Adjusted Indirect and Mixed Comparisons of Interventions for the Patient-Reported Outcomes Measures (PROMs) of Disabled Adults: A Systematic Review and Network Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria (PICOS)
2.2.1. Participants/Population
2.2.2. Intervention(s)
2.2.3. Comparator(s)/Control
2.2.4. Outcomes
2.2.5. Study Design(s)
2.3. Exclusion Criteria
2.4. Search Strategy
2.5. Risk of Bias Assessment
2.6. Data Extraction and Synthesis
2.7. Data Pre-Processings
2.7.1. Processing of a PROM with Subscales of Different Dimensions
2.7.2. Processing of Different PROMs of the Same Dimension in a Study
2.8. Network Meta-Analysis
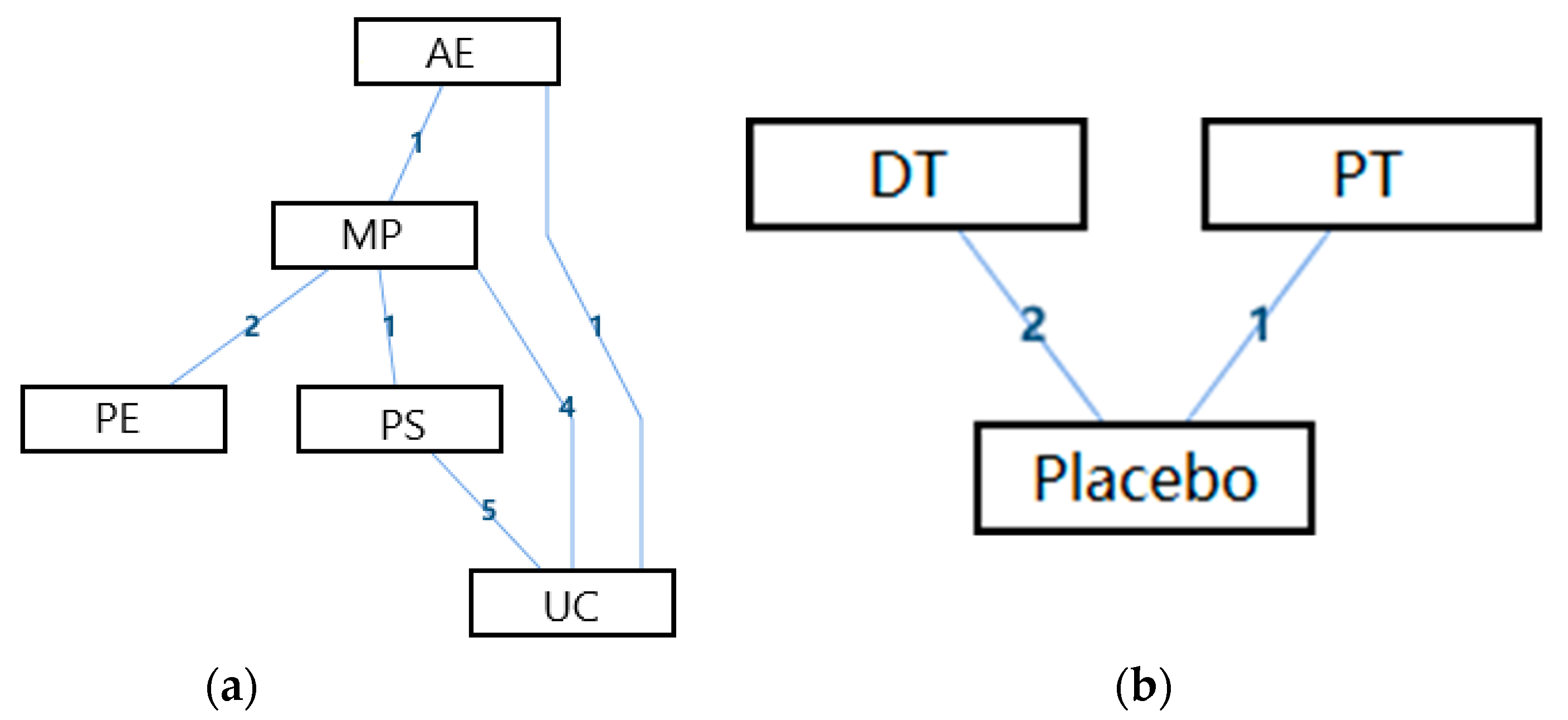
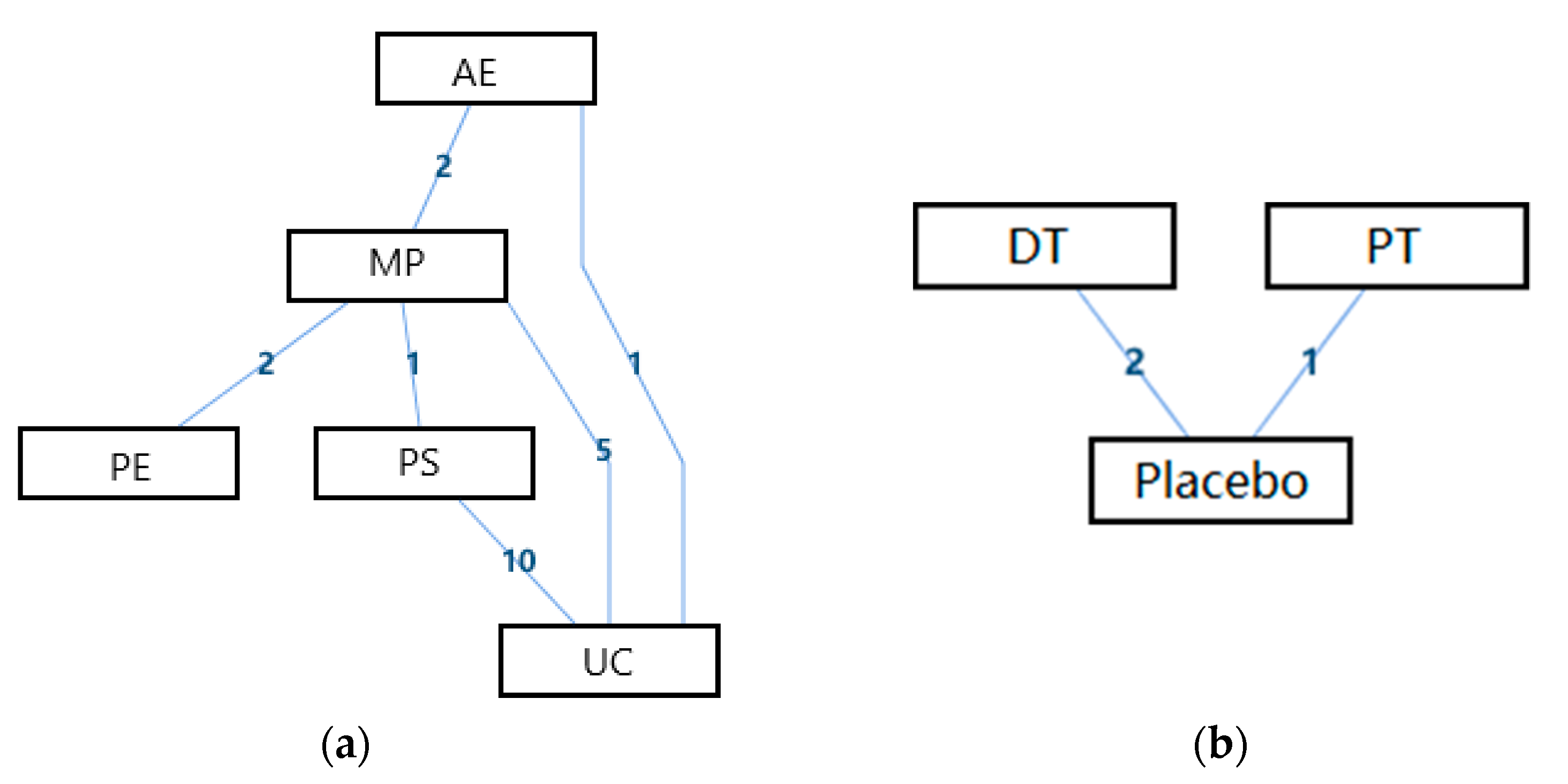
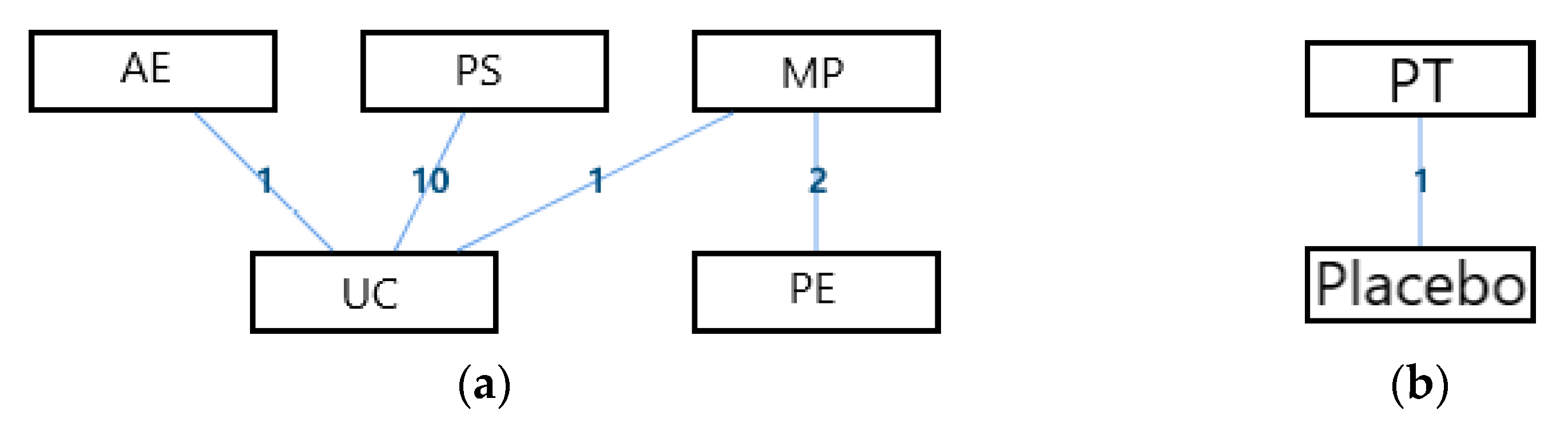
2.8.1. Network Geometry
2.8.2. Consistency and Inconsistency Analysis
2.8.3. Network Meta-Analysis
2.9. Additional Analysis
2.9.1. Pair-Wised Meta-Analysis
2.9.2. The Split Note Calculation
3. Results
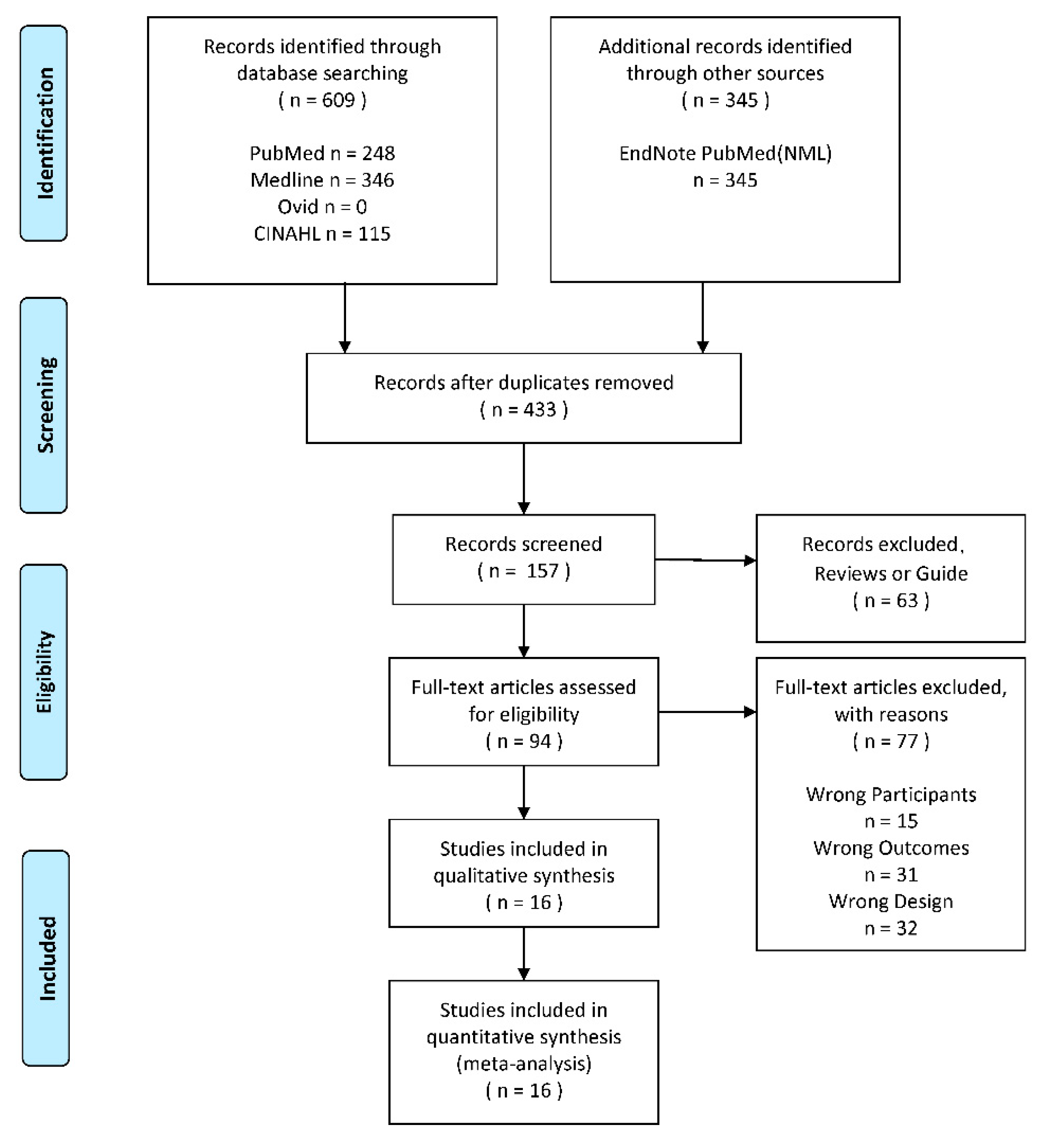
3.1. Search Strategy and Information Extraction
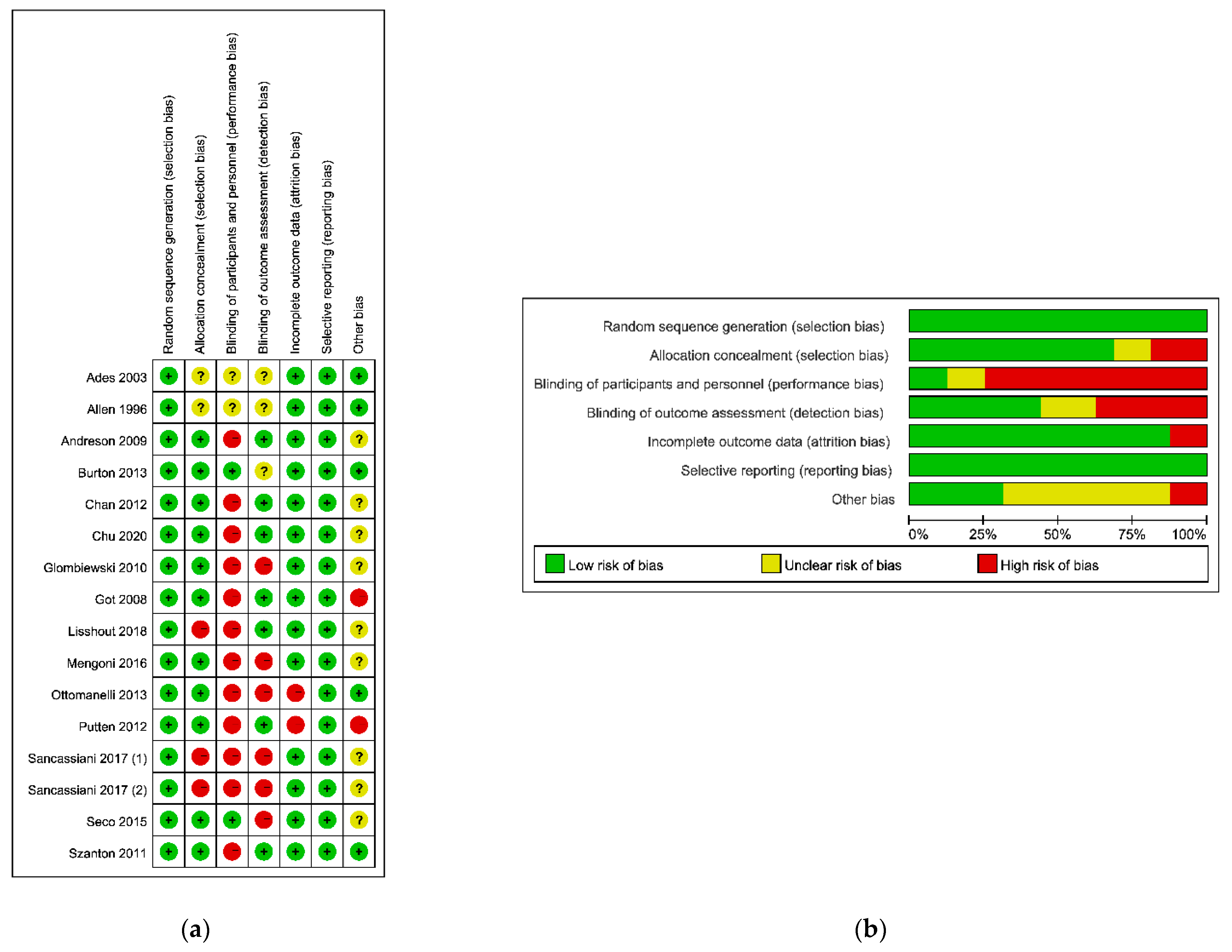
3.2. Risk of Bias
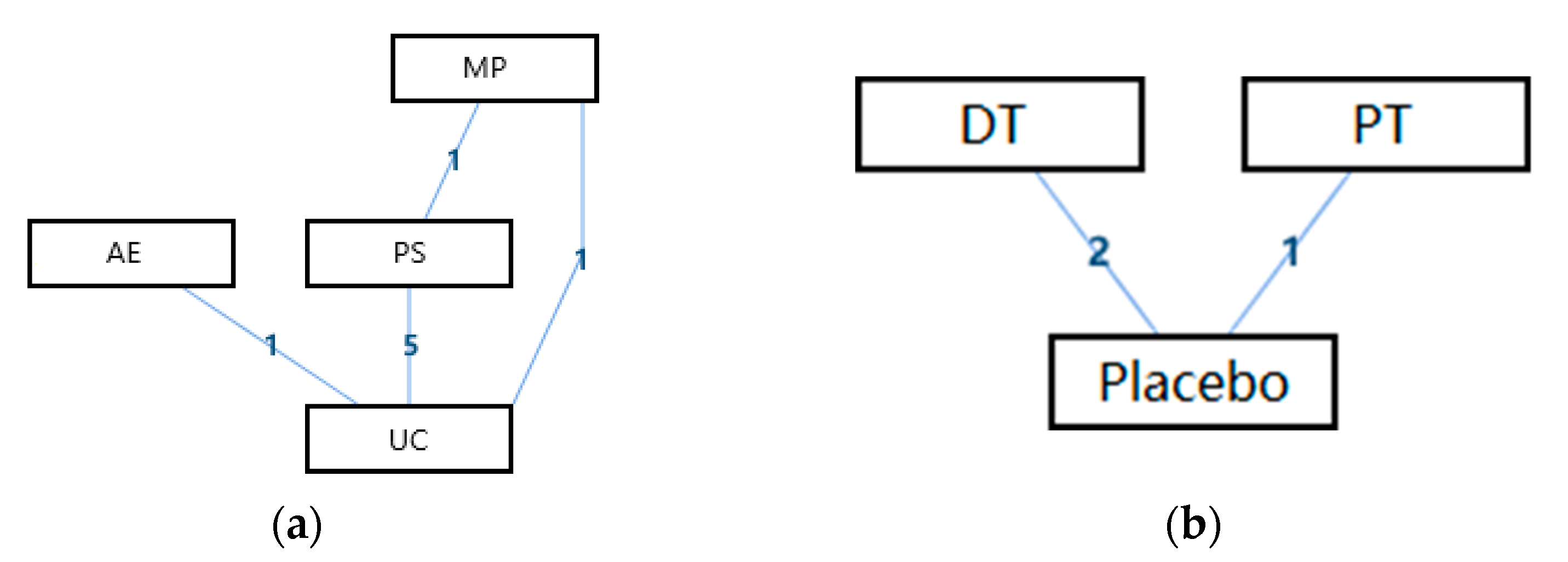
3.3. Network Meta-Analysis
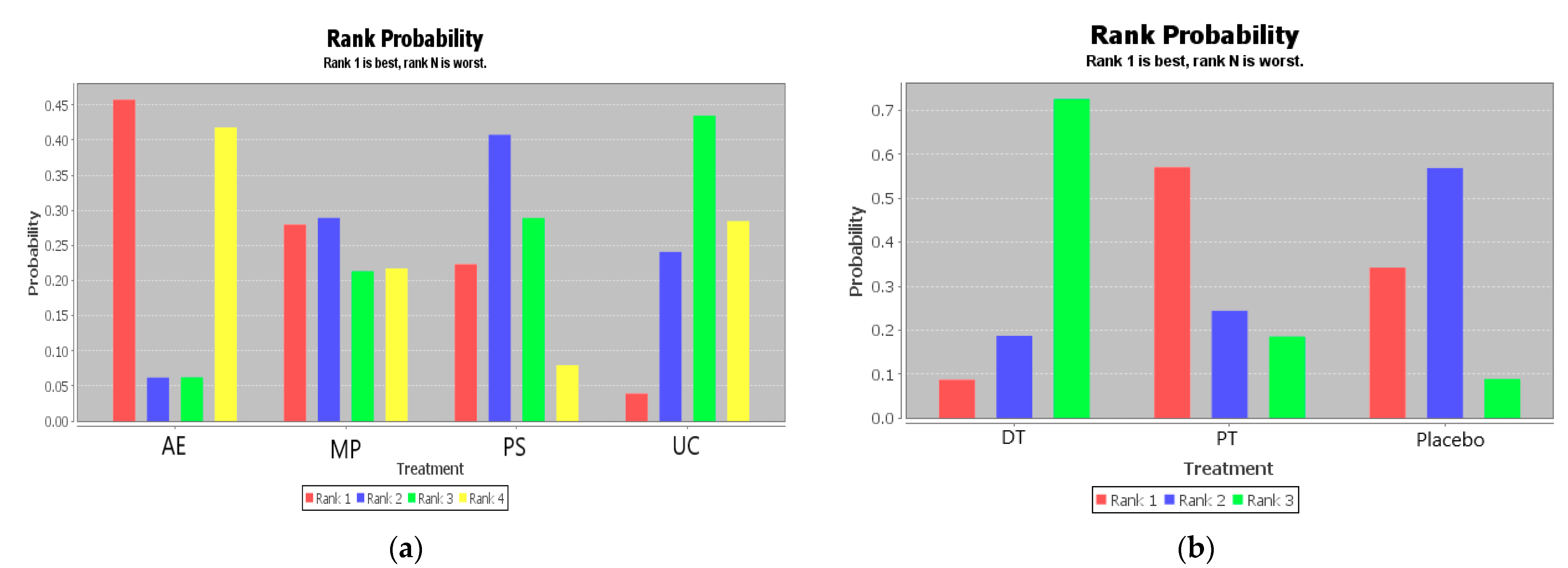
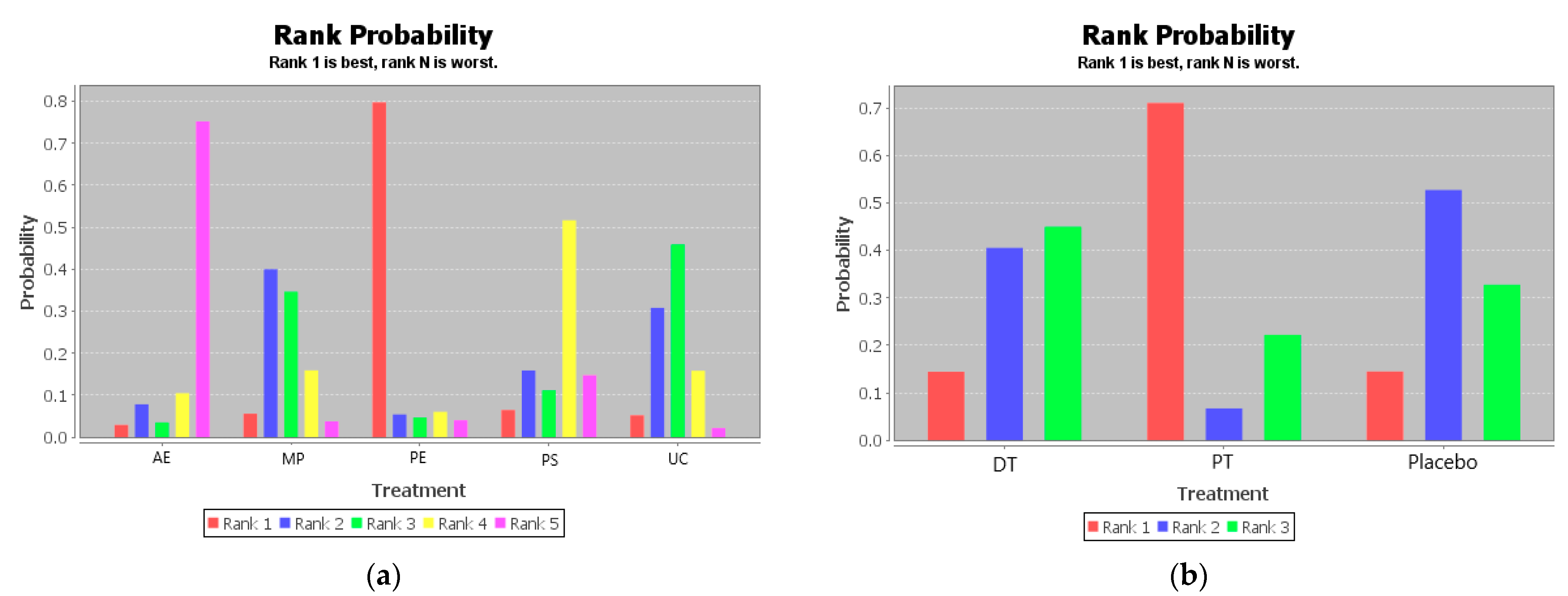
3.3.1. Overall Life Quality
3.3.2. Abilities of Daily Life Activity
3.3.3. Psychological Health
3.3.4. Social Functioning
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ravaud, J.F.; Madiot, B.; Ville, I. Discrimination towards disabled people seeking employment. Soc. Sci. Med. 1992, 35, 951–958. [Google Scholar] [CrossRef]
- Berghs, M.; Atkin, K.; Graham, H.; Hatton, C.; Thomas, C. Public health, research and rights: The perspectives of deliberation panels with politically and socially active disabled people. Disabil. Soc. 2017, 32, 945–965. [Google Scholar] [CrossRef]
- Office of Disability, Social Security Administration. Disability evaluation under Social Security; Office of Disability, Social Security Administration: Baltimore, MD, USA, 1998. [Google Scholar]
- Odp, O. Disability Evaluation Under Social Security; Office of Disability, Social Security Administration: Baltimore, MD, USA, 2003. [Google Scholar]
- Cocchiarella, L.; Anderson, G.B.J. Guides to the Evaluation of Permanent Impairment. Plast. Reconstr. Surg. 1994, 93, 1520. [Google Scholar]
- Park, D.-S.; Lee, S.-G. A Review of the AMA Guides to the Evaluation of Permanent Impairment. J. Korean Med. Assoc. 2009, 52, 567–572. [Google Scholar] [CrossRef][Green Version]
- Miller, P.S. Reclaiming the Vision: The ADA and Definition of Disability. Brandeis L.J. 2002, 32–33. Available online: https://heinonline.org/HOL/LandingPage?handle=hein.journals/branlaj41&div=42&id=&page= (accessed on 28 February 2021).
- Threats, T.T. WHO’s International Classification of Functioning, Disability, and Health: A Framework for Clinical and Research Outcomes; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- Pfaller, J.; Chan, F.; Iwanaga, K.; Wu, J.-R.; Berven, N.L. The International Classification of Functioning, Disability, and Health (ICF) as a community participation model for people with multiple sclerosis: A hierarchical regression analysis. Aust. J. Rehabil. Couns. 2020, 26, 1–18. [Google Scholar] [CrossRef]
- Roland, M.; Fairbank, J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine (Phila Pa 1976) 2000, 25, 3115–3124. [Google Scholar] [CrossRef]
- Garratt, A.M.; Ruta, D.A.; Abdalla, M.I.; Buckingham, J.K.; Russell, I.T. The SF36 health survey questionnaire: An outcome measure suitable for routine use within the NHS? BMJ 1993, 306, 1440–1444. [Google Scholar] [CrossRef]
- Chapman, J.R.; Norvell, D.C.; Hermsmeyer, J.T.; Bransford, R.J.; DeVine, J.; McGirt, M.J.; Lee, M.J. Evaluating common outcomes for measuring treatment success for chronic low back pain. Spine (Phila Pa 1976) 2011, 36, S54–S68. [Google Scholar] [CrossRef]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Roland, M.; Morris, R. A study of the natural history of back pain. Part I: Development of a reliable and sensitive measure of disability in low-back pain. Spine (Phila Pa 1976) 1983, 8, 141–144. [Google Scholar] [CrossRef]
- Waddell, G.; Main, C.J. Assessment of severity in low-back disorders. Spine (Phila Pa 1976) 1984, 9, 204–208. [Google Scholar] [CrossRef]
- Stratford, P.W.; Binkley, J.M.; Riddle, D.L. Development and initial validation of the back pain functional scale. Spine (Phila Pa 1976) 2000, 25, 2095–2102. [Google Scholar] [CrossRef]
- Ruta, D.A.; Garratt, A.M.; Wardlaw, D.; Russell, I.T. Developing a valid and reliable measure of health outcome for patients with low back pain. Spine (Phila Pa 1976) 1994, 19, 1887–1896. [Google Scholar] [CrossRef]
- Bolton, J.E.; Breen, A.C. The Bournemouth Questionnaire: A short-form comprehensive outcome measure. I. Psychometric properties in back pain patients. J. Manip. Physiol. Ther. 1999, 22, 503–510. [Google Scholar] [CrossRef]
- Manniche, C.; Asmussen, K.; Lauritsen, B.; Vinterberg, H.; Kreiner, S.; Jordan, A. Low Back Pain Rating scale: Validation of a tool for assessment of low back pain. Pain 1994, 57, 317–326. [Google Scholar] [CrossRef]
- Kopec, J.A.; Esdaile, J.M.; Abrahamowicz, M.; Abenhaim, L.; Wood-Dauphinee, S.; Lamping, D.L.; Williams, J.I. The Quebec Back Pain Disability Scale: Conceptualization and development. J. Clin. Epidemiol. 1996, 49, 151–161. [Google Scholar] [CrossRef]
- Fairbank, J.C.; Couper, J.; Davies, J.B.; O’Brien, J.P. The Oswestry low back pain disability questionnaire. Physiotherapy 1980, 66, 271–273. [Google Scholar]
- Velstra, I.M.; Ballert, C.S.; Cieza, A. A systematic literature review of outcome measures for upper extremity function using the international classification of functioning, disability, and health as reference. PM R 2011, 3, 846–860. [Google Scholar] [CrossRef]
- Hudak, P.L.; Amadio, P.C.; Bombardier, C. Development of an upper extremity outcome measure: The DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am. J. Ind. Med. 1996, 29, 602–608. [Google Scholar] [CrossRef]
- Chung, K.C.; Pillsbury, M.S.; Walters, M.R.; Hayward, R.A. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J. Hand. Surg. Am. 1998, 23, 575–587. [Google Scholar] [CrossRef]
- Ostelo, R.W.; de Vet, H.C.; Knol, D.L.; van den Brandt, P.A. 24-item Roland-Morris Disability Questionnaire was preferred out of six functional status questionnaires for post-lumbar disc surgery. J. Clin. Epidemiol. 2004, 57, 268–276. [Google Scholar] [CrossRef]
- Johanson, N.A.; Liang, M.H.; Daltroy, L.; Rudicel, S.; Richmond, J. American Academy of Orthopaedic Surgeons lower limb outcomes assessment instruments. Reliability, validity, and sensitivity to change. J. Bone Joint Surg. Am. 2004, 86, 902–909. [Google Scholar] [CrossRef]
- McNair, P.J.; Prapavessis, H.; Collier, J.; Bassett, S.; Bryant, A.; Larmer, P. The lower-limb tasks questionnaire: An assessment of validity, reliability, responsiveness, and minimal important differences. Arch. Phys. Med. Rehabil. 2007, 88, 993–1001. [Google Scholar] [CrossRef]
- Richards, J.S.; Nepomuceno, C.; Riles, M.; Suer, Z. Assessing pain behavior: The UAB Pain Behavior Scale. Pain 1982, 14, 393–398. [Google Scholar] [CrossRef]
- Chibnall, J.T.; Tait, R.C. The Pain Disability Index: Factor structure and normative data. Arch. Phys. Med. Rehabil. 1994, 75, 1082–1086. [Google Scholar] [CrossRef]
- Melzack, R. The McGill Pain Questionnaire: Major properties and scoring methods. Pain 1975, 1, 277–299. [Google Scholar] [CrossRef]
- Wenger, N.K.; Mattson, M.E.; Furberg, C.D.; Elinson, J. Assessment of quality of life in clinical trials of cardiovascular therapies. Am. J. Cardiol. 1984, 54, 908–913. [Google Scholar] [CrossRef]
- Pain Disability Index; Springer: Berlin/Heidelberg, Germany, 2007.
- Spanjer, J.; Groothoff, J.W.; Brouwer, S. Instruments used to assess functional limitations in workers applying for disability benefit: A systematic review. Disabil. Rehabil. 2011, 33, 2143–2150. [Google Scholar] [CrossRef][Green Version]
- Davidson, M.; Keating, J.L. A comparison of five low back disability questionnaires: Reliability and responsiveness. Phys. Ther. 2002, 82, 8–24. [Google Scholar] [CrossRef]
- Painter, J.; Trevithick, L.; Hastings, R.P.; Ingham, B.; Roy, A. Development and validation of the Learning Disabilities Needs Assessment Tool (LDNAT), a HoNOS-based needs assessment tool for use with people with intellectual disability. J. Intellect. Disabil. Res. 2016, 60, 1178–1188. [Google Scholar] [CrossRef]
- Alonso Fachado, A.; Montes Martinez, A.; Menendez Villalva, C.; Pereira, M.G. [Cultural adaptation and validation of the Medical Outcomes Study Social Support Survey questionnaire (MOS-SSS)]. Acta Med. Port. 2007, 20, 525–534. [Google Scholar]
- Jones, P.W.; Quirk, F.H.; Baveystock, C.M.; Littlejohns, P. A self-complete measure of health status for chronic airflow limitation. The St. George’s Respiratory Questionnaire. Am. Rev. Respir. Dis. 1992, 145, 1321–1327. [Google Scholar] [CrossRef]
- Leclerc, G.; Lefrancois, R.; Dube, M.; Hebert, R.; Gaulin, P. Criterion validity of a new measure of self-actualization. Psychol. Rep. 1999, 85, 1167–1176. [Google Scholar] [CrossRef] [PubMed]
- Garrow, A.P.; Papageorgiou, A.C.; Silman, A.J.; Thomas, E.; Jayson, M.I.; Macfarlane, G.J. Development and validation of a questionnaire to assess disabling foot pain. Pain 2000, 85, 107–113. [Google Scholar] [CrossRef]
- Rehman, A.U.; Hassali, M.A.A.; Harun, S.N.; Abbas, S.; Muneswarao, J.; Ali, I.; Hussain, R. Validation and clinical interpretation of the St George’s respiratory questionnaire for COPD (SGRQ-C) after adaptation to Malaysian language and culture, in patients with COPD. Health Qual. Life Outcomes 2020, 18, 138. [Google Scholar] [CrossRef] [PubMed]
- Çulhacik, G.D.; Durat, G.; Eren, N. Effects of activity groups, in which art activities are used, on resilience and related factors in families with disabled children. Perspect. Psychiatr. Care 2020. [Google Scholar] [CrossRef] [PubMed]
- Edgren, J.; Rantanen, T.; Heinonen, A.; Portegijs, E.; Alén, M.; Kiviranta, I.; Kallinen, M.; Sipilä, S. Effects of progressive resistance training on physical disability among older community-dwelling people with history of hip fracture. Aging Clin. Exp. Res. 2012, 24, 171–175. [Google Scholar] [CrossRef]
- Singh, N.N.; Yoon-Suk, H.; Hwang, Y.-S. Mindfulness-based programs and practices for people with intellectual and developmental disability. Curr. Opin. Psychiatry 2020, 33, 86–91. [Google Scholar] [CrossRef]
- Greenhalgh, J.; Long, A.F.; Flynn, R. The use of patient-reported outcome measures in routine clinical practice: Lack of impact or lack of theory? Soc. Sci. Med. 2005, 60, 833–843. [Google Scholar] [CrossRef] [PubMed]
- Weiss, C.H. Nothing as practical as good theory: Exploring theory-based evaluation for comprehensive community initiatives for children and families. New Approaches Eval. Community Initiat. Concepts Methods Contexts 1995, 1, 65–92. [Google Scholar]
- Connell, J.P.; Kubisch, A.C. Applying a theory of change approach to the evaluation of comprehensive community initiatives: Progress, prospects, and problems. New Approaches Eval. Community Initiat. 1998, 2, 1–16. [Google Scholar]
- Szanton, S.L.; Thorpe, R.J.; Boyd, C.; Tanner, E.K.; Leff, B.; Agree, E.; Xue, Q.-L.; Allen, J.K.; Seplaki, C.L.; Weiss, C.O.; et al. Community Aging in Place, Advancing Better Living for Elders: A Bio-Behavioral-Environmental Intervention to Improve Function and Health-Related Quality of Life in Disabled Older Adults. J. Am. Geriatr. Soc. 2011, 59, 2314–2320. [Google Scholar] [CrossRef]
- Mills, E.J.; Thorlund, K.; Ioannidis, J.P. Demystifying trial networks and network meta-analysis. BMJ 2013, 346, f2914. [Google Scholar] [CrossRef]
- Dias, S.; Welton, N.J.; Caldwell, D.M.; Ades, A.E. Checking consistency in mixed treatment comparison meta-analysis. Stat. Med. 2010, 29, 932–944. [Google Scholar] [CrossRef]
- Krahn, U.; Binder, H.; Konig, J. A graphical tool for locating inconsistency in network meta-analyses. BMC Med. Res. Methodol. 2013, 13, 35. [Google Scholar] [CrossRef]
- Jansen, J.P.; Naci, H. Is network meta-analysis as valid as standard pairwise meta-analysis? It all depends on the distribution of effect modifiers. BMC Med. 2013, 11, 159. [Google Scholar] [CrossRef]
- Efthimiou, O.; Mavridis, D.; Cipriani, A.; Leucht, S.; Bagos, P.; Salanti, G. An approach for modelling multiple correlated outcomes in a network of interventions using odds ratios. Stat. Med. 2014, 33, 2275–2287. [Google Scholar] [CrossRef]
- Cipriani, A.; Higgins, J.P.; Geddes, J.R.; Salanti, G. Conceptual and technical challenges in network meta-analysis. Ann. Intern. Med. 2013, 159, 130–137. [Google Scholar] [CrossRef]
- Salanti, G.; Ades, A.E.; Ioannidis, J.P. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: An overview and tutorial. J. Clin. Epidemiol. 2011, 64, 163–171. [Google Scholar] [CrossRef]
- Jansen, J.P.; Schmid, C.H.; Salanti, G. Directed acyclic graphs can help understand bias in indirect and mixed treatment comparisons. J. Clin. Epidemiol. 2012, 65, 798–807. [Google Scholar] [CrossRef]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H.R. An Introduction to Meta-Analysis; A John Wiley and Sons, Ltd.: Hoboken, NJ, USA, 2009. [Google Scholar]
- van Lieshout, M.R.J.; Bleijenberg, N.; Schuurmans, M.J.; de Wit, N.J. The Effectiveness of a PRoactive Multicomponent Intervention Program on Disability in Independently Living Older People: A Randomized Controlled Trial. J. Nutr. Health Aging 2018, 22, 1051–1059. [Google Scholar] [CrossRef]
- Van Der Putten, A.; Waninge, A.; Vlaskamp, C.; Van Der Schans, C. Powered-assisted exercises for people with profound intellectual and multiple disabilities: Effects on functional disabilities, alertness and quality of life. J. Intellect. Disabil. Res. 2012, 56, 787. [Google Scholar] [CrossRef]
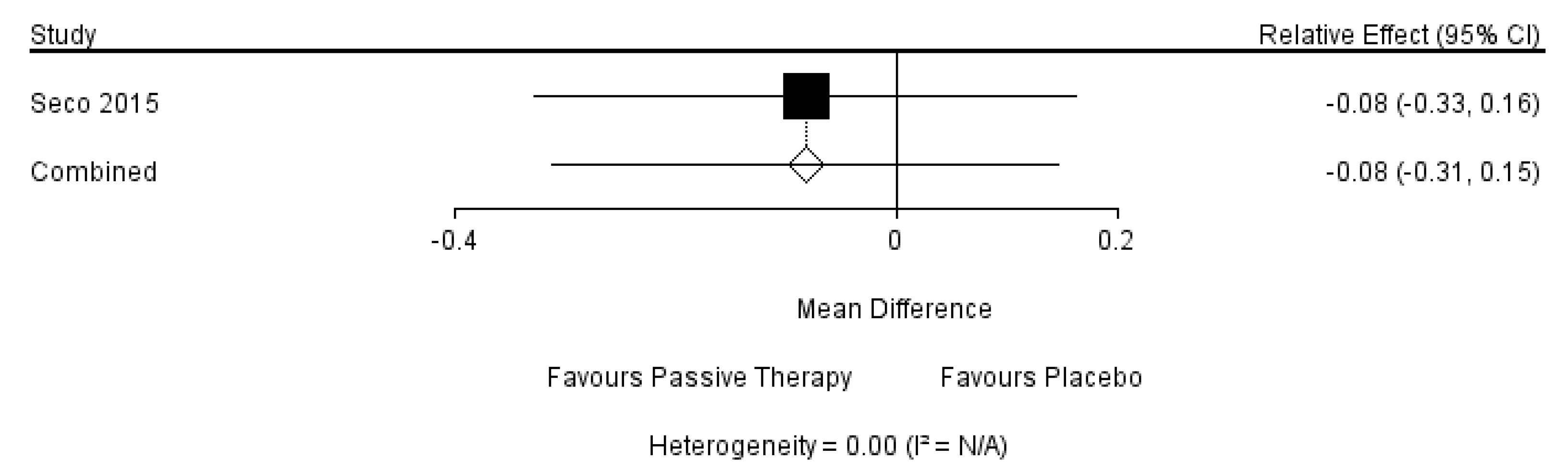
- Seco, J.; Rodriguez-Perez, V.; Lopez-Rodriguez, A.F.; Torres-Unda, J.; Echevarria, E.; Diez-Alegre, M.I.; Ortega, A.; Moran, P.; Mendoza-Laiz, N.; Abecia Inchaurregui, L.C. Effects of vibration therapy on hormone response and stress in severely disabled patients: A double-blind randomized placebo-controlled clinical trial. Rehabil. Nurs. 2015, 40, 166–178. [Google Scholar] [CrossRef]
- Sancassiani, F.; Lorrai, S.; Cossu, G.; Cocco, A.; Trincas, G.; Floris, F.; Mellino, G.; Machado, S.; Nardi, A.E.; Fabrici, E.P.; et al. The Effects of “VelaMente?!” Project on Social Functioning of People with Severe Psychosocial Disabilities. Clin. Pract. Epidemiol. Ment. Health 2017, 13, 220–232. [Google Scholar] [CrossRef]
- Sancassiani, F.; Cocco, A.; Cossu, G.; Lorrai, S.; Trincas, G.; Floris, F.; Mellino, G.; Machado, S.; Nardi, A.E.; Fabrici, E.P.; et al. “VelaMente?!”—Sailin in a Crew to Improve Self-Efficacy in People with Psychosocial Disabilities: A Randomized Controlled Trial. Clin. Pract. Epidemiol. Ment. Health 2017, 13, 200–212. [Google Scholar] [CrossRef] [PubMed]
- Ottomanelli, L.; Barnett, S.D.; Goetz, L.L. A prospective examination of the impact of a supported employment program and employment on health-related quality of life, handicap, and disability among Veterans with SCI. Qual. Life Res. 2013, 22, 2133–2141. [Google Scholar] [CrossRef] [PubMed]
- Mengoni, S.; Durand, M.A.; Parkes, G.; Barton, G.; Friedli, K.; Ring, H.; Wellsted, D.; Zia, A.; Gates, B. A wordless intervention for people with epilepsy and intellectual disabilities: A randomised controlled feasibility trial. J. Intellect. Disabil. Res. 2016, 60, 799. [Google Scholar]
- Got, I.L.S.; Cheng, S. The effects of art facilitation on the social functioning of people with developmental disability. Art Ther. J. Am. Art Ther. Assoc. 2008, 25, 32–37. [Google Scholar] [CrossRef]
- Glombiewski, J.A.; Hartwich-Tersek, J.; Rief, W. Two psychological interventions are effective in severely disabled, chronic back pain patients: A randomised controlled trial. Int. J. Behav. Med. 2010, 17, 97–107. [Google Scholar] [CrossRef]
- Chu, K.; Bu, X.; Sun, Z.; Wang, Y.; Feng, W.; Xiao, L.; Jiang, F.; Tang, X. Feasibility of a Nurse-Trained, Family Member-Delivered Rehabilitation Model for Disabled Stroke Patients in Rural Chongqing, China. J. Stroke Cerebrovasc. Dis. 2020, 29, 105382. [Google Scholar] [CrossRef]
- Chan, W.; Immink, M.A.; Hillier, S. Yoga and exercise for symptoms of depression and anxiety in people with poststroke disability: A randomized, controlled pilot trial. Altern. Ther. Health Med. 2012, 18, 34–43. [Google Scholar] [PubMed]
- Burton, L.A.; Sumukadas, D.; Witham, M.D.; Struthers, A.D.; McMurdo, M.E.T. Effect of spironolactone on physical performance in older people with self-reported physical disability. Am. J. Med. 2013, 126, 590–597. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Andresen, M.; Runge, U.; Hoff, M.; Puggaard, L. Perceived autonomy and activity choices among physically disabled older people in nursing home settings: A randomized trial. J. Aging Health 2009, 21, 1133–1158. [Google Scholar] [CrossRef]
- Allen, K.; Blascovich, J.; Allen, K.; Blascovich, J. The value of service dogs for people with severe ambulatory disabilities. A randomized controlled trial. JAMA J. Am. Med Assoc. 1996, 275, 1001–1006. [Google Scholar] [CrossRef]
- Ades, P.A.; Savage, P.; Cress, M.E.; Brochu, M.; Lee, N.M.; Poehlman, E.T. Resistance training on physical performance in disabled older female cardiac patients. Med. Sci. Sports Exerc. 2003, 35, 1265–1270. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Lungu, D.A.; Pennucci, F.; De Rosis, S.; Romano, G.; Melfi, F. Implementing successful systematic Patient Reported Outcome and Experience Measures (PROMs and PREMs) in robotic oncological surgery-The role of physicians. Int. J. Health Plann. Manag. 2020, 35, 773–787. [Google Scholar] [CrossRef]
- Petrozzi, M.J.; Leaver, A.; Jones, M.K.; Ferreira, P.H.; Rubinstein, S.M.; Mackey, M.G. Does an online psychological intervention improve self-efficacy and disability in people also receiving Multimodal Manual Therapy for chronic low back pain compared to Multimodal Manual Therapy alone? Design of a randomized controlled trial. Chiropr. Man. Therap 2015, 23, 35. [Google Scholar] [CrossRef]
- Martinez Aldao, D.; Martinez Lemos, R.I.; Penedo Vazquez, S.; Ayan Perez, C.L. Effects of a physical exercise programme on the risk of falls, balance, and walking speed in older people with intellectual disabilities. Rehabilitacion (Madr) 2020, 54, 19–24. [Google Scholar] [CrossRef]
- von Bonsdorff, M.B.; Leinonen, R.; Kujala, U.M.; Heikkinen, E.; Törmäkangas, T.; Hirvensalo, M.; Rasinaho, M.; Karhula, S.; Mänty, M.; Rantanen, T. Effect of physical activity counseling on disability in older people: A 2-year randomized controlled trial. J. Am. Geriatr. Soc. 2008, 56, 2188–2194. [Google Scholar] [CrossRef]
- Cameron, L.A.; Phillips, K.; Melvin, G.A.; Hastings, R.P.; Gray, K.M. Psychological interventions for depression in children and young people with an intellectual disability and/or autism: Systematic review. Br. J. Psychiatry 2020, 1–10. [Google Scholar] [CrossRef]
- Scott, K.; Hatton, C.; Knight, R.; Singer, K.; Knowles, D.; Dagnan, D.; Hastings, R.P.; Appleton, K.; Cooper, S.A.; Melville, C.; et al. Supporting people with intellectual disabilities in psychological therapies for depression: A qualitative analysis of supporters’ experiences. J. Appl. Res. Intellect. Disabil. 2019, 32, 323–335. [Google Scholar] [CrossRef]
- Jo, Y.J.; Kim, H. Effects of the model of human occupation-based home modifications on the time use, occupational participation and activity limitation in people with disabilities: A pilot randomized controlled trial. Disabil. Rehabil. Assist. Technol. 2020, 1–7. [Google Scholar] [CrossRef]
- Moorer, P.; Suurmeijer, T.P. A study of the unidimensionality and cumulativeness of the MOS Short-form General Health Survey. Psychol. Rep. 1994, 74, 467–470. [Google Scholar] [CrossRef] [PubMed]
- Simon, G.E.; Bauer, M.S.; Ludman, E.J.; Operskalski, B.H.; Unützer, J. Mood symptoms, functional impairment, and disability in people with bipolar disorder: Specific effects of mania and depression. J. Clin. Psychiatry 2007, 68, 1237–1245. [Google Scholar] [CrossRef]
- Fowler, D.; French, P.; Banerjee, R.; Barton, G.; Berry, C.; Byrne, R.; Clarke, T.; Fraser, R.; Gee, B.; Greenwood, K.; et al. Prevention and treatment of long-term social disability amongst young people with emerging severe mental illness with social recovery therapy (The PRODIGY Trial): Study protocol for a randomised controlled trial. Trials 2017, 18, 315. [Google Scholar] [CrossRef]
- Maber-Aleksandrowicz, S.; Avent, C.; Hassiotis, A. A Systematic Review of Animal-Assisted Therapy on Psychosocial Outcomes in People with Intellectual Disability. Res. Dev. Disabil. 2016, 49–50, 322–338. [Google Scholar] [CrossRef] [PubMed]
- Willner, P. The effectiveness of psychotherapeutic interventions for people with learning disabilities: A critical overview. J. Intellect. Disabil. Res. 2005, 49, 73–85. [Google Scholar] [CrossRef]
- Grills, N.J.; Hoq, M.; Wong, C.-P.P.; Allagh, K.; Singh, L.; Soji, F.; Murthy, G.V.S. Disabled People’s Organisations increase access to services and improve well-being: Evidence from a cluster randomized trial in North India. BMC Public Health 2020, 20, 1–9. [Google Scholar] [CrossRef]
- Bleich, S.N.; Sherrod, C.; Chiang, A.; Boyd, C.; Wolff, J.; Eva, C.; Salzberg, C.; Anderson, K.; Leff, B.; Anderson, G.; et al. Systematic Review of Programs Treating High-Need and High-Cost People With Multiple Chronic Diseases or Disabilities in the United States, 2008-2014. Prev. Chronic Dis. 2015, 12, 1–15. [Google Scholar] [CrossRef]
- Metzelthin, S.F.; van Rossum, E.; Hendriks, M.R.C.; De Witte, L.P.; Hobma, S.O.; Sipers, W.; Kempen, G.I.J.M. Reducing disability in community-dwelling frail older people: Cost-effectiveness study alongside a cluster randomised controlled trial. Age Ageing 2015, 44, 390–396. [Google Scholar] [CrossRef]
- Suijker, J.J.; MacNeil-Vroomen, J.L.; van Rijn, M.; Buurman, B.M.; de Rooij, S.E.; Moll van Charante, E.P.; Bosmans, J.E. Cost-effectiveness of nurse-led multifactorial care to prevent or postpone new disabilities in community-living older people: Results of a cluster randomized trial. PLoS ONE 2017, 12, e0175272. [Google Scholar] [CrossRef]

| Study | Participants | Intervention | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Disability | Mean Age | Gender (Female/All) | Operate Group | Control Group | |||||
| Intervention | Protocol | Classification | Intervention | Protocol | Classification | ||||
| Ades 2003 [71] | Disabled older female cardiac patients | 72.3 | 33/33 | Resistance training | 19 participants, 3 weekly, 6 months | Active exercise | Cardiac rehabilitation facility, a program of stretching, calisthenics, deep-breathing progressive-relaxation exercises, and light yoga | 14 participants, 3 weekly, 6 months | Multi-disciplinary program |
| Andreson 2009 [69] | Physically disabled older people | 84.0 | 35/50 | Nursing home settings program | 27 participants, 12 weeks | Multi-disciplinary program | Usual care and treatment | 20 participants, 12 weeks | Usual care |
| Button 2013 [68] | Older People with a self-reported physical disability | 74.6 | 55/120 | Spironolactone | 25 mg/day, 24 weeks | Drug treatment | Placebo | 25mg/day, 24 weeks | Placebo |
| Chan 2012 [67] | People with poststroke disability | 69.1 | 2/14 | Yoga and exercise program | 1 weekly group yoga, 4 weekly home exercise, 6 weeks | Multi-disciplinary program | Exercise | Self-reported home practice | Active exercise |
| Chu 2020 [66] | Disabled stroke patients | 64.5 | 37/61 | Caregiver education program | Rehabilitation training, self-care, and toileting delivered, post-discharge telephone calls | Psychosocial support program | Usual care | Usual care | Usual care |
| Glomebiewski 2020 [65] | Severely disabled, chronic back pain patients | 48.8 | 77/116 | Cognitive-behavioral therapy including biofeedback tools | An 18 sessions program including EMG feedback, 8 months | Multi-disciplinary program | Cognitive-behavioral therapy, 8 months | An 18 sessions program | Psychological education |
| Sancassiani 2017(1) [60] | People with severe psychosocial disabilities | 37.2 | 11/51 | Sailing course plus drugs treatments | A 3 months-lasting sailing course plus drug treatments as usual. | Multi-disciplinary program | Rehabilitation treatment as usual | Rehabilitation treatment as usual | Usual care |
| Seco 2015 [59] | Severely disabled patients | 45.5 | 7/20 | Vibration therapy | 2 weekly, 8 weeks | Passive therapy | Placebo vibration therapy | 2 weekly, 8 weeks | Placebo |
| Putten 2012 [58] | People with profound intellectual and multiple disabilities | 32.1 | Not mentioned | Power-assisted exercise | 3 weekly, 20 weeks | Active exercise | Therapy as usual | Therapy as usual | Usual care |
| Ottomanelli 2013 [62] | Veterans with spinal cord injury | 49.2 | 0/157 | Support employment program | Employment support in 48 weeks | Psychosocial support program | Treatment as usual | Treatment as usual | Usual care |
| Lieshout 2018 [57] | Independently living older people with disability | 74.0 | 155/281 | A proactive multicomponent intervention program | Spry-program, 23 weeks | Multi-disciplinary program | Usual care | Usual care | Usual care |
| Allen 1996 [70] | People with severe ambulatory disabilities | Not mentioned | 50/100 | Service dogs | 24 months staying with a service dog | Psychosocial support program | Waiting list | Waiting list | Usual care |
| Got 2008 [64] | People with a developmental disability | 27.0 | 16/38 | Art facilitation | 12 group art-making sessions in 12 weeks | Psychosocial support program | No-treatment | No-treatment | Usual care |
| Mengoni 2016 [63] | People with epilepsy and learning disabilities | 41.7 | 23/40 | Wordless intervention | Using a picture booklet with a trained researcher and a caregiver present at least twice more over 20 weeks. | Psychosocial support program | Blank | Blank | Usual care |
| Szanton 2011 [47] | Disabled old people | 78.2 | 38/40 | Bio-behavior-environmental intervention | The community aging in place, advancing better living for elders, 10 in-home sessions, 24 weeks | Multi-disciplinary program | Attention and education control | Attention and education control | Psychosocial support program |
| Sancassiani 2017(2) [61] | People with severe psychosocial disabilities | 37.2 | 11/51 | Sailing course plus drugs treatments | A 3 months-lasting sailing course plus drug treatments as usual. | Multi-disciplinary program | Rehabilitation treatment as usual | Rehabilitation treatment as usual | Usual care |
| Study | Patient-Reported Outcome Measures (PROM) | |||
|---|---|---|---|---|
| Scale | Total Score | Follow up (Weeks) | Classification | |
| Ades 2003 [71] | Continous-Scale Physical Performance Test (CS-PFP) | 100 | 0/24 | Abilities of daily life activity |
| MOS SF-36 Physical Functioning (SF 36-PF) | 100 | Abilities of daily life activity | ||
| Andreson 2009 [69] | The Measure of Actualization of Potential Test (MAP) | 100 | 0/12/24 | Abilities of daily life activity |
| Burton 2013 [68] | EuroQoL-Visual Analogue Scale (EQ-VAS) | 100 | 0/10/20 | Abilities of daily life activity |
| EuroQoL- 5 Dimensions (EQ-5D) | 1.59 | Overall life quality | ||
| The Function Limitation Profile (FLP) | 117 | Overall life quality | ||
| Hospital Anxiety and Depression Scale-Depression (HADS-D) | 21 | Psychological Health | ||
| Hospital Anxiety and Depression Scale-Anxiety (HADS-A) | 21 | Psychological Health | ||
| Chan 2012 [67] | The Geriatric Depression Scale-Short Form (GDS-15) | 15 | 0/6 | Psychological Health |
| State-Trait Anxiety Inventory- State (STAT-S/Y1) | 80 | Psychological Health | ||
| State-Trait Anxiety Inventory- Trait (STAT-T/Y2) | 80 | Psychological Health | ||
| Chu 2020 [66] | Caregiver Burden Inventory (CBI) | 96 | 0/32 | Social Functioning |
| EuroQoL- 5 Dimensions (EQ-5D) | 1.59 | Overall life quality | ||
| Barthel Index (BI) | 100 | Social Functioning | ||
| Glombiewski 2010 [65] | Pain Intensity Questionnaire (PIQ) | 10 | 0/32/56 | Abilities of daily life activity |
| Pain Diary | 10 | Abilities of daily life activity | ||
| Pain Disability Index (PDI) | 7 | Abilities of daily life activity | ||
| Health-related Life Satisfaction Scale | 35 | Psychological Health | ||
| Beck Depression Inventory (BDI) | 63 | Psychological Health | ||
| Coping Strategies Scale (CSS) | 112 | Social Functioning | ||
| Sancassian 2017 (1) [60] | Clinical Global Impression-Severity Scale (CGI-S) | 7 | 0/12 | Abilities of daily life activity |
| Biological Rhythms Interview of Assessment in Neuropsychiatry (BRAIN) | 84 | Overall life quality | ||
| Global Assessment of Functioning (GAF) | 100 | Abilities of daily life activity | ||
| The health of the Nation Outcome Scale - Total | 48 | Overall life quality | ||
| The health of the Nation Outcome Scale—Behavioral | 12 | Social Functioning | ||
| The health of the Nation Outcome Scale—Cognitive and physical impairment | 8 | Overall life quality | ||
| The health of the Nation Outcome Scale—Psychopathological symptoms | 12 | Psychological Health | ||
| The health of the Nation Outcome Scale—Social | 16 | Social Functioning | ||
| Sancassian 2017 (2) [61] | Sense of Coherence (SOC-13) | 91 | 0/12 | Psychological Health |
| The short-form health survey—Physical component score (SF-12 PCS) | 47 | Abilities of daily life activity | ||
| The short-form health survey—Mental component score (SF-12 MCS) | 47 | Psychological Health | ||
| General self-efficacy scale (GSES) | 40 | Psychological HealthGot | ||
| Seco 2015 [59] | WHO Quality of Life -Physical Health | 35 | 0/8 | Abilities of daily life activity |
| WHO Quality of Life -Psychological Health | 30 | Psychological Health | ||
| WHO Quality of Life -Social Relationship | 20 | Social Functioning | ||
| WHO Quality of Life -Environment | 40 | Social Functioning | ||
| WHO Quality of Life -General Health | 10 | Overall life quality | ||
| State-Trait Anxiety Inventory- State (STAT-S/Y1) | 80 | Psychological Health | ||
| Lieshout 2018 [57] | Groningen Frailty Indicator (GFI) | 15 | 0/75 | Abilities of daily life activity |
| Quality of Life-Physical Composite Scale (SF 12-PCS) | 50 | Abilities of daily life activity | ||
| Quality of Life-Mental Composite Scale (SF 12-MCS) | 50 | Psychological Health | ||
| Allen 1996 [70] | The Spheres of Control Scale (SCS) | 180 | 0/24/48 | Psychological Health |
| Rosenberg Self-esteem Scale (RSS) | 50 | Psychological Health | ||
| Affect Balance Scale (ABS) | 9 | Psychological Health | ||
| Community Integrated Questionnaire | 28 | Social Functioning | ||
| Putton 2012 [58] | Behavioral Appraisal Scale (BAS) | 100 | 0/20 | Overall life quality |
| Alertness Observation List | 100 | Psychological Health | ||
| Quality of Life-PMD Physical Wellbeing | 100 | Abilities of daily life activity | ||
| Quality of Life-PMD Material Wellbeing | 100 | Psychological Health | ||
| Quality of Life-PMD Communication Wellbeing | 100 | Social Functioning | ||
| Quality of Life-PMD Social Wellbeing | 100 | Social Functioning | ||
| Quality of Life-PMD Development | 100 | Social Functioning | ||
| Quality of Life-PMD Activities | 100 | Psychological Health | ||
| Got 2008 [64] | The scale of independent behavior—revised (SIB-R) Social interaction | 5 | 0/12 | Social Functioning |
| The scale of independent behavior—revised (SIB-R) Language comprehension | 5 | Social Functioning | ||
| The scale of independent behavior—revised (SIB-R) Language expression | 5 | Social Functioning | ||
| Quality of life enjoyment and satisfaction questionnaire (Q-LES-Q) Subjective feelings | 3 | Psychological Health | ||
| Quality of life enjoyment and satisfaction questionnaire (Q-LES-Q) Leisure time activities | 3 | Social Functioning | ||
| Quality of life enjoyment and satisfaction questionnaire (Q-LES-Q) Social relationship | 3 | Social Functioning | ||
| Quality of life enjoyment and satisfaction questionnaire (Q-LES-Q) General activities | 3 | Abilities of daily life activity | ||
| engoni 2016 [63] | Epilepsy and learning disabilities quality of life scale (ELDQOL)—Seizure severity | 70 | 0/4/12/20 | Abilities of daily life activity |
| Epilepsy and learning disabilities quality of life scale (ELDQOL)—The side effect | 95 | Abilities of daily life activity | ||
| Epilepsy and learning disabilities quality of life scale (ELDQOL)—Behavior | 45 | Social Functioning | ||
| Epilepsy and learning disabilities quality of life scale (ELDQOL)—Mood | 80 | Psychological Health | ||
| EuroQoL-Visual Analogue Scale (EQ-VAS) | 100 | Abilities of daily life activity | ||
| EuroQoL- 5 Dimensions (EQ-5D) | 1.59 | Overall life quality | ||
| Ottomanelli 2013 [62] | Veterans RAND 36-item health survey (VR-36)—Physical component score | 100 | 0/24/48 | Abilities of daily life activity |
| Veterans RAND 36-item health survey (VR-36)—Mental component score | 100 | Psychological Health | ||
| Functional independence measure—Total | 126 | Overall life quality | ||
| Functional independence measure—Cognitive function | 35 | Social Functioning | ||
| Functional independence measure—Motor function | 91 | Abilities of daily life activity | ||
| Craig handicap assessment and reporting technique (CHART)—Social interaction | 100 | Social Functioning | ||
| Craig handicap assessment and reporting technique (CHART)—Mobility | 100 | Abilities of daily life activity | ||
| Craig handicap assessment and reporting technique (CHART)—Cognitive independence | 100 | Psychological Health | ||
| Craig handicap assessment and reporting technique (CHART)—Occupation | 100 | Social Functioning | ||
| Craig handicap assessment and reporting technique (CHART)—Physical independence | 100 | Abilities of daily life activity | ||
| Craig handicap assessment and reporting technique (CHART)—Economic self-sufficiency | 100 | Social Functioning | ||
| Szanton 2011 [47] | The activity of daily life difficulties (ADL) | 5 | 0/24 | Abilities of daily life activity |
| The instrumental activity of daily life difficulties (IADL) | 6 | Abilities of daily life activity | ||
| Health-related quality of life (Euro-QOL) | 100 | Overall life quality | ||
| EuroQoL- 5 Dimensions (EQ-5D) | 6 | Overall life quality | ||
| Fall efficacy | 65 | Psychological Health | ||
| Active Exercise | −0.01 (−0.58, 0.54) | −0.01 (−0.57, 0.50) | −0.03 (−0.59, 0.47) |
|---|---|---|---|
| Multi-disciplinary Program | −0.00 (−0.17, 0.16) | −0.03 (−0.19, 0.13) | |
| Psychosocial Support Program | −0.02 (−0.08, 0.04) | ||
| Usual Care | |||
| Drug Treatment | 0.51 (−0.91, 1.95) | 0.40 (−0.43, 1.23) | |
| Passive Therapy | −0.11 (−1.26, 1.02) | ||
| Placebo |
| Treatment | Rank 1 | Rank 2 | Rank 3 | Rank 4 |
|---|---|---|---|---|
| Active Exercise | 0.46 | 0.06 | 0.06 | 0.42 |
| Multi-disciplinary Program | 0.28 | 0.29 | 0.21 | 0.22 |
| Psychosocial Support Program | 0.22 | 0.41 | 0.29 | 0.08 |
| Usual Care | 0.04 | 0.24 | 0.43 | 0.28 |
| Drug Treatment | 0.09 | 0.19 | 0.73 | |
| Passive Therapy | 0.57 | 0.24 | 0.19 | |
| Placebo | 0.34 | 0.57 | 0.09 |
| Name | Direct Effect | Indirect Effect | Overall | p-Value |
|---|---|---|---|---|
| MP, PS | −0.07 (−0.31, 0.20) | 0.02 (−0.18, 0.20) | −0.00 (−0.17, 0.16) | 0.62 |
| MP, UC | −0.01 (−0.19, 0.16) | −0.11 (−0.35, 0.16) | −0.03 (−0.19, 0.13) | 0.55 |
| PS, UC | −0.02 (−0.08, 0.04) | 0.07 (−0.28, 0.37) | −0.02 (−0.08, 0.04) | 0.62 |
| Active Exercise | −0.00 (−0.10, 0.08) | −0.00 (−0.10, 0.08) | −0.00 (−0.10, 0.08) | −0.00 (−0.10, 0.08) |
|---|---|---|---|---|
| Multi-disciplinary Program | 0.06 (−0.04, 0.17) | −0.01 (−0.04, 0.01) | −0.00 (−0.02, 0.02) | |
| Psychological Education | −0.08 (−0.19, 0.03) | −0.06 (−0.17, 0.04) | ||
| Psychosocial Support Program | 0.01 (−0.01, 0.04) | |||
| Usual Care | ||||
| Drug Treatment | 0.04 (−0.06, 0.14) | 0.00 (−0.03, 0.03) | ||
| Passive Therapy | −0.04 (−0.14, 0.06) | |||
| Placebo |
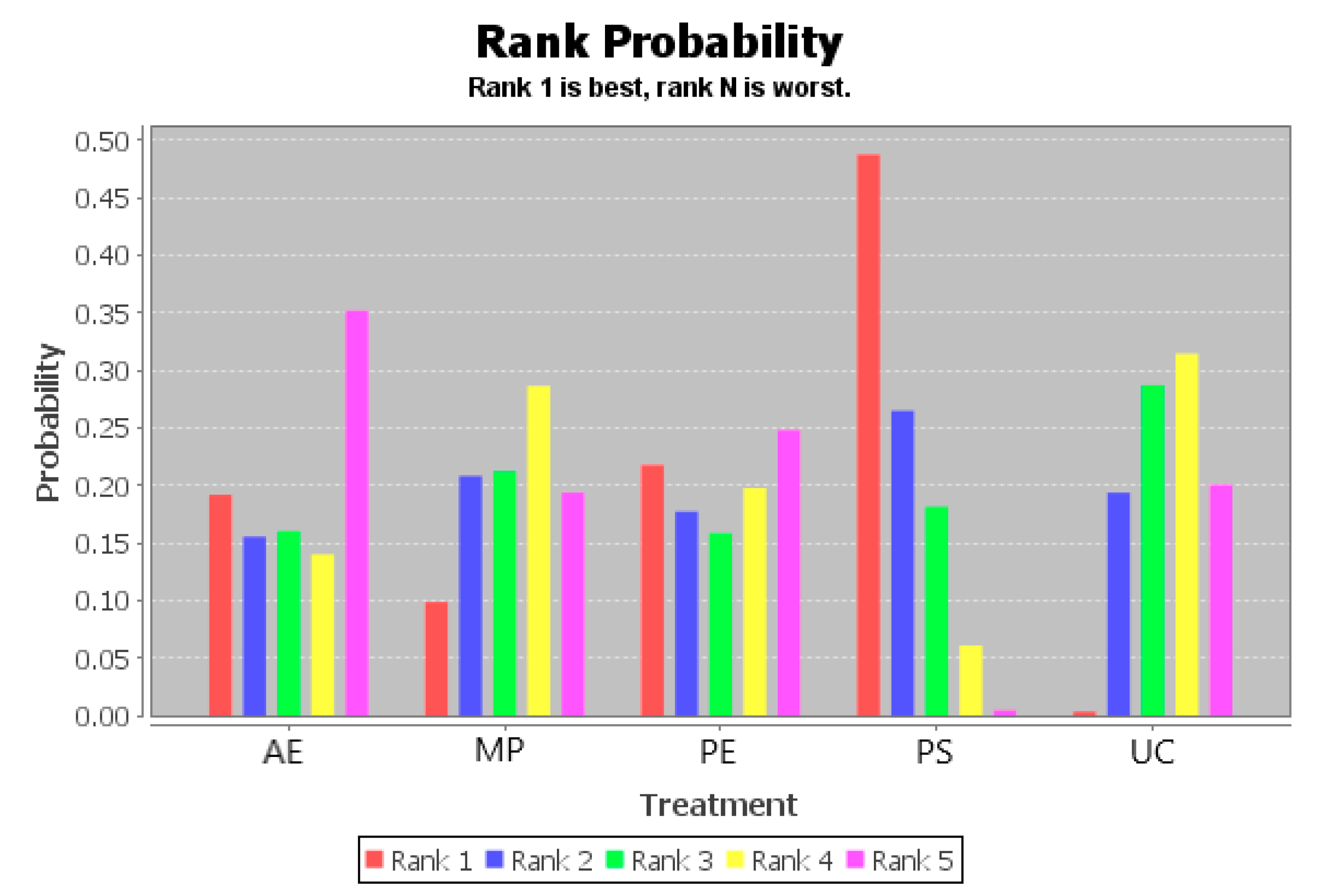
| Treatment | Rank 1 | Rank 2 | Rank 3 | Rank 4 | Rank 5 |
|---|---|---|---|---|---|
| Active Exercise | 0.04 | 0.1 | 0.03 | 0.08 | 0.75 |
| Multi-disciplinary Program | 0.04 | 0.47 | 0.35 | 0.12 | 0.01 |
| Psychological Education | 0.84 | 0.04 | 0.04 | 0.06 | 0.02 |
| Psychosocial Support Program | 0.01 | 0.04 | 0.11 | 0.63 | 0.21 |
| Usual Care | 0.07 | 0.35 | 0.47 | 0.11 | 0.01 |
| Drug Treatment | 0.14 | 0.41 | 0.45 | ||
| Passive Therapy | 0.71 | 0.07 | 0.22 | ||
| Placebo | 0.14 | 0.53 | 0.33 |
| Name | Direct Effect | Indirect Effect | Overall | p-Value |
|---|---|---|---|---|
| AE, MP | 0.03 (−0.16, 0.19) | 0.06 (−0.05, 0.18) | 0.05 (−0.05, 0.15) | 0.69 |
| AE, UC | 0.06 (−0.05, 0.19) | 0.02 (−0.13, 0.20) | 0.05 (−0.06, 0.15) | 0.68 |
| MP, PS | −0.19 (−0.53, 0.11) | −0.01 (−0.04, 0.02) | −0.01 (−0.04, 0.01) | 0.28 |
| MP, UC | −0.00 (−0.01, 0.02) | −0.03 (−0.17, 0.13) | −0.00 (−0.02, 0.02) | 0.75 |
| PS, UC | 0.01 (−0.01, 0.03) | 0.19 (−0.12, 0.48) | 0.01 (−0.01, 0.04) | 0.26 |
| Active Exercise | 0.00 (−0.40, 0.42) | 0.05 (−0.57, 0.67) | 0.12 (−0.35, 0.60) | −0.00 (−0.44, 0.44) |
|---|---|---|---|---|
| Multi-disciplinary Program | 0.05 (−0.42, 0.51) | 0.12 (−0.19, 0.42) | −0.00 (−0.26, 0.25) | |
| Psychological Education | 0.07 (−0.47, 0.63) | −0.05 (−0.57, 0.48) | ||
| Psychosocial Support Program | −0.12 (−0.32, 0.08) | |||
| Usual Care | ||||
| Drug Treatment | 0.02 (−0.17, 0.21) | −0.01 (−0.07, 0.04) | ||
| Passive Therapy | −0.04 (−0.22, 0.15) | |||
| Placebo |
| Treatment | Rank 1 | Rank 2 | Rank 3 | Rank 4 | Rank 5 |
|---|---|---|---|---|---|
| Active Exercise | 0.20 | 0.16 | 0.15 | 0.16 | 0.32 |
| Multi-disciplinary Program | 0.05 | 0.19 | 0.29 | 0.32 | 0.16 |
| Psychological Education | 0.32 | 0.16 | 0.12 | 0.13 | 0.27 |
| Psychosocial Support Program | 0.41 | 0.30 | 0.17 | 0.09 | 0.04 |
| Usual Care | 0.02 | 0.19 | 0.27 | 0.30 | 0.22 |
| Drug Treatment | 0.14 | 0.41 | 0.45 | ||
| Passive Therapy | 0.71 | 0.07 | 0.22 | ||
| Placebo | 0.14 | 0.53 | 0.33 |
| Name | Direct Effect | Indirect Effect | Overall | p-Value |
|---|---|---|---|---|
| AE, MP | −0.02 (−0.50, 0.47) | 0.05 (−0.68, 0.83) | 0.00 (−0.40, 0.42) | 0.86 |
| AE, UC | 0.04 (−0.66, 0.74) | −0.03 (−0.60, 0.53) | −0.00 (−0.44, 0.44) | 0.88 |
| MP, PS | 0.12 (−0.59, 0.82) | 0.11 (−0.25, 0.47) | 0.12 (−0.19, 0.42) | 0.98 |
| MP, UC | −0.01 (−0.31, 0.28) | 0.02 (−0.53, 0.60) | −0.00 (−0.26, 0.25) | 0.91 |
| PS, UC | −0.12 (−0.34, 0.10) | −0.11 (−0.88, 0.66) | −0.12 (−0.32, 0.08) | 0.98 |
| Active Exercise | 0.02 (−1.14, 1.20) | 0.05 (−1.29, 1.34) | 0.28 (−0.61, 1.16) | 0.01 (−0.83, 0.84) |
|---|---|---|---|---|
| Multi-disciplinary Program | 0.03 (−0.56, 0.58) | 0.26 (−0.58, 1.10) | −0.01 (−0.81, 0.79) | |
| Psychological Education | 0.23 (−0.80, 1.29) | −0.04 (−1.03, 0.99) | ||
| Psychosocial Support Program | −0.27 (−0.52, −0.01) | |||
| Usual Care |
| Treatment | Rank 1 | Rank 2 | Rank 3 | Rank 4 | Rank 5 |
|---|---|---|---|---|---|
| Active Exercise | 0.19 | 0.16 | 0.16 | 0.14 | 0.35 |
| Multi-disciplinary Program | 0.10 | 0.21 | 0.21 | 0.29 | 0.19 |
| Psychological Education | 0.22 | 0.18 | 0.16 | 0.20 | 0.25 |
| Psychosocial Support Program | 0.49 | 0.27 | 0.18 | 0.06 | 0.00 |
| Usual Care | 0.00 | 0.19 | 0.29 | 0.31 | 0.20 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, Y.; Li, X.; Sun, Z.; Song, Y.; Baker, J.S.; Gu, Y. Adjusted Indirect and Mixed Comparisons of Interventions for the Patient-Reported Outcomes Measures (PROMs) of Disabled Adults: A Systematic Review and Network Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 2406. https://doi.org/10.3390/ijerph18052406
Xu Y, Li X, Sun Z, Song Y, Baker JS, Gu Y. Adjusted Indirect and Mixed Comparisons of Interventions for the Patient-Reported Outcomes Measures (PROMs) of Disabled Adults: A Systematic Review and Network Meta-Analysis. International Journal of Environmental Research and Public Health. 2021; 18(5):2406. https://doi.org/10.3390/ijerph18052406
Chicago/Turabian StyleXu, Yining, Xin Li, Zhihong Sun, Yang Song, Julien S. Baker, and Yaodong Gu. 2021. "Adjusted Indirect and Mixed Comparisons of Interventions for the Patient-Reported Outcomes Measures (PROMs) of Disabled Adults: A Systematic Review and Network Meta-Analysis" International Journal of Environmental Research and Public Health 18, no. 5: 2406. https://doi.org/10.3390/ijerph18052406
APA StyleXu, Y., Li, X., Sun, Z., Song, Y., Baker, J. S., & Gu, Y. (2021). Adjusted Indirect and Mixed Comparisons of Interventions for the Patient-Reported Outcomes Measures (PROMs) of Disabled Adults: A Systematic Review and Network Meta-Analysis. International Journal of Environmental Research and Public Health, 18(5), 2406. https://doi.org/10.3390/ijerph18052406









