Abstract
The association between physical illness and depression implies a poorer management of chronic disease and a lower response to antidepressant treatments. Our study evaluates the effectiveness of a psychoeducational group intervention led by Primary Care (PC) nurses, aimed at patients of this kind. It is a randomized, multicenter clinical trial with intervention (IG) and control groups (CG), blind response variables, and a one year follow-up. The study included 380 patients ≥50 years of age from 18 PC teams. The participants presented depression (BDI-II > 12) and a physical comorbidity: diabetes mellitus type 2, ischemic heart disease, chronic obstructive pulmonary disease, and/or asthma. The IG (n = 204) received the psychoeducational intervention (12 weekly sessions of 90 min), and the CG (n = 176) had standard care. The patients were evaluated at baseline, and at 4 and 12 months. The main outcome measures were clinical remission of depressive symptoms (BDI-II ≤ 13) and therapeutic response (reduction of depressive symptoms by 50%). Remission was not significant at four months. At 12 months it was 53.9% in the IG and 41.5% in the CG. (OR = 0.61, 95% CI, 0.49–0.76). At 4 months the response in the IG (OR = 0.59, 95% CI, 0.44–0.78) was significant, but not at 12 months. The psychoeducational group intervention led by PC nurses for individuals with depression and physical comorbidity has been shown to be effective for remission at long-term and for therapeutic response at short-term.
1. Introduction
Depression affects around 300 million individuals worldwide, that is to say 4.4% of the population, and represents a frequent cause of morbidity, disability, and loss of productivity [1,2]. The World Health Organization (WHO) estimates that depression will be the main health problem by 2030 [3]. This disorder, which is common in Primary Care (PC) consultations, represents one of the main reasons for the loss of quality-adjusted life years (QALYs) [4]. There is some evidence linking physical illness and depression. According to the National Institute for Health and Care Excellence (NICE) [5] guidelines, depression is present in 20% of individuals presenting a chronic physical pathology, and its correct treatment may improve both life expectancy and its quality. Numerous studies have reported that in individuals with ischemic heart disease (IHD) the prevalence of postinfarction depression is around 27% which is considerably higher than that observed in the general population [6,7,8,9]. In the case of type 2 diabetes mellitus (DM), depression is associated with a worse quality of life, lower adhesion to pharmacological treatment, greater metabolic decompensation, and decreased preventive self-care irrespective of the individual’s chronic pathology [10,11,12]. Other studies with patients suffering from chronic obstructive pulmonary disease (COPD) have observed depression to be an indicator for emergency room care use and hospitalization due to acute exacerbation of the condition, irrespective of its severity. In addition, they have reported worse adherence to prescribed pharmacological treatment and a deterioration in quality of life [13,14,15,16].
Most clinical guidelines and studies [6,17,18,19] indicate psychotherapy as the first line of treatment for mild and moderate depression as it is less invasive and more effective. Nevertheless, antidepressant pharmacology continues to be the most commonly prescribed remedy in spite of the possibility of unwanted secondary effects and financial expense [20]. In our environment, the yearly cost of antidepressants per patient in 2017 was €98.1, which represented an increase of 2.9% with respect to the 2016 [21]. It should be noted that when patients who have not clinically improved under antidepressant treatment receive some type of psychotherapy, they present a better symptomatology and remission rate at short-term [16]. Patients with chronic physical comorbidities are accustomed to receiving complex treatments for the management of their pathology. Nevertheless, adding a new drug for depression management should be carefully considered in order to avoid possible interactions. Training programs can enable PC professionals detect and efficiently deal with individuals presenting both depression and physical comorbidity and thus optimize their care. The various non-pharmacological interventions that have shown to be effective in the treatment of depression include group psychoeducation [22,23,24], cognitive behavioral therapy (CBT) either in groups or individually [25,26], problem-solving therapy (PST) [27], and physical exercise, for instance, Tai-Chi [28] and indoor rock-climbing [29]. A systematic revision which assessed the efficacy of treatments for depression in adults who had experienced an acute coronary syndrome found that CBT, together with oral antidepressants, improved depressive symptomatology [6]. Other articles have described how CBT and PST improved depressive symptoms and blood glucose levels in patients with DM [30,31,32,33].
This article evaluated the effectiveness of a psychoeducational group intervention carried out by PC nurses. They had previously received training related to the objective of the study. Research, such as the study performed by Casañas et al. [23,34], has demonstrated good results for individuals with depression. We included patients with both depression and physical comorbidity. The principal objective was to evaluate the effectiveness of a group intervention through the remission rate of depressive symptoms and the therapeutic response (50% reduction in depressive symptoms with respect to initial evaluation). A secondary objective was to assess whether the improvement in depressive symptoms was related to an enhanced quality of life following the intervention and during follow-up.
2. Materials and Methods
2.1. Design and Procedure
A multi-center, randomized, clinical trial composed of an intervention group (IG) and a control one (CG). Variable responses were blinded and there was a one-year follow-up. The study methodology has been previously published [35]. The research was carried out in the PC centers, and 18 teams from urban and rural areas in Catalunya (Spain) took part. Patients were consecutively recruited by either the physician or nurse from the Primary Care Team (PCT) to which they corresponded. Informed consent was signed by the patients who were allocated by their PCT to either an IG or CG. Assignment to the groups was randomly generated by a centralized computer platform and the investigators were blinded to the outcome. Data were gathered at commencement of the study, and at four and twelve months following baseline evaluation. Patient assessment was carried out by external examiners who were unaware of which group they belonged to.
The study was approved by the Ethics Research Committee at the IDIAP Jordi Gol University Research Institute (P16/184).
2.2. Subjects
Taking into account a previous psychoeducational group study [23] which reported at nine-months follow-up a remission rate of depressive symptoms of 40% and 26% for the IG and CG, respectively, it was calculated that a sample of 504 individuals was required. Assuming a confidence interval (CI) of 95% and 5% precision, and anticipating 25% dropout, 252 participants were assigned to each group.
Inclusion criteria were (a) male and female patients aged >50 years; (b) presenting some of these physical comorbidities: DM, IHD, COPD, and/or asthma registered in the clinical records; (c) a rating >12 in the Beck Depression Inventory (BDI-II) according to the Spanish version adapted by Sanz et al. [36]; and (d) to have had one year follow-up in the same PCT.
Exclusion criteria were (a) patients diagnosed with dementia or moderate/elevated cognitive deterioration (5 or more errors on the Pfeiffer Scale); (b) major depressive disorder with psychotic symptoms or any other severe psychiatric comorbidities; (c) moderate/elevated risk of suicide (a rating of 6 on the MINI scale); (d) drug abuse or dependence (including alcohol); (e) physical illness at an advanced stage; (f) inability to attend the intervention; (g) referred to a psychologist at the Mental Health Community Team; and h) unable to understand the language of the tests (Spanish/Catalan).
2.3. Evaluation Tools and Variables
2.3.1. Baseline Variables: Sociodemographic and Clinical Ones
Data concerning the following sociodemographic variables were gathered: sex, age, civil status, educational level, employment situation, environment (rural/urban population >15,000 inhabitants), and socioeconomic status according to the MEDEA economic deprivation index [37] calculated for the urban population.
Hamilton
The Hamilton scale, with a score 0–56, was employed to measure anxiety [38]. As it quantifies intensity rather than the presence or not of anxiety it was useful to identify variations following the intervention.
Adjusted Morbidity Group (AMG)
The pooled adjusted morbidity (AMG) was also collected [39]. This measurement takes into account the individual’s multimorbidity according to illness typology and, in the case that it is chronic, identifies whether it affects one or more organic system. The range is from 1 to 4 according to the organs which present the pathology, there is a fifth category for when the patient presents an active neoplasm.
Pharmacological Prescription
The patients’ computerized clinical records were used to obtain this information. The number of prescribed antidepressants and anxiolytics was recorded.
Intervention Compliance
Participants’ attendance at the sessions was recorded with a register filled in by the observing nurses.
Satisfaction
On finishing the last group session the participants filled in a questionnaire in which they indicated their level of satisfaction with the intervention. The questions concerned such aspects as knowledge acquired during the sessions and its application, the organization and duration of the sessions, and the objectives reached.
2.3.2. Clinical Remission and/or Depression Response at Short and Long-Term (One Year Follow-Up)
The primary outcomes were the remission rate of depressive symptoms and therapeutic response (50% reduction in depressive symptoms with respect to initial evaluation), measured on finishing the intervention (4 months) and at one year follow-up. They were evaluated with the Spanish adaptation of the BDI-II [36,40] which has shown good psychometric characteristics with respect to construct validity, internal consistence of the items, and predictive value. The questionnaire has a score ranging from 0 to 63 points. The accepted cut-off points to determine the gravity of the symptoms are: minimum depression (0–13 points), slight (14–19 points), moderate (20–28 points), and severe (29–63 points). A score of ≤13 in the BDI-II was considered remission, and therapeutic response a 50% reduction in depressive symptoms with respect to the initial evaluation.
2.3.3. Secondary Outcomes: Quality of Life at Short and Long-Term (One Year Follow-Up)
Quality of life was measured by the EuroQol scale (EQ-5D) [41], the Spanish adaptation of which has shown good construct validity. It is a self-administered instrument composed of two parts, the descriptive EQ-5D system and the visual analogue scale (EQ-VAS). The former evaluates five health dimensions: mobility, personal care, daily activities, pain, and anxiety/depression. There are five response options for each item which range from “no problems” to “extreme problems”. The latter measures the individual’s global health level with a score from 0 (the worst state of health) to 100 (the best possible).
2.4. Psychoeducational Group Intervention
Patients assigned to the IG received a psychoeducational group intervention directed by PC nurses. The intervention consisted of 12 weekly sessions held consecutively for 3 months. Each session lasted 90 min. The program of the sessions is explained in the protocol [35]. It provided: (1) health education about chronic pathologies and depressive symptoms; (2) information regarding the relationship between a chronic pathology and depressive symptoms; (3) health education about: diet, physical exercise, sleep, agreeable activities, social skills, pharmacological treatment and adherence to it; (4) breathing techniques; (5) problem-solving techniques, behavioral activation, and cognitive-behavioral perspective about depression; and (6) confidence and assertiveness. After each session, in order to improve proactivity, the patients were assigned tasks to be carried out during the week which would be explained to the group in the following session. At the end of the final session the participants could fill out a satisfaction survey in order to evaluate the intervention.
The sessions were conducted by two PC nurses from each participating center and held in the same location, space and equipment permitting. The nurses had received prior training based on the psychoeducational group intervention protocol [42]. The twenty-hour program was given by psychologists, community nurses, and mental health specialists who had previous experience of leading groups. It included the content of the twelve sessions in order to ensure homogenization of the intervention.
Six months after commencement of the intervention the IG patients received a telephone call from the evaluators. They were asked about their mood and general health, and whether they were better/the same/worse than when the intervention had finished. Questions were asked about some of the goals achieved related to the proposed changes in diet, physical activity, rest, sleep, and free time/entertainment. In addition, patients’ responses to whether or not they had put into practice the techniques acquired during the intervention (controlled breathing, problem-solving, assertive communication, and restructuring of thoughts) were noted. They were also questioned about any pharmacological treatment they took and their compliance.
The CG patients received their usual attention from the PC team. They were seen by their physician/nurse without following any previously established pattern. Appointments were made according to the habitual clinical criteria corresponding to the patients’ chronic pathology or depressive symptomatology.
2.5. Data Analysis
The analyses were performed on an intention-to-treat basis. Missing data were accounted for through Predictive Mean Matching with ten imputations each of which has five interactions. The evaluation of the parameters of each imputation was carried out according to Rubin’s rules [43].
Descriptive statistics were employed to summarize data at a general level and for groups (IG and CG). Continuous variables are expressed by means and standard deviation (SD), the categorical categories are shown as frequencies and percentages.
So as to assess differences between characteristics (variables) according to group, chi-square test was used for categorical variables and Student’s T test for continuous ones. In both cases, a p-value < alpha 0.05 was considered statistically significant.
Logistic regression was employed for the main objective in order to evaluate the differences in both groups for clinical remission rate and 50% response post-intervention (4 months) and 12 months from baseline. Results are presented as crude and adjusted for sex, age, and anxiety symptoms. The Odds Ratios (OR) are shown with their 95% CI.
Finally, in order to compare the mean differences between the groups with respect to the BDI-II and Euroqol multi-level models with mixed effects were applied. In this way, the mean differences between groups were assessed and the 95% CI calculated. The statistical analyses were performed with R Software for Windows version 3.6.1, Vienna, Austria.
3. Results
A total of 380 patients were included with a mean age of 68.4 years (SD:8.8), women represented 81.8%. The flow of participants is depicted in Figure 1. They were randomized into two groups: the IG (n = 204) who received the psychoeducational intervention, and the CG (n = 176) who had the usual clinical attention from their PC physician/nurse. On termination of the intervention 66 participants (29 IG and 37 GC) were not evaluated as they had not answered the questionnaire. At one-year follow-up the BDI-II questionnaire had not been completed by 75 patients (IG n = 36, CG n = 39) which represents a drop-out rate of 17.6% and 22.2%, respectively. The principal causes were inability to get in touch with the patient at the time of the questionnaire, the patient declining to continue in the study, the patient located out of the area or hospitalized, and, in the case of two participants, death (Figure 1). The mean time from the first evaluation was 4.4 months (SD 1.3) for the post-intervention, and 11.5 months (SD 0.7) for the final evaluation for both groups.
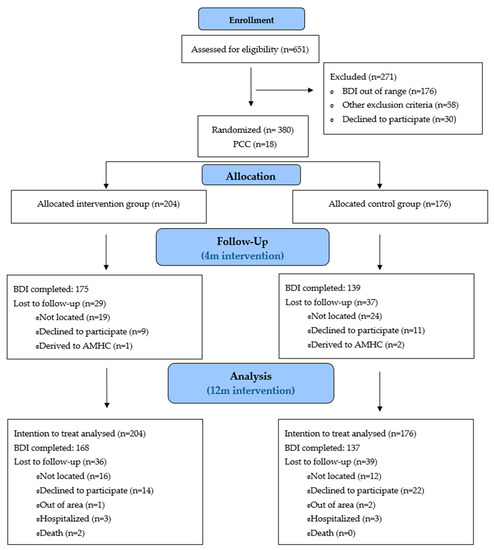
Figure 1.
The flow of participants. Abbreviations: PCC, primary care center. AMHC, Adult mental health center. BDI, Beck depression inventory.
Table 1 shows the baseline characteristics for both the IG and CG subjects. The groups were homogenous with respect to sociodemographic and clinical variables with the exception of asthma which was greater in the IG (p = 0.030). The most common sociodemographic profile was that of a woman, aged between 50 and 69 years, urban-dwelling, married, and retired who had finished primary education and presented high/medium-high socio-economic hardship. She suffered from chronic illnesses in more than four systems or organs (the most prevalent being DM), presented mobility problems and pain according to the eEQ-5D, and was prescribed antidepressants.

Table 1.
Sociodemographic and clinical variables at baseline.
Remission and therapeutic response results with imputed data are shown in Table 2. Remission represented 53.9% and 41.5% in the IG and GC, respectively, at twelve months of the intervention. A finding that was statistically significant (OR = 0.61, 95%CI, 0.49–0.76). These values were replicated when adjusted for age and sex (OR = 0.61, 95% CI, 0.48–0.76), and for age, sex, and anxiety according to Hamilton (OR = 0.61, 95%CI, 0.49–0.76). The therapeutic response improved at four months post-intervention in the IG (OR = 0.59, 95%CI, 0.44–0.78). When the model was adjusted for age and sex (OR = 0.59, 95%CI, 0.44–0.78), and age, sex, and anxiety according to Hamilton (OR = 0.59, 95% CI, 0.44–0.78) it did not vary.

Table 2.
Remission and therapeutic response of depression in the overall. mild and moderate depression patients. OR adjusted according to different models.
We also observed findings related to remission and therapeutic response in the patient subgroups according to the degree of depression (slight or moderate) in both IG and CG (Table 2). With respect to the IG, in patients with moderate depression, remission was observed at 12 months post-intervention (OR = 0.50, 95%CI, 0.35–0.71), and therapeutic response at 4 months (OR = 0.50, 95%CI, 0.35–0.71) and 12 months (OR = 0.53, 95% IC, 0.38–0.76). The values were maintained when the data were adjusted in the different models. The participants with slight depression in the IG had a remission at 12 months (OR = 0.66, 95%CI, 0.49–0.90), and a therapeutic response that was only statistically significant at 4 months (OR = 0.66, 95%CI, 0.45–0.97).
The therapeutic response was greater in the IG than in the CG at both 4 and 12 months according to the mean BDI-II values without achieving statistical significance (Table 3). With respect to the EQ-VAS, whilst the IG quality of life at 4 months was better perceived, at 12 months it matched that of the CG (Table 3).

Table 3.
Mean value (SD) of BDI-II and VAS Euroqol baseline, 4 m and 12 m. Changes BDI-II and VAS euroquol between groups.
Table 4 depicts the EQ-5D dimensions according to subgroups. Whilst the percentage of subjects who presented problems in the various dimensions was always higher in the CG than the IG at 4 and 12 months (with the exception of pain), these differences were not statistically significant. Nevertheless, the increase in the number of participants who had problems at 12 months in the CG was greater than in the IG with respect to mobility, selfcare, daily activities, and pain. In the area of depression and anxiety the percentages of subjects who presented problems was greater in the CG at 4 months (IG = 82.3% CG = 87.8%), and the same in both groups at 12 months (IG = 78.6 CG = 78.8).

Table 4.
EQ-5D dimensions for intervention group and control at baseline, 4 months, and 12 months.
At the end of the evaluation 61.9% and 62.0% of the IG and CG, respectively, were taking antidepressants. The percentage of subjects receiving these drugs remained the same in the IG (61.3% at commencement vs. 61.9% at 12 months), and increased in the CG (59.1 at commencement vs. 62.0%), without being statistically significant.
Mean attendance at the sessions was 7.2 (SD 4.24; range 0–12) and 65.2% of the participants (n = 133) received 7 or more sessions (Table 5). At 12 months those subjects that presented a remission had attended a mean of 8.5 sessions (SD 3.7), and those who did not present a depression remission had attended a mean of 7.1 (SD 4.2), with a statistical significance between groups (p = 0.021). Data concerning the satisfaction questionnaire are shown in Table 5. The level of satisfaction was a mean of 9.3 (SD 1.2) with a maximum of 10 and a minimum of 3. The topics that were considered the most useful were, in the following order: 1. Cognitive restructuring; 2. Behavioral activation and the education and identification of symptoms; 3. Diet; and 4. Breathing and relaxation techniques. Those considered less useful were: physical activity, use of time, and health education about pharmacological treatment.

Table 5.
Group intervention. Session attendance and level of satisfaction.
4. Discussion
Depression remission in patients presenting both depression and comorbidity was 12% higher in those who received the psychoeducational group intervention led by PC nurses than the control. The effect of the intervention on the response to depressive symptomatology was greater at short-term: a positive response in the IG was observed at 4-months post-intervention but not at 12. Such findings indicate that the intervention is efficient at short-term in decreasing symptomatology and at long-term in depression remission. In our sample more than 40% were aged over 70 years. In this regard, Wilkinson et al. [44] suggested that elderly individuals take longer to adapt to change. A possibility that could explain why our participants might have needed more time to assimilate the knowledge and skills imparted during the intervention sessions, and the reason remission appeared at long-term.
For the two IG depression severity subgroups (slight and moderate), a response at 4 months and remission at 12 months were greater, with statistical significance for both. Nevertheless, in the moderate depression subgroup the 50% improvement in symptomatology was maintained long-term up to 12 months, but not in the slight depression one. Such minor differences signify that intervention should not be focused solely on patients with moderate depression. Studies have demonstrated the efficacy, in a preventive manner, of behavioral activation and CBT in subjects with slight depression, thus avoiding the development of more severe symptoms [45].
Our results regarding effectiveness are similar to those of Casañas et al. [23,34,46] who also reported remission in the IG in a program very similar to ours, carried out by PC nurses but focused on subjects with depression from the general population. A systematic revision carried out by Kastner et al. reported that collaborative interventions with different care levels have been shown to be effective in improving depressive symptoms in adults with DM and cardiovascular disease [47]. Other studies have incorporated combinations of CBT and physical exercise into community-based interventions. Positive results were obtained with a 71% depression remission in patients with DM [32]. In addition, a study also performed in PC with CBT, but by final year medical students previously trained by psychiatrists, aimed at patients with depression and DM, obtained a significant decrease in the BDI-II [31].
Our intervention included psychoeducation related to depression and health education for the various comorbidities the patients presented. Emphasis was placed on healthy lifestyle habits: diet, physical activity, and rest. Such a mixed focus has been shown to be effective in other studies, mainly in patients with DM [32,33]. In contrast, other programs led by nurses for patients with DM and IHD, which only included CBT, did not obtain significant results (OR = 1.21, CI 95% 0.12 to 12.41) with respect to depressive symptoms [48].
Regarding our second objective, quality of life did not improve significantly with depression remission. Whilst an increase in the global ratings of the EQ-VAS in the IG was observed after the intervention, the findings were not statistically significant when compared to those in the CG. As reported by Orfila et al., quality of life in elderly individuals appears to strongly related to disability and functional limitation [49]. This could explain why it is not significantly affected by interventions aimed at improving depression. Indeed, other PC programs with patients presenting a similar profile to ours, aimed at promoting support and social participation in elderly individuals with a bad self-perception of health, did not report improvements in the subjects’ quality of life [50].
Research such as ours which evaluates a psychoeducational group intervention carried out by PC nurses for patients presenting depression and chronic organic pathology is scarce. The community nurse is the PC professional who is generally responsible for the follow-up of patients with chronic pathologies. It is, therefore, clear that training these nurses in group interventions is the most efficient way to deal with depression as one more comorbidity in such patients. The capacity of PC nurses, who have received prior training in mental health, to identify, evaluate, and manage the mental health risk of patients with chronic pathologies within a collaborative care regime has been demonstrated [51]. Aragonés et al. [52] reported that when nurses in charge of patient clinical follow-up encouraged treatment adherence and provided psychoeducational care to IG patients and their families, this resulted in favorable rates of remission (48.8% IG vs. 35.6% CG p = 0.026) and response to depression (66% IG vs. 51% CG p = 0.011). Qualitative research has evaluated impressions from both patients with depression and physical comorbidity (for instance, DM and IHD) and the PC nurses who attended them. It identified a low perception of need for care related to depression from the nurses, and the difficulty for patients to actively ask for help [53]. Evaluating the patient’s state of mind should form part of habitual clinical practice. The trust established between patients with chronic pathologies and their professionals of reference (doctors and nurses) should enable them to express their emotions, and permit negative states of mind such as depression be identified. Patients need time to speak and reflect on their feelings; their refusal to ask for help could be due to the stigma and negative connotations that depression continues to suffer from in our society. Lack of awareness about this condition, and the limitations some nurses may experience in addressing emotional distress, are barriers that could be overcome by our intervention. This could result in a correct management of patients similar to our study participants.
The group format of our intervention is an added value. It is well-known that group interventions provide therapeutic advantages and factors that differ from individual interventions [54]. Such benefits include social support, the feeling of belonging to a group, and the experience of sharing common problems.
The dropout rate in our study was lower than others carried out with patients presenting similar characteristics [23,50]. Attendance at the sessions was, however, moderate with a mean of seven sessions which has led to the possibility of shortening them. Such a figure is a little lower than that obtained by Casañas et al. who reported a mean of nine sessions [23], and in which there was also a decrease of the BDI-II in the IG. It is possible that the health status of the participants with comorbidities played a part. Such patients often feel unwell which hinders their leaving home to attend appointments. The support telephone call at six months probably influenced the good results obtained at long-term. Experience regarding telephoning in managing depression with physical comorbidities has been very positively rated by participants [55,56]. Such interventions could be a viable alternative when moving to a health center is complex, or in contexts such as the current Covid-19 pandemic where gatherings of patients represent a risk of infection. Telematically adapting interventions such as ours to maintain efficient management of depression, and its associated physical pathologies, could be an interesting possibility for the future. A meta-analysis assessing CBT efficacy through guided and non-guided line evaluation with respect to other kinds of interventions to treat depression, reported mean adherence rates very similar to ours, 76% in the case of guided CBT [57]. The therapeutical response of the patients in the guided line intervention was 48%, a figure close to the one we obtained at 12 months.
Consumption of medication was not reduced in the IG in spite of depression remission, and slightly increased in the CG. Such a finding may reflect the predisposition PC physicians have to introduce antidepressant treatment, and their reluctance to withdraw it at long-term despite the patient’s improvement. Such preferences do not always coincide with those of the patients who have been shown to be more in favor of some kind psychotherapy to treat depression rather than pharmacological treatment [58]. Moreover, as the current pandemic has resulted in a considerable increase in healthcare costs, interventions such as ours could have a better cost-effectiveness ratio.
One of the strengths of our study was that the intervention was carried out in an environment the patients frequently visited. In addition, the profile of the participants corresponded to that of the patients who generally attended PC consultations. Another strength is the study’s design, it was a randomized clinical trial with homogeneity between the IG and CG, and with a highly representative sample from both urban and rural areas. As the randomization was blinded the evaluations and statistical analysis provided greater validity to the results.
With regard to limitations, one of these is the lack of data in some subgroups with respect to civil status and employment situation which prevented us from carrying out an analysis from a social perspective. Another is that we did not make any distinctions regarding the date of diagnosis of depression. This meant we did not know whether the diagnosis of comorbidity was prior to diagnosis of depression or afterwards. Moreover, the fatigue resulting from dealing with chronic pathologies could be confused with a depressive state. Neither was the time of the evolution of depression assessed, another key factor in resistance to treatment. Another factor to take into consideration is the low participation of men which reflects the gender gap [59] regarding susceptibility to depression. Finally, at four months 21% of the IG participants and 8% of the CG had told the evaluator which group they belonged to. At 12 months the values were 23% and 8% for the IG and CG, respectively.
5. Conclusions
The psychoeducational group intervention conducted by PC nurses for patients with depression and physical comorbidity proved effective for depression remission at long-term and for therapeutic response short-term. Quality of life did not change significantly in both groups following the intervention.
Author Contributions
All the authors have contributed to the study. Conceptualization: A.R.-T., M.I.F.-S.-M., J.M.-R., and R.C.; methodology: A.R.-T., M.I.F.-S.-M., J.M.-P., R.C., G.S.-V., C.C.-S., R.M.-F., Q.F.-B., E.M.F.-L., J.M.-P., S.G.-T., and L.M.M.-L.; formal analysis: A.R.-T., M.I.F.-S.-M., E.N.-M., R.M.-F., and J.M.-R.; investigation: A.R.-T., M.I.F.-S.-M., J.M.-R., R.C., G.S.-V., C.C.-S., R.M.-F., and S.G.-T.; resources: M.I.F.-S.-M., J.M.-R., and R.C.; data curation: M.I.F.-S.-M., and E.N.-M.; writing—original draft preparation: A.R.-T.; writing—review and editing: A.R.-T., M.I.F.-S.-M., R.C., J.M.-R., Q.F.-B., M.C.-C., and M.F.J.-H.; supervision: M.I.F.-S.-M. and M.F.J.-H.; project administration: M.I.F.-S.-M.; funding acquisition: A.R.-T., M.I.F.-S.-M., J.M.-R., and R.C. All authors have read and agreed to the published version of the manuscript.
Funding
This study received a research grant from the Carlos III Institute of Health, Ministry of Economy and Competitiveness (Spain). It was awarded in the 2016 call for tenders under the Health Strategy Actions 2013–2016, with the National Research Programme aimed at Societal Challenges, within the Technical, Scientific and Innovation Research National Plan 2013–2016, with reference PI16/184, and was co-funded by European Union ERDF funds (European Regional Development Fund). In addition, this study has received a nursing research intensification grant from the Department of Health of the Generalitat de Catalunya (Spain). This was awarded in the 2017 call for tenders under the Health Research and Innovation Strategic Plan (PERIS) 2016–2020 with reference SLT002/17/00096. In addition, this study has received a predoctoral grant from University Institute of Research in Primary Care IDIAP Jordi Gol (Spain).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki. The study was approved by the Ethics Research Committee at the IDIAP Jordi Gol University Research Institute (P16/184).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All the principal investigators of the study had access to the complete database, and the datasets generated and analysed during the current study will be available from the corresponding author.
Acknowledgments
We would like to express our gratitude to all the nurses and other professionals who led the psychoeducational groups. We are grateful to all the professionals for their collaboration in the recruitment of participants in the different primary care centers that took part in the study.
Conflicts of Interest
All authors declare that they have no competing interests.
References
- World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organization; Licence: CC BY-NC-SA 3.0 IGO. Available online: https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf (accessed on 30 November 2020).
- Knapp, M.; McDaid, D.; Mossialos, E.; Thornicroft, G. Salud Mental en Europa: Políticas y Práctica. Líneas Futuras en Salud Mental. 2007, pp. 39–69. Available online: https://www.msssi.gob.es/organizacion/sns/planCalidadSNS/pdf/equidad/saludMentalEuropa.pdf (accessed on 13 October 2020).
- Organización Mundial de la Salud. La Carga Mundial de Morbilidad: Actualización de Ginebra: Organización Mundial de la Salud. Available online: www.who.int/healthinfo/global_burden_disease/2004_report_update/en/ (accessed on 30 November 2020).
- Fernández, A.; Saameño, J.Á.B.; Pinto-Meza, A.; Luciano, J.V.; Autonell, J.; Palao, D.; Salvador-Carulla, L.; Campayo, J.G.; Haro, J.M.; Serrano, A. Burden of chronic physical conditions and mental disorders in primary care. Br. J. Psychiatry 2010, 196, 302–309. [Google Scholar] [CrossRef] [PubMed]
- National Collaborating Centre for Mental Health. NICE Clinical Guideline 91- Depression in Adults with a Chronic Physical Health Problem: Treatment and Management; National Institute for Health and Clinical Excellence: London, UK, 2020; Available online: https://www.nice.org.uk/guidance/cg91/evidence/full-guideline-243876061 (accessed on 20 January 2021).
- Nieuwsma, J.; Williams, J.; Namdari, N.; Washam, J.; Raitz, G.; Blumenthal, J.; Jiang, W.; Yapa, R.; McBroom, A.; Lallinger, K. Diagnostic accuracy of screening test and treatment for post-acute coronary syndrome depression: A systematic review. Ann. Intern. Med. 2017, 167, 725. Available online: https://www.acpjournals.org/doi/10.7326/M17-1811 (accessed on 3 December 2020). [CrossRef] [PubMed]
- Doyle, F.; Freedland, K.; Carney, R.; de Jonge, P.; Dickens, C.; Pedersen, S.; Sorensen, J.; Dempster, M. Network meta-analysis of randomised trials of pharmacological, psychotherapeutic, exercise and collaborative care interventions for depressive symptoms in patients with coronary artery disease: Hybrid systematic review of systematic reviews protocol. Syst. Rev. 2019, 8, 71. [Google Scholar] [CrossRef] [PubMed]
- García Vicente, E.; Del Villar Sordo, V.; García, Y.; García, E.L. La depresión tras el infarto agudo de miocardio. Ann. Med. Intern. 2007, 24, 346–351. [Google Scholar] [CrossRef]
- Palacios, J.E.; Khondoker, M.; Achilla, E.; Tylee, A.; Hotopf, M. A single, one-off measure of depression and anxiety predicts future symptoms, higher healthcare costs, and lower quality of life in coronary heart disease patients: Analysis from a multi-wave, primary care cohort study. PLoS ONE 2016, 11, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Egede, L.E.; Grubaugh, A.L.; Ellis, C. The effect of major depression on preventive care and quality of life among adults with diabetes. Gen. Hosp. Psychiatry 2010, 32, 563–569. [Google Scholar] [CrossRef]
- Owens-Gary, M.D.; Zhang, X.; Jawanda, S.; Bullard, K.M.K.; Allweiss, P.; Smith, B.D. The Importance of Addressing Depression and Diabetes Distress in Adults with Type 2 Diabetes. J. Gen. Intern. Med. 2019, 34, 320–324. [Google Scholar] [CrossRef] [PubMed]
- Valenzuela, M.J.; Münzenmayer, B.; Osorio, T.; Arancibia, M.; Madrid, E. Sintomatologia depresiva y control metabólico en pacientes ambulatorios portadores de diabetes mellitus tipo. Rev. Med. Chil. 2018, 146, 1415–1421. [Google Scholar] [CrossRef] [PubMed]
- Blakemore, A.; Dickens, C.; Chew-Graham, C.A.; Afzal, C.W.; Tomenson, B.; Coventry, P.A.; Guthrie, E. Depression predicts emergency care use in people with chronic obstructive pulmonary disease: A large cohort study in primary care. Int. J. COPD 2019, 14, 1343–1353. [Google Scholar] [CrossRef]
- Iyer, A.S.; Bhatt, S.P.; Garner, J.J.; Wells, J.M.; Trevor, J.L.; Patel, N.M.; Kirkpatrick, D.; Williams, J.C.; Dransfield, M.T. Depression is associated with readmission for acute exacerbation of chronic obstructive pulmonary disease. Ann. Am. Thorac. Soc. 2016, 13, 197–203. [Google Scholar] [CrossRef]
- Albrecht, J.S.; Park, Y.; Hur, P.; Huang, T.Y.; Harris, I.; Netzer, G.; Lehmann, S.W.; Langenberg, P.; Khokhar, B.; Wei, Y.-J. Adherence to maintenance medications among older adults with chronic obstructive pulmonary disease the role of depression. Ann. Am. Thorac. Soc. 2016, 13, 1497–1504. [Google Scholar] [CrossRef]
- Ijaz, S.; Davies, P.; Cj, W.; Kessler, D.; Lewis, G.; Wiles, N. Psychological therapies for treatment-resistant depression in adults. Cochrane Database Syst. Rev. 2018, 5, CD010558. [Google Scholar] [CrossRef]
- Solomon, C.G.; Park, L.T.; Zarate, C.A. Depression in the primary care setting. N. Engl. J. Med. 2019, 380, 559–568. [Google Scholar]
- Linde, K.; Rücker, G.; Sigterman, K.; Jamil, S.; Meissner, K.; Schneider, A. Comparative effectiveness of psychological treatments for depressive disorders in primary care: Network meta-analysis. BMC Fam. Pract. 2015. [Google Scholar] [CrossRef] [PubMed]
- Registered Nurses’Association of Ontario (RNAO). Delirio, Demencia y Depresión en la Personas Mayores: Valoración y Cuidados. 2016. Available online: www.rnao.org/bestpractices (accessed on 22 November 2020).
- Martín, J.C.; Garriga, A.; Egea, C.; Diaz, G.; Campillo, M.-J.; Espinosa, R.M. Intervención psicológica escalonada con trastornos mentales comunes en Atención Primaria. Ann. Psicol. Ann. Psychol. 2017, 34, 30–40. [Google Scholar] [CrossRef]
- Observatori del Sistema de Salut de Catalunya. Central de resultats Atenció Primaria. 2018. Available online: http://observatorisalut.gencat.cat/ca/central_de_resultats/informes_cdr/dades_actuals (accessed on 17 September 2020).
- Sandberg, H.; Roaldset, Å. Effect of Group Psychoeducation for Major Depressive Disorder: A Systematic Review. Fac. Health Sci. 2019. Available online: https://munin.uit.no/bitstream/handle/10037/15371/thesis.pdf?isAllowed=y&sequence=2 (accessed on 30 November 2020).
- Casañas, R.; Catalán, R.; del Val, J.L.; Real, J.; Valero, S.; Casas, M. Effectiveness of a psycho-educational group program for major depression in primary care: A randomized controlled trial. BMC Psychiatry 2012, 12, 1–16. [Google Scholar] [CrossRef]
- Raya Tena, A.; Falder Serna, I.; Fernández Linares, E.M.; Casañas Sánchez, R. Impact of a psychoeducational group intervention for patients with mild/moderate depression in primary care consultations. Rev. Enferm. 2015, 38, 58–62. [Google Scholar] [PubMed]
- González-Blanch, C.; Ruiz-Torres, M.; Cordero-Andrés, P.; Umaran Alfageme, O.; Hernández Abellán, A.; Muñoz Navarro, R.; Cano Vindel, A. Terapia congnitivo-conductual transdiagnóstica en Atención Primaria. Rev. Psicoterapia 2018, 29, 37–52. [Google Scholar] [CrossRef]
- Cuijpers, P.; Noma, H.; Karyotaki, E.; Cipriani, A.; Furukawa, T.A. Effectiveness and Acceptability of Cognitive Behavior Therapy Delivery Formats in Adults with Depression: A Network Meta-analysis. JAMA Psychiatry 2019, 76, 700–707. [Google Scholar] [CrossRef]
- Zhang, A.; Park, S.; Sullivan, J.E.; Jing, S. The effectiveness of problem-solving therapy for primary care patients’ depressive and/or anxiety disorders: A systematic review and meta-Analysis. J. Am. Board Fam. Med. 2018, 31, 139–150. [Google Scholar] [CrossRef]
- Chi, I.; Jordan-Marsh, M.; Guo, M.; Xie, B.; Bai, Z. Tai chi and reduction of depressive symptoms for older adults: A meta-analysis of randomized trials. Geriatr. Gerontol. Int. 2013, 13, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Luttenberger, K.; Stelzer, E.M.; Först, S.; Schopper, M.; Kornhuber, J.; Book, S. Indoor rock climbing (bouldering) as a new treatment for depression: Study design of a waitlist-controlled randomized group pilot study and the first results. BMC Psychiatry 2015, 15, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, A.; Reimer, A.; Ehrmann, D.; Kulzer, B.; Haak, T.; Hermanns, N. Reduction of depressive symptoms predicts improved glycaemic control: Secondary results from the DIAMOS study. J. Diabet. Complicat. 2017, 31, 1608–1613. [Google Scholar] [CrossRef] [PubMed]
- Villamil-Salcedo, V.; Vargas-Terrez, B.E.; Caraveo-Anduaga, J.; González-Olvera, J.; Díaz-Anzaldúa, A.; Cortés-Sotres, J.; Pérez-Ávila, M. Glucose and cholesterol stabilization in patients with type 2 diabetes mellitus with depressive and anxiety symptoms by problem-solving therapy in primary care centers in Mexico City. Prim. Health Care Res. Dev. 2018, 19, 33–41. [Google Scholar] [CrossRef]
- De Groot, M.; Shubrook, J.H.; Hornsby, W.G.; Pillay, Y.; Mather, K.J.; Fitzpatrick, K.; Yang, Z.; Saha, C. Program ACTIVE II: Outcomes from a randomized, multistate community-based depression treatment for rural and urban adults with type 2 diabetes. Diabetes Care 2019, 42, 1185–1193. [Google Scholar] [CrossRef]
- Moncrieft, A.E.; Llabre, M.M.; McCalla, J.R.; Gutt, M.; Mendez, A.J.; Gellman, M.D.; Goldberg, R.B.; Schneiderman, N. Effects of a Multicomponent Life-Style Intervention on Weight, Glycemic Control, Depressive Symptoms, and Renal Function in Low-Income, Minority Patients with Type 2 Diabetes: Results of the Community Approach to Lifestyle Modification for Diabetes Random. Psychosom. Med. 2016, 78, 851–860. [Google Scholar] [CrossRef]
- Casañas, R.; Catalán, R.; Raya, A.; Real, J. Efectividad de un programa grupal psicoeducativo para la depresión mayor en atención primaria: Ensayo clínico controlado aleatorizado. Rev. Asoc. Esp. Neuropsiq. 2014, 34, 145–146. [Google Scholar] [CrossRef][Green Version]
- Casañas, R.; Martín Royo, J.; Fernandez-San-Martín, M.I.; Raya Tena, A.; Mendioroz, J.; Sauch Valmaña, G.; Masa-Font, R.; Casajuana-Closas, M.; Linares, E.M.F.; Cols-Sagarra, C. Effectiveness of a psychoeducation group intervention conducted by primary healthcare nurses in patients with depression and physical comorbidity: Study protocol for a randomized, controlled trial. BMC Health Serv. Res. 2019, 19, 3–9. [Google Scholar] [CrossRef]
- Sanz, J.; García-Vera, M.P.; Espinosa, R.; Fortún, M.; Vázquez, C. Adaptación española del Inventario para la Depresión de Beck-II ( BDI-II ), 3. Propiedades psicométricas en pacientes con trastornos psicológicos Spanish adaptation of the Beck Psychometric features in patiens with psychological disorders. Clínica Salud 2005, 16, 121–142. [Google Scholar]
- Domínguez-Berjón, M.F.; Borrell, C.; Cano-Serral, G.; Esnaola, S.; Nolasco, A.; Pasarín, M.I.; Ramis, R.; Saurina, C.; Escolar-Pujolar, A. Construcción de un índice de privación a partir de datos censales en grandes ciudades españolas (Proyecto MEDEA). Gac. Sanit. 2008, 22, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Lobo, A.; Chamorro, L.; Luque, A.; Dal-Ré, R.; Badia, X.; Baró, E. Validación de las versiones en español de la Montgomery-Asberg Depression Rating Scale y la Hamilton Anxiety Rating Scale para la evaluación de la depresión y de la ansiedad. Med. Clin. (Barc.) 2002, 118, 480–520. [Google Scholar] [CrossRef]
- Ministerio de Sanidad. Informe del Proyecto de Estratificación de la Población por Grupos de Morbilidad Ajustados (GMA) en el Sistema Nacional de Salud (2014–2016). España 2018; 103p. Available online: http://www.mscbs.gob.es/organizacion/sns/planCalidadSNS/pdf/informeEstratificacionGMASNS_20142016.pdf (accessed on 27 September 2020).
- Beck, A.T.; Steer, R.A.; Carbin, M.G. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin. Psychol. Rev. 1988, 8, 77–100. [Google Scholar] [CrossRef]
- Hernandez, G.; Garin, O.; Pardo, Y.; Vilagut, G.; Pont, À.; Suárez, M.; Neira, M.; Rajmil, L.; Gorostiza, I.; Ramallo-Fariña, Y. Validity of the EQ–5D–5L and reference norms for the Spanish population. Qual. Life Res. 2018, 27, 2337. [Google Scholar] [CrossRef]
- Casañas, R.; Falder, I.; Fernández, E.M.; Martín, J.; Moya, I.; Raya, A.; Psicodep, E. Programa de Sessions Grupals Psicoeducatives. Available online: http://ics.gencat.cat/web/.content/documents/assistencia/protocols/protocol_sesions_psicoeducatives.pdf (accessed on 8 December 2020).
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; John and Wiley & Sons: Hoboken, NJ, USA, 2004; p. 258. [Google Scholar]
- Wilkinson, P. Cognitive therapy with elderly people. Age Ageing 1997, 26, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Cuijpers, P.; Quero, S.; Dowrick, C.; Arroll, B. Psychological Treatment of Depression in Primary Care: Recent Developments. Curr. Psychiatry Rep. 2019, 21, 129. [Google Scholar] [CrossRef]
- Casañas Sánchez, R.; Raya Tena, A.; Ibáñez Pérez, L.; Valls Colomer, M.M. Psycho-education group therapy in patients with anxiety and depression in Barcelona Primary Care. Aten. Primaria 2009, 41, 227–228. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kastner, M.; Cardoso, R.; Lai, Y.; Treister, V.; Hamid, J.S.; Hayden, L.; Wong, G.; Ivers, N.M.; Liu, B.; Marr, S. Effectiveness of interventions for managing multiple high-burden chronic diseases in older adults: A systematic review and meta-analysis. CMAJ 2018, 190, E1004-12. [Google Scholar] [CrossRef]
- Pols, A.D.; Van Dijk, S.E.; Bosmans, J.E.; Hoekstra, T.; Van Marwijk, H.W.J.; van Tulder, M.W.; Adriaanse, M.C. Effectiveness of a stepped-care intervention to prevent major depression in patients with type 2 diabetes mellitus and/or coronary heart disease and subthreshold depression: A pragmatic cluster randomized controlled trial. PLoS ONE 2017, 12. [Google Scholar] [CrossRef]
- Orfila, F.; Ferrer, M.; Lamarca, R.; Tebe, C.; Domingo-Salvany, A.; Alonso, J. Gender differences in health-related quality of life among the elderly: The role of objective functional capacity and chronic conditions. Soc. Sci. Med. 2006, 63, 2367–2380. [Google Scholar] [CrossRef]
- Blancafort, S.; Monteserín, R.; Moral, I.; Roqué, M.; Rojano, X.; Coll, L. Promoting social capital, self-management and health literacy in older adults through a group-based intervention delivered in low-income urban areas: Results of the randomized trial aequalis. BMC Public Health 2021, 21, 1–12. [Google Scholar]
- Schlicht, K.; Morgan, M.A.J.; Fuller, J.; Coates, M.J.; Dunbar, J.A. Safety and acceptability of practice-nurse-managed care of depression in patients with diabetes or heart disease in the Australian TrueBlue study. BMJ Open 2013, 3, 1–6. [Google Scholar] [CrossRef][Green Version]
- Aragonès, E.; Piñol, J.L.; Caballero, A.; López, G.; Casaus, P.; Hernández, J.M.; Badia, W.; Folch, S. Effectiveness of a multi-component programme for managing depression in primary care: A cluster randomized trial. The INDI project. J. Affect. Disord. 2012, 142, 297–305. [Google Scholar] [CrossRef]
- Pols, A.D.; Schipper, K.; Overkamp, D.; Van Marwijk, H.W.J.; Van Tulder, M.W.; Adriaanse, M.C. Patients’ and practice nurses’ perceptions of depression in patients with type 2 diabetes and/or coronary heart disease screened for subthreshold depression. BMC Fam. Pract. 2018, 19, 1–14. [Google Scholar] [CrossRef]
- Guimón, J. Manual de Terapia de Grupos. Tipos, Modelos y Programas; Biblioteca Nueva: Madrid, Spain, 2003; 400p. [Google Scholar]
- Newby, J.; Robins, L.; Wilhelm, K.; Smith, J.; Fletcher, T.; Gillis, I.; Ma, T.; Finch, A.; Campbell, L.; Andrews, G. Web-based cognitive behavior therapy for depression in people with diabetes mellitus: A randomized controlled trial. J. Med. Internet Res. 2017, 19, e157. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Ell, K.; Jin, H.; Vidyanti, I.; Chou, C.P.; Lee, P.J.; Gross-Schulman, S.; Sklaroff, L.M.; Belson, D.; Nezu, A.M. Comparative effectiveness of a technology-facilitated depression care management model in safety-net primary care patients with type 2 diabetes: 6-Month outcomes of a large clinical trial. J. Med. Internet Res. 2018, 20. [Google Scholar] [CrossRef] [PubMed]
- Karyotaki, E.; Efthimiou, O.; Miguel, C.; Maas Genannt Bermpohl, F.; Furukawa, T.A.; Cuijpers, P. Internet-Based Cognitive Behavioral Therapy for Depression A Systematic Review and Individual Patient Data Network Meta-analysis Supplemental content. 2021. Available online: https://jamanetwork.com/ (accessed on 4 February 2021).
- Dorow, M.; Löbner, M.; Pabst, A.; Stein, J.; Riedel-Heller, S.G. Preferences for depression treatment including internet-based interventions: Results from a large sample of primary care patients. Front. Psychiatry 2018, 9, 1–13. [Google Scholar] [CrossRef]
- Kuehner, C. Why is depression more common among women than among men? Lancet Psychiatry 2017, 4, 146–158. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).