Did Expanded Dental Insurance Reduce Out-of-Pocket Expenditures on Dental Care among Older Adults in Korea? Interrupted Time-Series Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Resource
2.2. Study Population and Main Variable
2.3. Statistical Analysis
2.4. Ethics Approval and Consent to Participate
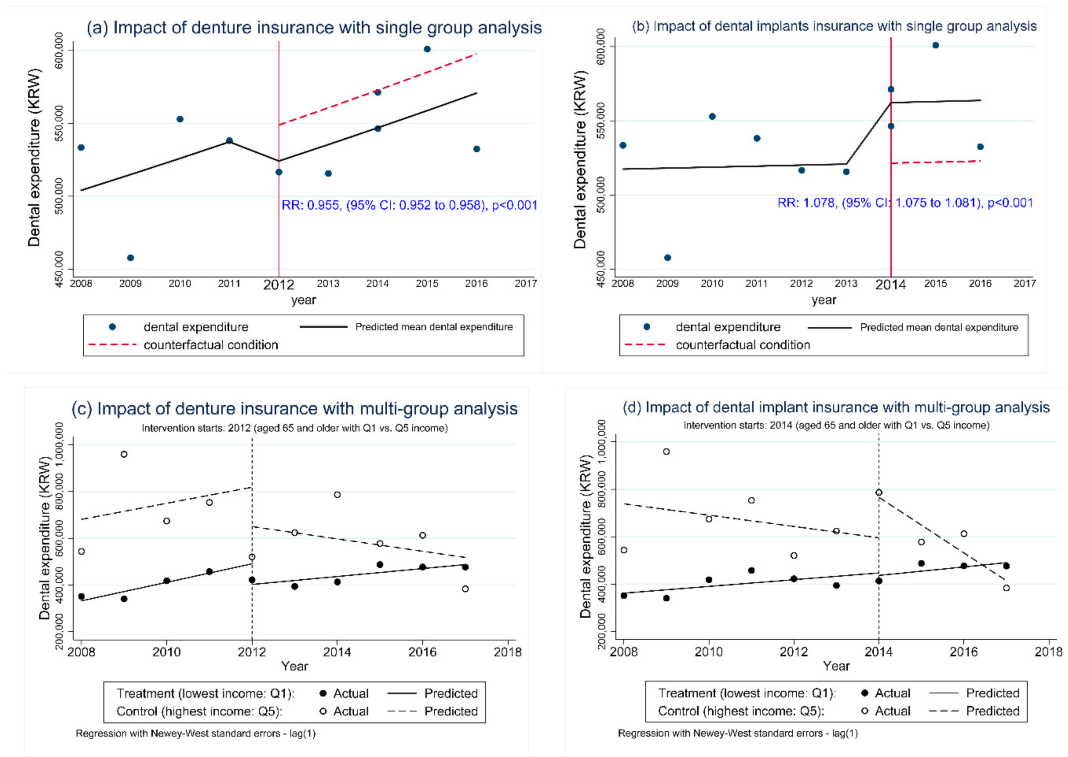
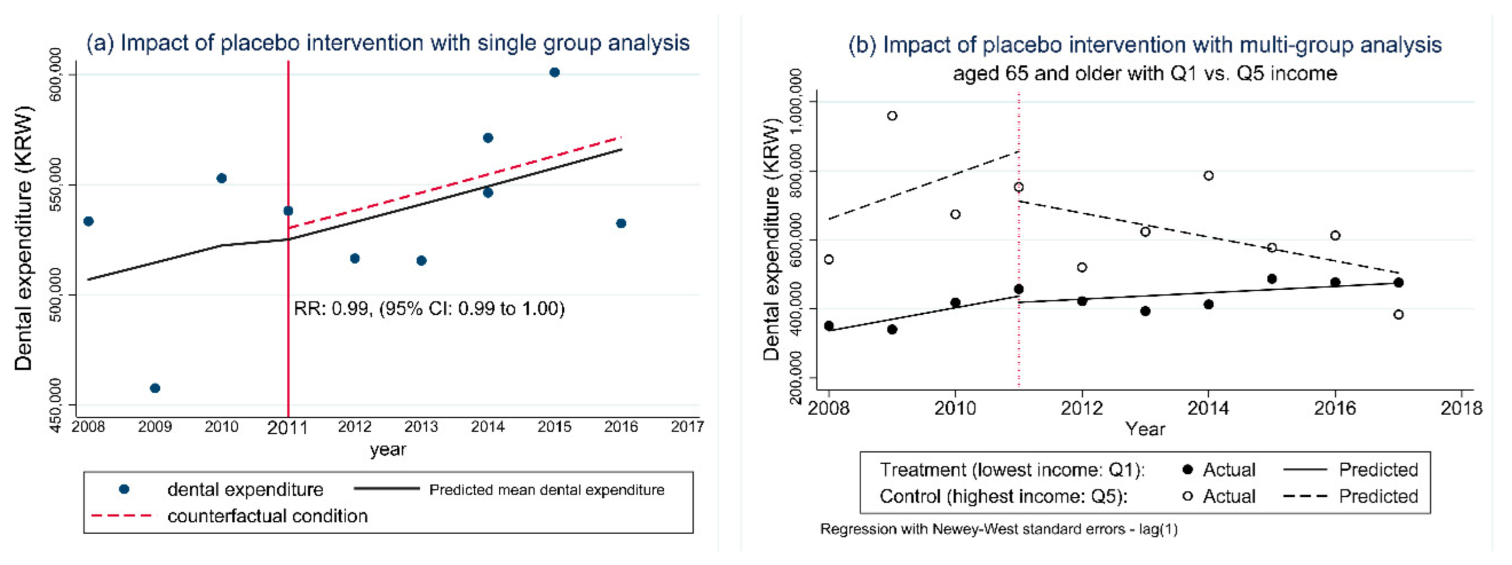
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Masood, M.; Sheiham, A.; Bernabé, E. Household expenditure for dental care in low and middle income countries. PLoS ONE 2015, 10, e0123075. [Google Scholar] [CrossRef] [PubMed]
- Peres, M.A.; Macpherson, L.M.D.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral diseases: A global public health challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef]
- Watt, R.G.; Daly, B.; Allison, P.; Macpherson, L.M.D.; Venturelli, R.; Listl, S.; Weyant, R.J.; Mathur, M.R.; Guarnizo-Herreño, C.C.; Celeste, R.K.; et al. Ending the neglect of global oral health: Time for radical action. Lancet 2019, 394, 261–272. [Google Scholar] [CrossRef]
- Choi, J.S.; Jung, S.H. The impact of expanded national health insurance coverage of dentures and dental implants on dental care utilization among older adults in south korea: A study based on the Korean health panel survey. Int. J. Environ. Res. Public Health 2020, 17, 6417. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.H.; Kawachi, I. Insurance coverage expansion and inequalities in unmet oral healthcare needs in Korea: Repeated cross-sectional analysis, 2007–2015. Community Dent. Oral Epidemiol. 2020. [Google Scholar] [CrossRef] [PubMed]
- KOSIS. Annual Gross Income of the Elderly. Available online: http://kosis.kr/statHtml/statHtml.do?orgId=117&tblId=DT_117071_030&vw_cd= (accessed on 1 December 2020).
- Mori, Y.; Arai, K.; Terauchi, R.; Kanehira, Y.; Uemura, N.; Baba, S.; Kawazoe, T. Analysis of dental treatment expenditures by income group. J. Osaka Dent. Univ. 2014, 48, 159–164. [Google Scholar] [CrossRef]
- Kim, N.-H.; Kawachi, I. Did the expansion of insurance coverage for oral health reduce self-reported oral health inequalities in korea? Results of repeated cross-sectional analysis, 2007–2015. J. Epidemiol. 2019. [Google Scholar] [CrossRef]
- Fuhmei, W.; Jung-Der, W.; Yu-Wen, H. Universal health insurance, health inequality and oral cancer in taiwan. PLoS ONE 2018, 13, e0205731. [Google Scholar] [CrossRef]
- Somkotra, T. Socioeconomic inequality in self-reported oral health status: The experience of thailand after implementation of the universal coverage policy. Community Dent. Health 2011, 28, 136. [Google Scholar] [CrossRef]
- Raittio, E.; Aromaa, A.; Kiiskinen, U.; Helminen, S.; Suominen, A.L. Income-related inequality in perceived oral health among adult finns before and after a major dental subsidization reform. Acta Odontol. Scand. 2016, 74, 348–354. [Google Scholar] [CrossRef]
- Castañeda, H.; Carrion, I.V.; Kline, N.; Tyson, D.M. False hope: Effects of social class and health policy on oral health inequalities for migrant farmworker families. Soc. Sci. Med. 2010, 71, 2028–2037. [Google Scholar] [CrossRef] [PubMed]
- Berkman, L.F.; Kawachi, I.; Glymour, M.M. Social Epidemiology, 2nd ed.; Oxford University Press: New York, NY, USA, 2014. [Google Scholar]
- Phelan, J.C.; Link, B.G.; Tehranifar, P. Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. J. Health Soc. Behav. 2010, 51, S28–S40. [Google Scholar] [CrossRef] [PubMed]
- McCartney, G.; Collins, C.; Mackenzie, M. What (or who) causes health inequalities: Theories, evidence and implications? Health Policy 2013, 113, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Dehmoobadsharifabadi, A.; Singhal, S.; Quinonez, C. Investigating the “inverse care law” in dental care: A comparative analysis of canadian jurisdictions. Can. J. Public Health 2017, 107, e538–e544. [Google Scholar] [CrossRef]
- Manski, R.J.; Goodman, H.S.; Reid, B.C.; Macek, M.D. Dental insurance visits and expenditures among older adults. Am. J. Public Health 2004, 94, 759–764. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Kim, S.; Park, H.K.; Ha, I.-H.; Jung, B.; Ryu, W.-H.; Lee, S.-I.; Sung, N.-J. Effect of having a usual source of care on medical expenses-using the Korea health panel data. J. Korean Med. Sci. 2019, 34, e229. [Google Scholar] [CrossRef]
- Lee, H.J.; Lee, D.W.; Choi, D.-W.; Oh, S.S.; Kwon, J.; Park, E.-C. Association between changes in economic activity and catastrophic health expenditure: Findings from the korea health panel survey, 2014–2016. Cost Eff. Resour. Alloc. 2020, 18, 1–36. [Google Scholar] [CrossRef]
- Kim, N.S. A Report on the Korea Health Panel Survey of 2015 (ii): Chronic Disease, Morbidity, Health Behaviour and Health Status; Korea Institute for Health and Social Affairs: Sejong, Korea, 2017. [Google Scholar]
- Gregori, D.; Petrinco, M.; Bo, S.; Desideri, A.; Merletti, F.; Pagano, E. Regression models for analyzing costs and their determinants in health care: An introductory review. Int. J. Qual. Health Care 2011, 23, 331–341. [Google Scholar] [CrossRef]
- Malehi, A.S.; Pourmotahari, F.; Angali, K.A. Statistical models for the analysis of skewed healthcare cost data: A simulation study. Health Econ. Rev. 2015, 5, 1–16. [Google Scholar] [CrossRef]
- Wagner, A.K.; Soumerai, S.B.; Zhang, F.; Ross-Degnan, D. Segmented regression analysis of interrupted time series studies in medication use research. J. Clin. Pharm. Ther. 2002, 27, 299–309. [Google Scholar] [CrossRef]
- Bernal, J.L.; Cummins, S.; Gasparrini, A. Interrupted time series regression for the evaluation of public health interventions: A tutorial. Int. J. Epidemiol. 2017, 46, 348–355. [Google Scholar] [CrossRef]
- Linden, A. Conducting interrupted time-series analysis for single- and multiple-group comparisons. Stata J. 2015, 15, 480–500. [Google Scholar] [CrossRef]
- Linden, A. Challenges to validity in single-group interrupted time series analysis. J. Eval. Clin. Pract. 2017, 23, 413–418. [Google Scholar] [CrossRef]
- Lopez Bernal, J.; Cummins, S.; Gasparrini, A. Difference in difference, controlled interrupted time series and synthetic controls. Int. J. Epidemiol. 2019, 48, 2062. [Google Scholar] [CrossRef]
- Cohen, L.K.; Gift, H.C. Disease Prevention and Oral Health Promotion: Socio-Dental Sciences in Action; Munksgaard: Copenhagen, Denmark, 1995. [Google Scholar]
- Mangalore, R. Income, health and health care utilization in the UK. Appl. Econ. 2006, 38, 605–617. [Google Scholar] [CrossRef]
- Hye-Won, S.; Young-Sil, K. Changes in dental care utilization and expenditure by the expansion policy of the health insurance coverage: Korea health panel survey 2012–2016. J. Korean Soc. Dent. Hyg. 2020, 20, 611–621. [Google Scholar] [CrossRef]
- Pourat, N.; Choi, M.K.; Chen, X. Evidence of effectiveness of preventive dental care in reducing dental treatment use and related expenditures. J. Public Health Dent. 2018, 78, 203–213. [Google Scholar] [CrossRef]
- Hye Sung, K.; Eun Suk, A.; Min Young, K.; Sun Mi, K.; Ho Sung, S. Trends of household income and dental care spending. J. Korean Acad. Oral Health 2014, 38, 17–24. [Google Scholar] [CrossRef][Green Version]
- Christian, B.; Chattopadhyay, A. Determinants and trends in dental expenditures in the adult us population: Medical expenditure panel survey 1996–2006. Community Dent. Health 2014, 31, 99–104. [Google Scholar]
- Duncan, L.; Bonner, A. Effects of income and dental insurance coverage on need for dental care in Canada. J. Can. Dent. Assoc. 2014, 80, e6. [Google Scholar] [PubMed]
- Thompson, B.; Cooney, P.; Lawrence, H.; Ravaghi, V.; Quiñonez, C. The potential oral health impact of cost barriers to dental care: Findings from a canadian population-based study. BMC Oral Health 2014, 14, 78. [Google Scholar] [CrossRef]
| Aged 65 and Older b | Income Quintile | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lowest Income (1st Quintile) | Highest Income (5th Quintile) | |||||||||||
| Year | n | Mean a | 95% CI c | n | Mean | 95% CI | n | Mean | 95% CI | |||
| Lower | Upper | Lower | Upper | Lower | Upper | |||||||
| 2008 | 2826 | 533,419 | 396,727 | 670,111 | 1159 | 351,243 | 229,066 | 473,420 | 199 | 543,440 | 265,229 | 821,651 |
| 2009 | 2829 | 457,749 | 356,623 | 558,876 | 1112 | 340,571 | 231,185 | 449,957 | 218 | 959,568 | 243,232 | 1,675,905 |
| 2010 | 2876 | 552,945 | 451,359 | 654,531 | 1127 | 418,162 | 259,423 | 576,900 | 232 | 674,084 | 395,857 | 952,311 |
| 2011 | 2967 | 538,179 | 440,376 | 635,982 | 1181 | 457,466 | 299,049 | 615,884 | 201 | 753,351 | 331,709 | 1,174,994 |
| 2012 | 2979 | 516,566 | 440,857 | 592,276 | 1168 | 422,420 | 322,145 | 522,696 | 200 | 520,553 | 291,492 | 749,615 |
| 2013 | 3003 | 515,598 | 444,563 | 586,633 | 1128 | 393,791 | 289,891 | 497,692 | 206 | 623,622 | 405,143 | 842,100 |
| 2014 | 4061 | 546,371 | 454,968 | 637,774 | 1665 | 413,100 | 333,199 | 493,001 | 270 | 786,488 | 52,650 | 1,520,326 |
| 2015 | 4047 | 571,270 | 496,892 | 645,648 | 1704 | 487,369 | 400,756 | 573,981 | 277 | 577,704 | 405,373 | 750,035 |
| 2016 | 4052 | 600,972 | 526,261 | 675,684 | 1620 | 477,076 | 395,055 | 559,097 | 284 | 612,729 | 424,484 | 800,974 |
| 2017 | 4158 | 532,489 | 476,690 | 588,288 | 1650 | 476,449 | 396,838 | 556,060 | 264 | 383,789 | 219,802 | 547,777 |
| Measure of Interest | Model Parameter | 2012 b | 2014 c | ||||
|---|---|---|---|---|---|---|---|
| Point Estimate | p-Value | 95% CI | Point Estimate | p-Value | 95% CI | ||
| Within-group comparison a | |||||||
| Pre-intervention trend: control | β1 | 34,426 | 0.53 | −81,194 to 150,044 | −23,911 | 0.50 | −98,843 to 51,022 |
| Pre-intervention trend: treatment | β5 + β1 | 39,626 | 0.001 | 23,939 to 55,313 | 142,17 | 0.13 | −4684 to 33,117 |
| Difference pre-intervention: treatment versus control | β5 | 5201 | 0.92 | −111,477 to 121,880 | 38,127 | 0.30 | −39,152 to 115,406 |
| Difference immediately following the intervention: treatment versus control | β6 | 80,095 | 0.61 | −249,356 to 409,546 | −181,221 | 0.11 | −412,852 to 50,409 |
| Post-intervention trend: control | β1 + β3 | −26,400 | 0.44 | −98,800 to 46,000 | −117,000 | 0.001 | −155,000 to −79,800 |
| Post-intervention trend: treatment | β1 + β3 + β5 + β7 | 17,000 | 0.001 | 6987 to 27,000 | 18,000 | 0.08 | −2220 to 38,200 |
| Difference post-intervention: treatment versus control | β5 + β7 | 43,400 | 0.22 | −2.9700 to 117,000 | 135,000 | 0.001 | 92,700 to 178,000 |
| Difference pre- versus post-intervention: control | β3 | −60,862 | 0.37 | −202,176 to 80,453 | −93,397 | 0.03 | −177,347 to −9447 |
| Difference pre- versus post-intervention: treatment | β3 + β7 | −22,647 | 0.03 | −42,329 to −2964 | 3759 | 0.81 | −29,035 to 36,552 |
| Difference pre- versus post-intervention: treatment versus control | β7 | 38,215 | 0.57 | −104,464 to 180,893 | 97,155 | 0.04 | 7028 to 187,283 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, N.-H.; Jung, S.-H.; Kawachi, I. Did Expanded Dental Insurance Reduce Out-of-Pocket Expenditures on Dental Care among Older Adults in Korea? Interrupted Time-Series Analysis. Int. J. Environ. Res. Public Health 2021, 18, 3003. https://doi.org/10.3390/ijerph18063003
Kim N-H, Jung S-H, Kawachi I. Did Expanded Dental Insurance Reduce Out-of-Pocket Expenditures on Dental Care among Older Adults in Korea? Interrupted Time-Series Analysis. International Journal of Environmental Research and Public Health. 2021; 18(6):3003. https://doi.org/10.3390/ijerph18063003
Chicago/Turabian StyleKim, Nam-Hee, Se-Hwan Jung, and Ichiro Kawachi. 2021. "Did Expanded Dental Insurance Reduce Out-of-Pocket Expenditures on Dental Care among Older Adults in Korea? Interrupted Time-Series Analysis" International Journal of Environmental Research and Public Health 18, no. 6: 3003. https://doi.org/10.3390/ijerph18063003
APA StyleKim, N.-H., Jung, S.-H., & Kawachi, I. (2021). Did Expanded Dental Insurance Reduce Out-of-Pocket Expenditures on Dental Care among Older Adults in Korea? Interrupted Time-Series Analysis. International Journal of Environmental Research and Public Health, 18(6), 3003. https://doi.org/10.3390/ijerph18063003







