19 | 35.77 ± 6.05 |
| Rectus femoris | 16.21 ± 3.81 | 14.43 ± 3.27 | |
| Biceps femoris | 12.03 ± 3.12 | 10.96 ± 2.69 |
| Asymmetry of vGRF (%) | Mean ± SD | TSK-11 Score | Strength of Relationship | |
|---|---|---|---|---|
| p Value | Correlation Coefficient | |||
| First peak | 6.98 ± 5.45 | 0.153 | 0.200 | Low |
| Second peak | −17.34 ± 7.21 | 0.002 * | 0.531 | High |
| Asymmetry of Muscle Activity (%) | Mean ± SD | TSK-11 Score | Strength of Relationship | ||
|---|---|---|---|---|---|
| p Value | Correlation Coefficient | ||||
| Contact phase | Medial gastrocnemius | 7.81 ± 13.62 | 0.391 | −0.055 | Trivial |
| Rectus femoris | 22.75 ± 4.92 | 0.007 * | 0.460 | Moderate | |
| Biceps femoris | 18.02 ± 8.18 | 0.011 * | 0.429 | Moderate | |
| Midstance/ propulsion phase | Medial gastrocnemius | −10.13 ± 11.76 | 0.212 | 0.157 | Low |
| Rectus femoris | 11.34 ± 5.35 | 0.098 | 0.252 | Low | |
| Biceps femoris | 8.97 ± 7.15 | 0.166 | 0.191 | Low | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tajdini, H.; Letafatkar, A.; Brewer, B.W.; Hosseinzadeh, M. Association between Kinesiophobia and Gait Asymmetry after ACL Reconstruction: Implications for Prevention of Reinjury. Int. J. Environ. Res. Public Health 2021, 18, 3264. https://doi.org/10.3390/ijerph18063264
Tajdini H, Letafatkar A, Brewer BW, Hosseinzadeh M. Association between Kinesiophobia and Gait Asymmetry after ACL Reconstruction: Implications for Prevention of Reinjury. International Journal of Environmental Research and Public Health. 2021; 18(6):3264. https://doi.org/10.3390/ijerph18063264
Chicago/Turabian StyleTajdini, Hossein, Amir Letafatkar, Britton W. Brewer, and Mahdi Hosseinzadeh. 2021. "Association between Kinesiophobia and Gait Asymmetry after ACL Reconstruction: Implications for Prevention of Reinjury" International Journal of Environmental Research and Public Health 18, no. 6: 3264. https://doi.org/10.3390/ijerph18063264
APA StyleTajdini, H., Letafatkar, A., Brewer, B. W., & Hosseinzadeh, M. (2021). Association between Kinesiophobia and Gait Asymmetry after ACL Reconstruction: Implications for Prevention of Reinjury. International Journal of Environmental Research and Public Health, 18(6), 3264. https://doi.org/10.3390/ijerph18063264









