Test–Retest Reliability of an iPhone® Inclinometer Application to Assess the Lumbar Joint Repositioning Error in Non-Specific Chronic Low Back Pain
Abstract
1. Introduction
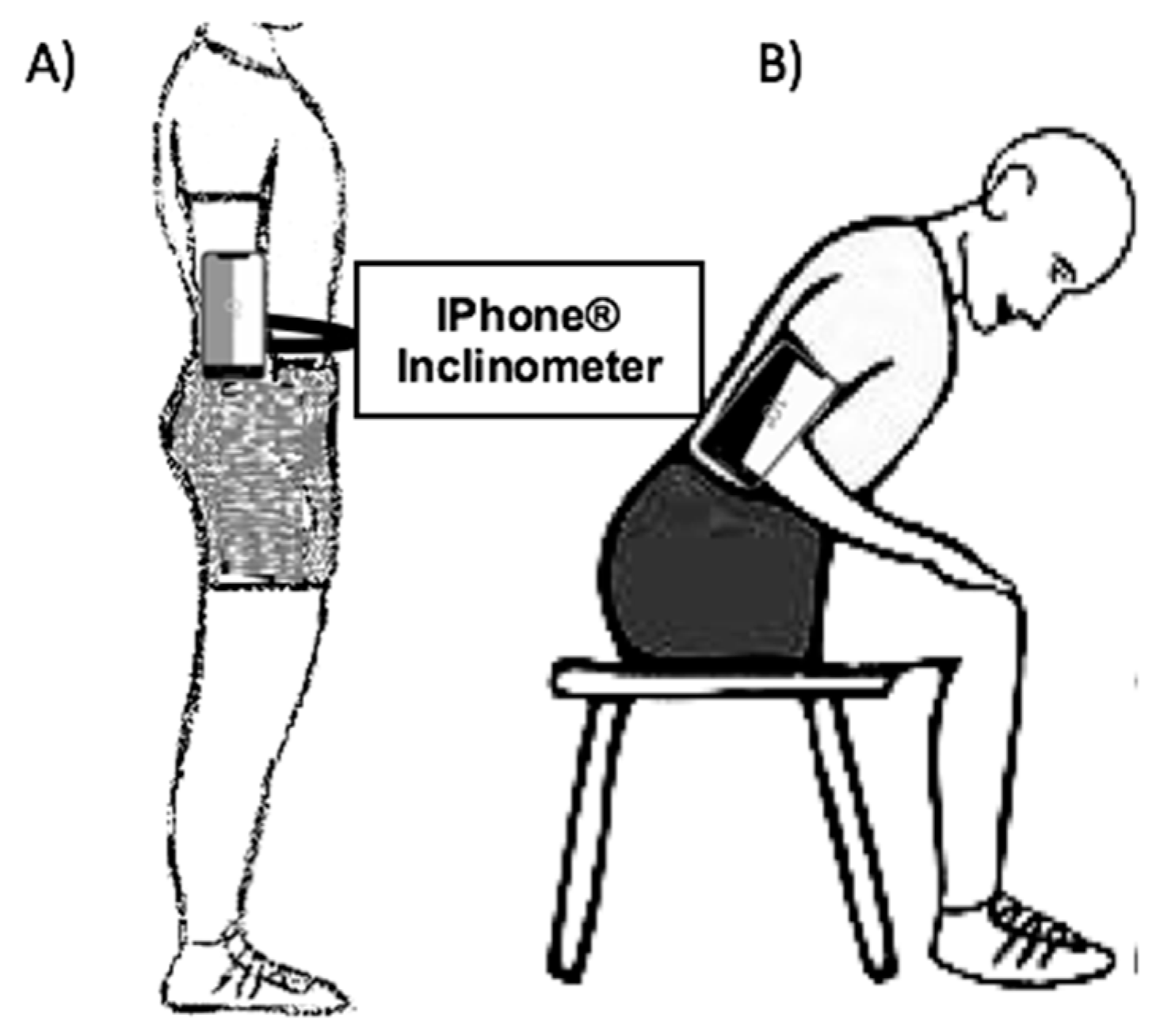
2. Materials and Methods
2.1. Sample Size
2.2. Participants
2.3. Measurements
2.4. Reliability Procedures
2.5. Statistical Analysis
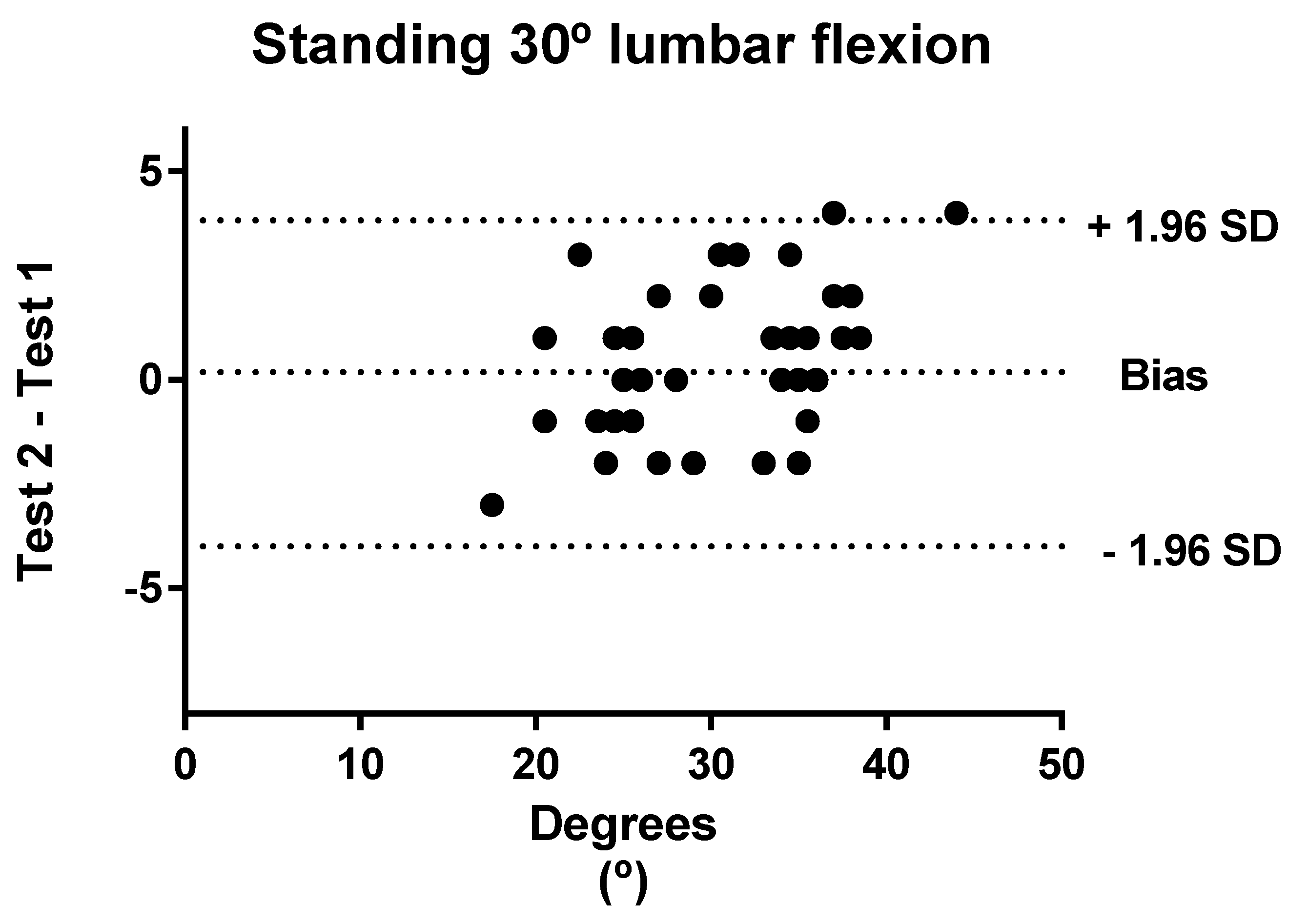
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alsufiany, M.B.; Lohman, E.B.; Daher, N.S.; Gang, G.R.; Shallan, A.I.; Jaber, H.M. Non-specific chronic low back pain and physical activity: A comparison of postural control and hip muscle isometric strength. Medicine 2020, 99, e18544. [Google Scholar] [CrossRef]
- Carragee, E.J.; Alamin, T.F.; Miller, J.L.; Carragee, J.M. Discographic, MRI and psychosocial determinants of low back pain disability and remission: A prospective study in subjects with benign persistent back pain. Spine J. 2005, 5, 24–35. [Google Scholar] [CrossRef] [PubMed]
- La Touche, R.; Grande-Alonso, M.; Arnes-Prieto, P.; Paris-Alemany, A. How Does Self-Efficacy Influence Pain Perception, Postural Stability and Range of Motion in Individuals with Chronic Low Back Pain? Pain Phys. 2019, 22, E1–E13. [Google Scholar] [CrossRef]
- Van Dieën, J.H.; Koppes, L.L.J.; Twisk, J.W.R. Postural sway parameters in seated balancing; their reliability and relationship with balancing performance. Gait Posture 2010, 31, 42–46. [Google Scholar] [CrossRef]
- Brumagne, S.; Cordo, P.; Lysens, R.; Verschueren, S.; Swinnen, S. The role of paraspinal muscle spindles in lumbosacral position sense in individuals with and without low back pain. Spine 2000, 25, 989–994. [Google Scholar] [CrossRef] [PubMed]
- Descarreaux, M.; Blouin, J.-S.; Teasdale, N. Repositioning accuracy and movement parameters in low back pain subjects and healthy control subjects. Eur. Spine J. 2005, 14, 185–191. [Google Scholar] [CrossRef]
- Sung, W.; Abraham, M.; Plastaras, C.; Silfies, S.P. Trunk motor control deficits in acute and subacute low back pain are not associated with pain or fear of movement. Spine J. 2015, 15, 1772–1782. [Google Scholar] [CrossRef]
- Da Silva, R.A.; Vieira, E.R.; Carvalho, C.E.; Oliveira, M.R.; Amorim, C.F.; Neto, E.N. Age-related differences on low back pain and postural control during one-leg stance: A case-control study. Eur. Spine J. 2016, 25, 1251–1257. [Google Scholar] [CrossRef] [PubMed]
- Caña-Pino, A.; Apolo-Arenas, M.D.; Moral-Blanco, J.; De la Cruz-Sánchez, E.; Espejo-Antúnez, L. A novel determination of energy expenditure efficiency during a balance task using accelerometers. A pilot study. Assist. Technol. 2017, 31, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Caffaro, R.R.; França, F.J.R.; Burke, T.N.; Magalhães, M.O.; Ramos, L.A.V.; Marques, A.P. Postural control in individuals with and without non-specific chronic low back pain: A preliminary case-control study. Eur. Spine J. 2014, 23, 807–813. [Google Scholar] [CrossRef][Green Version]
- Hodges, P.W.; Danneels, L. Changes in Structure and Function of the Back Muscles in Low Back Pain: Different Time Points, Observations, and Mechanisms. J. Orthop. Sports Phys. Ther. 2019, 49, 464–476. [Google Scholar] [CrossRef]
- Moseley, G.L.; Hodges, P.W. Are the changes in postural control associated with low back pain caused by pain interference? Clin. J. Pain 2005, 21, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Luomajoki, H.A.; Bonet Beltran, M.B.; Careddu, S.; Bauer, C.M. Effectiveness of movement control exercise on patients with non-specific low back pain and movement control impairment: A systematic review and meta-analysis. Musculoskelet. Sci. Pract. 2018, 36, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Romero-Franco, N.; Jiménez-Reyes, P.; González-Hernández, J.M.; Fernández-Domínguez, J.C. Assessing the concurrent validity and reliability of an iPhone application for the measurement of range of motion and joint position sense in knee and ankle joints of young adults. Phys. Ther. Sport 2020, 44, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Guerraz, M.; Provost, S.; Narison, R.; Brugnon, A.; Virolle, S.; Bresciani, J.-P. Integration of visual and proprioceptive afferents in kinesthesia. Neuroscience 2012, 223, 258–268. [Google Scholar] [CrossRef]
- El-Wishy, A.; Elsayed, E. Effect of Proprioceptive Training Program on Balance in Patients with Diabetic Neuropathy: A controlled randomized study. Bull. Fac. Phys. Ther. 2012, 17, 1–8. [Google Scholar]
- Zheng, Y.-L.; Wang, X.-F.; Chen, B.-L.; Gu, W.; Wang, X.; Xu, B.; Zhang, J.; Wu, Y.; Chen, C.-C.; Liu, X.-C.; et al. Effect of 12-Week Whole-Body Vibration Exercise on Lumbopelvic Proprioception and Pain Control in Young Adults with Nonspecific Low Back Pain. Med. Sci. Monit. 2019, 25, 443–452. [Google Scholar] [CrossRef]
- Claeys, K.; Dankaerts, W.; Janssens, L.; Pijnenburg, M.; Goossens, N.; Brumagne, S. Young individuals with a more ankle-steered proprioceptive control strategy may develop mild non-specific low back pain. J. Electromyogr. Kinesiol. 2015, 25, 329–338. [Google Scholar] [CrossRef]
- Shanbehzadeh, S.; Salavati, M.; Talebian, S.; Khademi-Kalantari, K.; Tavahomi, M. Attention demands of postural control in non-specific chronic low back pain subjects with low and high pain-related anxiety. Exp. Brain Res. 2018, 236, 1927–1938. [Google Scholar] [CrossRef]
- Mann, L.; Kleinpaul, J.F.; Pereira Moro, A.R.; Mota, C.B.; Carpes, F.P. Effect of low back pain on postural stability in younger women: Influence of visual deprivation. J. Bodyw. Mov. Ther. 2010, 14, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Hamacher, D.; Hamacher, D.; Schega, L. A cognitive dual task affects gait variability in patients suffering from chronic low back pain. Exp. Brain Res. 2014, 232, 3509–3513. [Google Scholar] [CrossRef]
- Mok, N.W.; Brauer, S.G.; Hodges, P.W. Hip strategy for balance control in quiet standing is reduced in people with low back pain. Spine 2004, 29, E107–E112. [Google Scholar] [CrossRef] [PubMed]
- Puntumetakul, R.; Chalermsan, R.; Hlaing, S.S.; Tapanya, W.; Saiklang, P.; Boucaut, R. The effect of core stabilization exercise on lumbar joint position sense in patients with subacute non-specific low back pain: A randomized controlled trial. J. Phys. Ther. Sci. 2018, 30, 1390–1395. [Google Scholar] [CrossRef]
- Wang, X.-Q.; Gu, W.; Chen, B.-L.; Wang, X.; Hu, H.-Y.; Zheng, Y.-L.; Zhang, J.; Zhang, H.-Y.; Chen, P.-J. Effects of whole-body vibration exercise for non-specific chronic low back pain: An assessor-blind, randomized controlled trial. Clin. Rehabil. 2019, 33, 1445–1457. [Google Scholar] [CrossRef]
- Kong, Y.-S.; Jang, G.-U.; Park, S. The effects of prone bridge exercise on the Oswestry disability index and proprioception of patients with chronic low back pain. J. Phys. Ther. Sci. 2015, 27, 2749–2752. [Google Scholar] [CrossRef][Green Version]
- Tong, M.H.; Mousavi, S.J.; Kiers, H.; Ferreira, P.; Refshauge, K.; van Dieën, J. Is There a Relationship Between Lumbar Proprioception and Low Back Pain? A Systematic Review with Meta-Analysis. Arch. Phys. Med. Rehabil. 2017, 98, 120–136.e2. [Google Scholar] [CrossRef]
- Bontrup, C.; Taylor, W.R.; Fliesser, M.; Visscher, R.; Green, T.; Wippert, P.-M.; Zemp, R. Low back pain and its relationship with sitting behaviour among sedentary office workers. Appl. Ergon. 2019, 81, 102894. [Google Scholar] [CrossRef]
- Villafañe, J.H.; Zanetti, L.; Isgrò, M.; Cleland, J.A.; Bertozzi, L.; Gobbo, M.; Negrini, S. Methods for the assessment of neuromotor capacity in non-specific low back pain: Validity and applicability in everyday clinical practice. J. Back Musculoskelet. Rehabil. 2015, 28, 201–214. [Google Scholar] [CrossRef]
- Smith, A.; Beales, D.; O’Sullivan, P.; Bear, N.; Straker, L. Low Back Pain with Impact at 17 Years of Age Is Predicted by Early Adolescent Risk Factors From Multiple Domains: Analysis of the Western Australian Pregnancy Cohort (Raine) Study. J. Orthop. Sports Phys. Ther. 2017, 47, 752–762. [Google Scholar] [CrossRef]
- Claus, A.P.; Hides, J.A.; Moseley, G.L.; Hodges, P.W. Is ‘ideal’ sitting posture real?: Measurement of spinal curves in four sitting postures. Man. Ther. 2009, 14, 404–408. [Google Scholar] [CrossRef]
- Saragiotto, B.T.; Maher, C.G.; Yamato, T.P.; Costa, L.O.; Costa, L.C.M.; Ostelo, R.W.; Macedo, L.G. Motor control exercise for chronic non-specific low-back pain. Cochrane Database Syst. Rev. 2016, 8, CD012004. [Google Scholar] [CrossRef]
- McCaskey, M.A.; Schuster-Amft, C.; Wirth, B.; Suica, Z.; de Bruin, E.D. Effects of proprioceptive exercises on pain and function in chronic neck- and low back pain rehabilitation: A systematic literature review. BMC Musculoskelet. Disord. 2014, 15, 382. [Google Scholar] [CrossRef]
- Malfliet, A.; Ickmans, K.; Huysmans, E.; Coppieters, I.; Willaert, W.; Bogaert, W.V.; Rheel, E.; Bilterys, T.; Wilgen, P.V.; Nijs, J. Best Evidence Rehabilitation for Chronic Pain Part 3: Low Back Pain. J. Clin. Med. 2019, 8, 1063. [Google Scholar] [CrossRef]
- Georgy, E.E. Lumbar Repositioning Accuracy as a Measure of Proprioception in Patients with Back Dysfunction and Healthy Controls. Asian Spine J. 2011, 5, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Han, S. Validation of Joint Position Sense of Dorsi-Plantar Flexion of Ankle Measurements Using a Smartphone. Healthc. Inform. Res. 2017, 23, 183–188. [Google Scholar] [CrossRef][Green Version]
- Guidetti, L.; Placentino, U.; Baldari, C. Reliability and Criterion Validity of the Smartphone Inclinometer Application to Quantify Cervical Spine Mobility. Clin. Spine Surg. 2017, 30, E1359–E1366. [Google Scholar] [CrossRef]
- Ghorbani, F.; Kamyab, M.; Azadinia, F. Smartphone Applications as a Suitable Alternative to CROM Device and Inclinometers in Assessing the Cervical Range of Motion in Patients with Nonspecific Neck Pain. J. Chiropr. Med. 2020, 19, 38–48. [Google Scholar] [CrossRef]
- Kolber, M.J.; Pizzini, M.; Robinson, A.; Yanez, D.; Hanney, W.J. The reliability and concurrent validity of measurements used to quantify lumbar spine mobility: An analysis of an iphone® application and gravity based inclinometry. Int. J. Sports Phys. Ther. 2013, 8, 129–137. [Google Scholar] [PubMed]
- Pourahmadi, M.; Momeni, E.; Mohseni, N.; Hesarikia, H.; Ghanjal, A.; Shamsoddini, A. The reliability and concurrent validity of a new iPhone® application for measuring active lumbar spine flexion and extension range of motion in patients with low back pain. Physiother. Theory Pract. 2019, 37, 204–217. [Google Scholar] [CrossRef]
- Pourahmadi, M.R.; Taghipour, M.; Jannati, E.; Mohseni-Bandpei, M.A.; Ebrahimi Takamjani, I.; Rajabzadeh, F. Reliability and validity of an iPhone(®) application for the measurement of lumbar spine flexion and extension range of motion. PeerJ 2016, 4, e2355. [Google Scholar] [CrossRef]
- Bucke, J.; Spencer, S.; Fawcett, L.; Sonvico, L.; Rushton, A.; Heneghan, N.R. Validity of the Digital Inclinometer and iPhone When Measuring Thoracic Spine Rotation. J. Athl. Train 2017, 52, 820–825. [Google Scholar] [CrossRef]
- Salamh, P.A.; Kolber, M. The reliability, minimal detectable change and concurrent validity of a gravity-based bubble inclinometer and iphone application for measuring standing lumbar lordosis. Physiother. Theory Pract. 2014, 30, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Banwell, H.A.; Uden, H.; Marshall, N.; Altmann, C.; Williams, C.M. The iPhone Measure app level function as a measuring device for the weight bearing lunge test in adults: A reliability study. J. Foot Ankle Res. 2019, 12, 37. [Google Scholar] [CrossRef]
- Balsalobre-Fernández, C.; Romero-Franco, N.; Jiménez-Reyes, P. Concurrent validity and reliability of an iPhone app for the measurement of ankle dorsiflexion and inter-limb asymmetries. J. Sports Sci. 2019, 37, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Pourahmadi, M.R.; Ebrahimi Takamjani, I.; Sarrafzadeh, J.; Bahramian, M.; Mohseni-Bandpei, M.A.; Rajabzadeh, F.; Taghipour, M. Reliability and concurrent validity of a new iPhone® goniometric application for measuring active wrist range of motion: A cross-sectional study in asymptomatic subjects. J. Anat. 2017, 230, 484–495. [Google Scholar] [CrossRef] [PubMed]
- Walter, S.D.; Eliasziw, M.; Donner, A. Sample size and optimal designs for reliability studies. Stat. Med. 1998, 17, 101–110. [Google Scholar] [CrossRef]
- Lee, C.-W.; Hyun, J.; Kim, S.G. Influence of Pilates Mat and Apparatus Exercises on Pain and Balance of Businesswomen with Chronic Low Back Pain. J. Phys. Ther. Sci. 2014, 26, 475–477. [Google Scholar] [CrossRef] [PubMed]
- Maher, C.; Underwood, M.; Buchbinder, R. Non-specific low back pain. Lancet 2017, 389, 736–747. [Google Scholar] [CrossRef]
- Amundsen, P.A.; Evans, D.W.; Rajendran, D.; Bright, P.; Bjørkli, T.; Eldridge, S.; Buchbinder, R.; Underwood, M.; Froud, R. Inclusion and exclusion criteria used in non-specific low back pain trials: A review of randomised controlled trials published between 2006 and 2012. BMC Musculoskelet. Disord. 2018, 19, 113. [Google Scholar] [CrossRef]
- Dworkin, R.H.; Turk, D.C.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Katz, N.P.; Kerns, R.D.; Stucki, G.; Allen, R.R.; Bellamy, N.; et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005, 113, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Scholz, J.; Finnerup, N.B.; Attal, N.; Aziz, Q.; Baron, R.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Cruccu, G.; Davis, K.D.; et al. The IASP classification of chronic pain for ICD-11: Chronic neuropathic pain. Pain 2019, 160, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Portney, L.; Watkins, M. Construct Validity. In Foundations of Clinical Research: Applications to Practice; Prentice Hall Health: Upper Saddle River, NJ, USA, 2000; pp. 87–91. [Google Scholar]
- Weir, J.P. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J. Strength Cond. Res. 2005, 19, 231–240. [Google Scholar]
- Gray, V.L.; Ivanova, T.D.; Garland, S.J. Reliability of center of pressure measures within and between sessions in individuals post-stroke and healthy controls. Gait Posture 2014, 40, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Lee, A.S.; Cholewicki, J.; Reeves, N.P.; Zazulak, B.T.; Mysliwiec, L.W. Comparison of Trunk Proprioception Between Patients With Low Back Pain and Healthy Controls. Arch. Phys. Med. Rehabil. 2010, 91, 1327–1331. [Google Scholar] [CrossRef] [PubMed]
- Wellmon, R.H.; Gulick, D.T.; Paterson, M.L.; Gulick, C.N. Validity and Reliability of 2 Goniometric Mobile Apps: Device, Application, and Examiner Factors. J. Sport Rehabil. 2016, 25, 371–379. [Google Scholar] [CrossRef]
- Korakakis, V.; O’Sullivan, K.; O’Sullivan, P.B.; Evagelinou, V.; Sotiralis, Y.; Sideris, A.; Sakellariou, K.; Karanasios, S.; Giakas, G. Physiotherapist perceptions of optimal sitting and standing posture. Musculoskelet. Sci. Pract. 2019, 39, 24–31. [Google Scholar] [CrossRef]

| Total (n = 50) | Men (n = 25) | Women (n = 25) | p * | |
|---|---|---|---|---|
| Age (years) | 33.58 (7.29) | 32.16 (7.53) | 35 (6.88) | 0.170 |
| Height (cm) | 174.30 (0.14) | 174.84 (0.13) | 172.64 (0.14) | 0.225 |
| Weight (kg) | 71.40 (5.20) | 71.52 (5.20) | 70.48 (5.26) | 0.486 |
| BMI (kg/m2) | 24.49 (3.09) | 24.05 (2.18) | 24.93 (3.79) | 0.321 |
| Intensity of pain perception (NPRS) | 6.9 (1.2) | 7.3 (1.0) | 6.6 (1.4) | 0.068 |
| Average pain duration (months) | 37.5 (36.7) | 28.1 (28.4) | 46.8 (41.9) | 0.071 |
| Standing joint position sense (°) | 5.55 (3.07) | 5.57 (2.91) | 5.52 (3.28) | 0.953 |
| Sitting joint position sense (°) | 4.22 (2.52) | 4.19 (2.47) | 4.25 (2.63) | 0.927 |
| iPhone® Inclinometer | |||
|---|---|---|---|
| Measure 1 | Measure 2 | ||
| Test Measurement | Mean (SD) | Mean (SD) | p * |
| All participants | |||
| Standing 30° lumbar flexion (°) | 30.14 (5.87) | 30.44 (6.81) | 0.244 |
| Sitting 30° lumbar flexion (°) | 27.84 (3.67) | 27.62 (4.23) | 0.297 |
| Men | |||
| Standing 30° lumbar flexion (°) | 30.80 (6.53) | 31.16 (7.82) | 0.376 |
| Sitting 30° lumbar flexion (°) | 28.68 (4.22) | 28.52 (4.48) | 0.476 |
| Women | |||
| Standing 30° lumbar flexion (°) | 29.48 (5.18) | 29.72 (5.68) | 0.465 |
| Sitting 30° lumbar flexion (°) | 27 (2.86) | 26.72 (3.84) | 0.442 |
| All (n = 50) | iPhone® Inclinometer | ||||
|---|---|---|---|---|---|
| Assessed Action | ICC (95% CI) | SEM (°) | SEM (%) | SRD (°) | SRD (%) |
| Standing 30° lumbar flexion | 0.96 (0.93–0.98) | 1.27 | 4.2 | 3.51 | 11.6 |
| Sitting 30° lumbar flexion | 0.93 (0.88–0.96) | 1.05 | 3.8 | 2.90 | 10.4 |
| Men (n = 25) | |||||
| Standing 30° lumbar flexion | 0.96 (0.92–0.98) | 1.40 | 4.5 | 3.88 | 12.5 |
| Sitting 30° lumbar flexion | 0.97 (0.93–0.99) | 0.78 | 2.7 | 2.16 | 7.5 |
| Women (n = 25) | |||||
| Standing 30° lumbar flexion | 0.96 (0.91–0.98) | 1.90 | 6.4 | 5.26 | 17.8 |
| Sitting 30° lumbar flexion | 0.86 (0.71–0.94) | 1.24 | 4.6 | 3.45 | 12.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caña-Pino, A.; Espejo-Antúnez, L.; Adsuar, J.C.; Apolo-Arenas, M.D. Test–Retest Reliability of an iPhone® Inclinometer Application to Assess the Lumbar Joint Repositioning Error in Non-Specific Chronic Low Back Pain. Int. J. Environ. Res. Public Health 2021, 18, 2489. https://doi.org/10.3390/ijerph18052489
Caña-Pino A, Espejo-Antúnez L, Adsuar JC, Apolo-Arenas MD. Test–Retest Reliability of an iPhone® Inclinometer Application to Assess the Lumbar Joint Repositioning Error in Non-Specific Chronic Low Back Pain. International Journal of Environmental Research and Public Health. 2021; 18(5):2489. https://doi.org/10.3390/ijerph18052489
Chicago/Turabian StyleCaña-Pino, Alejandro, Luís Espejo-Antúnez, José Carmelo Adsuar, and María Dolores Apolo-Arenas. 2021. "Test–Retest Reliability of an iPhone® Inclinometer Application to Assess the Lumbar Joint Repositioning Error in Non-Specific Chronic Low Back Pain" International Journal of Environmental Research and Public Health 18, no. 5: 2489. https://doi.org/10.3390/ijerph18052489
APA StyleCaña-Pino, A., Espejo-Antúnez, L., Adsuar, J. C., & Apolo-Arenas, M. D. (2021). Test–Retest Reliability of an iPhone® Inclinometer Application to Assess the Lumbar Joint Repositioning Error in Non-Specific Chronic Low Back Pain. International Journal of Environmental Research and Public Health, 18(5), 2489. https://doi.org/10.3390/ijerph18052489









