Assessment of Optimism in Women with Polycystic Ovary Syndrome: A Case Control-Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Materials
2.4. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Lizneva, D.; Suturina, L.; Walker, W.; Brakta, S.; Gavrilova-Jordan, L.; Azziz, R. Criteria, prevalence, and phenotypes of polycystic ovary syndrome. Fertil. Steril. 2016, 106, 6–15. [Google Scholar] [CrossRef] [PubMed]
- Rzońca, E.; Iwanowicz-Palus, G.; Bień, A.; Wdowiak, A.; Szymański, R.; Chołubek, G. Generalized Self-Efficacy, Dispositional Optimism, and Illness Acceptance in Women with Polycystic Ovary Syndrome. Int. J. Environ. Res. Public Health 2018, 15, 2484. [Google Scholar] [CrossRef]
- Teede, H.; Deeks, A.; Moran, L. Polycystic ovary syndrome: A complex condition with psychological, reproductive and meta-bolic manifestations that impacts on health across the lifespan. BMC Med. 2010, 8, 1–10. [Google Scholar] [CrossRef]
- Denny, E. “I Never Know From One Day to Another How I Will Feel”: Pain and Uncertainty in Women With Endometriosis. Qual. Health Res. 2009, 19, 985–995. [Google Scholar] [CrossRef]
- Hinz, A.; Sander, C.; Glaesmer, H.; Brähler, E.; Zenger, M.; Hilbert, A.; Kocalevent, R.-D. Optimism and pessimism in the general population: Psychometric properties of the Life Orientation Test (LOT-R). Int. J. Clin. Health Psychol. 2017, 17, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Avvenuti, G.; Baiardini, I.; Giardini, A. Optimism’s Explicative Role for Chronic Diseases. Front. Psychol. 2016, 7, 295. [Google Scholar] [CrossRef] [PubMed]
- Carver, C.S.; Scheier, M.F.; Segerstrom, S.C. Optimism. Clin. Psychol. Rev. 2010, 30, 879–889. [Google Scholar] [CrossRef] [PubMed]
- Carver, C.S.; Scheier, M.F. Dispositional optimism. Trends Cogn. Sci. 2014, 18, 293–299. [Google Scholar] [CrossRef]
- Moyer, C.A.; Fontana, R.J.; Hussain, K.; Lok, A.S.F.; Schwartz, S. The Role of Optimism/Pessimism in HRQOL in Chronic Hepatitis C Patients. J. Clin. Psychol. Med. Settings 2003, 10, 41–49. [Google Scholar] [CrossRef]
- Thornton, A.A.; Perez, M.A.; Oh, S.; Crocitto, L. Optimism and Prostate Cancer-Specific Expectations Predict Better Quality of Life after Robotic Prostatectomy. J. Clin. Psychol. Med. Settings 2011, 19, 165–176. [Google Scholar] [CrossRef] [PubMed]
- Carver, C.S.; Scheier, M.F. On the Self-Regulation of Behavior; Cambridge University Press: Cambridge, UK, 1998. [Google Scholar]
- Schwarzer, R. Optimism, Vulnerability, and self-beliefs as health-related cognitions: A systematic overview. Psychol. Health 1994, 9, 161–180. [Google Scholar] [CrossRef]
- Scheier, M.F.; Carver, C.S. Dispositional optimism and physical health: A long look back, a quick look forward. Am. Psychol. 2018, 73, 1082–1094. [Google Scholar] [CrossRef]
- Burger, J.M.; Palmer, M.L. Changes in and Generalization of Unrealistic Optimism Following Experiences with Stressful Events: Reactions to the 1989 California Earthquake. Pers. Soc. Psychol. Bull. 1992, 18, 39–43. [Google Scholar] [CrossRef]
- Sweeny, K.; Carroll, P.J.; Shepperd, J.A. Is Optimism Always Best? Curr. Dir. Psychol. Sci. 2006, 15, 302–306. [Google Scholar] [CrossRef]
- Jason, L.A.; Witter, E.; Torres-Harding, S. Chronic fatigue syndrome, coping, optimism and social support. J. Ment. Health 2003, 12, 109–118. [Google Scholar] [CrossRef]
- Sánchez-Ferrer, M.L.; Prieto-Sánchez, M.T.; Corbalán-Biyang, S.; Mendiola, J.; Adoamnei, E.; Hernández-Peñalver, A.I.; Carmona-Barnosi, A.; Salido-Fiérrez, E.J.; Torres-Cantero, A.M. Are there differences in basal thrombophilias and C-reactive protein between women with or without PCOS? Reprod. Biomed. Online 2019, 38, 1018–1026. [Google Scholar] [CrossRef]
- Cooney, L.G.; Dokras, A. Beyond fertility: Polycystic ovary syndrome and long-term health. Fertil. Steril. 2018, 110, 794–809. [Google Scholar] [CrossRef] [PubMed]
- Brutocao, C.; Zaiem, F.; Alsawas, M.; Morrow, A.S.; Murad, M.H.; Javed, A. Psychiatric disorders in women with polycystic ovary syndrome: A systematic review and meta-analysis. Endocrine 2018, 62, 318–325. [Google Scholar] [CrossRef]
- Cooney, L.G.; Lee, I.; Sammel, M.D.; Dokras, A. High prevalence of moderate and severe depressive and anxiety symptoms in polycystic ovary syndrome: A systematic review and meta-analysis. Hum. Reprod. 2017, 32, 1075–1091. [Google Scholar] [CrossRef]
- Blay, S.L.; Aguiar, J.V.A.; Passos, I.C. Polycystic ovary syndrome and mental disorders: A systematic review and exploratory me-ta-analysis. Neuropsychiatr. Dis. Treat. 2016, 12, 2895–2903. [Google Scholar] [CrossRef] [PubMed]
- Sayyah-Melli, M.; Alizadeh, M.; Pourafkary, N.; Ouladsahebmadarek, E.; Jafari-Shobeiri, M.; Abbassi, J.; Kazemi-Shishvan, M.A.; Sedaghat, K. Psychosocial Factors Associated with Polycystic Ovary Syndrome: A Case Control Study. J. Caring Sci. 2015, 4, 225–231. [Google Scholar] [CrossRef]
- Gustin, S.M.; Burke, L.A.; Peck, C.C.; Murray, G.M.; Henderson, L.A. Pain and Personality: Do Individuals with Different Forms of Chronic Pain Exhibit a Mutual Personality? Pain Pract. 2016, 16, 486–494. [Google Scholar] [CrossRef] [PubMed]
- Aguirre-Camacho, A.; Moreno-Jiménez, B. Depression and Anxiety in Patients with Pulmonary Hypertension: The Role of Life Satisfaction and Optimism. J. Psychosom. Res. 2018, 59, 575–583. [Google Scholar] [CrossRef]
- Bleil, M.E.; Pasch, L.A.; Gregorich, S.E.; Millstein, S.G.; Katz, P.P.; Adler, N.E. Fertility treatment response: Is it better to be more optimistic or less pessimistic? Psychosom. Med. 2012, 74, 193. [Google Scholar] [CrossRef] [PubMed]
- Morán-Sánchez, I.; Adoamnei, E.; Sánchez-Ferrer, M.L.; Prieto-Sánchez, M.T.; Arense-Gonzalo, J.J.; Casanova-Mompeán, V.; Carmona-Barnosi, A.; Mendiola, J.; Torres-Cantero, A.M. Is dispositional optimism associated with endometriomas and deep infiltrating endometriosis? J. Psychosom. Obstet. Gynecol. 2020, 21, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Ferrer, M.L.; Mendiola, J.; I Hernández-Peñalver, A.; Corbalán-Biyang, S.; Carmona-Barnosi, A.; Prieto-Sánchez, M.T.; Nieto, A.; Torres-Cantero, A.M. Presence of polycystic ovary syndrome is associated with longer anogenital distance in adult Mediterranean women. Hum. Reprod. 2017, 32, 2315–2323. [Google Scholar] [CrossRef]
- Ferriman, D.; Gallwey, J.D. Clinical Assessment of body hair growth in women. J. Clin. Endocrinol. Metab. 1961, 21, 1440–1447. [Google Scholar] [CrossRef] [PubMed]
- Afifi, L.; Saeed, L.; Pasch, L.A.; Huddleston, H.G.; Cedars, M.I.; Zane, L.T.; Shinkai, K. Association of ethnicity, Fitzpatrick skin type, and hirsutism: A retrospective cross-sectional study of women with polycystic ovarian syndrome. Int. J. Women’s Dermatol. 2017, 3, 37–43. [Google Scholar] [CrossRef]
- Conway, G.; Dewailly, D.; Diamanti-Kandarakis, E.; Escobar-Morreale, H.F.; Franks, S.; Gambineri, A.; Kelestimur, F.; Macut, D.; Micic, D.; Pasquali, R.; et al. The polycystic ovary syndrome: A position statement from the Euro-pean Society of Endocrinology. Eur. J. Endocrinol. 2014, 171, P1–P29. [Google Scholar] [CrossRef]
- Facchin, F.; Barbara, G.; Saita, E.; Mosconi, P.; Roberto, A.; Fedele, L.; Vercellini, P. Impact of endometriosis on quality of life and mental health: Pelvic pain makes the difference. J. Psychosom. Obstet. Gynecol. 2015, 36, 135–141. [Google Scholar] [CrossRef]
- Vilagut, G.; Valderas, J.M.; Ferrer, M.; Garin, O.; López-García, E.; Alonso, J. Interpretation of SF-36 and SF-12 Questionnaires in Spain: Physical and Mental Components. Med. Clin. 2008, 130, 726–735. [Google Scholar] [CrossRef]
- Ware, J.E.; Kosinski, M.; Turner-Bowker, D.M.; Gandek, B. How to Score Version 2 of the SF-12 Health Survey (with a Supplement Documenting Version 1), 1st ed.; Quality Metric Incorporated: Lincoln, RI, USA, 2002. [Google Scholar]
- Piqueras, O.M.; Arizaleta, L.H.; Rodríguez, J.A.P. Population based norms of the Spanish version of the SF-12V2 for Murcia (Spain). Gac. Sanit. 2011, 25, 50–61. [Google Scholar]
- Scheier, M.F.; Carver, C.S.; Bridges, M.W. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. J. Pers. Soc. Psychol. 1994, 67, 1063–1078. [Google Scholar] [CrossRef] [PubMed]
- Ferrando, P.J.; Chico, E.; Tous, J.M. Propiedades psicométricas del test de optimismo Life Orientation Test. Psicothema 2002, 14, 673–680. [Google Scholar]
- Facchin, F.; Barbara, G.; Saita, E.; Erzegovesi, S.; Martoni, R.M.; Vercellini, P. Personality in women with endometriosis: Temperament and character dimensions and pelvic pain. Hum. Reprod. 2016, 31, 1515–1521. [Google Scholar] [CrossRef]
- Sánchez-Román, S.; Téllez-Zenteno, J.F.; Zermeño-Phols, F.; García-Ramos, G.; Velázquez, A.; Derry, P.; Hernández, M.; Resendiz, A.; Guevara-López, U.M. Personality in patients with migraine evaluated with the “Temperament and Character Inventory”. J. Headache Pain 2007, 8, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Fishbain, D.A.; Cole, B.; Cutler, R.B.; Lewis, J.; Rosomoff, H.L.; Rosomoff, R.S. Chronic Pain and the Measurement of Personality: Do States Influence Traits? Pain Med. 2006, 7, 509–529. [Google Scholar] [CrossRef]
- Buggio, L.; Barbara, G.; Facchin, F.; Frattaruolo, M.P.; Aimi, G.; Berlanda, N. Self-management and psychological-sexological interventions in patients with endometriosis: Strategies, outcomes, and integration into clinical care. Int. J. Womens Health 2017, 9, 281–293. [Google Scholar] [CrossRef] [PubMed]
- Fournier, M.; De Ridder, D.; Bensing, J. Is Optimism Sensitive to the Stressors of Chronic Disease? The Impact of Type 1 Diabetes Mellitus and Multiple Sclerosis on Optimistic Beliefs. Psychol. Health 2003, 18, 277–294. [Google Scholar] [CrossRef]
- Aerts, L.; Grangier, L.; Streuli, I.; Dällenbach, P.; Marci, R.; Wenger, J.-M.; Pluchino, N. Psychosocial impact of endometriosis: From co-morbidity to intervention. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 50, 2–10. [Google Scholar] [CrossRef]
| Variable | Cases (n = 117) | Controls (n = 156) | p-Value * |
|---|---|---|---|
| Age (years), (mean and SD) | 27.2 (5.0) | 30.7 (5.9) | <0.001 |
| Body Mass Index (Kg/m2), (mean and SD) | 25.5 (5.9) | 23.4 (4.5) | 0.001 |
| Marital status, n (%) | |||
| Single or divorced | 56 (47.9) | 76 (48.7) | 0.89 |
| Married | 61 (52.1) | 80 (51.3) | |
| Educational level, n (%) | |||
| Primary | 25 (21.9) | 15 (9.7) | 0.001 |
| Secondary | 38 (33.3) | 39 (25.2) | |
| University | 51 (44.7) | 101 (65.2) | |
| Employment status, n (%) | |||
| Unemployed | 24 (21.2) | 22 (14.1) | 0.09 |
| Studying | 32 (28.3) | 35 (22.4) | |
| Working | 57 (50.4) | 99 (63.5) | |
| Infertility/sterility problems, n (%) | 24 (20.5) | 13 (8.4) | <0.001 |
| Bodily pain (mean and SD) ** | 81.3 (24.6) | 90.5 (18.3) | <0.001 |
| Psychiatric medication, n (%) | |||
| Anxiolytics | 8 (6.8) | 9 (5.8) | 0.73 |
| Antidepressants | 6 (5.1) | 6 (3.9) | 0.63 |
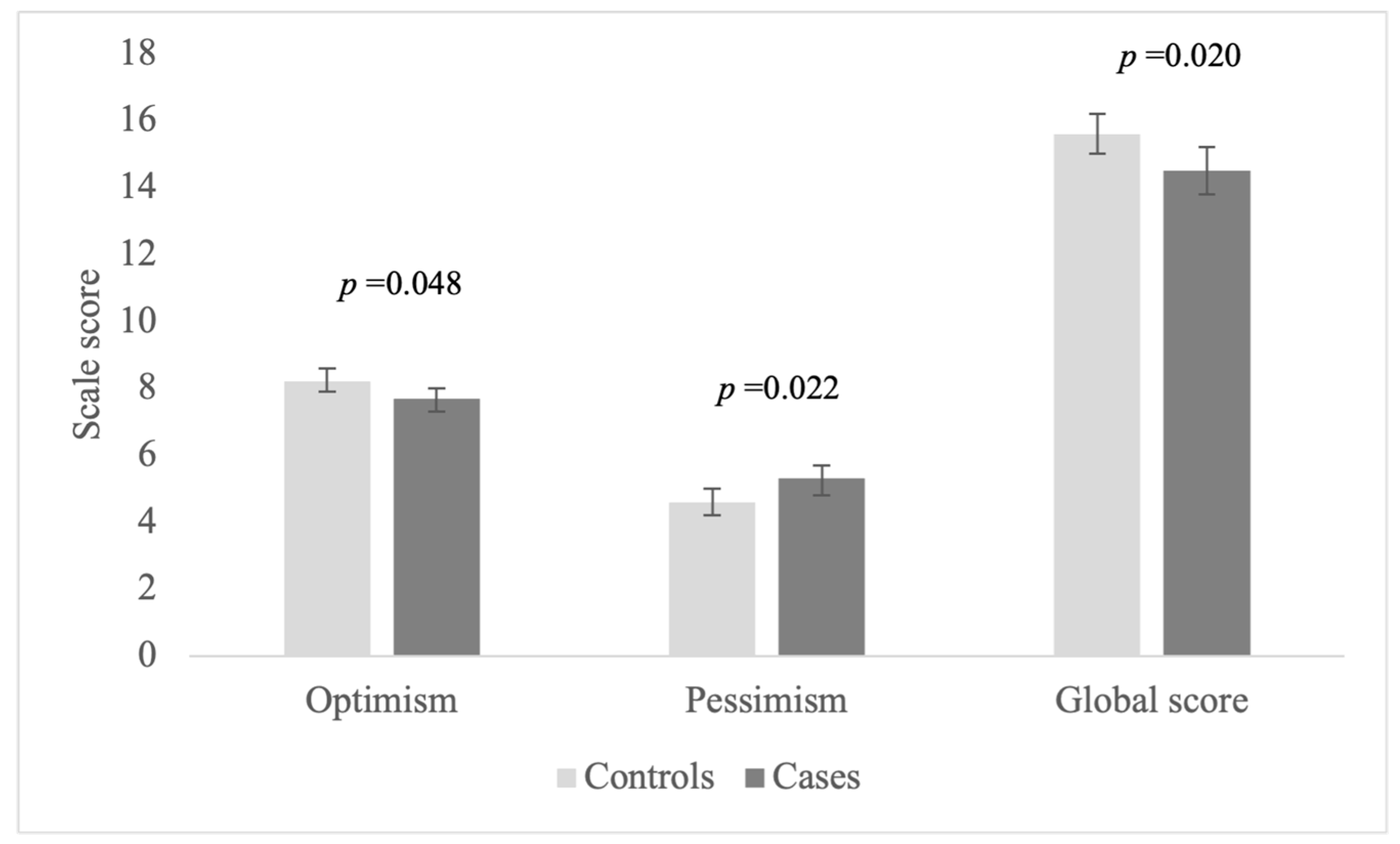
| LOT-R Variables | Cases (n = 117) | Controls (n = 156) | p-Value a | Adjusted p-Value |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||
| LOT optimism | 7.7 (2.3) | 8.3 (1.9) | 0.03 | 0.048 b |
| LOT pessimism | 5.6 (2.6) | 4.3 (2.2) | <0.01 | 0.022 c |
| LOT global score | 14.1 (3.9) | 15.9 (3.2) | <0.01 | 0.020 d |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morán-Sánchez, I.; Adoamnei, E.; Sánchez-Ferrer, M.L.; Prieto-Sánchez, M.T.; Arense-Gonzalo, J.J.; Carmona-Barnosi, A.; Hernandez-Peñalver, A.I.; Mendiola, J.; Torres-Cantero, A.M. Assessment of Optimism in Women with Polycystic Ovary Syndrome: A Case Control-Study. Int. J. Environ. Res. Public Health 2021, 18, 2352. https://doi.org/10.3390/ijerph18052352
Morán-Sánchez I, Adoamnei E, Sánchez-Ferrer ML, Prieto-Sánchez MT, Arense-Gonzalo JJ, Carmona-Barnosi A, Hernandez-Peñalver AI, Mendiola J, Torres-Cantero AM. Assessment of Optimism in Women with Polycystic Ovary Syndrome: A Case Control-Study. International Journal of Environmental Research and Public Health. 2021; 18(5):2352. https://doi.org/10.3390/ijerph18052352
Chicago/Turabian StyleMorán-Sánchez, Inés, Evdochia Adoamnei, María L. Sánchez-Ferrer, María T. Prieto-Sánchez, Julián J. Arense-Gonzalo, Ana Carmona-Barnosi, Ana I. Hernandez-Peñalver, Jaime Mendiola, and Alberto M. Torres-Cantero. 2021. "Assessment of Optimism in Women with Polycystic Ovary Syndrome: A Case Control-Study" International Journal of Environmental Research and Public Health 18, no. 5: 2352. https://doi.org/10.3390/ijerph18052352
APA StyleMorán-Sánchez, I., Adoamnei, E., Sánchez-Ferrer, M. L., Prieto-Sánchez, M. T., Arense-Gonzalo, J. J., Carmona-Barnosi, A., Hernandez-Peñalver, A. I., Mendiola, J., & Torres-Cantero, A. M. (2021). Assessment of Optimism in Women with Polycystic Ovary Syndrome: A Case Control-Study. International Journal of Environmental Research and Public Health, 18(5), 2352. https://doi.org/10.3390/ijerph18052352









