Changes in Six-Month Prevalence of Circulatory System Diseases among People Aged 20 Years and Older between 2013 and 2018 in Hunan, China
Abstract
1. Introduction
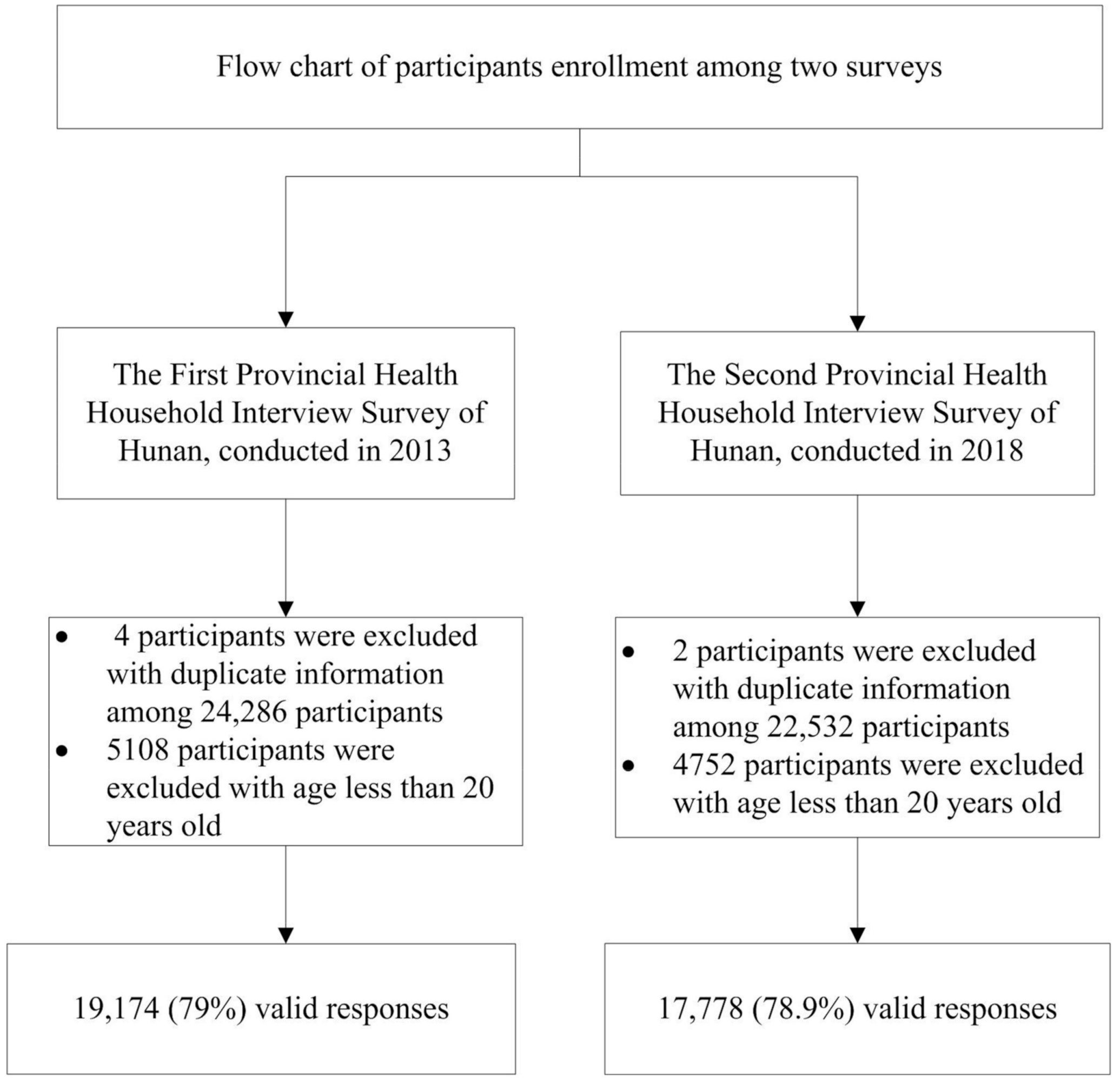
2. Materials and Methods
2.1. Data Source
2.2. Operational Definition of CSD Event
2.3. Socio-Demographic Variables
2.4. Statistical Analysis
2.5. Ethical Approval
3. Results
3.1. Characteristics of Survey Participants
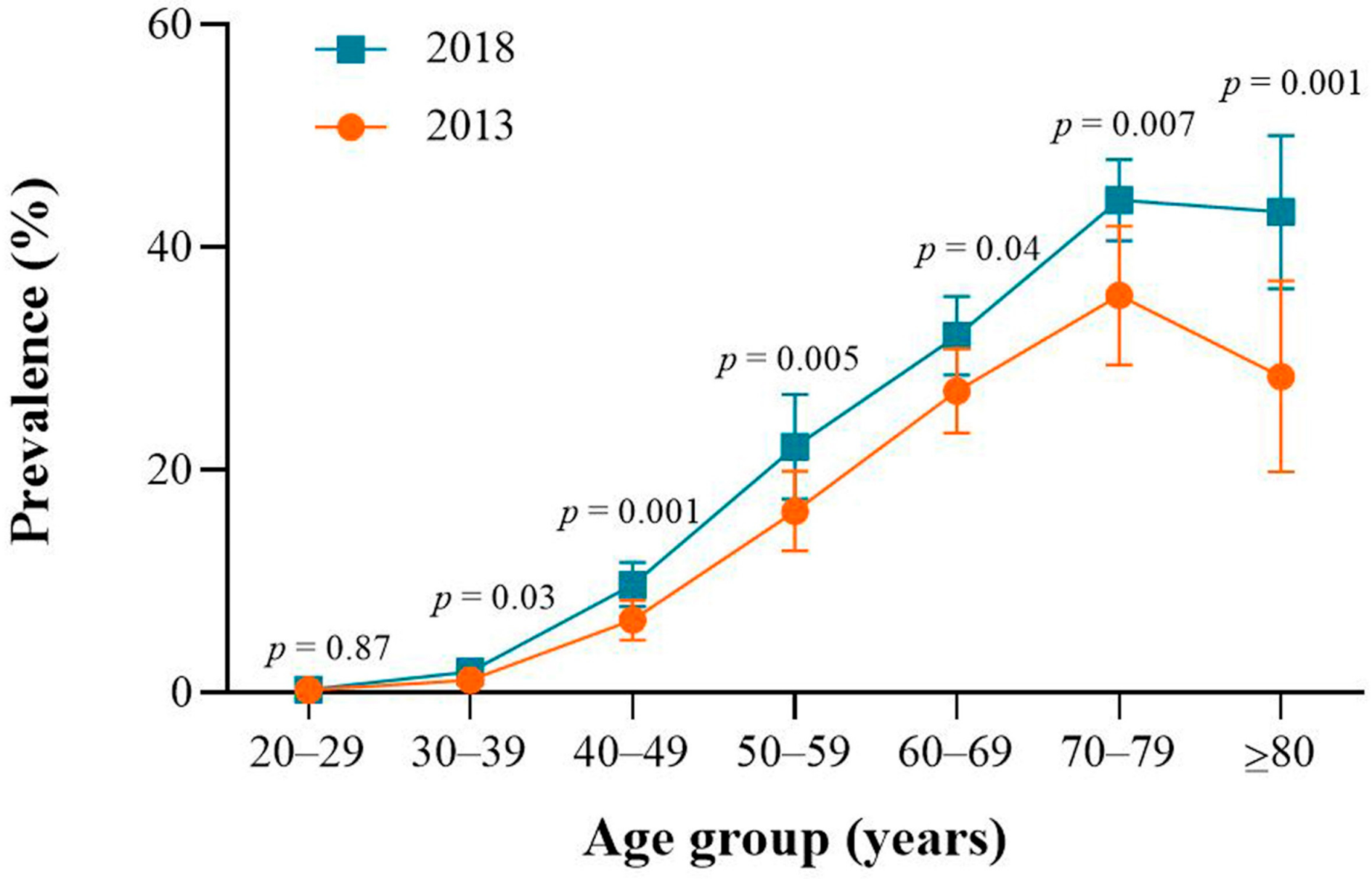
3.2. Six-Month CSD Prevalence Rate between 2013 and 2018
3.3. Six-Month CSD Prevalence Rate between 2013 and 2018
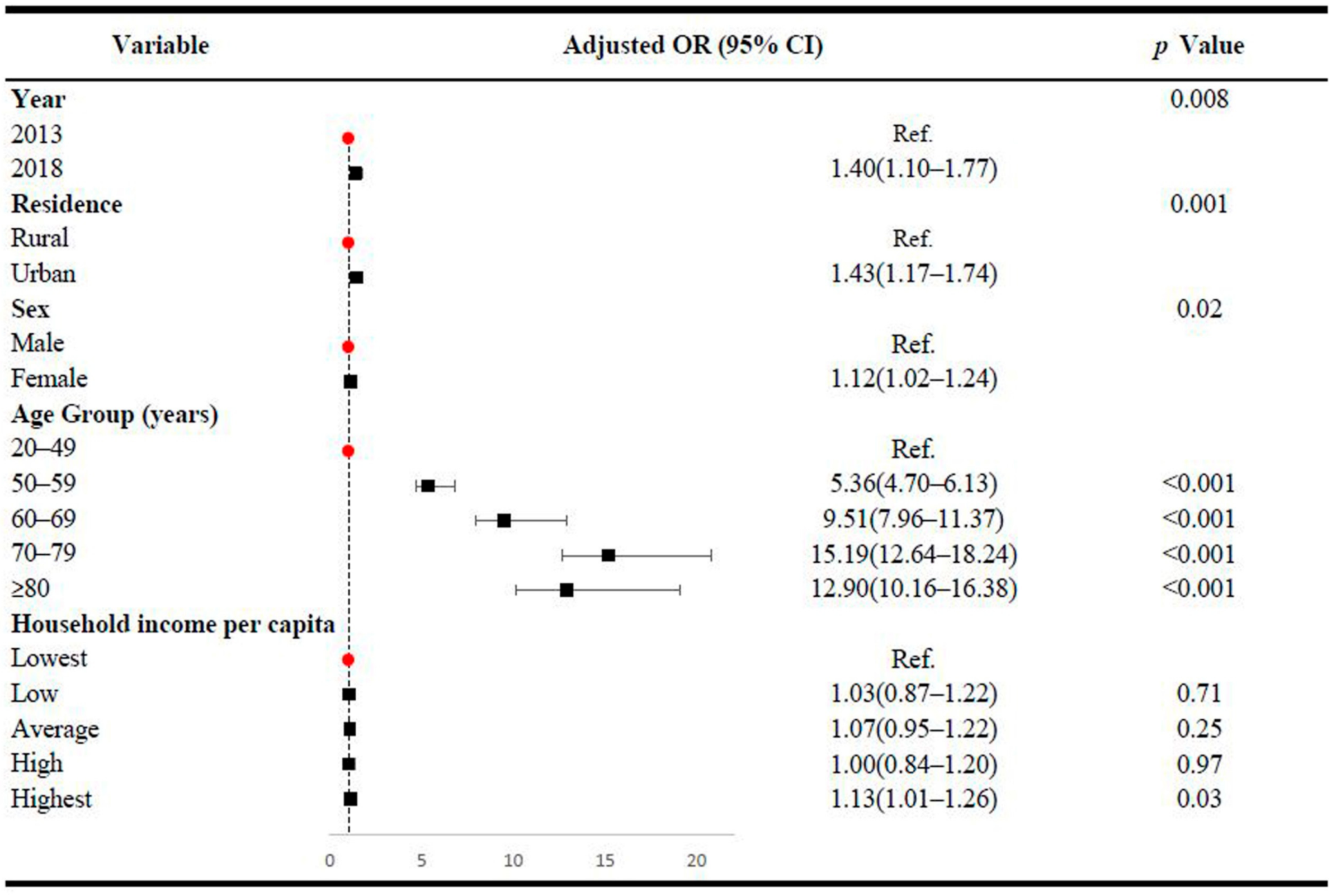
3.4. Associations between the 6-Month CSD Prevalence and Socio-Demographic Variables
4. Discussion
4.1. Primary Findings
4.2. Interpretation of the Findings
4.3. Policy Implications
4.4. Limitations of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liu, S.; Li, Y.; Zeng, X.; Wang, H.; Yin, P.; Wang, L.; Liu, Y.; Liu, J.; Qi, J.; Ran, S.; et al. Burden of Cardiovascular Diseases in China, 1990–2016: Findings From the 2016 Global Burden of Disease Study. JAMA Cardiol. 2019, 4, 342–352. [Google Scholar] [CrossRef]
- Ma, L.Y.; Chen, W.W.; Gao, R.L.; Liu, L.S.; Zhu, M.L.; Wang, Y.J.; Wu, Z.S.; Li, H.J.; Gu, D.F.; Yang, Y.J.; et al. China cardiovascular diseases report 2018: An updated summary. J. Geriatr. Cardiol. 2020, 17, 1–8. [Google Scholar] [CrossRef]
- Moran, A.; Gu, D.; Zhao, D.; Coxson, P.; Wang, Y.C.; Chen, C.-S.; Liu, J.; Cheng, J.; Bibbins-Domingo, K.; Shen, Y.-M.; et al. Future Cardiovascular Disease in China. Circ. Cardiovasc. Qual. Outcomes 2010, 3, 243–252. [Google Scholar] [CrossRef]
- Yang, Z.J.; Liu, J.; Ge, J.P.; Chen, L.; Zhao, Z.G.; Yang, W.Y. Prevalence of cardiovascular disease risk factor in the Chinese population: The 2007–2008 China National Diabetes and Metabolic Disorders Study. Eur. Heart J. 2012, 33, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Gu, D.; Gupta, A.; Muntner, P.; Hu, S.; Duan, X.; Chen, J.; Reynolds, R.F.; Whelton, P.K.; He, J. Prevalence of cardiovascular disease risk factor clustering among the adult population of China: Results from the International Collaborative Study of Cardiovascular Disease in Asia (InterAsia). Circulation 2005, 112, 658–665. [Google Scholar] [CrossRef]
- People’s Republic of China–United States Cardiovascular and Cardiopulmonary Epidemiology Research Group. An epidemiological study of cardiovascular and cardiopulmonary disease risk factors in four populations in the People’s Republic of China. Baseline report from the P.R.C.-U.S.A. Collaborative Study. Circulation 1992, 85, 1083–1096. [Google Scholar] [CrossRef]
- Wu, Z.; Yao, C.; Zhao, D.; Wu, G.; Wang, W.; Liu, J.; Zeng, Z.; Wu, Y. Sino-MONICA Project. Circulation 2001, 103, 462–468. [Google Scholar] [CrossRef]
- Li, W.; Gu, H.; Teo, K.K.; Bo, J.; Wang, Y.; Yang, J.; Wang, X.; Zhang, H.; Sun, Y.; Jia, X.; et al. Hypertension prevalence, awareness, treatment, and control in 115 rural and urban communities involving 47 000 people from China. J. Hypertens. 2016, 34, 39–46. [Google Scholar] [CrossRef]
- Wang, W.; Jiang, B.; Sun, H.; Ru, X.; Sun, D.; Wang, L.; Wang, L.; Jiang, Y.; Li, Y.; Wang, Y.; et al. Prevalence, Incidence, and Mortality of Stroke in China: Results from a Nationwide Population-Based Survey of 480 687 Adults. Circulation 2017, 135, 759–771. [Google Scholar] [CrossRef]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Ning, P.; Cai, M.; Cheng, P.; Zhang, Y.; Schwebel, D.C.; Yang, Y.; Zhang, W.; Cheng, X.; Gao, Y.; Ling, X.; et al. Trends in injury morbidity in China, 1993–2013: A longitudinal analysis of population-based survey data. Accid. Anal. Prev. 2018, 113, 179–186. [Google Scholar] [CrossRef]
- People’s Government of Hunan Province. Available online: http://www.hunan.gov.cn/hnszf/zfsj/tjgb/201903/t20190313_5294248.html (accessed on 26 February 2021).
- Qin, H.; Zhang, L.; Zhang, L.; Zhang, W.; Li, L.; Deng, X.; Tian, D.; Deng, J.; Hu, G. Prevalence of Breastfeeding: Findings from the First Health Service Household Interview in Hunan Province, China. Int. J. Environ. Res. Public Health 2017, 14, 150. [Google Scholar] [CrossRef]
- Hua, J.; Zhang, L.; Gao, D.; Huang, Y.; Ning, P.; Cheng, P.; Li, Y.; Hu, G. Prevalence of Overweight and Obesity among People Aged 18 Years and Over between 2013 and 2018 in Hunan, China. Int. J. Environ. Res. Public Health 2020, 17, 4048. [Google Scholar] [CrossRef]
- National Health Commission of the People’s Republic of China. Classification of Diseases in the Sixth National Health Service Survey Table. Available online: http://www.nhc.gov.cn/ewebeditor/uploadfile/2018/10/20181011143139169.pdf (accessed on 9 December 2020).
- ICD-10 Version: 2019. Available online: https://icd.who.int/browse10/2019/en (accessed on 26 February 2021).
- Zhao, D.; Liu, J.; Wang, M.; Zhang, X.; Zhou, M. Epidemiology of cardiovascular disease in China: Current features and implications. Nat. Rev. Cardiol. 2019, 16, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Du, X.; Patel, A.; Anderson, C.S.; Dong, J.; Ma, C. Epidemiology of Cardiovascular Disease in China and Opportunities for Improvement: JACC International. J. Am. Coll. Cardiol. 2019, 73, 3135–3147. [Google Scholar] [CrossRef]
- Deng, X.; Dong, P.; Zhang, L.; Tian, D.; Zhang, L.; Zhang, W.; Li, L.; Deng, J.; Ning, P.; Hu, G. Health-related quality of life in residents aged 18 years and older with and without disease: Findings from the First Provincial Health Services Survey of Hunan, China. BMJ Open 2017, 7, e015880. [Google Scholar] [CrossRef]
- Tian, D.; Sun, L.; Zhang, L.; Zhang, L.; Zhang, W.; Li, L.; Deng, X.; Ning, P.; Cheng, X.; Deng, J.; et al. Large urban–rural disparity in the severity of two-week illness: Updated results based on the first health service survey of Hunan Province, China. Int. J. Equity Health 2016, 15, 37. [Google Scholar] [CrossRef]
- Institute for Health Metrics and Evaluation (IHME). GBD Results Tool. 2019. Available online: http://ghdx.healthdata.org/gbd-results-tool (accessed on 20 December 2020).
- National Health Commission of the People’s Republic of China. The Nutrition and Health Status of the Chinese People (2015 Report). Available online: http://www.nhc.gov.cn/jkj/s5879/201506/4505528e65f3460fb88685081ff158a2.shtml (accessed on 20 December 2020).
- National Health Commission of the People’s Republic of China. The Nutrition and Health Status of the Chinese People (2020 Report). Available online: http://www.gov.cn/xinwen/2020-12/24/content_5572983.htm (accessed on 20 December 2020).
- Chen, Y.; Peng, Q.; Yang, Y.; Zheng, S.; Wang, Y.; Lu, W. The prevalence and increasing trends of overweight, general obesity, and abdominal obesity among Chinese adults: A repeated cross-sectional study. BMC Public Health 2019, 19, 1293. [Google Scholar] [CrossRef]
- World Health Organization. China Adult Tobacco Survey 2018. Available online: https://www.who.int/docs/default-source/wpro---documents/countries/china/2018-gats-china-factsheet-cn-en.pdf?sfvrsn=3f4e2da9_2 (accessed on 21 December 2020).
- Chinese Center for Disease Control and Prevention. Report on Adult Tobacco in China. Available online: http://www.tcrc.org.cn/html/xwzx/1294.html (accessed on 21 December 2020).
- Center for Health Statistics and Information. An Analysis Report of National Health Services Survey in China. 2013. Available online: http://www.nhc.gov.cn/ewebeditor/uploadfile/2016/10/20161026163512679.pdf (accessed on 21 December 2020).
- Zhang, L.; Zhang, W.; Zhang, L.; Tian, D.; Li, L.; Deng, X.; Deng, J.; Ning, P.; Hu, G. Associations of Undergoing a Routine Medical Examination or Not with Prevalence Rates of Hypertension and Diabetes Mellitus: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2016, 13, 628. [Google Scholar] [CrossRef]
- Liu, K.; Hsieh, C.; Zhuang, N.; Gao, Y.; Li, Z.; Ren, X.; Yang, L.; Zhang, J.; Budoff, M.J.; Lu, B. Current utilization of cardiac computed tomography in mainland China: A national survey. J. Cardiovasc. Comput. Tomogr. 2016, 10, 76–81. [Google Scholar] [CrossRef]
- Li, X.; Wu, C.; Lu, J.; Chen, B.; Li, Y.; Yang, Y.; Hu, S.; Li, J. Cardiovascular risk factors in China: A nationwide population-based cohort study. Lancet Public Health 2020, 5, e672–e681. [Google Scholar] [CrossRef]
- Tian, Y.; Jiang, C.; Wang, M.; Cai, R.; Zhang, Y.; He, Z.; Wang, H.; Wu, D.; Wang, F.; Liu, X.; et al. BMI, leisure-time physical activity, and physical fitness in adults in China: Results from a series of national surveys, 2000–2014. Lancet Diabetes Endocrinol. 2016, 4, 487–497. [Google Scholar] [CrossRef]
- Ng, S.W.; Howard, A.-G.; Wang, H.J.; Su, C.; Zhang, B. The physical activity transition among adults in China: 1991–2011. Obes. Rev. 2014, 15, 27–36. [Google Scholar] [CrossRef]
- Cao, Y.; Chai, L. Drivers of the Growing Water, Carbon and Ecological Footprints of the Chinese Diet from 1961 to 2017. Int. J. Environ. Res. Public Health 2020, 17, 1803. [Google Scholar] [CrossRef] [PubMed]
- Muntner, P.; Gu, D.; Wildman, R.P.; Chen, J.; Qan, W.; Whelton, P.K.; He, J. Prevalence of physical activity among Chinese adults: Results from the International Collaborative Study of Cardiovascular Disease in Asia. Am. J. Public Health 2005, 95, 1631–1636. [Google Scholar] [CrossRef] [PubMed]
- Ding, C.; Feng, G.; Yuan, F.; Gong, W.; Yao, Y.; Ma, Y.; Zhang, Y.; Liu, A. Temporal Trends and Recent Correlates in Sedentary Behaviors among Chinese Adults from 2002 to 2010–2012. Int. J. Environ. Res. Public Health 2020, 17, 158. [Google Scholar] [CrossRef]
- Gong, P.; Liang, S.; Carlton, E.J.; Jiang, Q.; Wu, J.; Wang, L.; Remais, J.V. Urbanisation and health in China. Lancet 2012, 379, 843–852. [Google Scholar] [CrossRef]
- Bennett, D.A.; Du, H.; Clarke, R.; Guo, Y.; Yang, L.; Bian, Z.; Chen, Y.; Millwood, I.; Yu, C.; He, P.; et al. Association of Physical Activity With Risk of Major Cardiovascular Diseases in Chinese Men and Women. JAMA Cardiol. 2017, 2, 1349–1358. [Google Scholar] [CrossRef]
- Van de Poel, E.; O’Donnell, O.; Van Doorslaer, E. Is there a health penalty of China’s rapid urbanization? Health Econ. 2012, 21, 367–385. [Google Scholar] [CrossRef]
- Liu, M.; Zhang, Q.; Lu, M.; Kwon, C.S.; Quan, H. Rural and urban disparity in health services utilization in China. Med. Care 2007, 45, 767–774. [Google Scholar] [CrossRef]
- Jian, W.; Chan, K.Y.; Reidpath, D.D.; Xu, L. China’s Rural-Urban Care Gap Shrank for Chronic Disease Patients, But Inequities Persist. Health Aff. 2010, 29, 2189–2196. [Google Scholar] [CrossRef] [PubMed]
- Nanayakkara, S.; Marwick, T.H.; Kaye, D.M. The ageing heart: The systemic and coronary circulation. Heart 2018, 104, 370–376. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | 2013 | 2018 | p Value | ||
|---|---|---|---|---|---|
| Number | Percentage (95%) | Number | Percentage (95%) | ||
| All participants | 19,174 | 100.00 | 17,778 | 100.00 | |
| Residence | |||||
| Urban | 9816 | 23.48 (4.57–42.40) | 9103 | 30.61 (6.27–54.95) | 0.70 |
| Rural | 9358 | 76.52 (57.61–95.43) | 8675 | 69.39 (45.05–93.73) | |
| Sex | |||||
| Male | 9390 | 48.94 (48.19–49.69) | 8642 | 48.10 (47.21–49.00) | 0.13 |
| Female | 9784 | 51.06 (50.31–51.81) | 9136 | 51.90 (51.00–52.79) | |
| Age group (years) | <0.001 | ||||
| 20–29 | 2235 | 12.19 (10.14–14.23) | 1455 | 7.42 (6.68–8.16) | |
| 30–39 | 2516 | 12.34 (10.88–13.79) | 2295 | 11.48 (9.51–13.44) | |
| 40–49 | 4387 | 23.49 (21.54–25.45) | 3295 | 17.95 (17.25–18.65) | |
| 50–59 | 4153 | 21.73 (18.78–24.69) | 4401 | 26.01 (24.14–27.88) | |
| 60–69 | 3571 | 18.07 (15.96–20.18) | 3891 | 23.41 (21.76–25.06) | |
| 70–79 | 1745 | 9.05 (7.16–10.94) | 1901 | 10.04 (8.77–11.31) | |
| ≥80 | 567 | 3.13 (2.40–3.86) | 540 | 3.69 (2.48–4.90) | |
| Education | |||||
| College or above | 1952 | 11.74 (8.86–14.61) | 1509 | 8.59 (6.25–10.93) | 0.60 |
| Technical School | 5602 | 32.01 (26.12–37.90) | 5321 | 30.18 (24.23–36.13) | |
| Senior High school | 6386 | 33.58 (31.14–36.03) | 5923 | 32.95 (31.54–34.36) | |
| Junior High School | 2475 | 10.84 (7.86–13.82) | 2289 | 13.47 (10.14–16.80) | |
| Elementary | 911 | 4.36 (2.82–5.91) | 930 | 5.09 (3.59–6.59) | |
| Illiteracy | 1848 | 7.47 (3.46–11.48) | 1806 | 9.72 (5.46–13.97) | |
| Marital status | 0.001 | ||||
| Single | 1376 | 7.01 (5.81–8.20) | 948 | 5.09 (4.19–5.99) | |
| Married | 16,121 | 84.20 (82.49–85.90) | 15,214 | 84.71 (82.70–86.72) | |
| Widowed | 1376 | 7.51 (6.49–8.52) | 1291 | 8.16 (6.74–9.59) | |
| Divorced | 283 | 1.22 (0.84–1.60) | 305 | 1.84 (1.38–2.31) | |
| Average income per capita a | 0.008 | ||||
| Lowest | 3756 | 15.70 (12.08–19.32) | 3614 | 17.26 (15.07–19.45) | |
| Low | 2736 | 11.91 (10.12–13.70) | 3592 | 17.69 (14.30–21.07) | |
| Average | 4284 | 22.87 (19.68–26.06) | 4029 | 23.26 (20.51–26.02) | |
| High | 3499 | 16.86 (13.77–19.95) | 3020 | 16.49 (14.09–18.88) | |
| Highest | 4845 | 32.67 (26.65–38.68) | 3508 | 25.30 (20.01–30.60) | |
| Variable | 2013 | 2018 | Crude OR | Adjusted OR a | ||
|---|---|---|---|---|---|---|
| Number of Cases | Prevalence (95% CI) | Number of Cases | Prevalence (95% CI) | |||
| Overall | 2929 | 14.25 (11.98–16.51) | 3563 | 21.25 (18.86–23.63) | 1.63 (1.28–2.01) ** | 1.59 (1.24–2.04) ** |
| Residence | ||||||
| Urban | 1718 | 17.23 (12.68–21.77) | 1899 | 22.49 (20.88–24.10) | 1.39 (1.00–1.94) * | 1.37 (0.99–1.91) |
| Rural | 1211 | 13.33 (10.73–15.94) | 1664 | 20.70 (17.10–24.30) | 1.70 (1.24–2.32) ** | 1.71 (1.21–2.41) ** |
| Sex | ||||||
| Male | 1358 | 13.87 (10.85–16.90) | 1676 | 20.52 (18.11–22.92) | 1.60 (1.19–2.16) ** | 1.58 (1.13–2.20) ** |
| Female | 1571 | 14.61 (12.84–16.37) | 1887 | 21.92 (19.31–24.54) | 1.64 (1.33–2.03) ** | 1.61 (1.29–2.00) ** |
| Rank | Type of Disease | 2013 | 2018 | ||
|---|---|---|---|---|---|
| Prevalence % | Proportion % | Prevalence % | Proportion % | ||
| 1 | Hypertensive diseases | 12.43 | 87.24 | 17.81 | 83.83 |
| 2 | Cerebrovascular diseases | 0.61 | 4.30 | 1.65 | 7.76 |
| 3 | Other forms of heart disease a | 0.44 | 3.06 | 1.73 | 3.45 |
| 4 | Other types of ischemic heart diseases b | 0.32 | 2.25 | 0.42 | 1.98 |
| 5 | Angina pectoris | 0.09 | 0.62 | 0.08 | 0.39 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rao, Z.; Hua, J.; Li, R.; Fu, Y.; Li, J.; Xiao, W.; He, J.; Hu, G. Changes in Six-Month Prevalence of Circulatory System Diseases among People Aged 20 Years and Older between 2013 and 2018 in Hunan, China. Int. J. Environ. Res. Public Health 2021, 18, 2599. https://doi.org/10.3390/ijerph18052599
Rao Z, Hua J, Li R, Fu Y, Li J, Xiao W, He J, Hu G. Changes in Six-Month Prevalence of Circulatory System Diseases among People Aged 20 Years and Older between 2013 and 2018 in Hunan, China. International Journal of Environmental Research and Public Health. 2021; 18(5):2599. https://doi.org/10.3390/ijerph18052599
Chicago/Turabian StyleRao, Zhenzhen, Junjie Hua, Ruotong Li, Yanhong Fu, Jie Li, Wangxin Xiao, Jieyi He, and Guoqing Hu. 2021. "Changes in Six-Month Prevalence of Circulatory System Diseases among People Aged 20 Years and Older between 2013 and 2018 in Hunan, China" International Journal of Environmental Research and Public Health 18, no. 5: 2599. https://doi.org/10.3390/ijerph18052599
APA StyleRao, Z., Hua, J., Li, R., Fu, Y., Li, J., Xiao, W., He, J., & Hu, G. (2021). Changes in Six-Month Prevalence of Circulatory System Diseases among People Aged 20 Years and Older between 2013 and 2018 in Hunan, China. International Journal of Environmental Research and Public Health, 18(5), 2599. https://doi.org/10.3390/ijerph18052599







