Identifying the Risk Factors Associated with Nursing Home Residents’ Pressure Ulcers Using Machine Learning Methods
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection and Retrieval
2.2. Data Preparation
2.3. Variable Selection
2.4. Data Analysis
2.5. Ethical Considerations
3. Results
3.1. Participating NHs’ Organizational Characteristics
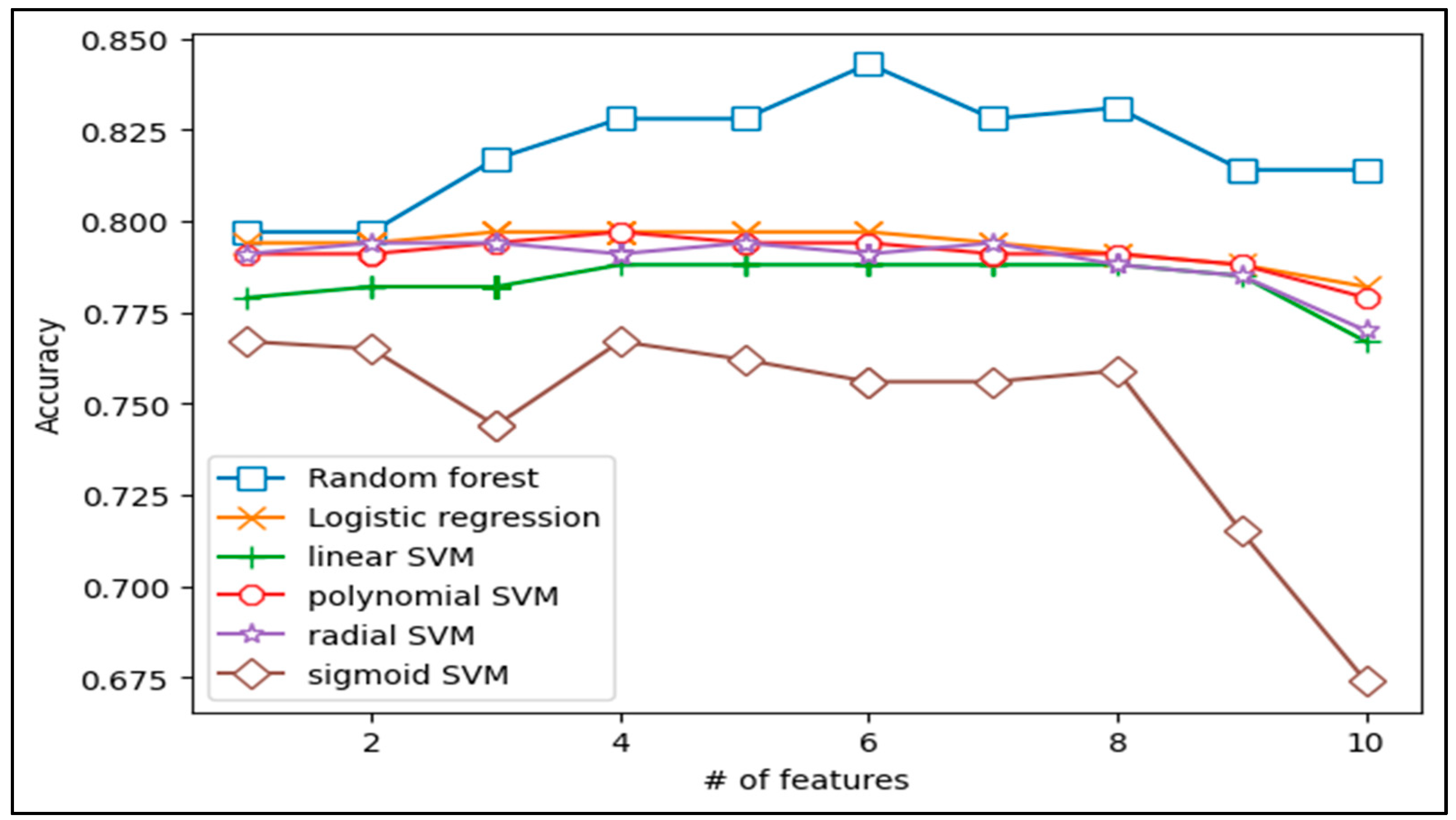
3.2. Predictive Performance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pacific, P. Prevention and Treatment of Pressure Ulcers: Quick Reference Guide. Natl. Press. Ulcer Advis. Panel. 2014, 1–75. [Google Scholar]
- Kojima, G. Prevalence of Frailty in Nursing Homes: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2015, 16, 940–945. [Google Scholar] [CrossRef] [PubMed]
- Haugan, G. Nurse–patient Interaction is a Resource for Hope, Meaning in Life and Self-transcendence in Nursing Home Patients. Scandinavian. Scand. J. Caring Sci. 2014, 28, 74–88. [Google Scholar] [CrossRef] [PubMed]
- Arens, O.B.; Fierz, K.; Zúñiga, F. Elder Abuse in Nursing Homes: Do Special Care Units Make a Difference? A Secondary Data Analysis of the Swiss Nursing Homes Human Resources Project. Gerontology 2017, 63, 169–179. [Google Scholar] [CrossRef]
- Myhre, J.; Saga, S.; Malmedal, W.; Ostaszkiewicz, J.; Nakrem, S. Elder Abuse and Neglect: An Overlooked Patient Safety Issue. A Focus Group Study of Nursing Home Leaders’ Perceptions of Elder Abuse and Neglect. BMC Health Serv. Res. 2020, 20, 199. [Google Scholar] [CrossRef] [PubMed]
- Mearns, E.S.; Liang, M.; Limone, B.L.; Gilligan, A.M.; Miller, J.D.; Schaum, K.D.; Waycaster, C.R. Economic Analysis and Budget Impact of Clostridial Collagenase Ointment Compared with Medicinal Honey for Treatment of Pressure Ulcers in the US. Clin. Outcomes Res. Ceor. 2017, 9, 485. [Google Scholar] [CrossRef]
- Gorecki, C.; Brown, J.M.; Nelson, E.A.; Briggs, M.; Schoonhoven, L.; Dealey, C.; Defloor, T.; Nixon, J. European Quality of Life Pressure Ulcer Project Group. Impact of Pressure Ulcers on Quality of Life in Older Patients: A Systematic Review. J. Am. Geriatr. Soc. 2009, 57, 1175–1183. [Google Scholar] [CrossRef]
- Gorecki, C.; Nixon, J.; Madill, A.; Firth, J.; Brown, J. What Influences the Impact of Pressure Ulcers on Health-Related Quality of Life? A Qualitative Patient-Focused Exploration of Contributory Factors. J. Tissue Viability 2012, 21, 3–12. [Google Scholar] [CrossRef]
- VanGilder, C.; Lachenbruch, C.; Algrim-Boyle, C.; Meyer, S. The International Pressure Ulcer Prevalence™ Survey: 2006–2015. J. Wound Ostomy Cont. Nurs. 2017, 44, 20–28. [Google Scholar] [CrossRef]
- Ahn, H.; Cowan, L.; Garvan, C.; Lyon, D.; Stechmiller, J. Risk Factors for Pressure Ulcers Including Suspected Deep Tissue Injury in Nursing Home Facility Residents: Analysis of National Minimum Data Set 3.0. Adv. Ski. Wound Care 2016, 29, 178–190. [Google Scholar] [CrossRef]
- Chun, S.Y.; Park, H.; Kim, W.; Joo, Y.J.; Lee, T.H.; Park, E.C. Ownership of Long-term Care Facility and Incidence of Pressure Ulcers among Republic of Korea. Health Policy Manag. 2020, 30, 522–530. [Google Scholar]
- Shin, J.H.; Choi, G.Y.; Lee, J. Impact of Nurse Staffing, Skill Mix and Stability on Resident Health Outcomes in Korean Nursing Homes. J. Korean Gerontol. Nurs. 2020, 22, 291–303. [Google Scholar] [CrossRef]
- Shin, J.H.; Renaut, R.A.; Reiser, M.; Lee, J.Y.; Tang, T.Y. Increasing Registered Nurse Hours Per Resident Day for Improved Nursing Home Residents’ Outcomes Using a Longitudinal Study. Int. J. Environ. Res. Public Health 2021, 18, 402. [Google Scholar] [CrossRef]
- Coleman, S.; Gorecki, C.; Nelson, E.A.; Closs, S.J.; Defloor, T.; Halfens, R.; Farrin, A.; Brown, J.; Schoonhoven, L.; Nixon, J. Patient Risk Factors for Pressure Ulcer Development: Systematic Review. Int. J. Nurs. Stud. 2013, 50, 974–1003. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Lam, K.M.; Deng, Z.; Choi, K.S. Prediction of Mortality after Radical Cystectomy for Bladder Cancer by Machine Learning Techniques. Comput. Biol. Med. 2015, 63, 124–132. [Google Scholar] [CrossRef] [PubMed]
- Salzberg, S.L. C4. 5: Programs for Machine Learning by J. Ross Quinlan. Morgan Kaufmann Publishers, Inc., 1993. Mach. Learn. 1994, 16, 235–240. [Google Scholar] [CrossRef]
- Senders, J.T.; Staples, P.C.; Karhade, A.V.; Zaki, M.M.; Gormley, W.B.; Broekman, M.L.; Smith, T.R.; Arnaout, O. Machine Learning and Neurosurgical Outcome Prediction: A Systematic Review. World Neurosurg. 2018, 109, 476–486. [Google Scholar] [CrossRef]
- Ambale-Venkatesh, B.; Yang, X.; Wu, C.O.; Liu, K.; Hundley, W.G.; McClelland, R.; Gomes, A.S.; Folsom, A.R.; Shea, S.; Guallar, E.; et al. Cardiovascular Event Prediction by Machine Learning: The Multi-ethnic Study of Atherosclerosis. Circ. Res. 2017, 121, 1092–1101. [Google Scholar] [CrossRef] [PubMed]
- Jhee, J.H.; Lee, S.; Park, Y.; Lee, S.E.; Kim, Y.A.; Kang, S.W.; Kwon, J.-Y.; Park, J.T. Prediction Model Development of Late-onset Preeclampsia Using Machine Learning-based Methods. PLoS ONE 2019, 14, e0221202. [Google Scholar] [CrossRef]
- Raita, Y.; Goto, T.; Faridi, M.K.; Brown, D.F.; Camargo, C.A.; Hasegawa, K. Emergency Department Triage Prediction of Clinical Outcomes Using Machine Learning Models. Crit. Care 2019, 23, 64. [Google Scholar] [CrossRef]
- Lee, S.K.; Ahn, J.; Shin, J.H.; Lee, J.Y. Application of Machine Llearning Methods in Nursing Home Research. Int. J. Environ. Res. Public Health 2020, 17, 6234. [Google Scholar] [CrossRef] [PubMed]
- Breiman, L. Statistical modeling: The Two Cultures (with comments and a rejoinder by the author). Stat. Sci. 2001, 16, 199–231. [Google Scholar] [CrossRef]
- Furey, T.S.; Cristianini, N.; Duffy, N.; Bednarski, D.W.; Schummer, M.; Haussler, D. Support Vector Machine Classification and Validation of Cancer Tissue Samples Using Microarray Expression Data. Bioinformatics 2000, 16, 906–914. [Google Scholar] [CrossRef]
- Boyle, C.A.; Boulet, S.; Schieve, L.A.; Cohen, R.A.; Blumberg, S.J.; Yeargin-Allsopp, M.; Visser, S.; Kogan, M.D. Trends in the Prevalence of Developmental Disabilities in US Children, 1997–2008. Pediatrics 2011, 127, 1034–1042. [Google Scholar] [CrossRef]
- Amir, Y.; Lohrmann, C.; Halfens, R.J.; Schols, J.M. Pressure Ulcers in Four Indonesian Hospitals: Prevalence, Patient Characteristics, Ulcer Characteristics, Prevention and Treatment. Int. Wound J. 2017, 14, 184–193. [Google Scholar] [CrossRef]
- Kottner, J.; Black, J.; Call, E.; Gefen, A.; Santamaria, N. Microclimate: A Critical Review in the Context of Pressure Ulcer Prevention. Clin. Biomech. 2018, 59, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Arai, K.; Yamamoto, K.H.; Suzuki, T.; Mitsukawa, N.; Ishii, I. Risk Factors Affecting Pressure Ulcer Healing: Impact of Prescription Medications. Wound Repair Regen. 2020, 28, 409–415. [Google Scholar] [CrossRef]
- Jaul, E.; Meiron, O.; Menczel, J. The Effect of Pressure Ulcers on the Survival in Patients with Advanced Dementia and Domorbidities. Exp. Aging Res. 2016, 42, 382–389. [Google Scholar] [CrossRef]
- Ahn, H.; Stechmiller, J.; Horgas, A. Pressure Ulcer-related Pain in Nursing Home Residents with Cognitive Impairment. Adv. Ski. Wound Care 2013, 26, 375–380. [Google Scholar] [CrossRef]
- Hartmann, T. Parasocial Interaction, Parasocial Relationships, and Well-being. In The Routledge Handbook of Media Use and Well-Being: International Perspectives on Theory and Research on Positive Media Effects; Routledge: Abingdon, UK, 2016; pp. 131–144. [Google Scholar]
- Shin, J.H. Nursing Staff Characteristics on Resident Outcomes in Nursing Homes. J. Nurs. Res. 2019, 27, 1. [Google Scholar] [CrossRef]
- Rolland, Y.; Mathieu, C.; Piau, C.; Cayla, F.; Bouget, C.; Vellas, B.; de Souto Barreto, P. Improving the Quality of Care of Long-Stay Nursing Home Residents in France. J. Am. Geriatr. Soc. 2016, 64, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Sharkey, S.; Hudak, S.; Horn, S.D.; Barrett, R.; Spector, W.; Limcangco, R. Exploratory Study of Nursing Home Factors Associated with Successful Implementation of Clinical Decision Support Tools for Pressure Ulcer Prevention. Adv. Ski. Wound Care 2013, 26, 83–92. [Google Scholar] [CrossRef] [PubMed]
| No. | Variable | Importance Score |
|---|---|---|
| 1 | Hours per resident day of director | 4.431 |
| 2 | Proportion of bedridden residents | 4.387 |
| 3 | Proportion of residents taking antidepressants or sleeping pills | 4.129 |
| 4 | Proportion of residents with cognitive dysfunction | 4.031 |
| 5 | Proportion of residents with urinary incontinence | 3.862 |
| 6 | Proportion of residents with restraint | 3.700 |
| 7 | Hours per resident day of the certified nurse aide | 3.411 |
| 8 | Number of current residents | 3.150 |
| 9 | Ratio of Grade A | 3.105 |
| 10 | Retention rate of care worker | 3.013 |
| Variable | Label (Range) | n | % | M ± SD |
|---|---|---|---|---|
| Average number of current residents | 70.03±51.11 | |||
| Long-term care facility grade (%) | Grade A (Superior) a | 23 | 38.3 | |
| Grade B (Above average) b | 8 | 13.3 | ||
| Grade C (Average) c | 6 | 10.0 | ||
| Grade D (Below average) d | 7 | 11.7 | ||
| Grade E (Poor) e | 16 | 26.7 | ||
| HPRD of staff | Director | 0.26 ± 0.23 | ||
| Secretary general | 0.12 ±0.12 | |||
| Social worker | 0.39 ± 0.27 | |||
| Dietician | 0.09 ± 0.09 | |||
| Administrative staff | 0.14 ± 0.22 | |||
| Registered nurses | 0.19 ± 0.24 | |||
| Certified nurse aides | 0.36 ± 0.26 | |||
| Care worker | 3.82 ± 1.63 | |||
| Retention rate of staff | Director | 78.71 ± 20.78 | ||
| Secretary general | 79.72 ± 31.16 | |||
| Social worker | 88.12 ± 20.21 | |||
| Dietician | 72.12 ± 20.11 | |||
| Administrative staff | 68.72 ± 23.19 | |||
| Registered nurses | 81.72 ± 30.29 | |||
| Certified nurse aide | 76.82 ± 28.29 | |||
| Care worker | 67.72 ± 30.22 | |||
| Age | 83.60 ± 2.40 | |||
| Gender (%) | Female | 78.95 ± 11.30 | ||
| Male | 20.77 ± 11.35 | |||
| Quality of care of residents | Cognitive dysfunction | 61.56 | ||
| Urinary Incontinence | 41.10 | |||
| Antidepressants or sleeping pills | 26.73 | |||
| Fecal Incontinence | 21.42 | |||
| Bedridden | 25.91 | |||
| Physically restrained | 7.40 | |||
| Tube feeding | 8.66 | |||
| Aggressive behavior | 4.62 | |||
| Depression | 5.55 | |||
| Fall prevalence | 4.84 | |||
| Help for daily living | 4.27 | |||
| Slip prevalence | 3.36 | |||
| Hospital admission | 2.69 | |||
| Range of motion | 2.52 | |||
| 10% Weight loss | 1.68 | |||
| 5% Weight loss | 1.12 | |||
| Pressure sore prevalence | 1.21 | |||
| Dehydration | 0.73 |
| Model | Accuracy | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|
| Random forest | 0.843 | 0.513 | 0.943 | 0.732 | 0.865 |
| Logistic regression | 0.797 | 0.200 | 0.977 | 0.727 | 0.801 |
| Linear SVM | 0.788 | 0.125 | 0.989 | 0.769 | 0.789 |
| Polynomial SVM | 0.797 | 0.138 | 0.996 | 0.917 | 0.792 |
| Radial SVM | 0.794 | 0.138 | 0.992 | 0.846 | 0.792 |
| Sigmoid SVM | 0.767 | 0.150 | 0.955 | 0.500 | 0.767 |
| Model | Combined Variables |
|---|---|
| Random forest | Grade A + CAN HPRD + HPRD of director + urinary incontinence + medication + restraint |
| Logistic regression | Grade A + cognitive dysfunction + bedridden |
| Linear SVM | Average number of current residents + Grade A + urinary incontinence + bedridden |
| Polynomial SVM | Average number of current residents + cognitive dysfunction + urinary incontinence + restraint |
| Radial SVM | Average number of current residents + Grade A + HPRD of CNA + retention rate of CW + cognitive dysfunction |
| Sigmoid SVM | Grade A + HPRD of director + bed ridden + medication |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.-K.; Shin, J.H.; Ahn, J.; Lee, J.Y.; Jang, D.E. Identifying the Risk Factors Associated with Nursing Home Residents’ Pressure Ulcers Using Machine Learning Methods. Int. J. Environ. Res. Public Health 2021, 18, 2954. https://doi.org/10.3390/ijerph18062954
Lee S-K, Shin JH, Ahn J, Lee JY, Jang DE. Identifying the Risk Factors Associated with Nursing Home Residents’ Pressure Ulcers Using Machine Learning Methods. International Journal of Environmental Research and Public Health. 2021; 18(6):2954. https://doi.org/10.3390/ijerph18062954
Chicago/Turabian StyleLee, Soo-Kyoung, Juh Hyun Shin, Jinhyun Ahn, Ji Yeon Lee, and Dong Eun Jang. 2021. "Identifying the Risk Factors Associated with Nursing Home Residents’ Pressure Ulcers Using Machine Learning Methods" International Journal of Environmental Research and Public Health 18, no. 6: 2954. https://doi.org/10.3390/ijerph18062954
APA StyleLee, S.-K., Shin, J. H., Ahn, J., Lee, J. Y., & Jang, D. E. (2021). Identifying the Risk Factors Associated with Nursing Home Residents’ Pressure Ulcers Using Machine Learning Methods. International Journal of Environmental Research and Public Health, 18(6), 2954. https://doi.org/10.3390/ijerph18062954








