Does Lung Ultrasound Have a Role in the Clinical Management of Pregnant Women with SARS COV2 Infection?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Inclusion Criteria
- Singleton pregnancy
- A positive result to the nasopharyngeal swab and detection of SARS-CoV-2 by RT-PCR testing
- Age between 18 and 45 years
- A body mass index (BMI) ≤ 30
- Absence of previous or current pregnancy comorbidities
- Absence of maternal comorbidities
2.3. Exclusion Criteria
- Twin pregnancies
- A previous SARS-CoV-2 infection
- A maternal age >45 years
- BMI > 30
- A presence of maternal or pregnancy-related comorbidities.
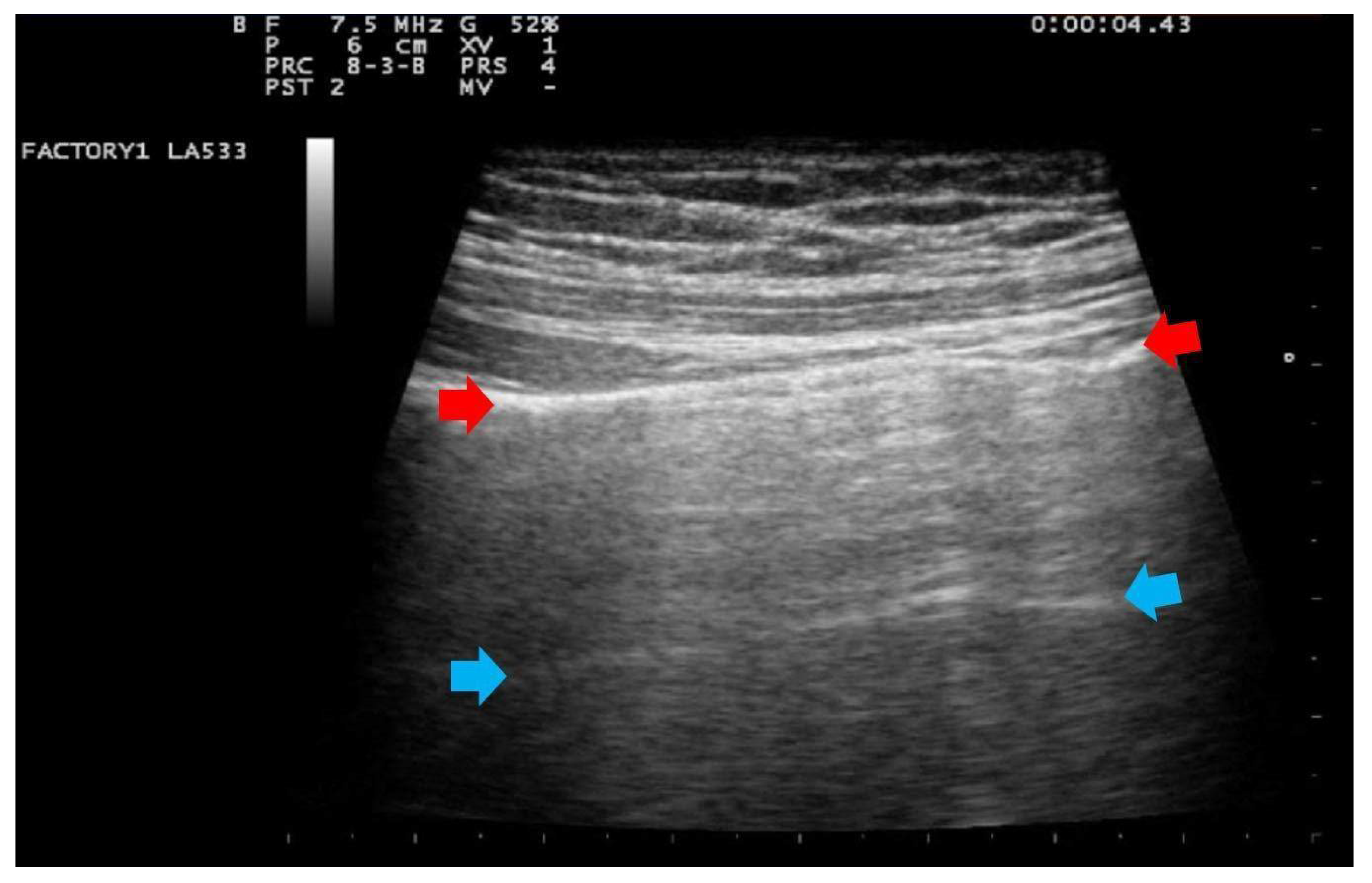
- Score 0:
- predominant A-lines or <3 separated B-lines. (Figure 1)
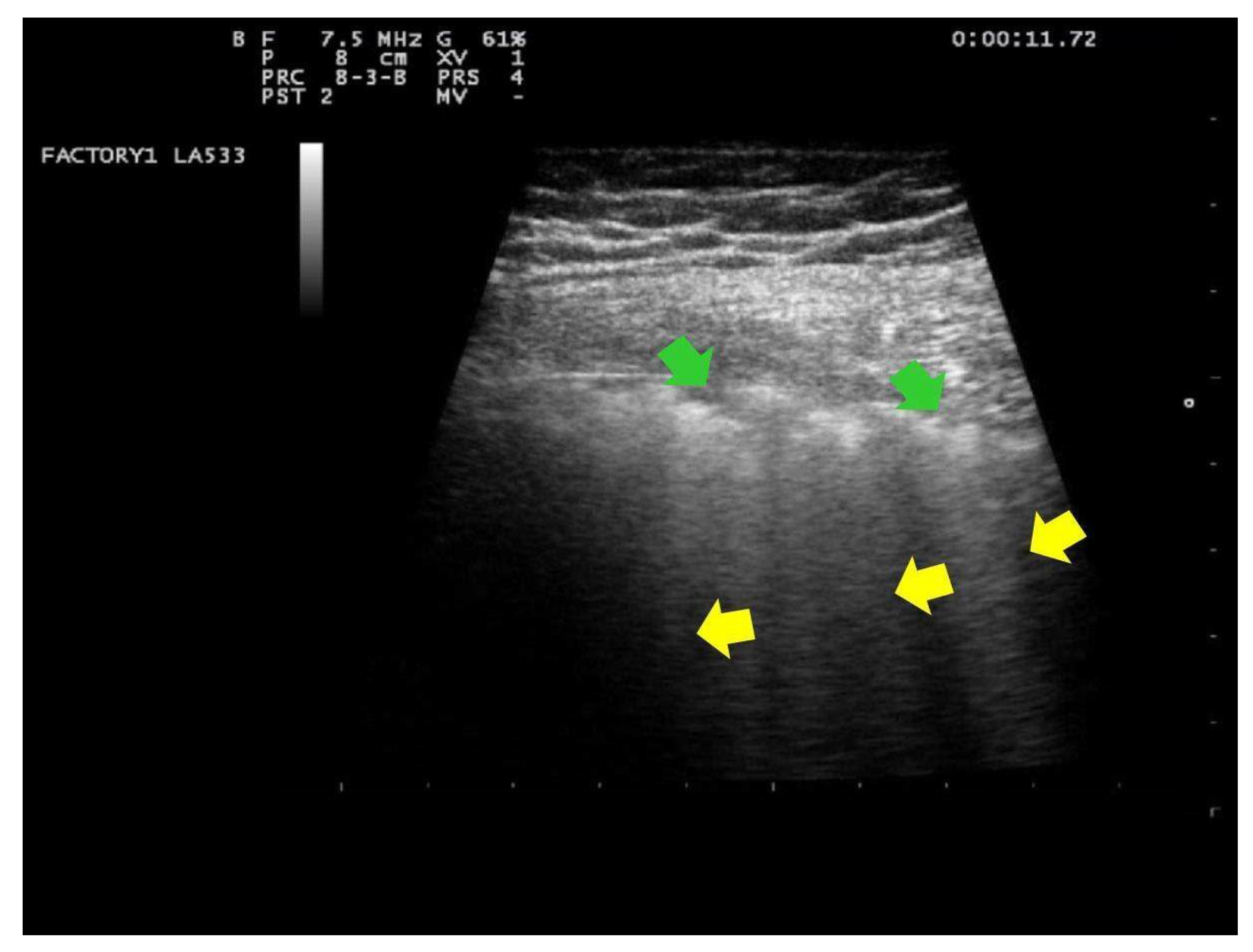
- Score 1:
- Score 1: at least three B-lines or confluent B-lines which occupy ≤ 50% of the screen without irregularities of pleural line. (Figure 2) Score 1p: B-lines with a clearly irregular pleural line.
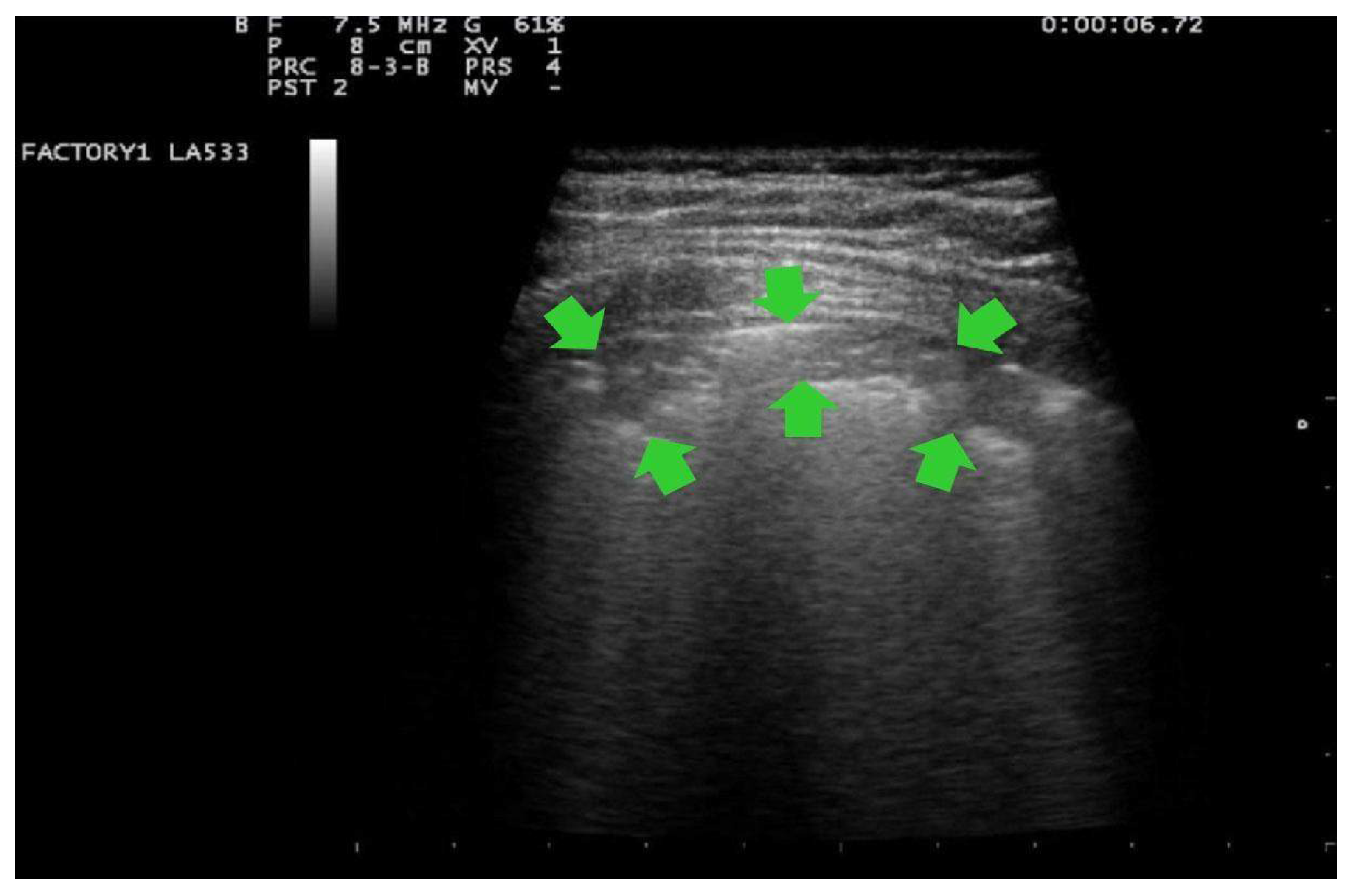
- Score 2:
- confluent B-lines which occupy >50% of the screen without irregularities pleural line. Score 2p: confluent B-lines with a clearly irregular pleural line (Figure 3).
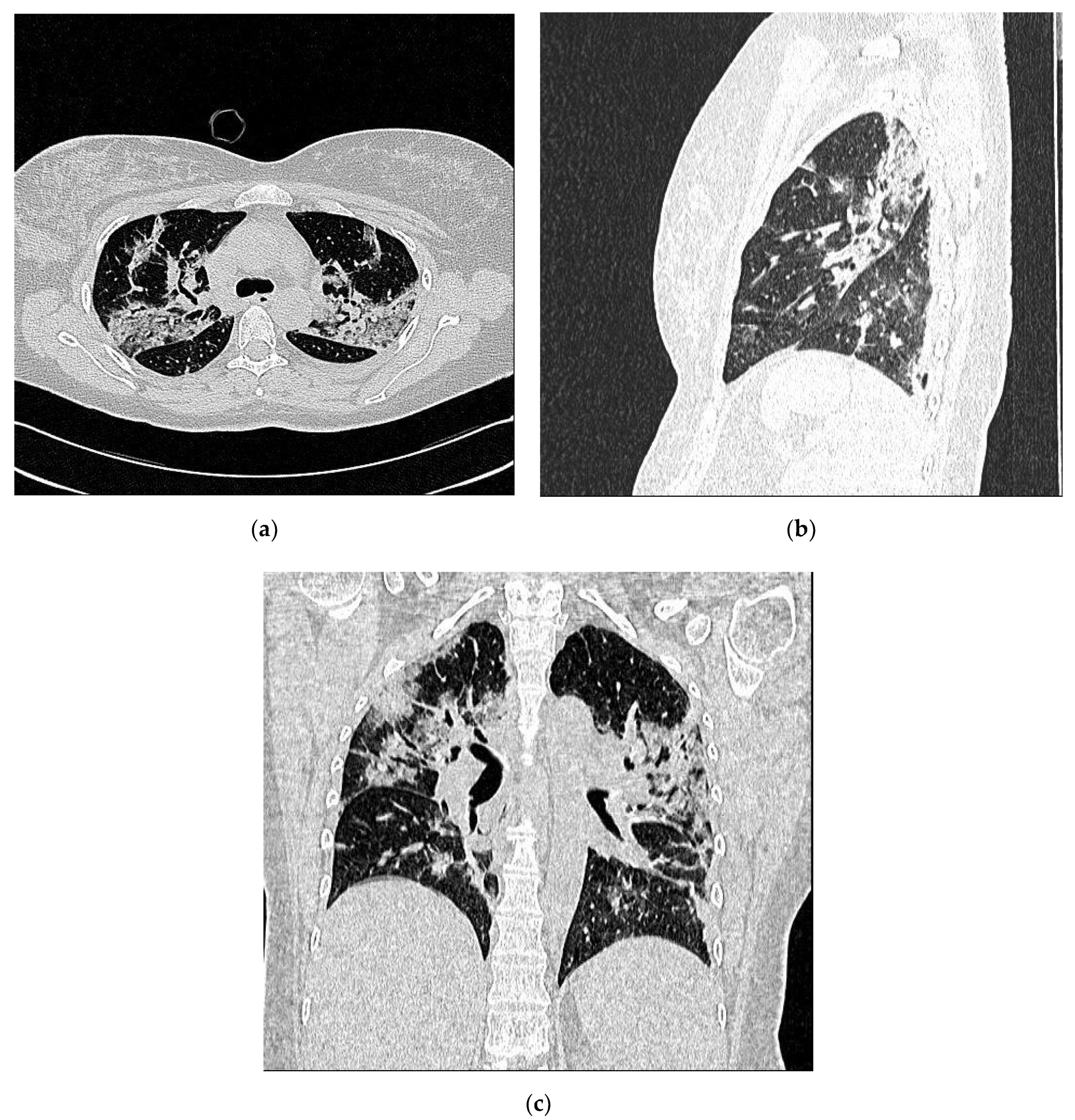
- Score 3:
- consolidations of large dimensions (at least >1 cm). (Figure 4)
2.4. Statistics
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cheruiyot, I.; Henry, B.M.; Lippi, G. Is there evidence of intra-uterine vertical transmission potential of COVID-19 infection in samples tested by quantitative RT-PCR? Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 249, 100–101. [Google Scholar] [CrossRef] [PubMed]
- Dong, E.; Du, H.; Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020, 20, 533–534. [Google Scholar] [CrossRef]
- Zaigham, M.; Andersson, O. Maternal and perinatal outcomes with COVID-19: A systematic review of 108 pregnancies. Acta Obstet. Gynecol. Scand. 2020, 99, 823–829. [Google Scholar] [CrossRef] [PubMed]
- Bellos, I.; Pandita, A.; Panza, R. Maternal and perinatal outcomes in pregnant women infected by SARS-CoV-2: A meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 256, 194–204. [Google Scholar] [CrossRef]
- Di Mascio, D.; Khalil, A.; Saccone, G.; Rizzo, G.; Buca, D.; Liberati, M.; Vecchiet, J.; Nappi, L.; Scambia, G.; Berghella, V.; et al. Outcome of coronavirus spectrum infections (SARS, MERS, COVID-19) during pregnancy: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. MFM 2020, 2, 107. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.F.; Chow, K.M.; Leung, T.N.; Ng, W.F.; Ng, T.K.; Shek, C.C.; Ng, P.C.; Lam, P.W.; Ho, L.C.; To, W.W.; et al. Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. Am. J. Obstet. Gynecol. 2004, 191, 292–297. [Google Scholar] [CrossRef]
- Zambrano, L.D.; Ellington, S.; Strid, P.; Galang, R.R.; Oduyebo, T.; Tong, V.T.; Woodworth, K.R.; Nahabedian, J.F.; Baumgartner, A.E.; Gilboa, S.M.; et al. Update: Characteristics of Symptomatic Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status—United States, 22 January–3 October. MMWR. Morb. Mortal. Wkly. Rep. 2020, 69, 1641–1647. [Google Scholar] [CrossRef]
- Piccinni, M.P.; Romagnani, S. Regulation of fetal allograft survival by hormone-controlled Th1- and Th2-type cytokines. Immunol. Res. 1996, 15, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Siiteri, P.K.; Febres, F.; Clemens, L.E.; Chang, R.J.; Gondos, B.; Stites, D. Progesterone and Maintenance of Pregnancy: Is Progesterone Nature’s Immunosuppressant? Ann. N. Y. Acad. Sci. 1977, 286, 384–397. [Google Scholar] [CrossRef]
- Druckmann, R.; Druckmann, M.A. Progesterone and the immunology of pregnancy. J. Steroid Biochem. Mol. Biol. 2005, 97, 389–396. [Google Scholar] [CrossRef]
- Hall, O.J.; Klein, S.L. Progesterone-based compounds affect immune responses and susceptibility to infections at diverse mucosal sites. Mucosal Immunol. 2017, 10, 1097–1107. [Google Scholar] [CrossRef]
- Ramsey, P.S.; Ramin, K.D. Pneumonia in Pregnancy. Obstet. Gynecol. Clin. N. Am. 2001, 28, 553–569. [Google Scholar] [CrossRef]
- Cruikshank, D.P.; Wigton, T.R.; Hays, P.M. Maternal physiology in pregnancy. In Obstetrics: Normal and Problem Pregnancies; Gabbe, S.G., Niebyl, J.R., Simpson, J.L., Eds.; CEPD: New York, NY, USA, 1996; pp. 93–95. [Google Scholar]
- Bremme, A.K. Haemostatic changes in pregnancy. Best Pract. Res. Clin. Haematol. 2003, 16, 153–168. [Google Scholar] [CrossRef]
- Dahlman, T.; Hellgren, M.; Blombäck, M. Changes in Blood Coagulation and Fibrinolysis in the Normal Puerperium. Gynecol. Obstet. Investig. 1985, 20, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Riordan, O.M.N.; Higgins, J.R. Haemostasis in normal and abnormal pregnancy. Best Pract. Res. Clin. Obstet. Gynaecol. 2003, 17, 385–396. [Google Scholar] [CrossRef]
- Di Renzo, G.C.; Giardina, I. Coronavirus disease 2019 in pregnancy: Consider thromboembolic disorders and thromboprophylaxis. Am. J. Obstet. Gynecol. 2020, 223, 135. [Google Scholar] [CrossRef]
- Dashraath, P.; Wong, J.L.J.; Lim, M.X.K.; Lim, L.M.; Li, S.; Biswas, A.; Choolani, M.; Mattar, C.; Su, L.L. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am. J. Obstet. Gynecol. 2020, 222, 521–531. [Google Scholar] [CrossRef]
- Jafari, M.; Pormohammad, A.; Neshin, S.A.S.; Ghorbani, S.; Bose, D.; Alimohammadi, S.; Basirjafari, S.; Mohammadi, M.; Ivey, R.C.; Razizadeh, M.H.; et al. Clinical characteristics and outcomes of pregnant women with COVID-19 and comparison with control patients: A systematic review and meta-analysis. Rev. Med. Virol. 2021, e2208, 2208. [Google Scholar] [CrossRef]
- Zhao, J.Y.; Yan, J.Y.; Qu, J.M. Interpretations of “Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 7)”. Chin. Med. J. 2020, 133, 1347–1349. [Google Scholar] [CrossRef]
- Fang, Y.; Zhang, H.; Xie, J.; Lin, M.; Ying, L.; Pang, P.; Ji, W. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology 2020, 296, E115–E117. [Google Scholar] [CrossRef]
- Zu, Z.Y.; Di Jiang, M.; Xu, P.P.; Chen, W.; Ni, Q.Q.; Lu, G.M.; Zhang, L.J. Coronavirus Disease 2019 (COVID-19): A Perspective from China. Radiology 2020, 296, E15–E25. [Google Scholar] [CrossRef]
- Bernheim, A.; Mei, X.; Huang, M.; Yang, Y.; Fayad, Z.A.; Zhang, N.; Diao, K.; Lin, B.; Zhu, X.; Li, K.; et al. Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. Radiology 2020, 295, 463. [Google Scholar] [CrossRef]
- Francone, M.; Iafrate, F.; Masci, G.M.; Coco, S.; Cilia, F.; Manganaro, L.; Panebianco, V.; Andreoli, C.; Colaiacomo, M.C.; Zingaropoli, M.A.; et al. Chest CT score in COVID-19 patients: Correlation with disease severity and short-term prognosis. Eur. Radiol. 2020, 30, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Gargani, L.; Picano, E. The risk of cumulative radiation exposure in chest imaging and the advantage of bedside ultrasound. Crit. Ultrasound J. 2015, 7, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Peng, Q.Y.; Wang, X.T.; Zhang, L.N. Chinese Critical Care Ultrasound Study Group (CCUSG). Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensiv. Care Med. 2020, 46, 849–850. [Google Scholar] [CrossRef]
- Moro, F.; Buonsenso, D.; Moruzzi, M.C.; Inchingolo, R.; Smargiassi, A.; Demi, L.; Larici, A.R.; Scambia, G.; Lanzone, A.; Testa, A.C. How to perform lung ultrasound in pregnant women with suspected COVID. Ultrasound Obstet. Gynecol. 2020, 55, 593–598. [Google Scholar] [CrossRef]
- Buonsenso, D.; Raffaelli, F.; Tamburrini, E.; Biasucci, D.G.; Salvi, S.; Smargiassi, A.; Inchingolo, R.; Scambia, G.; Lanzone, A.; Testa, A.C.; et al. Clinical role of lung ultrasound for diagnosis and monitoring of COVID-19 pneumonia in pregnant women. Ultrasound Obstet. Gynecol. 2020, 56, 106–109. [Google Scholar] [CrossRef]
- Bouhemad, B.; Mongodi, S.; Via, G.; Rouquette, I. Ultrasound for “Lung Monitoring” of Ventilated Patients. Anesthesiology 2015, 122, 437–447. [Google Scholar] [CrossRef]
- Youssef, A.; Cavalera, M.; Azzarone, C.; Serra, C.; Brunelli, E.; Casadio, P.; Pilu, G. The use of lung ultrasound during the COVID-19 pandemic. J. Popul. Ther. Clin. Pharmacol. 2020, 27, e64–e75. [Google Scholar] [CrossRef]
- World Health Organization. Clinical Management of COVID-19: Interim Guidance. Available online: https://apps.who.int/iris/handle/10665/332196 (accessed on 27 May 2020).
- Gargani, L.; Aboumarie, S.H.; Volpicelli, G.; Corradi, F.; Pastore, M.C.; Cameli, M. Why, when, and how to use lung ultrasound during the COVID-19 pandemic: Enthusiasm and caution. Eur. Hear. J. Cardiovasc. Imaging 2020, 21, 941–948. [Google Scholar] [CrossRef] [PubMed]
- Fonsi, G.B.; Sapienza, P.; Brachini, G.; Andreoli, C.; De Cicco, M.L.; Cirillo, B.; Meneghini, S.; Pugliese, F.; Crocetti, D.; Fiori, E.; et al. Is Lung Ultrasound Imaging a Worthwhile Procedure for Severe Acute Respiratory Syndrome Coronavirus 2 Pneumonia Detection? J. Ultrasound Med. 2020. [Google Scholar] [CrossRef]
- Hansell, D.M.; Bankier, A.A.; MacMahon, H.; McLoud, T.C.; Müller, N.L.; Remy, J. Fleischner Society: Glossary of Terms for Thoracic Imaging. Radiology 2008, 246, 697–722. [Google Scholar] [CrossRef] [PubMed]
- Pan, F.; Ye, T.; Sun, P.; Gui, S.; Liang, B.; Li, L.; Zheng, D.; Wang, J.; Hesketh, R.L.; Yang, L.; et al. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology 2020, 295, 715–721. [Google Scholar] [CrossRef] [PubMed]
- Casadio, P.; Youssef, A.; Arena, A.; Gamal, N.; Pilu, G.; Seracchioli, R. Increased rate of ruptured ectopic pregnancy in COVID-19 pandemic: Analysis from the North of Italy. Ultrasound Obstet. Gynecol. 2020, 56, 289. [Google Scholar] [CrossRef]
- Diaz, A.; Sarac, B.A.; Schoenbrunner, A.R.; Janis, J.E.; Pawlik, T.M. Elective surgery in the time of COVID. Am. J. Surg. 2020, 219, 900–902. [Google Scholar] [CrossRef]
- Iacobucci, G. Covid-19: All non-urgent elective surgery is suspended for at least three months in England. BMJ 2020, 368, 1106. [Google Scholar] [CrossRef]
- Mor, G.; Aldo, P.; Alvero, A.B. The unique immunological and microbial aspects of pregnancy. Nat. Rev. Immunol. 2017, 17, 469–482. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Wang, L.L.; Zhao, S.J.; Kim, K.J.; Mor, G.; Liao, A.H. Why are pregnant women susceptible to COVID-19? An immunological viewpoint. J. Reprod. Immunol. 2020, 139, 3122. [Google Scholar] [CrossRef] [PubMed]
- Lei, D.; Wang, C.; Li, C.; Fang, C.; Yang, W.; Chen, B.; Wei, M.; Xu, X.; Yang, H.; Wang, S.; et al. Clinical characteristics of COVID-19 in pregnancy: Analysis of nine cases. Chin. J. Perinat. Med. 2020, 23, 159–165. [Google Scholar] [CrossRef]
- Zhang, L.; Jiang, Y.; Wei, M.; Cheng, B.H.; Zhou, X.C.; Li, J.; Tian, J.H.; Dong, L.; Hu, R.H. Analysis of the pregnancy out-comes in pregnant women with COVID-19 in Hubei Province. Zhonghua Fu Chan Ke Za Zhi 2020, 55, 166–171. [Google Scholar] [CrossRef]
- Huang, W.; Zhao, Z.; He, Z.; Liu, S.; Wu, Q.; Zhang, X.; Qiu, X.; Yuan, H.; Yang, K.; Tang, X.; et al. Unfavorable outcomes in pregnant patients with COVID. J. Infect. 2020, 81, e99–e101. [Google Scholar] [CrossRef]
- Sutton, D.; Fuchs, K.; Alton, D.M.; Goffman, D. Universal Screening for SARS-CoV-2 in Women Admitted for Delivery. N. Engl. J. Med. 2020, 382, 2163–2164. [Google Scholar] [CrossRef]
- Liu, H.; Liu, F.; Li, J.; Zhang, T.; Wang, D.; Lan, W. Clinical and CT imaging features of the COVID-19 pneumonia: Focus on pregnant women and children. J. Infect. 2020, 80, e7–e13. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases from the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239–1242. [Google Scholar] [CrossRef]
- Xu, L.; Yang, Q.; Shi, H.; Lei, S.; Liu, X.; Zhu, Y.; Wu, Q.; Ding, X.; Tian, Y.; Hu, Q.; et al. Clinical presentations and outcomes of SARS-CoV-2 infected pneumonia in pregnant women and health status of their neonates. Sci. Bull. 2020, 65, 1537–1542. [Google Scholar] [CrossRef]
- Chen, L.; Li, Q.; Zheng, D.; Jiang, H.; Wei, Y.; Zou, L.; Feng, L.; Xiong, G.; Sun, G.; Wang, H.; et al. Clinical Characteristics of Pregnant Women with Covid-19 in Wuhan, China. N. Engl. J. Med. 2020, 382, 9226. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Wang, M.; Zhu, Z.; Liu, Y. Coronavirus disease 2019 (COVID-19) and pregnancy: A systematic review. J. Matern. Neonatal Med. 2020, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Guo, J.; Wang, C.; Luo, F.; Yu, X.; Zhang, W.; Li, J.; Zhao, D.; Xu, D.; Gong, Q.; et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. Lancet 2020, 395, 809–815. [Google Scholar] [CrossRef]
- Nie, R.; Wang, S.; Yang, O.; Fan, C.; Liu, Y.; He, W.; Jiang, M.; Liu, C.; Zeng, W.; Wu, J.; et al. Clinical features and the maternal and neonatal outcomes of pregnant women with coronavirus disease. MedRxiv 2020, 81, 1061. [Google Scholar] [CrossRef]
- Baud, D.; Greub, G.; Favre, G.; Gengler, C.; Jaton, K.; Dubruc, E.; Pomar, L. Second-Trimester Miscarriage in a Pregnant Woman With SARS-CoV-2 Infection. JAMA 2020, 323, 2198–2200. [Google Scholar] [CrossRef] [PubMed]
- Dong, L.; Tian, J.; He, S.; Zhu, C.; Wang, J.; Liu, C.; Yang, J. Possible Vertical Transmission of SARS-CoV-2 From an Infected Mother to Her Newborn. JAMA 2020, 323, 1846–1848. [Google Scholar] [CrossRef]
- Fan, C.; Lei, D.; Fang, C.; Li, C.; Wang, M.; Liu, Y.; Bao, Y.; Sun, Y.; Huang, J.; Guo, Y.; et al. Perinatal Transmission of 2019 Coronavirus Disease–Associated Severe Acute Respiratory Syndrome Coronavirus 2: Should We Worry? Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Li, Y.; Zhao, R.; Zheng, S.; Chen, X.; Wang, J.; Sheng, X.; Zhou, J.; Cai, H.; Fang, Q.; Yu, F.; et al. Lack of Vertical Transmission of Severe Acute Respiratory Syndrome Coronavirus 2, China. Emerg. Infect. Dis. 2020, 26, 1335–1336. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Zhou, Z.; Zhang, J.; Zhu, F.; Tang, Y.; Shen, X. A Case of 2019 Novel Coronavirus in a Pregnant Woman with Preterm Delivery. Clin. Infect. Dis. 2020, 71, 844–846. [Google Scholar] [CrossRef]
- Yin, M.; Zhang, L.; Deng, G.; Han, C.; Shen, M.; Sun, H.; Zeng, F.; Zhang, W.; Chen, L.; Luo, Q.; et al. Severe acute respirato-ry syndrome coronavirus 2 (SARS-CoV-2) infection during pregnancy in China: A retrospective cohort study (Preprint). MedRxiv 2020. [Google Scholar] [CrossRef]
- Yu, N.; Li, W.; Kang, Q.; Xiong, Z.; Wang, S.; Lin, X.; Liu, Y.; Xiao, J.; Liu, H.; Deng, D.; et al. Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: A retrospective, single-centre, descriptive study. Lancet Infect. Dis. 2020, 20, 559–564. [Google Scholar] [CrossRef]
- Zambrano, L.I.; Barahona, F.I.C.; Torres, B.D.A.; Bustillo, C.; Gonzales, G.; Chinchilla, V.G.; Martínez, S.F.E.; Reconco, V.J.A.; Sierra, M.; Aldana, B.D.K.; et al. A pregnant woman with COVID-19 in Central America. Travel Med. Infect. Dis. 2020, 36, 1639. [Google Scholar] [CrossRef]
- Zeng, H.; Xu, C.; Fan, J.; Tang, Y.; Deng, Q.; Zhang, W.; Long, X. Antibodies in Infants Born to Mothers with COVID-19 Pneumonia. JAMA 2020, 323, 1848–1849. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Wang, L.; Fang, C.; Peng, S.; Zhang, L.; Chang, G.; Xia, S.; Zhou, W. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl. Pediatr. 2020, 9, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Di Guardo, F.; Di Grazia, F.M.; Di Gregorio, L.M.; Zambrotta, E.; Carrara, G.; Gulino, F.A.; Tuscano, A.; Palumbo, M. Poor maternal–neonatal outcomes in pregnant patients with confirmed SARS-Cov-2 infection: Analysis of 145 cases. Arch. Gynecol. Obstet. 2021, 1–6. [Google Scholar] [CrossRef]
- Badr, D.A.; Mattern, J.; Carlin, A.; Cordier, A.G.; Maillart, E.; El Hachem, L.; El Kenz, H.; Andronikof, M.; De Bels, D.; Damoisel, C.; et al. Are clinical outcomes worse for pregnant women at ≥20 weeks’ gestation infected with coronavirus disease 2019? A multicenter case-control study with propensity score matching. Am. J. Obstet. Gynecol. 2020, 223, 764–768. [Google Scholar] [CrossRef] [PubMed]
- Allotey, J.; Stallings, E.; Bonet, M.; Yap, M.; Chatterjee, S.; Kew, T.; Debenham, L.; Llavall, A.C.; Dixit, A.; Zhou, D.; et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: Living systematic review and meta-analysis. BMJ 2020, 370, 3320. [Google Scholar] [CrossRef] [PubMed]
- Burwick, R.M.; Yawetz, S.; Stephenson, K.E.; Collier, A.R.Y.; Sen, P.; Blackburn, B.G.; Kojic, E.M.; Hirshberg, A.; Suarez, J.F.; Sobieszczyk, M.E.; et al. Compassionate Use of Remdesivir in Pregnant Women with Severe Coronavirus Disease. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Kang, S.; Tian, R.; Zhang, X.; Wang, Y. Imaging manifestations and diagnostic value of chest CT of coronavirus disease 2019 (COVID-19) in the Xiaogan area. Clin. Radiol. 2020, 75, 341–347. [Google Scholar] [CrossRef]
- Hu, Z.; Song, C.; Xu, C.; Jin, G.; Chen, Y.; Xu, X.; Ma, H.; Chen, W.; Lin, Y.; Zheng, Y.; et al. Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Sci. China Life Sci. 2020, 63, 706–711. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, Y.; Liu, L.; Wang, X.; Luo, N.; Li, L. Clinical Outcomes in 55 Patients with Severe Acute Respiratory Syndrome Coronavirus 2 Who Were Asymptomatic at Hospital Admission in Shenzhen, China. J. Infect. Dis. 2020, 221, 1770–1774. [Google Scholar] [CrossRef]
- Inchingolo, R.; Smargiassi, A.; Moro, F.; Buonsenso, D.; Salvi, S.; Del Giacomo, P.; Scoppettuolo, G.; Demi, L.; Soldati, G.; Testa, A.C. The diagnosis of pneumonia in a pregnant woman with coronavirus disease 2019 using maternal lung ultrasound. Am. J. Obstet. Gynecol. 2020, 223, 9–11. [Google Scholar] [CrossRef]
- Poon, L.C.; Abramowicz, J.S.; Asta, D.A.; Sande, R.; Haar, G.; Maršal, K.; Brezinka, C.; Miloro, P.; Basseal, J.; Westerway, S.C.; et al. ISUOG Safety Committee Position Statement on safe performance of obstetric and gynecological scans and equipment cleaning in context of COVID. Ultrasound Obstet. Gynecol. 2020, 55, 709–712. [Google Scholar] [CrossRef] [PubMed]
- Nouvenne, A.; Zani, M.D.; Milanese, G.; Parise, A.; Baciarello, M.; Bignami, E.G.; Odone, A.; Sverzellati, N.; Meschi, T.; Ticinesi, A. Lung Ultrasound in COVID-19 Pneumonia: Correlations with Chest CT on Hospital admission. Respiration 2020, 99, 617–624. [Google Scholar] [CrossRef]
- Falgarone, G.; Pamoukdjian, F.; Cailhol, J.; Auregan, G.A.; Guis, S.; Bousquet, G.; Bouchaud, O.; Seror, O. Lung ultrasound is a reliable diagnostic technique to predict abnormal CT chest scan and to detect oxygen requirements in COVID-19 pneumonia. Aging 2020, 12, 19945–19953. [Google Scholar] [CrossRef]
- Yassa, M.; Birol, P.; Mutlu, A.M.; Tekin, A.B.; Sandal, K.; Tug, N. Lung Ultrasound Can Influence the Clinical Treatment of Pregnant Women with COVID. J. Ultrasound Med. 2021, 40, 191–203. [Google Scholar] [CrossRef]
- Maraschini, A.; Corsi, E.; Salvatore, M.A.; Donati, S. ItOSS COVID-19 Working Group. Coronavirus and birth in Italy: Results of a national population-based cohort study. Ann. Ist. Super. Sanita 2020, 56, 378–389. [Google Scholar] [CrossRef]
- Della Gatta, A.N.; Rizzo, R.; Pilu, G.; Simonazzi, G. Coronavirus disease 2019 during pregnancy: A systematic review of reported cases. Am. J. Obstet. Gynecol. 2020, 223, 36–41. [Google Scholar] [CrossRef]
- Knight, M.; Bunch, K.; Vousden, N.; Morris, E.; Simpson, N.; Gale, C.; Brien, O.P.; Quigley, M.; Brocklehurst, P.; Kurinczuk, J.J. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: National population based cohort study. BMJ 2020, 369, 2107. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Collaborating Centre for Women’s Health University of Birmingham. COVID-19 in Pregnancy (PregCOV-19 LRS). Available online: www.birmingham.ac.uk/research/whocollaborating-centre/pregcov/index.aspx (accessed on 2 January 2021).
- Oncel, M.Y.; Akın, I.M.; Kanburoglu, M.K.; Tayman, C.; Coskun, S.; Narter, F.; Er, I.; Oncan, T.G.; Memisoglu, A.; Centinkaya, M.; et al. A multicenter study on epidemiological and clinical characteristics of 125 newborns born to women infected with COVID-19 by Turkish Neonatal Society. Eur. J. Pediatr. 2021, 180, 743–744. [Google Scholar] [CrossRef]
- Yang, Z.; Liu, Y. Vertical Transmission of Severe Acute Respiratory Syndrome Coronavirus 2: A Systematic Review. Am. J. Perinatol. 2020, 37, 1055–1060. [Google Scholar] [CrossRef]
- Chen, M.M.; Coakley, F.V.; Kaimal, A.; Laros, R.K. Guidelines for Computed Tomography and Magnetic Resonance Imaging Use During Pregnancy and Lactation. Obstet. Gynecol. 2008, 112, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Youssef, A.; Serra, C.; Pilu, G. Lung ultrasound in the coronavirus disease 2019 pandemic: A practical guide for obstetricians and gynecologists. Am. J. Obstet. Gynecol. 2020, 223, 128–131. [Google Scholar] [CrossRef]
- Demi, L.; Demi, M.; Smargiassi, A.; Inchingolo, R.; Faita, F.; Soldati, G.; Task Force Group. Ultrasonography in lung pathologies: New perspectives. Multidiscip. Respir. Med. 2014, 9, 27. [Google Scholar] [CrossRef] [PubMed]
- Smargiassi, A.; Inchingolo, R.; Soldati, G.; Copetti, R.; Marchetti, G.; Zanforlin, A.; Giannuzzi, R.; Testa, A.; Nardini, S.; Valente, S. The role of chest ultrasonography in the management of respiratory diseases: Document II. Multidiscip. Respir. Med. 2013, 8, 55. [Google Scholar] [CrossRef] [PubMed]
- Soldati, G.; Demi, M.; Smargiassi, A.; Inchingolo, R.; Demi, L. The role of ultrasound lung artifacts in the diagnosis of respiratory diseases. Expert Rev. Respir. Med. 2019, 13, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Schnettler, W.T.; Al Ahwel, Y.; Suhag, A. Severe acute respiratory distress syndrome in coronavirus disease 2019–infected pregnancy: Obstetric and intensive care considerations. Am. J. Obstet. Gynecol. MFM 2020, 2, 120. [Google Scholar] [CrossRef] [PubMed]
- Soldati, G.; Smargiassi, A.; Inchingolo, R.; Buonsenso, D.; Perrone, T.; Briganti, D.F.; Perlini, S.; Torri, E.; Mariani, A.; Mossolani, E.E.; et al. Is There a Role for Lung Ultrasound During the COVID -19 Pandemic? J. Ultrasound Med. 2020, 39, 1459–1462. [Google Scholar] [CrossRef] [PubMed]
- Buonsenso, D.; Piano, A.; Raffaelli, F.; Bonadia, N.; de Gaetano Donati, K.; Franceschi, F. Point-of-Care Lung Ultrasound find-ings in novel coronavirus disease-19 pneumoniae: A case report and potential applications during COVID-19 outbreak. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 2776–2780. [Google Scholar] [CrossRef]
- Kalafat, E.; Yaprak, E.; Cinar, G.; Varli, B.; Ozisik, S.; Uzun, C.; Azap, A.; Koc, A. Lung ultrasound and computed tomographic findings in pregnant woman with COVID. Ultrasound Obstet. Gynecol. 2020, 55, 835–837. [Google Scholar] [CrossRef] [PubMed]

| PATIENT CHARACTERISTICS (N = 30) | DESCRIPTIVE ANALYSIS Median (Range) |
|---|---|
| AGE (years) | 33.5 (27–35) |
| BMI | 27 (23–29) |
| GESTATIONAL AGE AT TEST POSITIVITY (weeks) | 36 (28–38) |
| PARTIAL SATURATION OF OXYGEN (SpO2)%) | 97.5 (96–99) |
| D-DIMER VALUE (µg/mL) | 2320 (2070–3489) |
| LUS SCORE | 3 (0–8) |
| CT SCORE | 4 (2–7.5) |
| GESTATIONAL AGE AT DELIVERY (weeks) | 38 (37–39) |
| MODE OF DELIVERY Vaginal Delivery Cesarean Section | N. % 18 (60) 12 (40) |
| LUS SCORE (N) | NO CLINICAL SYMPTOMS N (%) | COUGH N (%) | FEVER N (%) | WEAKNESS N (%) | DYSPNOEA N (%) | LENGTH of HOSPITALIZATION Mean (SD) |
|---|---|---|---|---|---|---|
| ≤ 6 (22) | 14 (63.6) | 3 (13.6) | 2 (9.1) | 5 (22.7) | 0 | 6.7 (±2.3) |
| >7 and <20 (5) | 0 | 5 (100) | 3 (60) | 2 (40) | 0 | 10 (±2) |
| ≥20 (3) | 0 | 3 (100) | 3 (100) | 3 (100) | 2 (66.7) | 17.6 (±2.5) |
| Patient ID | LUS SCORE | TC SCORE |
|---|---|---|
| 1 | 23 | 16 |
| 2 | 20 | 7 |
| 3 | 10 | 3 |
| 4 | 10 | 3 |
| 5 | 12 | 5 |
| 6 | 10 | 4 |
| 7 | 22 | 8 |
| 8 | 8 | 1 |
| 9 | 6 | 1 |
| LUS SCORE | CORRELATIONS | Coefficient | p-Value |
| SpO2 | −0.499 | <0.01 | |
| Mode of delivery | 0.225 | 0.81 | |
| GA at birth | −0.652 | <0.01 | |
| CT score | 0.888 | <0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Porpora, M.G.; Merlino, L.; Masciullo, L.; D’Alisa, R.; Brandolino, G.; Galli, C.; De Luca, C.; Pecorini, F.; Fonsi, G.B.; Mingoli, A.; et al. Does Lung Ultrasound Have a Role in the Clinical Management of Pregnant Women with SARS COV2 Infection? Int. J. Environ. Res. Public Health 2021, 18, 2762. https://doi.org/10.3390/ijerph18052762
Porpora MG, Merlino L, Masciullo L, D’Alisa R, Brandolino G, Galli C, De Luca C, Pecorini F, Fonsi GB, Mingoli A, et al. Does Lung Ultrasound Have a Role in the Clinical Management of Pregnant Women with SARS COV2 Infection? International Journal of Environmental Research and Public Health. 2021; 18(5):2762. https://doi.org/10.3390/ijerph18052762
Chicago/Turabian StylePorpora, Maria Grazia, Lucia Merlino, Luisa Masciullo, Rossella D’Alisa, Gabriella Brandolino, Cecilia Galli, Casimiro De Luca, Francesco Pecorini, Giovanni Battista Fonsi, Andrea Mingoli, and et al. 2021. "Does Lung Ultrasound Have a Role in the Clinical Management of Pregnant Women with SARS COV2 Infection?" International Journal of Environmental Research and Public Health 18, no. 5: 2762. https://doi.org/10.3390/ijerph18052762
APA StylePorpora, M. G., Merlino, L., Masciullo, L., D’Alisa, R., Brandolino, G., Galli, C., De Luca, C., Pecorini, F., Fonsi, G. B., Mingoli, A., Franchi, C., Oliva, A., Manganaro, L., Mastroianni, C. M., & Piccioni, M. G. (2021). Does Lung Ultrasound Have a Role in the Clinical Management of Pregnant Women with SARS COV2 Infection? International Journal of Environmental Research and Public Health, 18(5), 2762. https://doi.org/10.3390/ijerph18052762










