Analysis on Effectiveness of Impact Based Heatwave Warning Considering Severity and Likelihood of Health Impacts in Seoul, Korea
Abstract
1. Introduction
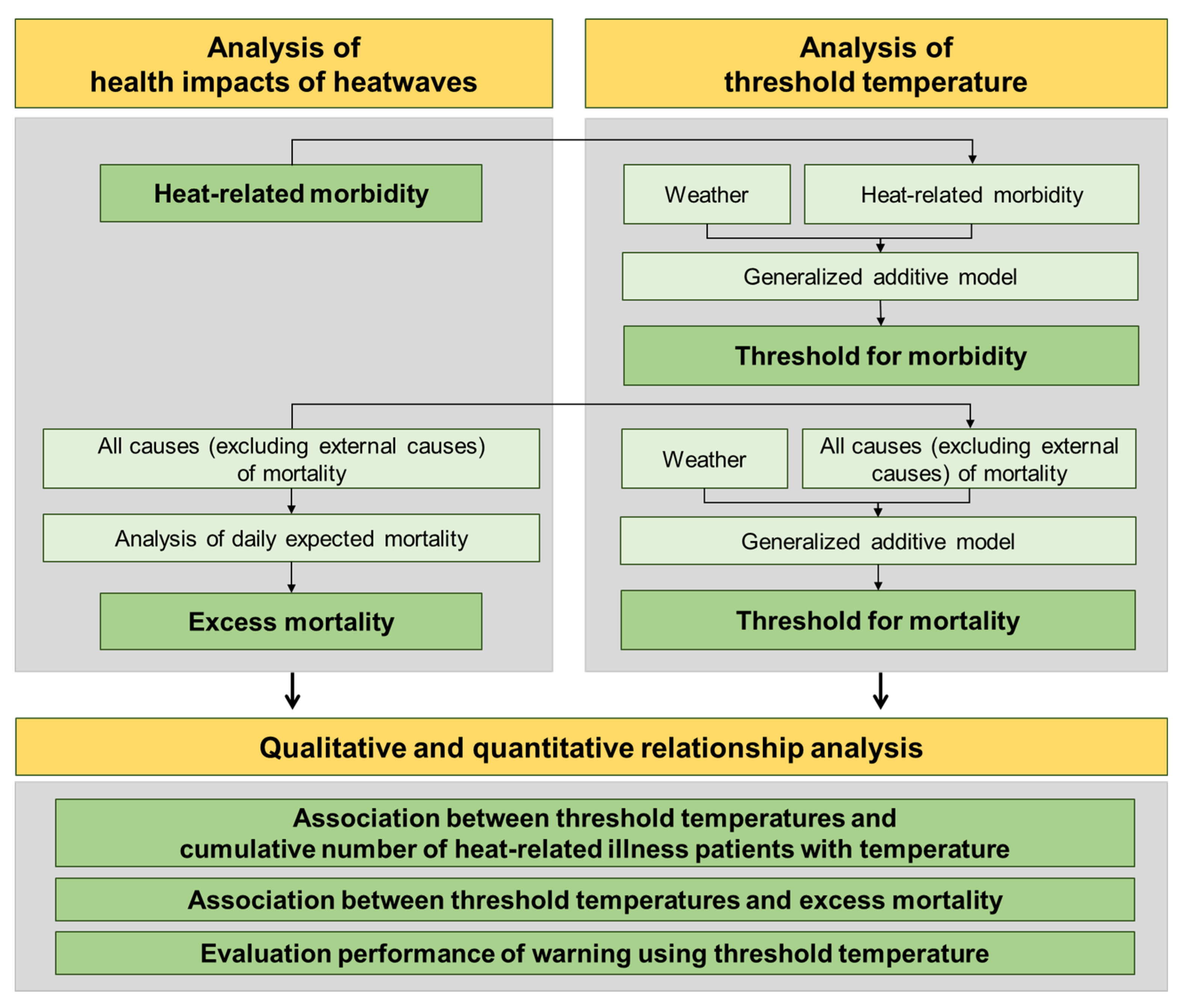
2. Materials and Methodology
2.1. Research Scope
2.2. Materials
2.3. Statistical Methods
2.4. Evaluation Methods Using Skill Score
3. Results
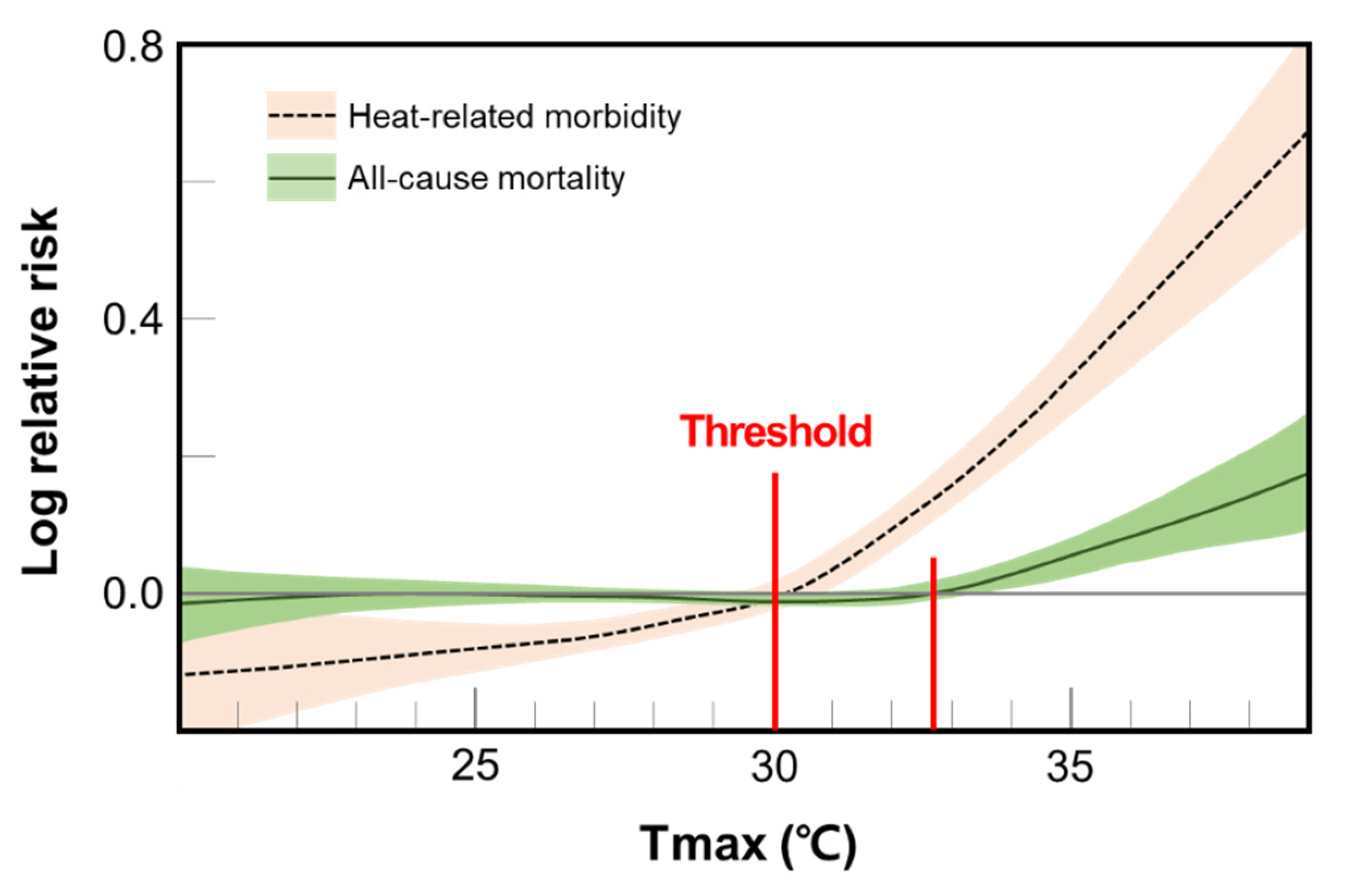
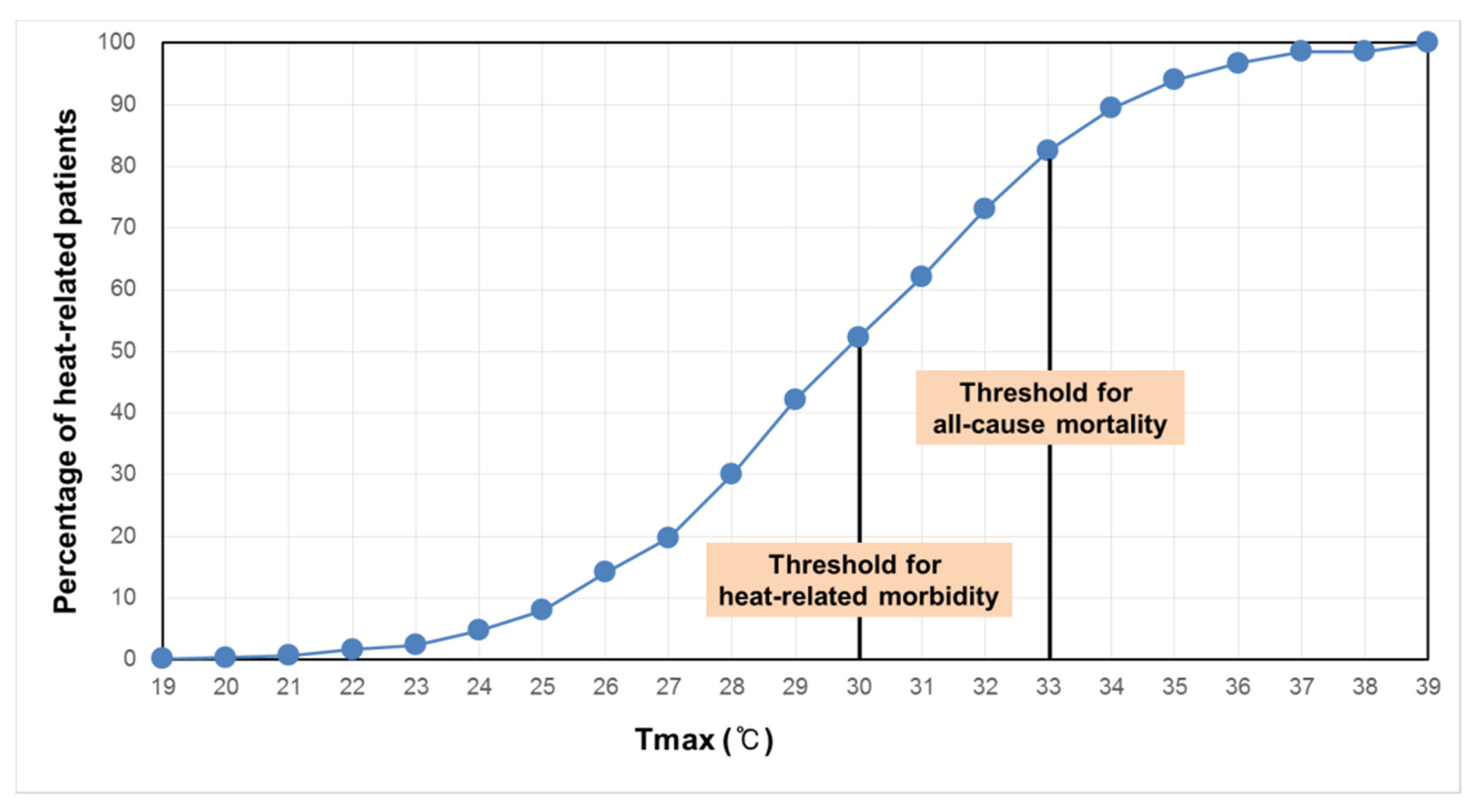
3.1. Threshold Temperatures and HRI Patients
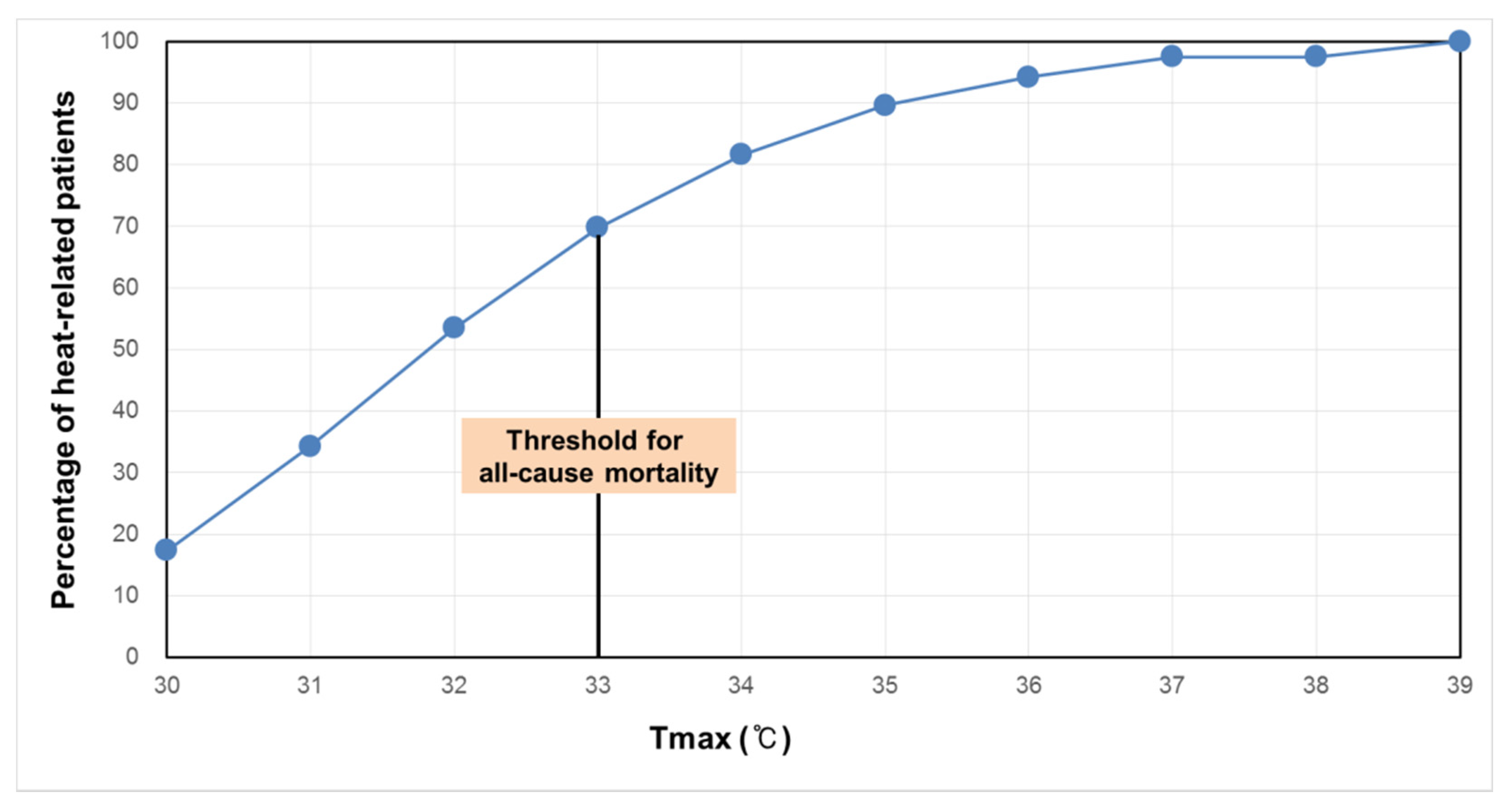
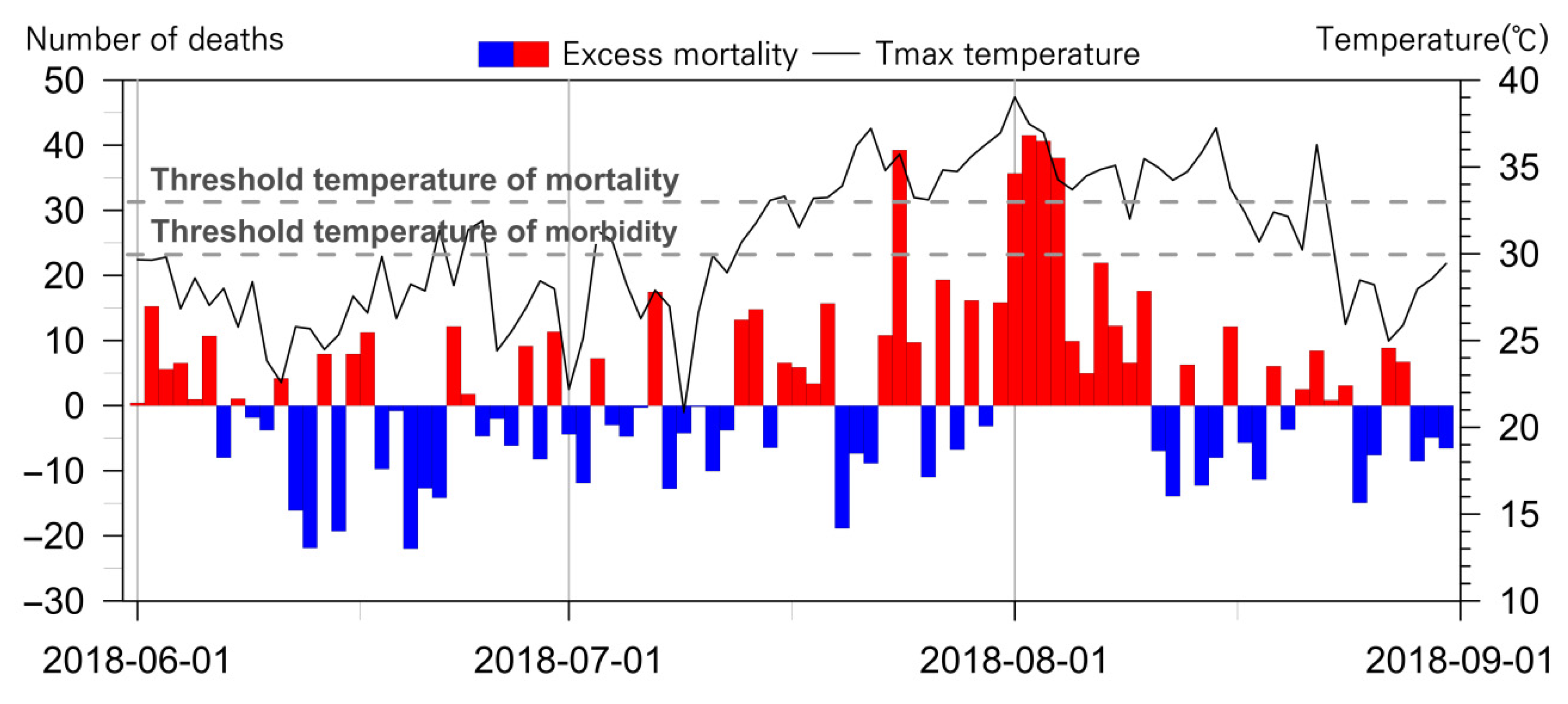
3.2. Threshold Temperatures and Excess Mortality
3.3. Performance Comparison of Heatwave Early Warnings
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Country | HWWS | Warning Level | Criteria for Warnings | Health Impact Proxy | Reference |
|---|---|---|---|---|---|
| Australia | Heat health alert system | 1 | Alert: When forecast daily average temperatures are predicted to reach or exceed the heat health temperature threshold. | Heat-related illness | [53,54,55] |
| England | Heat-health alert service | 1~4 | Level 2: When there is a 60% risk of heatwave in the next 2 to 3 days. Level 3: When threshold temperatures have been reached in any one region or more. | Excess mortality | [24] |
| France | Heat Health Watch Warning System | 1~4 | Level 2: When thresholds are to be reached within three days. Level 3: When the thresholds are reached. | Excess mortality | [14,26,27,56] |
| Japan | Heatstroke prevention information | 1~4 | Levels 1 to 4 will be issued, when WBGT is more than 21, 25, 28, and 31 °C, respectively. | Heat stroke | [28] |
| South Korea | Heat Watch Warning System | 1 & 2 | Level 1: When maximum temperature is more than 33 °C for at least two consecutive days. Level 2: When maximum temperature is more than 35 °C for at least two consecutive days. | Excess mortality | [37,38,39] |
| USA | Heat Safety | 1~4 | Excessive Heat Outlooks: When the potential for an excessive heat event in the next 3–7 days is identified. Excessive Heat Watches: When conditions are favorable for an excessive heat event in the next 24 to 72 h. Heat Advisory: Within 12 h of the onset of extremely dangerous heat conditions. The general rule of thumb for this Advisory is when the maximum heat index temperature is expected to be 100°F or higher for at least 2 days, and night time air temperatures will not drop below 75°F; however, these criteria vary across the country, especially for areas that are not considered to exhibit dangerous heat conditions. Excessive Heat Warning: Within 12 h of the onset of extremely dangerous heat conditions. The general rule of thumb for this Warning is when the maximum heat index temperature is expected to be 105°F or higher for at least 2 days and night time air temperatures will not drop below 75°F; however, these criteria vary across the country, especially for areas not used to extreme heat conditions. | Human experimentation | [15] |
References
- KMA (Korea Meteorological Administration). Comparison of heatwaves in 2018 and 1994 (Press release 2018.08.17.); National Climate Data Center: Seoul, Korea, 2018.
- Hayashida, K.; Shimizu, K.; Yokota, H. Severe heatwave in Japan. Acute Med. Surg. 2019, 6, 206–207. [Google Scholar] [CrossRef]
- Li, M.; Yao, Y.; Luo, D.; Zhong, L. The Linkage of the Large-Scale Circulation Pattern to a Long-Lived Heatwave over Mideastern China in 2018. Atmosphere 2019, 10, 89. [Google Scholar] [CrossRef]
- Bureau of Meteorology, AUS. Climate Change—Trends and Extremes. 2020. Available online: http://www.bom.gov.au/climate/change (accessed on 1 June 2020).
- Opernicus and Climate Change Service. Observed Temperature Extremes. 2019. Available online: https://surfobs.climate.copernicus.eu/stateoftheclimate/observed_extremes.php (accessed on 3 March 2020).
- Oliver, E.C.J.; Donat, M.G.; Burrows, M.T.; Moore, P.J.; Smale, D.A.; Alexander, L.V.; Benthuysen, J.A.; Feng, M.; Gupta, A.S.; Hobday, A.J.; et al. Longer and more frequent marine heatwaves over the past century. Nat. Commun. 2018, 9, 1324. [Google Scholar] [CrossRef]
- Shin, J.; Olson, R.; An, S.I. Projected heat wave characteristics over the Korean Peninsula during the twenty-first Century. Asia-Pac. J. Atmos. Sci. 2018, 54, 53–61. [Google Scholar] [CrossRef]
- Lee, J.Y.; Kim, E.; Lee, W.S.; Chae, Y.; Kim, H. Projection of future mortality due to temperature and population changes under Representative Concentration Pathways and Shared Socioeconomic Pathways. Int. J. Environ. Res. Public Health 2018, 15, 822. [Google Scholar] [CrossRef]
- Park, J.; Choi, S.H.; Chae, Y. Analysis of mortality change rate from temperature in summer by age, occupation, household type, and chronic diseases in 229 Korean municipalities from 2007 to 2016. Int. J. Environ. Res. Public Health 2019, 16, 1561. [Google Scholar] [CrossRef]
- López, J.A.; Julio, D.; Sánchez-Guevara, C.; Sanchez Martinez, G.; Franco, M.; Gullón, P.; Miguel, N.P.; Valero, I.; Cristina, L. The impact of heat waves on daily mortality in districts in Madrid: The effect of sociodemographic factors. Environ. Res. 2020, 190, 109993. [Google Scholar] [CrossRef]
- Ostro, B.D.; Roth, L.A.; Green, R.S.; Basu, R. Estimating the mortality effect of the July 2006 California heat wave. Environ. Res. 2009, 109, 614–619. [Google Scholar] [CrossRef]
- Chan, E.Y.Y.; Goggins, W.B.; Kim, J.J.; Griffiths, S.M. A study of intracity variation of temperature-related mortality and socioeconomic status among the Chinese population in Hong Kong. J. Epidemiol. Community Health 2010, 66, 322–327. [Google Scholar] [CrossRef] [PubMed]
- Met Office. Heat-Health Watch. 2020. Available online: https://www.metoffice.gov.uk/public/weather/heat-health/?tab=heatHealth&season=normal (accessed on 1 June 2020).
- Météo-France. Vigilance Meteo France. 2020. Available online: https://vigilance.meteofrance.fr/fr (accessed on 1 June 2020).
- NWS. Heat Watch vs. Warning. 2020. Available online: https://www.weather.gov/safety/heat-ww (accessed on 1 June 2020).
- PHU. Heat Warning and Information System. 2020. Available online: https://www2.health.vic.gov.au/public-health/environmental-health/climate-weather-and-public-health/heatwaves-and-extreme-heat/heat-health-alert-status (accessed on 1 June 2020).
- HHS. Heat-Health Related Alert System. 2020. Available online: http://www.health.gov.on.ca/en/common/ministry/publications/reports/heat_warning_information_system/heat_warning_information_system.aspx (accessed on 1 June 2020).
- Lowe, D.; Ebi, K.L.; Forsberg, B. Heatwave early warning systems and adaptation advice to reduce human health consequences of heatwaves. Int. J. Environ. Res. Public Health 2011, 8, 4623–4648. [Google Scholar] [CrossRef] [PubMed]
- Ebi, K.L.; Teisberg, T.J.; Kalkstein, L.S.; Robinson, L.; Weiher, R.F. Heat watch/warning systems save lives: Estimated costs and benefits for Philadelphia 1995–98. Bull. Am. Meteorol. Soc. 2004, 85, 1067–1074. [Google Scholar] [CrossRef]
- Fouillet, A.; Rey, G.; Wagner, V.; Laaidi, K.; Empereur-Bissonnet, P.; Le Tertre, A.; Frayssinet, P.; Bessemoulin, P.; Laurent, F.; De Crouy-Chanel, P.; et al. Has the impact of heat waves on mortality changed in France since the European heat wave of summer 2003? A study of the 2006 heat wave. Int. J. Epidemiol. 2008, 37, 309–317. [Google Scholar] [CrossRef]
- Bai, L.; Ding, G.; Gu, S.; Bi, P.; Su, B.; Qin, D.; Xu, G.; Liu, Q. The effects of summer temperature and heat waves on heat-related illness in a coastal city of China, 2011–2013. Environ. Res. 2014, 132, 212–219. [Google Scholar] [CrossRef]
- Bell, M.L.; Dominici, F. Effect modification by community characteristics on the short-term effects of ozone exposure and mortality in 98 US communities. Am. J. Epidemiol. 2008, 167, 986–997. [Google Scholar] [CrossRef]
- WMO. WMO Risk Management Framework; Communications and Public Affairs Office: Geneva, Switzerland, 2013. [Google Scholar]
- PHE. Heatwave Plan for England; PHE: London, UK, 2018.
- Casanueva, A.; Burgstall, A.; Kotlarski, S.; Messeri, A.; Morabito, M.; Flouris, A.D.; Nybo, L.; Spirig, C.; Schwierz, C. Overview of existing heat-health warning systems in Europe. Int. J. Environ. Res. Public Health 2019, 16, 2657. [Google Scholar] [CrossRef]
- Santé publique France. Bulletin de santé publique. 2019. Available online: https://www.santepubliquefrance.fr/determinants-de-sante/climat/fortes-chaleurs-canicule/documents/bulletin-national/bulletin-de-sante-publique-canicule.-bilan-ete-2019 (accessed on 1 July 2020).
- Laaidi, A.; Ung, A.; Wagner, V.; Beaudeau, P.; Pascal, M. The French Heat and Health Watch Warning System: Principles, Fundamentals and Assessment; French Institute for Public Health Surveillance, Department of Environmental Health: Paris, France, 2013. [Google Scholar]
- Japan ME (Ministry of the Environment). HRI Prevention Information. 2020. Available online: www.wbgt.env.go.jp (accessed on 3 March 2020).
- Williams, L.; Erens, B.; Ettelt, S.; Hajat, S.; Manacorda, T.; Mays, N. Evaluation of the Heatwave Plan for the UK: Final Report; Policy Innovation Evaluation Research Unit, London School of Hygiene and Tropical Medicine: London, UK, 2019. [Google Scholar]
- Gasparrini, A.; Guo, Y.; Hashizume, M.; Lavigne, E.; Zanobetti, A.; Schwartz, J.; Tobias, A.; Tong, S.; Rocklöv, J.; Forsberg, B.; et al. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. Lancet 2015, 386, 369–375. [Google Scholar] [CrossRef]
- Hajat, S.; Kovats, R.S.; Atkinson, R.W.; Haines, A. Impact of hot temperatures on death in London: A time series approach. J. Epidemiol. Community Health 2002, 56. [Google Scholar] [CrossRef]
- Sun, X.; Sun, Q.; Yang, M.; Zhou, X.; Li, X.; Yu, A.; Geng, F.; Guo, Y. Effects of temperature and heat waves on emergency department visits and emergency ambulance dispatches in Pudong New Area, China: A time series analysis. Environ. Health 2014, 13. [Google Scholar] [CrossRef]
- Ma, W.; Chen, R.; Kan, H. Temperature-related mortality in 17 large Chinese cities: How heat and cold affect mortality in China. Environ. Res. 2014, 134, 127–133. [Google Scholar] [CrossRef]
- Lippmann, S.J.; Fuhrmann, C.M.; Waller, A.E.; Richardson, D.B. Ambient temperature and emergency department visits for heat-related illness in North Carolina, 2007–2008. Environ. Res. 2013, 124, 35–42. [Google Scholar] [CrossRef]
- Lee, M.; Shi, L.; Zanobetti, A.; Schwartz, J.D. Study on the association between ambient temperature and mortality using spatially resolved exposure data. Environ. Res. 2016, 151, 610–617. [Google Scholar] [CrossRef] [PubMed]
- Oudin Åström, D.; Forsberg, B.; Ebi, K.; Rocklöv, J. Attributing mortality from extreme temperatures to climate change in Stockholm, Sweden. Nat. Clim. Chang. 2013, 3, 1050–1054. [Google Scholar] [CrossRef]
- Park, J.K.; Jung, W.S.; Kim, E.B. A study on the influence of extreme heat on daily mortality. J. Korean Soc. Atmos. Environ. 2008, 24, 523–537. [Google Scholar] [CrossRef][Green Version]
- Park, J.K.; Jung, W.S.; Kim, E.B. Study on the establishment of threshold criteria for heat health watch warning system in Korea; Part I: Establishment of criteria and verification. J. Environ. Sci. 2009, 18, 767–780. [Google Scholar] [CrossRef][Green Version]
- Hwang, M.K.; Kang, Y.H.; Kim, S.; Kim, Y.K. Investigation of operation and improvement for heat watch. J. Environ. Sci. Int. 2019, 28, 277–285. [Google Scholar] [CrossRef]
- KMA. 2020. Available online: https://www.weather.go.kr/weather/warning/heatwave.jsp (accessed on 20 August 2020).
- Lee, W.; Choi, H.M.; Lee, J.Y.; Kim, D.H.; Honda, Y.; Kim, H. Temporal changes in mortality impacts of heat wave and cold spell in Korea and Japan. Environ. Int. 2018, 116, 136–146. [Google Scholar] [CrossRef]
- Campbell, S.; Remenyi, T.A.; White, C.J.; Johnston, F.H. Heatwave and health impact research: A global review. Health Place 2018, 53, 210–218. [Google Scholar] [CrossRef]
- Carmona, R.; Linares, C.; Ortiz, C.; Mirón, I.J.; Luna, M.Y.; Díaz, J. Spatial variability in threshold temperatures of heat wave mortality: Impact assessment on prevention plans. Int. J. Environ. Health Res. 2017, 27, 463–475. [Google Scholar] [CrossRef]
- Hess, J.J.; Sathish, L.M.; Knowlton, K.; Saha, S.; Dutta, P.; Ganguly, P.; Tiwari, A.; Jaiswal, A.; Sheffield, P.; Sarkar, J.; et al. Building resilience to climate change: Pilot evaluation of the impact of India’s first heat action plan on all-cause mortality. J. Environ. Public Health 2018, 2018, 7973519. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Joh, S. A vulnerability study of the low-income elderly in the context of high temperature and mortality in Seoul, Korea. Sci. Total Environ. 2006, 371, 82–88. [Google Scholar] [CrossRef]
- Royé, D.; Codesido, R.; Tobías, A.; Taracido, M. Heat wave intensity and daily mortality in four of the largest cities of Spain. Environ. Res. 2020, 182, 109027. [Google Scholar] [CrossRef]
- Yang, H.J.; Yi, C.; Chae, Y.; Park, J. Comparison of statistical interpolation methods for downscaling of summer temperature data from the Korea Meteorological Administration’s digital forecasts. J. Assoc. Korean Photo Geogr. 2019, 29, 19–32. [Google Scholar] [CrossRef]
- Gasparrini, A.; Armstrong, B.; Kenward, M.G. Distributed lag non-linear models. Stat. Med. 2010, 29, 2224–2234. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.; Kim, I.G.; Lee, D.G.; Shin, J.; Kim, B.J. Study on the vulnerability regarding high temperature related mortality in Korea. J. Korean Geogr. Soc. 2014, 49, 245–263. [Google Scholar]
- FluMOMO v4.2. Available online: https://www.euromomo.eu/how-it-works/flumomo/ (accessed on 28 April 2020).
- Fawcett, T. An introduction to ROC analysis. Pattern Recognit. Lett. 2006, 27, 861–874. [Google Scholar] [CrossRef]
- Robin, X.; Turck, N.; Hainard, A.; Tiberti, N.; Lisacek, F.; Sanchez, J.-C.; Müller, M. pROC: An open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform. 2011, 12, 77. [Google Scholar] [CrossRef]
- Nairn, J.R.; Fawcett, R.J. Defining Heatwaves: Heatwave Defined as a Heat-Impact Event Servicing All Community and Business Sectors in Australia; CAWCR Technical Report; The Centre for Australian Weather and Climate Research: Adelaide, Australia, 2013.
- Nairn, J.R.; Fawcett, R.J. Excess heat factor: A metric for heatwave intensity and its use in classifying heatwave severity. Int. J. Environ. Res. Public Health 2015, 12, 227–253. [Google Scholar] [CrossRef]
- Department of Health. Heat Health Alert System: Information for Local Government and Other Stakeholders; Victorian Government: Melbourne, Australia, 2020.
- Pascal, M.; Laaidi, K.; Ledrans, M.; Baffert, E.; Caserio-Schönemann, C.; Le Tertre, A.; Manach, J.; Medina, S.; Rudant, J.; Empereur-Bissonnet, P. France’s heat health watch warning system. Int. J. Biometeorol. 2006, 50, 144–153. [Google Scholar] [CrossRef]

| Type of Day | Number of Days |
|---|---|
| ① Number of days when the daily maximum temperature ≥30 °C and <33 °C | 194 |
| ② Number of days when the warning was issued | 54 |
| ③ Number of days when the daily maximum temperature <30 °C in cases ② | 22 |
| ④ Number of days missed from the warning in cases ① (① − (② − ③)) | 162 |
| Quartile | 30 ≤ Tmax < 33 (n = 195) | 33 ≤ Tmax (n = 81) |
|---|---|---|
| Max | 24.54 | 44.79 |
| 75% | 5.89 | 14.06 |
| Mean | −0.02 | 5.79 |
| 25% | −5.88 | −6.47 |
| Min | −26.43 | −21.56 |
| Threshold Type | AUC | Warning Criteria | |
|---|---|---|---|
| Level-1 | Level-2 | ||
| Mortality | 0.60 | 0.86 | Level-1: The mortality threshold will be exceeded within the next 2 days Level-2: The mortality threshold has been exceeded |
| Morbidity | 0.73 | 0.78 | Level-1: The morbidity threshold has been exceeded Level-2: The morbidity threshold has been exceeded for at least two days |
| Morbidity and mortality | 0.74 | 0.86 | Level-1: The morbidity threshold has been exceeded Level-2: The mortality threshold has been exceeded |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chae, Y.; Park, J. Analysis on Effectiveness of Impact Based Heatwave Warning Considering Severity and Likelihood of Health Impacts in Seoul, Korea. Int. J. Environ. Res. Public Health 2021, 18, 2380. https://doi.org/10.3390/ijerph18052380
Chae Y, Park J. Analysis on Effectiveness of Impact Based Heatwave Warning Considering Severity and Likelihood of Health Impacts in Seoul, Korea. International Journal of Environmental Research and Public Health. 2021; 18(5):2380. https://doi.org/10.3390/ijerph18052380
Chicago/Turabian StyleChae, Yeora, and Jongchul Park. 2021. "Analysis on Effectiveness of Impact Based Heatwave Warning Considering Severity and Likelihood of Health Impacts in Seoul, Korea" International Journal of Environmental Research and Public Health 18, no. 5: 2380. https://doi.org/10.3390/ijerph18052380
APA StyleChae, Y., & Park, J. (2021). Analysis on Effectiveness of Impact Based Heatwave Warning Considering Severity and Likelihood of Health Impacts in Seoul, Korea. International Journal of Environmental Research and Public Health, 18(5), 2380. https://doi.org/10.3390/ijerph18052380






