Comparative Assessment of Female Sexual Function Following Transobturator Midurethral Sling for Stress Urinary Incontinence
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Data Collection
- Stage II and stage III stress incontinence confirmed by ultrasound scan and interview;
- hormone replacement therapy (HRT) before or after the surgical procedure;
- informed written consent of the patient to take part in the project;
- age: 45–65 years.
- women with overactive bladders (OAB) or mixed urinary incontinence (MUI);
- women with urinary tract fistulas;
- women with congenital or acquired defects of the urethra or bladder;
- women with urinary tract infections;
- women taking medicines contributing to an overactive bladder.
- Inserting a catheter in the urinary bladder;
- incision and dissection of the vaginal mucosa and fascia;
- proper insertion of the tape;
- preventing implants from wrapping and rolling up;
- avoiding infection of the implants;
- optimal tension-free stitching of vaginal walls [23].
2.2. Measures
3. Statistical Analysis
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chu, C.A.L.; Andy, U. Impact of urinary incontinence on female sexual health in women during midlife. Womens Midlife Health 2015, 1, 6. [Google Scholar] [CrossRef]
- Domingo, S.; Alamá, P.; Ruiz, N.; Lázaro, G.; Morell, M.; Pellicer, A. Transobturator tape procedure outcome: A clinical and quality of life analysis of a 1-year follow-up. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2007, 18, 895–900. [Google Scholar] [CrossRef]
- Toye, F.; Barker, K. A meta- ethnography to understand the experience of living with urinary incontinence: Is it just part and parcel of life? BMC Urol. 2020, 20, 1. [Google Scholar] [CrossRef] [PubMed]
- Roumeguère, T.; Quackels, T.; Bollens, R.; de Groote, A.; Zlotta, A.; Bossche, M.V.; Schulman, C. Trans-obturator vaginal tape (TOT) for female stress incontinence: One year follow-up in 120 patients. Eur. Urol. 2005, 48, 805–809. [Google Scholar] [CrossRef]
- Saiki, L.; Meize -Grochowski, R. Urinary Incontinence and Psychosocial Factors Associated with Intimate Relationship Satisfaction Among Midlife Women. J. Obstet. Gynecol. Neonatal Nurs. 2017, 46, 555–566. [Google Scholar] [CrossRef]
- Minassian, V.; Devore, E.; Hagan, K. Severity of urinary incontinence and effect on quality of life in women by incontinence type. Obstet. Gynecol. 2013, 121, 1083–1090. [Google Scholar] [CrossRef]
- Cayan, F.; Dilek, S.; Akbay, E.; Cayan, S. Sexual function after surgery for stress urinary incontinence: Vaginal sling versus Burch colposuspen sion. Arch. Gynecol. Obstet. 2008, 277, 31–36. [Google Scholar] [CrossRef]
- Olsson, F.; Berterö, C. Living with faecal incontinence: Trying to control the daily life that is out of control. J. Clin. Nurs. 2015, 24, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Hayder, D. The effects of urinary incontinence on sexuality: Seeking an intimate partnership. J. Wound Ostomy Cont. Nurs. 2012, 39, 539–544. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.M.; Vaughan, C.P.; Goode, P.S.; Redden, D.T.; Burgio, K.L.; Richter, H.E.; Markland, A.D. Prevalence and trends of symptomatic pelvic floor disorders in US women. Obstet. Gynecol. 2014, 123, 141–148. [Google Scholar] [CrossRef]
- Duralde, E.R.; Rowen, T.S. Urinary Incontinence and Associated Female Sexual Dysfunction. Sex Med. Rev. 2017, 5, 470–485. [Google Scholar] [CrossRef]
- Zyczynski, H.M.; Rickey, L.; Dyer, K.Y.; Wilson, T.; Stoddard, A.M.; Gormley, E.A.; Hsu, Y.; Kusek, J.W.; Brubaker, L.; Network, U.I.T. Sexual activity and function in women more than 2 years after midurethral sling placement. Am. J. Obstet. Gynecol. 2012, 207, 421.e1–421.e6. [Google Scholar] [CrossRef]
- Glavind, K.; Larsen, T.; Lindquist, A.S.I. Sexual function in women before and after tension-free vaginal tape operation for stress urinary incontinence. Acta Obstet. Gynecol. Scand. 2014, 93, 986–990. [Google Scholar] [CrossRef]
- Fürst, M.C.B.; Leite, P.H.B.; Glina, F.; Baccaglini, W.; Fürst, R.V.D.C.; Bezerra, C.A.; Glina, S. Female Sexual Function Following Surgical Treatment of Stress Urinary Incontinence: Systematic Review and Meta-Analysis. Sex Med. Rev. 2018, 6, 224–233. [Google Scholar] [CrossRef]
- Mota, R.L. Female urinary incontinence and sexuality. Int. Braz. J. Urol. 2017, 43, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Glass Clark, S.M.; Huang, Q.; Sima, A.P.; Siff, L.N. Effect of Surgery for Stress Incontinence on Female Sexual Function. Obstet. Gynecol. 2020, 135, 1232–1233. [Google Scholar] [CrossRef]
- Morgan, D.M.; Dunn, R.L.; Stoffel, J.T.; Fenner, D.E.; DeLancey, J.O.; McGuire, E.J.; Wei, J.T. Are persistent or recurrent symptoms of urinary incontinence after surgery associated with adverse effects on sexual activity or function? Int. Urogynecol. J. Pelvic Floor Dysfunct. 2008, 19, 509–515. [Google Scholar] [CrossRef]
- Laumann, E.O.; Nicolosi, A.; Glasser, D.B.; Paik, A.; Gingell, C.; Moreira, E.; Wang, T. GSSAB Investigators Group. Sexual problems among women and men aged 40–80 y: Prevalence and correlates identified in the Global Study of Sexual Attitudes and B ehaviors. Int. J. Impot. Res. 2005, 17, 39–57. [Google Scholar] [CrossRef] [PubMed]
- Salonia, A.; Munarriz, R.M.; Naspro, R.; Nappi, R.E.; Briganti, A.; Chionna, R.; Federghini, F.; Mirone, V.; Rigatti, P.; Goldstein, I.; et al. Women’s sexual dysfunction: A pathophysiological review. BJU Int. 2004, 93, 1156–1164. [Google Scholar] [CrossRef]
- Asoglu, M.R.; Selcuk, S.; Cam, C.; Cogendez, E.; Karateke, A. Effects of urinary incontinence subtypes on women’s quality of life (including sexual life) and psychosocial state. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 176, 187–190. [Google Scholar] [CrossRef] [PubMed]
- Su, C.; Sun, B.; Jiann, B. Association of urinary incontinence and sexual function in women. Int. J. Urol. Off. J. Jpn. Urol. Assoc. 2015, 22, 109–113. [Google Scholar] [CrossRef]
- Thiagamoorthy, G.; Srikrishna, S.; Cardozo, L. Sexual function after urinary incon tinence surgery. Eur. Menopause J. 2015, 81, 243–247. [Google Scholar]
- Ianoși, N.G.; Călbureanu-Popescu, M.X.; Ianoși, S.L. Impact of Hysterectomy on Urethral Suspension with Transobturator Sling for Treatment of Stress Urinary Incontinence in Women. Curr. Health Sci. J. 2019, 45, 59–65. [Google Scholar]
- Delorme, E. Transobturator urethral suspension: Mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog. Urol. 2001, 11, 1306–1313. [Google Scholar] [PubMed]
- Pacagnella, R.C.; Vieira, E.M., Jr.; Souza, C.D. Adaptação transcultural do Female Sexual Function Index. Cad. Saúde Pública. 2008, 24, 11. [Google Scholar] [CrossRef]
- Sacomori, C.; Cardoso, F.L. Predictors of improvement in sexual function of women with urinary incontinence after treatment with pelvic floor exercises: A secondary analysis. J. Sex. Med. 2015, 12, 746–755. [Google Scholar] [CrossRef] [PubMed]
- Rogers, G.R.; Villarreal, A.; Kammerer-Doak, D.; Qualls, C. Sexual function in woman with and without urinary incotinence and/or pelvic organ prolapse. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2001, 12, 361–365. [Google Scholar] [CrossRef]
- Caruso, S.; Rugolo, S.; Bandiera, S.; Mirabella, D.; Cavallaro, A.; Cianci, A. Clitoral blood flow changes after surgery for stress urinary incontinence: Pilot study on TVT Versu s TOT procedures. Urology 2007, 70, 554–557. [Google Scholar] [CrossRef] [PubMed]
- Jha, S.; Moran, P.; Greenham, H.; Ford, C. Sexual function following surgery for urodynamic stress incontinence. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2007, 18, 845–850. [Google Scholar] [CrossRef]
- Mazouni, C.; Karsenty, G.; Bretelle, F.; Bladou, F.; Gamerre, M.; Serment, G. Urinary complications and sexual function after the tension-free vaginal tape procedure. Acta Obstet. Gynecol. Scand. 2004, 83, 955–961. [Google Scholar] [CrossRef]
- Ghezzi, F.; Serati, M.; Cromi, A.; Uccella, S.; Triacca, P.; Boli, P. Impact of tension-free vaginal tape on sexual function: Results of a prospective study. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2006, 17, 54–59. [Google Scholar] [CrossRef]
- El-Azab, A.S.; Yousef, H.A.; Seifeldein, G.S. Coital incontinence: Relation to detrusor over activity and stress incontinence. Neurourol. Urodyn. 2011, 30, 520–524. [Google Scholar] [CrossRef]
- Lemack, G.E.; Litman, H.J.; Nager, C.; Brubaker, L.; Lowder, J.; Norton, P.; Sirls, L.; Lloyd, K.; Kusek, J.W. Preoperative clinical, demographic, and urodynamic measures associated with failure to demonstrate urodynamic stress incontinence in women enrolled in two randomized clinical trials of surgery for stress urinary incontinence. Int. Urogynecol. J. 2013, 24, 269–274. [Google Scholar] [CrossRef][Green Version]
- Serati, M.; Braga, A.; Di Dedda, M.C. Benefit of pelvic floor muscle therapy in improving sexual function in women with stress urinary incontinence: A pretest—Post test intervention study. J. Sex Marital Ther. 2015, 41, 254–261. [Google Scholar] [CrossRef]
- Altman, D.; Forsman, M.; Falconer, C. Genetic Influance on stress s urinary intoctinence and POP. Eur. Urol. 2007, 54, 918–922. [Google Scholar] [CrossRef]
- Fatton, B.; Tayrac, R.; Costa, P. Stress urinary incontinence and LUTS in women-effects on sexual function. Nat. Rev. Urol. 2014, 11, 565–578. [Google Scholar] [CrossRef] [PubMed]
- Komesu, Y.M.; Rogers, R.G.; Kammerer-Doak, D.N.; Barber, M.D.; Olsen, A.L. Posterior repair and sexual function. Am. J. Obstet. Gynecol. 2007, 197, 101.e1-6. [Google Scholar] [CrossRef] [PubMed]
- Nyström, E.; Sjöström, M.; Stenlund, H. ICIQ symptom and quality of life instruments measure clinically relevant improvements in women with stress urinary incontinence. Neurourol. Urodyn. 2015, 34, 747–751. [Google Scholar] [CrossRef]
- Felippe, M.R.; Zambon, J.P.; Girotti, M.E.; Burti, J.S.; Hacad, C.R.; Cadamuro, L.; Almeida, F. What Is the Real Impact of Urinary Incontinence on Female Sexual Dysfunction? A Case Control Study. Sex Med. 2017, 5, 54–60. [Google Scholar] [CrossRef][Green Version]
- Kılıç, M. Incidence and risk factors of urinary incontinence in women visiting Family Health Centers. Springerplus 2016, 5, 1331. [Google Scholar] [CrossRef]
- Lee, D.M.; Tetley, J.; Pendleton, N. Urinary incontinence and sexual health in a population sample of older people. BJU Int. 2018, 122, 300–308. [Google Scholar] [CrossRef]
- Munaganuru, N.; van den Eeden, S.K.; Creasman, J.; Subak, L.L.; Strano- Paul, L.; Huang, A.J. Urine leakage during sexual activity among ethnically diverse, community-dwelling middle-aged and older women. Am. J. Obstet. Gynecol. 2017, 217, 439.e1–439.e8. [Google Scholar] [CrossRef]
- Suzme, R.; Yalcin, A.; Gutdol, F. Connective tissue alterations in woman with pelvic organ prolapse and urinary incontinance. Acta Obstet. Gynecol. Scand. 2007, 86, 882–888. [Google Scholar] [CrossRef]
- Simonelli, C.; Tripodi, F. Psycho-relational aspects of urinary incontinence in female sexuality. Urologia 2008, 75, 14–19. [Google Scholar] [CrossRef]

| Before Surgery n = 50 | After Surgery n = 50 | p-Value | |
|---|---|---|---|
| Desire | 57.14 (0–100) 49.43 (27.11) | 57.14 (0–100) 52.57 (27.30) | 0.3104 |
| Arousal | 67.86 (0–100) 68.86 (24.18) | 85.71 (14.29–100) 73.86 (20.49) | 0.5960 |
| Lubrication | 95.00 (0–100) 85.90 (20.72) | 95.00 (20–100) 83.90 (17.62) | 0.2294 |
| Orgasm | 86.67 (0–100) 79.20 (17.80) | 86.67 (20–100) 83.60 (13.88) | 0.1181 |
| Satisfaction | 75.00 (0–100) 72.50 (22.03) | 75.00 (0–100) 75.67 (18.04) | 0.8808 |
| Pain | 63.64 (0–100) 69.09 (16.22) | 63.64 (45.45–100) 64.18 (7.66) | 0.0041 |
| Question | Response | Before Surgery n (%) | After Surgery n (%) | p-Value |
|---|---|---|---|---|
| How often did you feel sexual desire or interest? | Almost always or always | 1 (2%) | 1 (2%) | 0.3022 |
| Most times (more than half a time) | 11 (22%) | 19 (38%) | ||
| Sometimes (about half the time) | 26 (52%) | 21 (42%) | ||
| A few times (less than half the time) | 2 (4%) | 0 (0%) | ||
| Almost never or never | 10 (20%) | 9 (18%) | ||
| How would you rate your level (degree) of sexual desire or interest? | Very high | 0 (0%) | 0 (0%) | 1 |
| High | 5 (10%) | 4 (8%) | ||
| Moderate | 31 (62%) | 32 (64%) | ||
| Low | 5 (10%) | 5 (10%) | ||
| Very low or none at all | 9 (18%) | 9 (18%) |
| Question | Response | Before Surgery n (%) | After Surgery n (%) | p-Value |
|---|---|---|---|---|
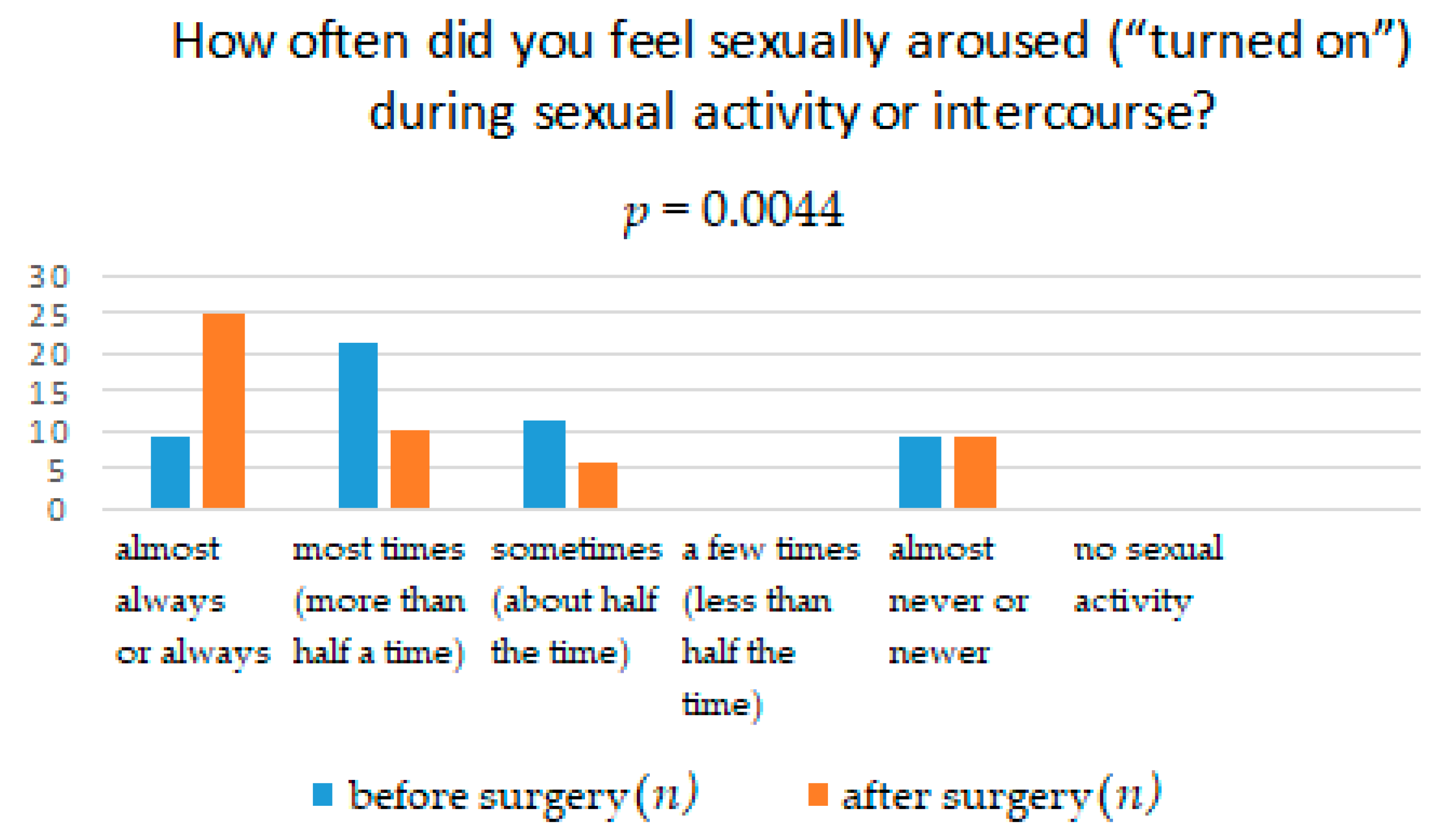
| How often did you feel sexually aroused (“turned on”) during sexual activity or intercourse? | Almost always or always | 9 (18%) | 25 (50%) | 0.0044 |
| Most times (more than half a time) | 21 (42%) | 10 (20%) | ||
| Sometimes (about half the time) | 11 (22%) | 6 (12%) | ||
| A few times (less than half the time) | 0 (0%) | 0 (0%) | ||
| Almost never or never | 9 (18%) | 9 (18%) | ||
| No sexual activity | 0 (0%) | 0 (0%) | ||
| How would you rate your level of sexual arousal (“turn on”) during sexual activity or intercourse? | Very high | 1 (2%) | 2 (4%) | 0.8181 |
| High | 19 (36%) | 22 (44%) | ||
| Moderate | 13 (26%) | 15 (30%) | ||
| Low | 15 (30%) | 10 (20%) | ||
| Very low or none at all | 1 (2%) | 1 (2%) | ||
| No sexual activity | 1 (2%) | 0 (0%) | ||
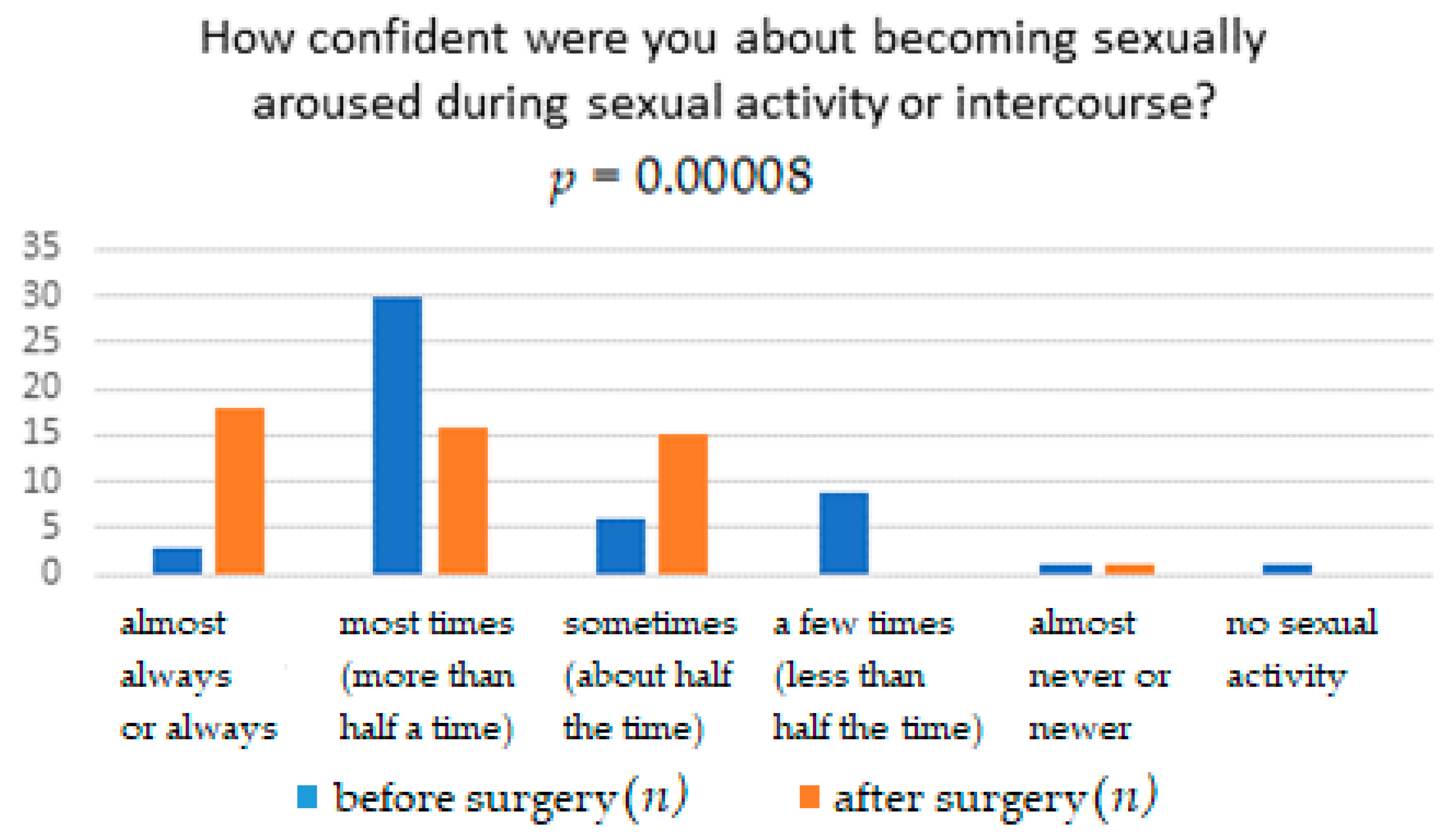
| How confident were you about becoming sexually aroused during sexual activity or intercourse? | Very high confidence | 17 (34%) | 7 (14%) | 0.00008 |
| High confidence | 11(22%) | 30 (60%) | ||
| Moderate confidence | 7 (14%) | 10 (20%) | ||
| Low confidence | 13 (26%) | 2 (4%) | ||
| Very low or no confidence | 1 (2%) | 1 (2%) | ||
| No sexual activity | 1 (2%) | 0 (0%) | ||
| How often have you been satisfied with your arousal (excitement) during sexual activity or intercourse? | Almost always or always | 17 (34%) | 14 (28%) | 0.3561 |
| Most times (more than half a time) | 19 (38%) | 28 (56%) | ||
| Sometimes (about half the time) | 11 (22%) | 7 (14%) | ||
| A few times (less than half the time) | 1 (2%) | 0 (0%) | ||
| Almost never or never | 1 (2%) | 1 (2%) | ||
| No sexual activity | 1(2%) | 0 (0%) |
| Question | Response | Before Surgery n (%) | After Surgery n (%) | p-Value |
|---|---|---|---|---|
| How often did you become lubricated (“wet”) during sexual activity or intercourse? | Almost always or always | 21 (42%) | 27 (52%) | 0.4697 |
| Most times (more than half a time) | 12 (24%) | 14 (28%) | ||
| Sometimes (about half the time) | 14 (28%) | 7 (14%) | ||
| A few times (less than half the time) | 1 (2%) | 1 (2%) | ||
| Almost never or never | 1 (2%) | 1 (2%) | ||
| No sexual activity | 1 (2%) | 0 (0%) | ||
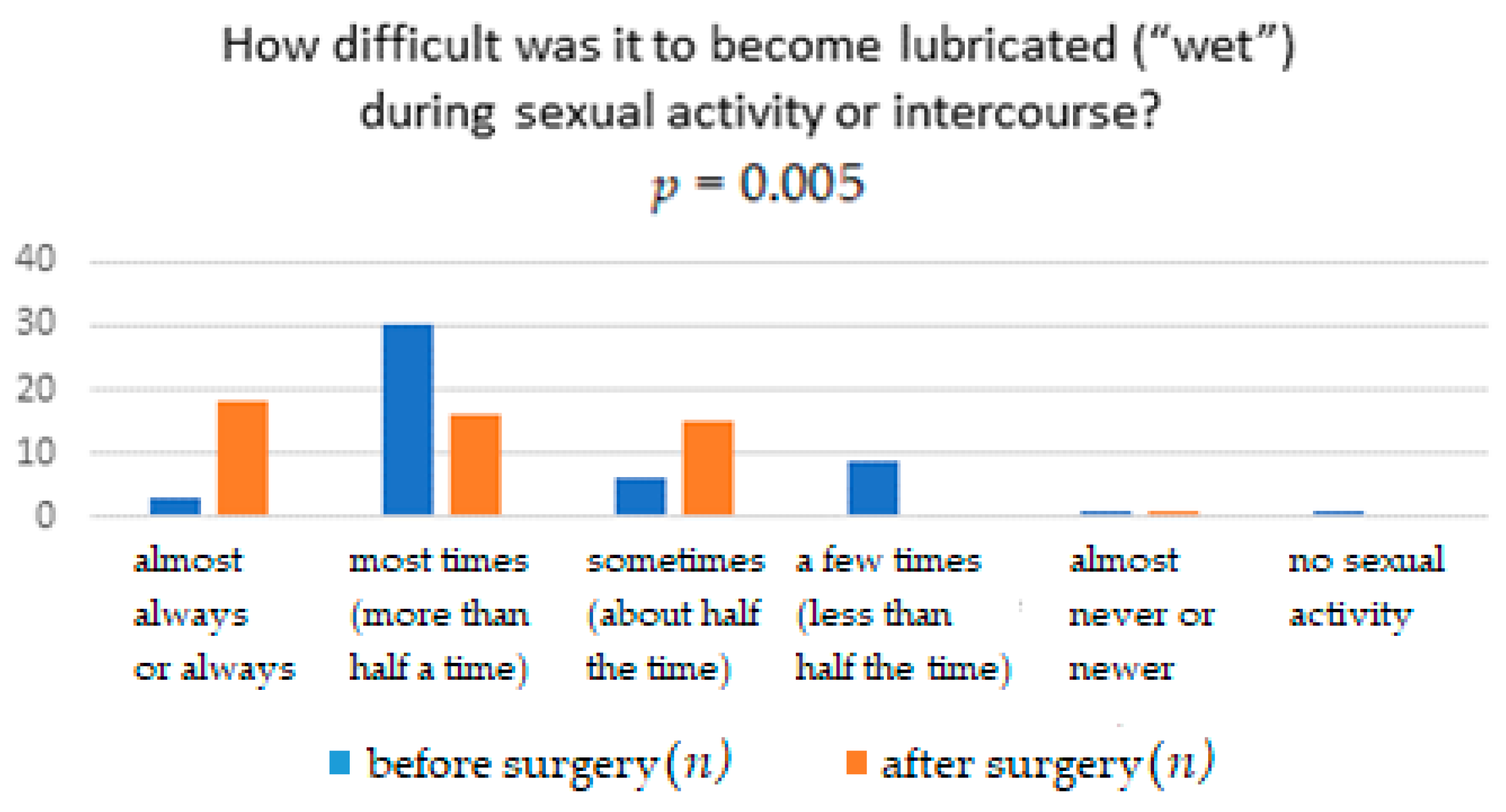
| How difficult was it to become lubricated (“wet”) during sexual activity or intercourse? | Extremely difficult or impossible | 1 (2%) | 1 (2%) | 0.0050 |
| Very difficult | 0 (0%) | 8 (16%) | ||
| Difficult | 4 (8%) | 0 (0%) | ||
| Slightly difficult | 7 (14%) | 7 (14%) | ||
| Not difficult | 37 (72%) | 34 (68%) | ||
| No sexual activity | 1 (2%) | 0 (0%) | ||
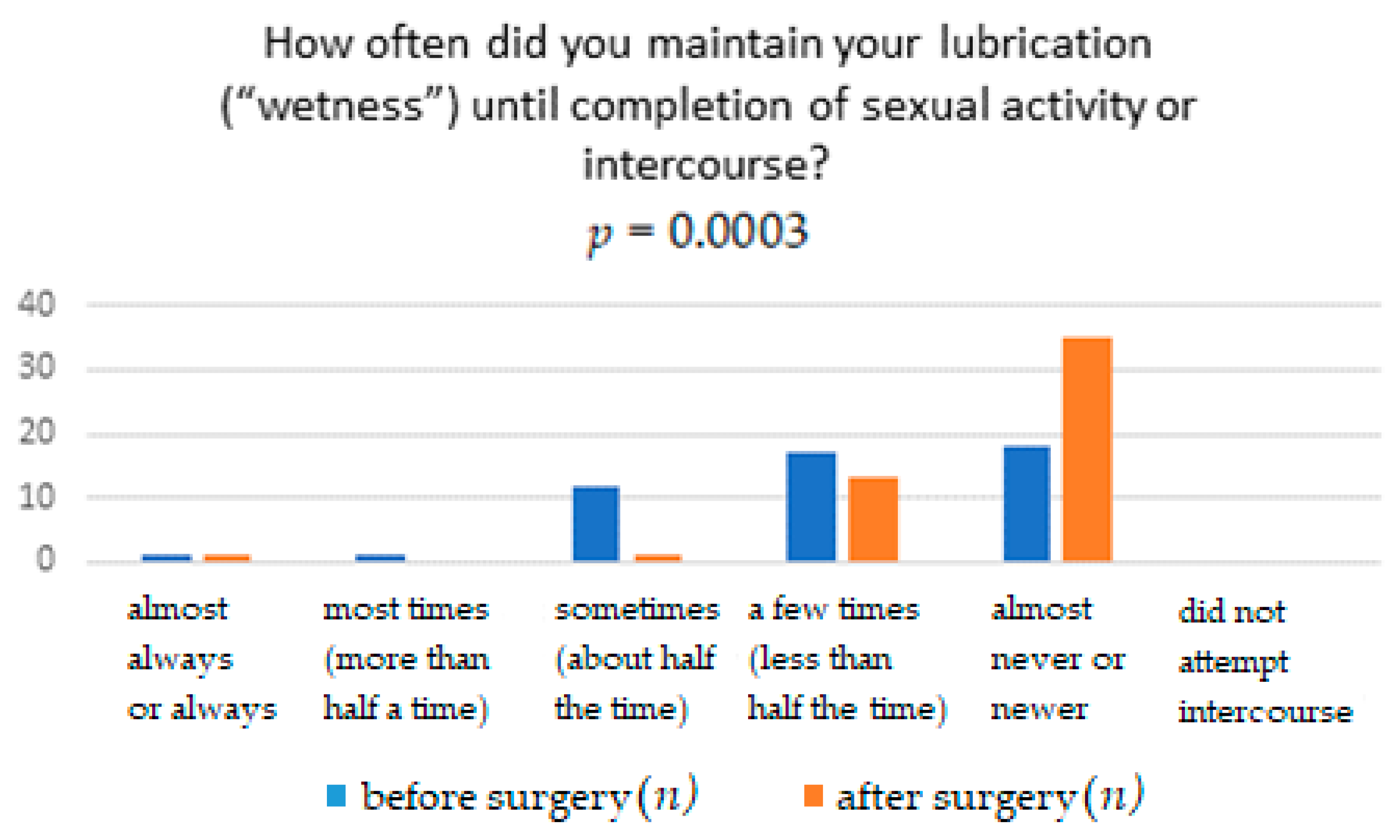
| How often did you maintain your lubrication (“wetness”) until completion of sexual activity or intercourse? | Almost always or always | 32 (64%) | 15 (30%) | 0.0003 |
| Most times (more than half a time) | 7 (14%) | 18 (36%) | ||
| Sometimes (about half the time) | 6 (12%) | 3 (6%) | ||
| A few times (less than half the time) | 2 (4%) | 12 (24%) | ||
| Almost never or never | 2 (4%) | 2 (4%) | ||
| No sexual activity | 1 (2%) | 0 (0%) | ||
| How difficult was it to maintain your lubrication (“wetness”) until completion of sexual activity or intercourse? | Extremely difficult or impossible | 2 (4%) | 4 (8%) | 0.3389 |
| Very difficult | 0 (0%) | 0 (0%) | ||
| Difficult | 3 (6%) | 0 (0%) | ||
| Slightly difficult | 8 (16%) | 7 (14%) | ||
| Not difficult | 36 (72%) | 39 (78%) | ||
| No sexual activity | 1 (2%) | 0 (0%) |
| Question | Response | Before Surgery n (%) | After Surgery n (%) | p-Value |
|---|---|---|---|---|
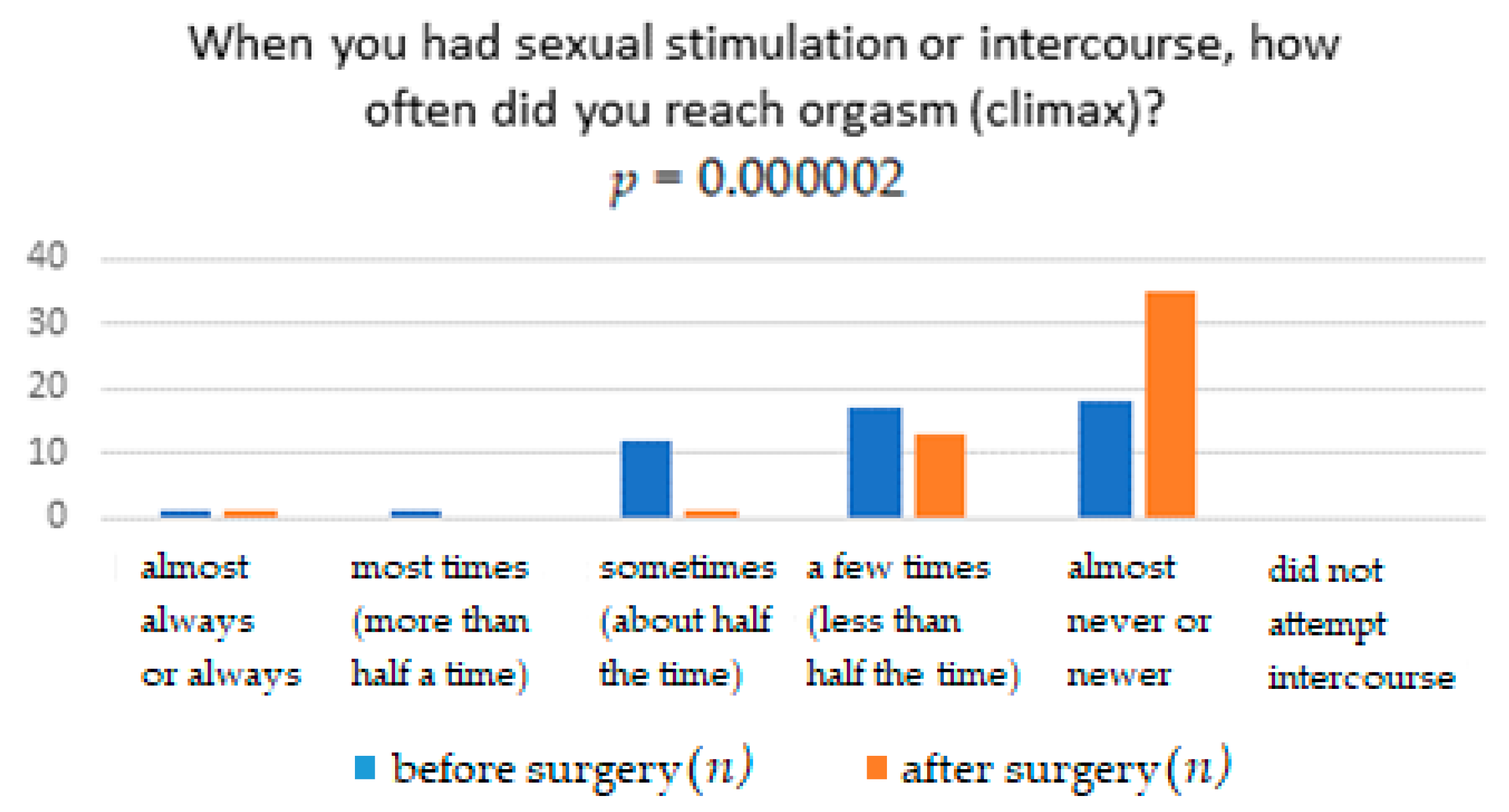
| When you had sexual stimulation or intercourse, how often did you reach orgasm (climax)? | Almost always or always | 3 (6%) | 18 (36%) | 0.000002 |
| Most times (more than half a time) | 30 (60%) | 16 (32%) | ||
| Sometimes (about half the time) | 6 (12%) | 15 (30%) | ||
| A few times (less than half the time) | 9 (18%) | 0 (0%) | ||
| Almost never or never | 1 (2%) | 1 (2%) | ||
| No sexual activity | 1 (2%) | 0 (0%) | ||
| When you had sexual stimulation or intercourse, how difficult was it for you to reach orgasm (climax)? | Extremely difficult or impossible | 1 (2%) | 1 (2%) | 0.9288 |
| Very difficult | 0 (0%) | 0 (0%) | ||
| Difficult | 2 (4%) | 2 (4%) | ||
| Slightly difficult | 10 (20%) | 13 (26%) | ||
| Not difficult | 36 (72%) | 34 (68%) | ||
| No sexual activity | 1 (2%) | 0 (0%) | ||
| How satisfied were you with your ability to reach orgasm (climax) during sexual activity or intercourse? | Very satisfied | 10 (20%) | 6 (12%) | 0.7165 |
| Moderately satisfied | 32 (64%) | 39 (78%) | ||
| About equally satisfied and dissatisfied | 4 (8%) | 3 (6%) | ||
| Moderately dissatisfied | 2 (4%) | 1 (2%) | ||
| Very dissatisfied | 1 (2%) | 1 (2%) | ||
| No sexual activity | 1 (2%) | 0 (0%) |
| Question | Response | Before Surgery n (%) | After Surgery n (%) | p-Value |
|---|---|---|---|---|
| How satisfied have you been with the amount of emotional closeness during sexual activity between you and your partner? | Very satisfied | 11 (22%) | 17 (34%) | 0.2427 |
| Moderately satisfied | 28 (56%) | 19 (38%) | ||
| About equally satisfied and dissatisfied | 9 (18%) | 13 (26%) | ||
| Moderately dissatisfied | 0 (0%) | 0 (0%) | ||
| Very dissatisfied | 1 (2%) | 1 (2%) | ||
| No sexual activity | 1 (2%) | 0 (0%) | ||
| How satisfied have you been with your sexual relationship with your partner? | Very satisfied | 12 (24%) | 17 (34%) | 0.6301 |
| Moderately satisfied | 27 (54%) | 26 (52%) | ||
| About equally satisfied and dissatisfied | 6 (12%) | 5 (10%) | ||
| Moderately dissatisfied | 4 (8%) | 1 (2%) | ||
| Very dissatisfied | 1 (2%) | 1 (2%) | ||
| No sexual activity | 0 (0%) | 0 (0%) | ||
| How satisfied have you been with your overall sexual life? | Very satisfied | 11 (22%) | 5 (10%) | 0.1893 |
| Moderately satisfied | 29 (58%) | 39 (78%) | ||
| About equally satisfied and dissatisfied | 5 (10%) | 4 (8%) | ||
| Moderately dissatisfied | 4 (8%) | 1 (2%) | ||
| Very dissatisfied | 1 (2%) | 1 (2%) | ||
| No sexual activity | 0 (0%) | 0 (0%) |
| Question | Response | Before Surgery n (%) | After Surgery n (%) | p-Value |
|---|---|---|---|---|
| How often did you experience discomfort or pain during vaginal penetration? | Almost always or always | 1 (2%) | 1 (2%) | 0.0005 |
| Most times (more than half a time) | 1 (2%) | 0 (0%) | ||
| Sometimes (about half the time) | 12 (24%) | 1 (2%) | ||
| A few times (less than half the time) | 17 (34%) | 13 (26%) | ||
| Almost never or never | 18 (36%) | 35 (70%) | ||
| Did not attempt intercourse | 0 (0%) | 0 (0%) | ||
| How often did you experience discomfort or pain following vaginal penetration? | Almost always or always | 1 (2%) | 1 (2%) | 0.2234 |
| Most times (more than half a time) | 1 (2%) | 1 (2%) | ||
| Sometimes (about half the time) | 3 (6%) | 9 (18%) | ||
| A few times (less than half the time) | 13 (26%) | 7 (14%) | ||
| Almost never or never | 31 (62%) | 32 (64%) | ||
| Did not attempt intercourse | 1 (2%) | 0 (0%) | ||
| How would you rate your level (degree) of discomfort or pain during or following vaginal penetration? | Very high | 1 (2%) | 1 (2%) | 0.4481 |
| High | 0 (0%) | 0 (0%) | ||
| Moderate | 9 (18%) | 16 (32%) | ||
| Low | 15 (30%) | 12 (24%) | ||
| Very low or none at all | 24 (48%) | 21 (42%) | ||
| Did not attempt intercourse | 1 (2%) | 0 (0%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zalewski, M.; Kołodyńska, G.; Zalewska, A.; Andrzejewski, W. Comparative Assessment of Female Sexual Function Following Transobturator Midurethral Sling for Stress Urinary Incontinence. Int. J. Environ. Res. Public Health 2021, 18, 2286. https://doi.org/10.3390/ijerph18052286
Zalewski M, Kołodyńska G, Zalewska A, Andrzejewski W. Comparative Assessment of Female Sexual Function Following Transobturator Midurethral Sling for Stress Urinary Incontinence. International Journal of Environmental Research and Public Health. 2021; 18(5):2286. https://doi.org/10.3390/ijerph18052286
Chicago/Turabian StyleZalewski, Maciej, Gabriela Kołodyńska, Agata Zalewska, and Waldemar Andrzejewski. 2021. "Comparative Assessment of Female Sexual Function Following Transobturator Midurethral Sling for Stress Urinary Incontinence" International Journal of Environmental Research and Public Health 18, no. 5: 2286. https://doi.org/10.3390/ijerph18052286
APA StyleZalewski, M., Kołodyńska, G., Zalewska, A., & Andrzejewski, W. (2021). Comparative Assessment of Female Sexual Function Following Transobturator Midurethral Sling for Stress Urinary Incontinence. International Journal of Environmental Research and Public Health, 18(5), 2286. https://doi.org/10.3390/ijerph18052286






