The Impact of Education, COVID-19 and Risk Factors on the Quality of Life in Patients with Type 2 Diabetes
Abstract
1. Introduction
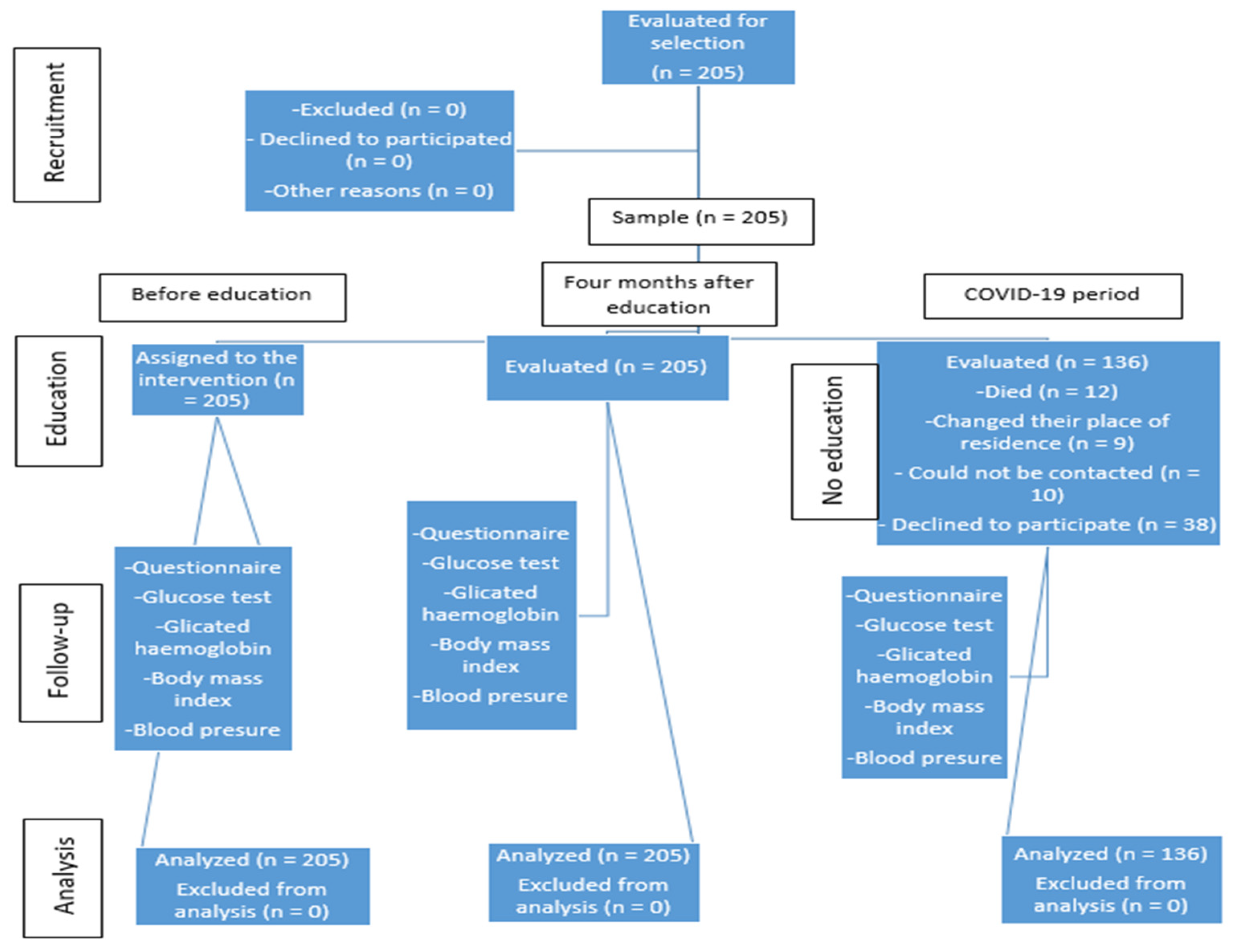
2. Materials and Methods
2.1. Study Tools
2.2. Ethical Consideration
2.3. Statistical Analysis
3. Results
3.1. Socio-Demographic Characteristics
3.2. Diabetes Health Parameters before and after Education and during the COVID-19 Period
3.3. Quality of Life by Domains before and after Education and in the COVID-19 Period, and Differences Regarding Gender, Place of Residence and Age
3.4. Self-Assessment of Behavior during the COVID-19 Pandemic
3.5. Predictors of Worse Quality of Life in Patients with Type 2 Diabetes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- IDF. Diabetes Atlas, 9th ed.; International Diabetes Federation IDF: Brussels, Belgium, 2019; Available online: https://www.diabetesatlas.org/en/ (accessed on 22 July 2020).
- Buse, J.B.; Polonsky, K.S.; Burant, C.F. Type 2 Diabetes Mellitus. In Williams Textbook of Endocrinology, 12th ed.; Melmed, S., Polonsky, K.S., Larsen, P.R., Kronenberg, H.M., Eds.; Saunders: Philadelphia, PA, USA, 2011. [Google Scholar]
- Angelidi, A.M.; Belanger, M.J.; Mantzoros, C.S. Commentary: COVID-19 and diabetes mellitus: What we know, how our patients should be treated now, and what should happen next. Metabolism 2020, 107, 154245. [Google Scholar] [CrossRef]
- Croatian Institute of Public Health. Diabetes in the Republic of Croatia 2019. Available online: https://www.hzjz.hr/aktualnosti/svjetski-dan-secerne-bolesti-2019/ (accessed on 20 July 2020).
- Holman, R.R.; Paul, S.K.; Bethel, M.A.; Matthews, D.R.; Neil, H.A. 10-year follow-up of intensive glucose control in type 2 diabetes. N. Engl. J. Med. 2008, 359, 1577–1589. [Google Scholar] [CrossRef]
- Funnell, M.M.; Brown, T.L.; Childs, B.P.; Haas, L.B.; Hosey, G.M.; Jensen, B.; Kent, D. National Standards for diabetes self-management education. Diabetes Care 2011, 34 (Suppl. 1), S89–S96. [Google Scholar] [CrossRef] [PubMed]
- Riemenschneider, H.; Saha, S.; van den Broucke, S.; Maindal, T.H.; Doyle, G.; Zamir, D.L. State of diabetes self-management education in the European Union member states and non-EU countries: The diabetes literacy project. J. Diabetes Res. 2018, 2018, 1467171. [Google Scholar] [CrossRef] [PubMed]
- Beck, J.; Greenwood, D.A.; Blanton, L.; Bollinger, S.T.; Butcher, M.K.; Condon, J.E.; Jodi, L. 2017 National standards for diabetes self-management education and support. Diabetes Care 2017, 40, 1409–1419. [Google Scholar] [CrossRef]
- Zang, Y.; Chu, L. Effectivenes of systematic health education model for type 2 diabetes patients. Int. J. Endocrinol. 2018, 2018, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Gallivan, J.; Greenberg, R.; Brown, C. The National Diabetes Education Program evaluation framework: How to design an evaluation of a multifaceted public health education program. Prev. Chronic Dis. 2008, 5, A134. [Google Scholar] [PubMed]
- Gvozdanović, Z.; Farčić, N.; Placento, H.; Lovrić, R.; Dujmić, Ž.; Jurić, A.; Miškić, B.; Prlić, N. Diet education as a success factor of glycemia regulation in diabetes patients: A prospective study. Int. J. Environ. Res. Public Health 2019, 16, 4003. [Google Scholar] [CrossRef]
- Boren, S.A.; Fitzner, K.A.; Panhalkar, P.S.; Specker, J.E. Costs and benefits associated with diabetes education: A review of the literature. Diabetes Educ. 2009, 35, 72–96. [Google Scholar] [CrossRef] [PubMed]
- Evans, N.R.; Richardson, L.S.; Dhatariya, K.K.; Sampson, M.J. Diabetes specialist nurse telemedicine: Admissions avoidance, costs and casemix. Eur. Diab. Nurs. 2012, 9, 17–21. [Google Scholar] [CrossRef]
- Vig, S.; Sevak, L. Diabetes specialist nursing: Apivotal role to play in the care of the diabetic foot. J. Diab. Nurs. 2012, 16, 206–208. [Google Scholar]
- American Diabetes Association. Strategies for improving care. Diabetes Care 2015, 38 (Suppl. 1), 5–7. [Google Scholar] [CrossRef] [PubMed]
- Burke, S.D.; Sherr, D.; Lipman, R.D. Partnering with diabetes educators to improve patient outcomes. Diabetes Metab. Syndr. Obes. 2014, 7, 45–53. [Google Scholar] [CrossRef]
- Reyes-Olavarría, D.; Latorre-Román, P.Á.; Guzmán-Guzmán, I.P.; Jerez-Mayorga, D.; Caamaño-Navarrete, F.; Delgado-Floody, P. Positive and negative changes in food habits, physical activity patterns, and weight status during COVID-19 confinement: Associated factors in the Chilean population. Int. J. Environ. Res. Public Health 2020, 17, 5431. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Ran, L.; Liu, Q.; Hu, Q.; Du, X.; Tan, X. Hand hygiene, mask-wearing behaviors and its associated factors during the COVID-19 epidemic: A cross-sectional study among primary school students in Wuhan, China. Int. J. Environ. Res. Public Health 2020, 17, 2893. [Google Scholar] [CrossRef] [PubMed]
- Roncon, L.; Zuin, M.; Rigatelli, G.; Zuliani, G. Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome. J. Clin. Virol. 2020, 127, 104354. [Google Scholar] [CrossRef]
- Emami, A.; Javanmardi, F.; Pirbonyeh, N.; Akbari, A. Prevalence of underlying diseases in hospitalized patients with COVID-19: A systematic review and meta-analysis. Arch. Acad. Emerg. Med. 2020, 8, e35. [Google Scholar] [PubMed]
- Hartmann-Boyce, J.; Morris, E.; Goyder, C.; Kinton, J.; Perring, J.; Nunan, D. Diabetes and COVID-19: Risks, management, and learnings from other national disasters. Diabetes Care 2020, 43, 1695–1703. [Google Scholar] [CrossRef]
- Khan, M.A.; Moverley Smith, J.E. “Covibesity,” a new pandemic. Obes. Med. 2020, 19, 100282. [Google Scholar]
- International Curriculum for Diabetes Health Professional Education; International Diabetes Federation [IDF]: Brussels, Belgium, 2008; Available online: https://www.idf.org/e-library/education/64-the-internationalcurriculum-for-diabetes-health-professional-education,en.html (accessed on 15 October 2018).
- American Diabetes Association. Standards of medical care in diabetes 2012. Diabetes Care 2012, 35, 11–63. [Google Scholar] [CrossRef]
- Palamenghi, L.; Carlucci, M.M.; Graffigna, G. Measuring the quality of life in diabetic patients: A scoping review. J. Diabetes Res. 2020, 2020, 1–19. [Google Scholar] [CrossRef]
- Ferrens, C.E.; Powers, M.J. The Quality of Life Index (QLI)–Diabetes III Version. 1998. Available online: https://qli.org.uic.edu/questionaires/questionnairehome.htm (accessed on 22 July 2020).
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front Psychol. 2013, 4, 863. [Google Scholar] [CrossRef]
- Gagliardino, J.J.; Chantelot, J.M.; Domenger, C.; Ramachandran, A.; Kaddaha, G.; Mbanya, C.; Chan, J. Impact of diabetes education and self-management of the quality of care for people with type 1 diabetes mellitus in the Middle East. Diabetes Res. Clin. Pract. 2019, 147, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Trento, M.; Passera, P.; Borgo, E.; Tomalino, M.; Bajardi, M.; Cavallo, F.; Porta, M. A 5-year randomized controlled study of learning, problem solving ability and quality of life modifications in people with type 2 diabetes managedby group care. Diabetes Care 2004, 27, 670–675. [Google Scholar] [CrossRef]
- Lee, S.K.; Shin, D.H.; Kim, Y.H.; Lee, K.S. Effect of diabetes education through pattern management on self-care and self-efficacy in patients with Type 2 Diabetes. Int. J. Environ. Res. Public Health 2019, 16, 3323. [Google Scholar] [CrossRef] [PubMed]
- Scain, S.F.; Friedman, R.; Gross, J.L. A structured educational program improves metabolic control in patients with type 2 diabetes: A randomized controlled trial. Diabetes Educ. 2009, 35, 603–611. [Google Scholar] [CrossRef] [PubMed]
- Gillani, S.W.; Ansari, I.A.; Zaghloul, H.A.; Abdul, M.I.M.; Sulaiman, S.A.S.; Baig, M.R. Bridging glycated hemoglobin with quality of life and health state; a randomized case–control study among type 2 diabetes patients. Diabetol. Metab. Syndr. 2018, 10, 23. [Google Scholar] [CrossRef]
- Lau, C.Y.; Qureshi, A.K.; Scott, S.G. Association between glycaemic control and quality of life in diabetes mellitus. J. Postgrad. Med. 2004, 50, 189–194. Available online: https://www.jpgmonline.com/text.asp?2004/50/3/189/12571 (accessed on 22 July 2020). [PubMed]
- Hsu, H.C.; Lee, Y.J.; Wang, R.H. Influencing pathways to Quality of Life and HbA1c in patients with diabetes: AlLongitudinal study that inform evidence-based practice. Worldviews Evid. Based. Nurs. 2018, 15, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Redwood-Campbell, L.; Abrahams, J. Primary health care and disasters-the current state of the literature: What we know, gaps and next steps. Prehosp. Disaster Med. 2011, 26, 184–191. [Google Scholar] [CrossRef] [PubMed]
- Mostafa, N.M.; Ahmed, G.H.; Anwar, W. Effect of educational nursing program on quality of life for patients with type II diabetes mellitus at Assiut University Hospital. J. Nurs. Educ. Pract. 2018, 8, 11. [Google Scholar] [CrossRef]
- Antunes, R.; Frontini, R.; Amaro, N.; Salvador, R.; Matos, R.; Morouço, P. Exploring lifestyle habits, physical activity, anxiety and basic psychological needs in a sample of Portuguese adults during COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 4360. [Google Scholar] [CrossRef]
- Prajapati, V.B.; Blake, R.; Acharya, L.D.; Seshadri, S. Assessment of quality of life in type II diabetic patients using the modified diabetes quality of life (MDQoL)-17 questionnaire. Braz. J. Pharm. Sci. 2017, 53, e17144. [Google Scholar] [CrossRef]
- Albader, A.S.; Albahlei, S.; Almishary, M. Measuring quality of life in type 2 diabetic patients at the Al-Wazarat Healthcare Center in Riyadh. Cureus 2019, 11, e6474. [Google Scholar] [CrossRef] [PubMed]
- de las Heras-Pedrosa, C.; Sánchez-Núñez, P.; Peláez, J.I. Sentiment analysis and emotion understanding during the COVID-19 pandemic in Spain and its impact on digital ecosystems. Int. J. Environ. Res. Public Health 2020, 17, 5542. [Google Scholar] [CrossRef]
- Joensen, L.E.; Madsen, K.P.; Holm, L.; Nielsen, K.A.; Rod, M.H.; Petersen, A.A.; Rod, N.; Willaing, I. Diabetes and COVID-19: Psychosocial consequences of the COVID-19 pandemic in people with diabetes in Denmark-what characterizes people with high levels of COVID-19-related worries? Diabet. Med. 2020, 37, 1146–1154. [Google Scholar] [CrossRef] [PubMed]
- Wicaksana, A.L.; Hertanti, N.S.; Ferdiana, A.; Pramono, R.B. Diabetes management and specific considerations for patients with diabetes during coronavirus diseases pandemic: A scoping review. Diabetes Metab. Syndr. 2020, 14, 1109–1120. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Roso, M.B.; Knott-Torcal, C.; Matilla-Escalante, D.C.; Garcimartín, A.; Sampedro-Nuñez, M.A.; Dávalos, A.; Marazuela, M. COVID-19 lockdown and changes of the dietary pattern and physical activity habits in a cohort of patients with type 2 diabetes mellitus. Nutrients. 2020, 12, 2327. [Google Scholar] [CrossRef]
- Han, X.; Wang, J.; Zhang, M.; Wang, X. Using social media to mine and analyze public opinion related to COVID-19 in China. Int. J. Environ. Res. Public Health 2020, 17, 2788. [Google Scholar] [CrossRef] [PubMed]
- Nazir, M.; Hussain, I.; Tian, J.; Akram, S.; Mangenda Tshiaba, S.; Mushtaq, S.; Shad, M.A. A multidimensional model of public health approaches against COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 3780. [Google Scholar] [CrossRef]
- Alshareef, R.; Al Zahrani, A.; Alzahrani, A.; Ghandoura, L. Impact of the COVID-19 lockdown on diabetes patients in Jeddah, Saudi Arabia. Diabetes Metab. Syndr. 2020, 14, 1583–1587. [Google Scholar] [CrossRef]
- Pal, R.; Bhadada, S.K. COVID-19 and diabetes mellitus: An unholy interaction of two pandemics. Diabetes Metab. Syndr. 2020, 14, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Baghianimoghadam, M.H.; Ardekani, M.; Baghianimoghadam, B. Effect of education on improvement of quality of life by SF-20 in type 2 diabetic patients. Acta. Med. Indones. 2009, 41, 175–180. [Google Scholar] [PubMed]
- Petersen, B.; Vesper, I.; Pachwald, B.; Dagenbach, N.; Buck, S.; Waldenmaier, D.; Heinemann, L. Diabetes management intervention studies: Lessons learned from two studies. Trials 2021, 22, 61. [Google Scholar] [CrossRef] [PubMed]
- Trikkalinou, A.; Papazafiropoulou, A.K.; Melidonis, A. Type 2 diabetes and quality of life. World J. Diabetes 2017, 8, 120–129. [Google Scholar] [CrossRef] [PubMed]
- Lael-Monfared, E.; Tehrani, H.; Teiho, Z.; Jafari, A. The study of eye care behaviors in patients with type 2 diabetes. J. Diabetes Metab Disord. 2020, 19, 257–263. [Google Scholar] [CrossRef]
| Sociodemographic Characteristics | [n (%)] |
|---|---|
| Gender [n (%)] | |
| Male | 111 (54) |
| Female | 94 (46) |
| Age [n (%)] | |
| up to 50 years | 23 (11) |
| 51–60 years | 73 (36) |
| 61–70 years | 73 (36) |
| 71 and older | 36 (18) |
| Level of education [n (%)] | |
| Unfinished primary school | 14 (7) |
| Elementary school | 54 (26) |
| High school education | 99 (49) |
| Higher education | 37 (18) |
| Place of residence [n (%)] | |
| Rural | 123 (60) |
| Urban | 82 (40) |
| Marriage status [n (%)] | |
| Unmarried | 19 (9) |
| Married | 149 (73) |
| Divorced | 7 (3) |
| Widower | 29 (14) |
| Minor children in the family [n (%)] | 46 (22) |
| Family members over the age of 60 [n (%)] | 93 (45) |
| Duration of diabetes (years) [n (%)] | |
| Up to a year | 25 (13) |
| 2–5 | 83 (41) |
| 6–10 | 50 (25) |
| 11–15 | 23 (11) |
| ≥16 | 21 (10) |
| Health Parameters | Median (Interquartile Range) | p * | Effect Size (Cohen’s d) | ||||
|---|---|---|---|---|---|---|---|
| Before Education (1) | After Education (2) | COVID-19 Period (3) | 1 vs. 2 | 1 vs. 3 | 2 vs. 3 | ||
| Blood glucose [fasted] | 7.3 (6.2–8.7) | 7.1 (6.1–8.3) | 7 (5.8–8.3) | 0.34 | 0.01 | 0.07 | 0.11 |
| HbA1c [%] | 6.7 (6–7.7) | 6.6 (6–7.3) | 6.4 (5.7–7.1) | 0.002 † | 0.19 | 0.04 | 0.08 |
| Systolic pressure (mmHg) | 130 (120–140) | 130 (120–140) | 130 (120–140) | 0.54 | 0.10 | 0.12 | 0.03 |
| Diastolic pressure (mmHg) | 80 (75–90) | 80 (75–90) | 80 (80–90) | 0.53 | 0.03 | 0.14 | 0.09 |
| Weight (kg) | 90 (78–102) | 89 (76.8–100) | 88 (75–102) | <0.001 † | 0.07 | 0.02 | 0.05 |
| BMI (kg/m2) | 31 (27.6–34) | 30.8 (27.5–34) | 31 (27.5–34) | 0.008 ‡ | 0.06 | 0.02 | 0.03 |
| Satisfaction with the Surrounding Life | Median (Interquartile Range) | p * | Effect Size (Cohen’s d) | ||||
|---|---|---|---|---|---|---|---|
| Before Education (1) | After Education (2) | COVID-19 Period (3) | 1 vs. 2 | 1 vs. 3 | 2 vs. 3 | ||
| Health and functioning | 21.3 (17.8–24.4) | 21.5 (18.4–24.8) | 13.4 (12.3–15.2) | <0.001 † | 0.06 | 2.12 | 2.19 |
| Male | 20.8 (17.7–24.0) | 21.3 (18–24.4) | 13.1 (11.9–14.5) | <0.001 † | 0.03 | 2.20 | 2.25 |
| Female | 22.3 (18.0–24.6) | 22.4 (19.1–25.3) | 14.4 (12.8–16) | <0.001 ‡ | 0.10 | 2.07 | 2.17 |
| Rural | 20.9 (17.5–24.0) | 21.3 (18–24.4) | 13.4 (12–15.2) | <0.001 † | 0.05 | 1.98 | 2.05 |
| Urban | 22.4 (18.0–24.8) | 22.2 (18.6–25.7) | 13.5 (12.4–15.5) | <0.001 † | 0.08 | 2.36 | 2.43 |
| Age up to 62 years | 21.8 (18.5–24.4) | 21.9 (19.1–25.1) | 13.4 (12.4–15.2) | <0.001 † | 0.08 | 2.32 | 2.35 |
| ≥62 years | 20.8 (17.2–24.4) | 20.7 (17.2–24.4) | 13.4 (11.7–15.3) | <0.001 † | 0.04 | 1.93 | 2.02 |
| Socioeconomic domain | 21.6 (18–26) | 22.1 (17.9–25.8) | 23.3 (19.5–26.6) | <0.001 ‡ | 0.01 | 0.24 | 0.23 |
| Male | 21.3 (17.6–25) | 21.93 (17.6–25) | 22.7 (18.9–26.5) | <0.001 ‡ | 0.002 | 0.19 | 0.20 |
| Female | 22.1 (18.6–26.3) | 22.3 (18.9–26.2) | 23.9 (19.9–26.9) | <0.001 ‡ | 0.03 | 0.29 | 0.27 |
| Rural | 20.7 (17.5–24.6) | 20.8 (17.6–24.5) | 22.6 (18.7–26.3) | <0.001 ‡ | 0.004 | 0.31 | 0.33 |
| Urban | 23.6 (18.8–27.5) | 23.9 (18.9–27.4) | 24 (19.8–27) | 0.91 | 0.04 | 0.14 | 0.10 |
| Age up to 62 years | 23 (18.4–26.3) | 23.2 (18.9–26.2) | 23.7 (19.9–27.8) | 0.003 ‡ | 0.02 | 0.25 | 0.24 |
| ≥62 years | 20.3 (17.2–25) | 20.5 (17.2–25) | 22.6 (16.7–25.5) | 0.001 ‡ | 0.001 | 0.23 | 0.23 |
| Psychological/spiritual domain | 23.1 (19.2–26.6) | 23.6 (19.3–27) | 22.1 (18.2–25.5) | <0.001 ‡ | 0.009 | 0.20 | 0.21 |
| Male | 22.8 (17.6–26.7) | 23.1 (17.7–26.4) | 21.9 (17.9–25) | 0.03 ‡ | 0.04 | 0.19 | 0.16 |
| Female | 23.9 (20–26.6) | 24.3 (20.5–27.5) | 22.5 (18.3–26.3) | <0.001 ‡ | 0.07 | 0.21 | 0.28 |
| Rural | 23.1 (18.6–26.3) | 23.1 (18.7–26.1) | 21.7 (17.8–24.2) | <0.001 ‡ | 0.03 | 0.29 | 0.26 |
| Urban | 23.9 (19.8–28.3) | 24.3 (20.7–28.8) | 24.3 (18.6–26.8) | 0.05 | 0.07 | 0.07 | 0.15 |
| Age up to 62 years | 23.1 (18.5–27) | 23.7 (18.9–27.7) | 23.0 (20.0–26.1) | 0.12 | 0.04 | 0.05 | 0.09 |
| ≥62 years | 23.6 (19.7–26.6) | 23.6 (19.8–26.1) | 20.7 (17.2–25.0) | <0.001 ‡ | 0.04 | 0.39 | 0.36 |
| Family domain | 24.8 (21.4–28.5) | 24.6 (21.7–28.5) | 15.3 (13.2–17.3) | <0.001 ‡ | 0.04 | 2.33 | 2.42 |
| Male | 24.3 (21.4–28.8) | 24 (21.2–28.3) | 14.4 (12.9–16.8) | <0.001 ‡ | 0.02 | 2.43 | 2.44 |
| Female | 25.1 (21.3–27.7) | 25.2 (22.2–28.5) | 16.1 (13.8–18.3) | <0.001 ‡ | 0.11 | 2.24 | 2.45 |
| Rural | 24.6 (21.4–28.6) | 24.1 (21.5–28.5) | 15.1 (13–17.1) | <0.001 ‡ | 0.02 | 2.19 | 2.25 |
| Urban | 25.2 (21.3–28.2) | 25.3 (22.3–28.5) | 15.4 (13.2–17.6) | <0.001 ‡ | 0.08 | 2.58 | 2.76 |
| Age up to 62 years (n = 112) | 25.2 (21.6–28.8) | 25.3 (21.6–28.8) | 15.4 (13.5–17.3) | <0.001 ‡ | 0.06 | 2.30 | 2.43 |
| ≥62 years (n = 93) | 24.6 (20.7–27.9) | 24 (21.5–27.7) | 15.2 (12.6–17.2) | <0.001‡ | 0.01 | 2.36 | 2.43 |
| Quality of life | 22.4 (18.6–25.4) | 22.6 (18.8–25.6) | 17.7 (15.8–19.8) | <0.001 † | 0.04 | 1.29 | 1.32 |
| Male | 22.2 (18.6–25) | 22.2 (18.6–24.8) | 17.3 (15.3–19.2) | <0.001 ‡ | 0.001 | 1.33 | 1.30 |
| Female | 22.71 (19–25.7) | 23.1 (19.5–26.1) | 18.2 (16.1–20.5) | <0.001 † | 0.09 | 1.27 | 1.37 |
| Rural | 22.1 (18.3–24.8) | 22.3 (18.3–24.7) | 17.6 (15.3–19.3) | <0.001 † | 0.02 | 1.24 | 1.23 |
| Urban | 22.9 (19.2–26.6) | 23.5 (19.9–26.7) | 18 (16.1–20.4) | <0.001 † | 0.08 | 1.40 | 1.49 |
| Age up to 62 years | 22.5 (18.9–25.8) | 23.1 (19.5–25.9) | 18.3 (16.0–20.2) | <0.001 ‡ | 0.06 | 1.28 | 1.32 |
| ≥62 years | 21.9 (18.5–25.2) | 21.9 (18.5–24.9) | 17.6 (15.4–19.0) | <0.001 ‡ | 0.01 | 1.32 | 1.34 |
| Number (%) of Participants | ||||||
|---|---|---|---|---|---|---|
| Entirely Incorrect (0) | 1 | 2 | 3 | Entirely Exactly (4) | In Total | |
| Because of the COVID-19 pandemic, I follow the news more than I normally do | 12 (8.8) | 10 (7.4) | 24 (17.6) | 41 (30.1) | 49 (36) | 136 (100) |
| I do not think it is more dangerous than the flu | 1 | 2 | 3 | Much more dangerous from the flu | In total | |
| To what extent do you believe that COVID-19 is more dangerous than the common flu? | 9 (6.7) | 10 (7.4) | 24 (17.8) | 55 (40.7) | 37 (27.4) | 135 (100) |
| Not at all worried | 1 | 2 | 3 | Very worried | In total | |
| How worried are you about the COVID-19? | 8 (5.9) | 17 (12.5) | 20 (14.7) | 42 (30.9) | 49 (36) | 136 (100) |
| Not at all worried | 1 | 2 | 3 | Very worried | In total | |
| What is the probability that you become infected with the COVID-19 virus? | 8 (5.9) | 18 (13.3) | 36 (26.7) | 48 (35.6) | 25 (18.5) | 135 (100) |
| How likely is it that a member of your family is infected with the COVID-19 virus? | 11 (8.3) | 21 (15.8) | 37 (27.8) | 46 (34.6) | 18 (13.5) | 133 (100) |
| Number (%) | |
|---|---|
| Diabetes mellitus | 56 (27.3) |
| Lung diseases | 52 (25.4) |
| Hypertension | 25 (12.2) |
| Age | 21 (10.2) |
| Heart disease | 20 (9.8) |
| Any chronic disease | 20 (9.8) |
| Malignant diseases | 17 (8.3) |
| Asthma | 7 (3.4) |
| Obesity | 6 (2.9) |
| Compromised immune system | 3 (1.5) |
| Internal organs diseases | 2 (1) |
| Autoimmune diseases | 1 (0.5) |
| There are no risky diseases | 3 (1.5) |
| I do not know | 12 (5.9) |
| ß | Standard Error | Wald | OR | 95%CI for ß | p | |
|---|---|---|---|---|---|---|
| Quality of life | ||||||
| Male | 1.31 | 0.46 | 7.97 | 3.69 | 1.49 to 9.13 | 0.005 |
| Rural | 1.15 | 0.51 | 5.06 | 3.14 | 1.16 to 8.52 | 0.02 |
| Intercept | −4.07 | 0.78 | 26.8 | 0.02 | 0.004 to 0.07 | <0.001 |
| Health and functioning | ||||||
| Male | 0.44 | 0.17 | 6.54 | 1.56 | 1.11 to 2.21 | 0.01 |
| Intercept | −1.5 | 0.26 | 32.5 | 0.22 | 0.13 to 0.37 | <0.001 |
| Socioeconomic domain | ||||||
| - | - | - | - | - | - | - |
| Psychological/spiritual domain | ||||||
| Male | 1.14 | 0.52 | 4.81 | 3.11 | 1.13 to 8.57 | 0.03 |
| Duration of the disease (≤ 5 years) | 2.25 | 1.04 | 4.61 | 9.51 | 1.22 to 74.31 | 0.03 |
| Intercept | −4.98 | 1.26 | 15.5 | 0.007 | 0.001 to 0.08 | <0.001 |
| Family domain | ||||||
| Male | 0.89 | 0.23 | 14.3 | 2.43 | 1.53 to 3.85 | <0.001 |
| Marital status (married) | −0.65 | 0.32 | 4.29 | 0.52 | 0.28 to 0.96 | 0.04 |
| Intercept | −1.75 | 0.29 | 34.8 | 0.17 | 0.09 to 0.31 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gvozdanović, Z.; Farčić, N.; Šimić, H.; Buljanović, V.; Gvozdanović, L.; Katalinić, S.; Pačarić, S.; Gvozdanović, D.; Dujmić, Ž.; Miškić, B.; et al. The Impact of Education, COVID-19 and Risk Factors on the Quality of Life in Patients with Type 2 Diabetes. Int. J. Environ. Res. Public Health 2021, 18, 2332. https://doi.org/10.3390/ijerph18052332
Gvozdanović Z, Farčić N, Šimić H, Buljanović V, Gvozdanović L, Katalinić S, Pačarić S, Gvozdanović D, Dujmić Ž, Miškić B, et al. The Impact of Education, COVID-19 and Risk Factors on the Quality of Life in Patients with Type 2 Diabetes. International Journal of Environmental Research and Public Health. 2021; 18(5):2332. https://doi.org/10.3390/ijerph18052332
Chicago/Turabian StyleGvozdanović, Zvjezdana, Nikolina Farčić, Hrvoje Šimić, Vikica Buljanović, Lea Gvozdanović, Sven Katalinić, Stana Pačarić, Domagoj Gvozdanović, Željka Dujmić, Blaženka Miškić, and et al. 2021. "The Impact of Education, COVID-19 and Risk Factors on the Quality of Life in Patients with Type 2 Diabetes" International Journal of Environmental Research and Public Health 18, no. 5: 2332. https://doi.org/10.3390/ijerph18052332
APA StyleGvozdanović, Z., Farčić, N., Šimić, H., Buljanović, V., Gvozdanović, L., Katalinić, S., Pačarić, S., Gvozdanović, D., Dujmić, Ž., Miškić, B., Barać, I., & Prlić, N. (2021). The Impact of Education, COVID-19 and Risk Factors on the Quality of Life in Patients with Type 2 Diabetes. International Journal of Environmental Research and Public Health, 18(5), 2332. https://doi.org/10.3390/ijerph18052332






