Hospitalization Costs of Lower Limb Ulcerations and Amputations in Patients with Diabetes in Romania
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collection
2.3. Statistical Analysis
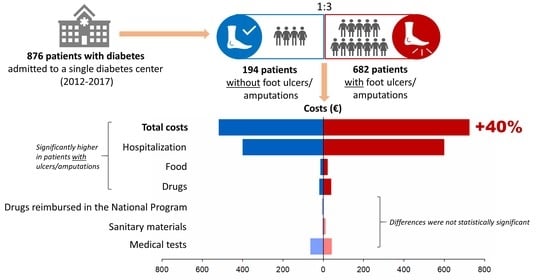
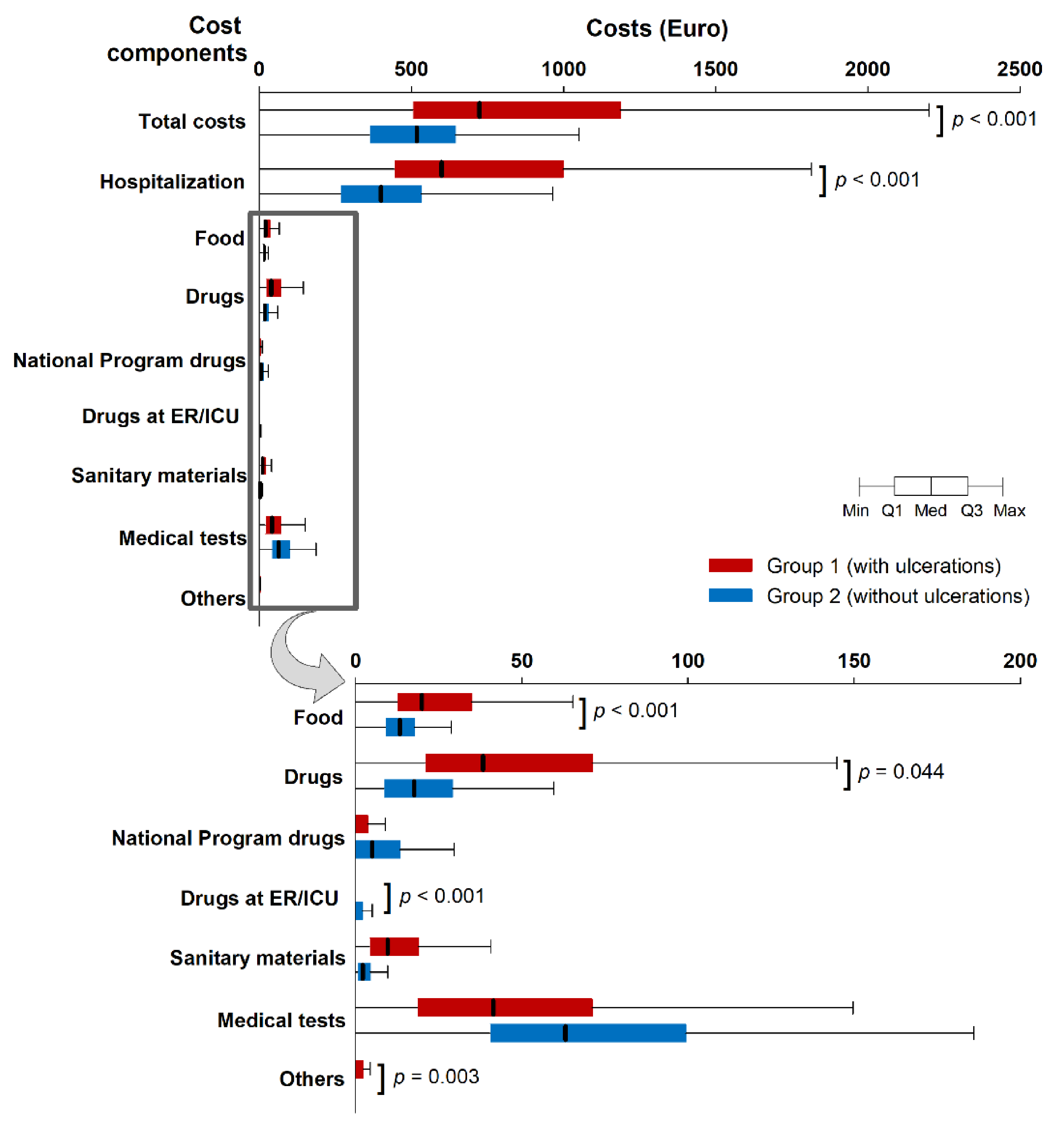
3. Results
3.1. Patient Characteristics
3.2. Cost Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- International Diabetes Foundation. IDF Diabetes Atlas—9th Edition. 2019. Available online: https://diabetesatlas.org/upload/resources/material/20200302_133351_IDFATLAS9e-final-web.pdf (accessed on 3 June 2020).
- Hussain, M.A.; Al-Omran, M.; Salata, K.; Sivaswamy, A.; Forbes, T.L.; Sattar, N.; Aljabri, B.; Kayssi, A.; Verma, S.; de Mestral, C. Population-based secular trends in lower-extremity amputation for diabetes and peripheral artery disease. CMAJ 2019, 191, E955–E961. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. Diabetic foot problems: Prevention and Management. 2015. Available online: https://www.nice.org.uk/guidance/ng19/resources/diabetic-foot-problems-prevention-and-management-pdf-1837279828933 (accessed on 19 February 2021).
- Hicks, C.W.; Selvin, E. Epidemiology of peripheral neuropathy and lower extremity disease in diabetes. Curr. Diab. Rep. 2019, 19, 86. [Google Scholar] [CrossRef]
- Boulton, A.J.M.; Vileikyte, L.; Ragnarson-Tenvall, G.; Apelqvist, J. The global burden of diabetic foot disease. Lancet 2005, 366, 1719–1724. [Google Scholar] [CrossRef]
- Veresiu, I.A.; Iancu, S.S.; Bondor, C.I. Trends in diabetes-related lower extremities amputations in Romania—A five year nationwide evaluation. Diabetes Res. Clin. Pract. 2015, 109, 293–298. [Google Scholar] [CrossRef]
- Liebl, A.; Spannheimer, A.; Reitberger, U.; Görtz, A. Costs of long-term complications in type 2 diabetes patients in Germany. Results of the CODE-2 Study. Med. Klin. 2002, 97, 713–719. [Google Scholar] [CrossRef]
- Kerr, M.; Barron, E.; Chadwick, P.; Evans, T.; Kong, W.M.; Rayman, G.; Sutton-Smith, M.; Todd, G.; Young, B.; Jeffcoate, W.J. The cost of diabetic foot ulcers and amputations to the National Health Service in England. Diabet. Med. 2019, 36, 995–1002. [Google Scholar] [CrossRef] [PubMed]
- Toscano, C.M.; Sugita, T.H.; Rosa, M.Q.M.; Pedrosa, H.C.; Rosa, R.D.S.; Bahia, L.R. Annual direct medical costs of diabetic foot disease in Brazil: A cost of illness study. Int. J. Environ. Res. Public Health 2018, 15, 89. [Google Scholar] [CrossRef] [PubMed]
- Morgovan, C.; Cosma, S.A.; Valeanu, M.; Juncan, A.M.; Rus, L.L.; Gligor, F.G.; Buturca, D.; Tit, M.; Bungau, S.; Ghibu, S. An exploratory research of 18 years on the economic burden of diabetes for the Romanian National Health Insurance System. Int. J. Environ. Res. Public Health 2020, 17, 4456. [Google Scholar] [CrossRef] [PubMed]
- Eurostat. Mean and Median Income by Household Type—EU-SILC and ECHP Survey. Available online: https://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=ilc_di04&lang=en (accessed on 4 November 2020).
- Petrakis, I.; Kyriopoulos, I.J.; Ginis, A.; Athanasakis, K. Losing a foot versus losing a dollar; a systematic review of cost studies in diabetic foot complications. Expert Rev. Pharmacoecon. Outcomes Res. 2017, 17, 165–180. [Google Scholar] [CrossRef]
- Stockl, K.; Vanderplas, A.; Tafesse, E.; Chang, E. Costs of lower-extremity ulcers among patients with diabetes. Diabetes Care 2004, 27, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Driver, V.R.; Fabbi, M.; Lavery, L.A.; Gibbons, G. The costs of diabetic foot: The economic case for the limb salvage team. J. Vasc. Surg. 2010, 52, 17S–22S. [Google Scholar] [CrossRef]
- Shahbazian, H.; Yazdanpanah, L.; Latifi, S.M. Risk assessment of patients with diabetes for foot ulcers according to risk classification consensus of International Working Group on Diabetic Foot (IWGDF). Pak. J. Med. Sci. 2013, 29, 730–734. [Google Scholar] [CrossRef]
- Prompers, L.; Huijberts, M.; Apelqvist, J.; Jude, E.; Piaggesi, A.; Bakker, K.; Edmonds, M.; Holstein, P.; Jirkovska, A.; Mauricio, D.; et al. High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia 2007, 50, 18–25. [Google Scholar] [CrossRef]
- Veresiu, I.A.; Bondor, C.I.; Florea, B.; Vinik, E.J.; Vinik, A.I.; Gavan, N.A. Detection of undisclosed neuropathy and assessment of its impact on quality of life: A survey in 25,000 Romanian patients with diabetes. J. Diabetes Complicat. 2015, 29, 644–649. [Google Scholar] [CrossRef]
- Ibrahim, M.; Tuomilehto, J.; Aschner, P.; Beseler, L.; Cahn, A.; Eckel, R.H.; Fischl, A.H.; Guthrie, G.; Hill, J.O.; Kumwenda, M.; et al. Global status of diabetes prevention and prospects for action: A consensus statement. Diabetes Metab. Res. Rev. 2018, 34, e3021. [Google Scholar] [CrossRef]
- Stirban, A.; Heinemann, L. Skin autofluorescence—A non-invasive measurement for assessing cardiovascular risk and risk of diabetes. Eur. Endocrinol. 2014, 10, 106–110. [Google Scholar] [CrossRef]
- Singh, N.; Armstrong, D.G.; Lipsky, B.A. Preventing foot ulcers in patients with diabetes. JAMA 2005, 293, 217–228. [Google Scholar] [CrossRef]
- Zhang, P.; Lu, J.; Jing, Y.; Tang, S.; Zhu, D.; Bi, Y. Global epidemiology of diabetic foot ulceration: A systematic review and meta-analysis. Ann. Med. 2017, 49, 106–116. [Google Scholar] [CrossRef]
- Moxey, P.W.; Gogalniceanu, P.; Hinchliffe, R.J.; Loftus, I.M.; Jones, K.J.; Thompson, M.M.; Holt, P.J. Lower extremity amputations—a review of global variability in incidence. Diabet. Med. 2011, 28, 1144–1153. [Google Scholar] [CrossRef]
- Mota, M.; Popa, S.G.; Mota, E.; Mitrea, A.; Catrinoiu, D.; Cheta, D.M.; Guja, C.; Hancu, N.; Ionescu-Tirgoviste, C.; Lichiardopol, R.; et al. Prevalence of diabetes mellitus and prediabetes in the adult Romanian population: PREDATORR study. J. Diabetes 2016, 8, 336–344. [Google Scholar] [CrossRef]
- Bondor, C.I.; Veresiu, I.A.; Florea, B.; Vinik, E.J.; Vinik, A.I.; Gavan, N.A. Epidemiology of diabetic foot ulcers and amputations in Romania: Results of a cross-sectional quality of life questionnaire-based survey. J. Diab. Res. 2016, 2016, 5439521. [Google Scholar] [CrossRef]
- Ollendorf, D.A.; Kotsanos, J.G.; Wishner, W.J.; Friedman, M.; Cooper, T.; Bittoni, M.; Oster, G. Potential economic benefits of lower-extremity amputation prevention strategies in diabetes. Diabetes Care 1998, 21, 1240–1245. [Google Scholar] [CrossRef] [PubMed]
- Ortegon, M.M.; Redekop, W.K.; Niessen, L.W. Cost-effectiveness of prevention and treatment of the diabetic foot: A Markov analysis. Diabetes Care 2004, 27, 901–907. [Google Scholar] [CrossRef] [PubMed]
- Horswell, R.L.; Birke, J.A.; Patout, C.A., Jr. A staged management diabetes foot program versus standard care: A 1-year cost and utilization comparison in a state public hospital system. Arch. Phys. Med. Rehabil. 2003, 84, 1743–1746. [Google Scholar] [CrossRef]
- Bakker, K.; Apelqvist, J.; Lipsky, B.A.; Van Netten, J.J.; International Working Group on the Diabetic Foot. The 2015 IWGDF guidance documents on prevention and management of foot problems in diabetes: Development of an evidence-based global consensus. Diabetes Metab. Res. Rev. 2016, 32 (Suppl. 1), 2–6. [Google Scholar] [CrossRef] [PubMed]
- Matricali, G.A.; Dereymaeker, G.; Muls, E.; Flour, M.; Mathieu, C. Economic aspects of diabetic foot care in a multidisciplinary setting: A review. Diabetes Metab. Res. Rev. 2007, 23, 339–347. [Google Scholar] [CrossRef] [PubMed]
| Emergency Clinical County Hospital “Cluj Napoca” | |||
|---|---|---|---|
| Patient Expense Statement | |||
| Name, surname: | |||
| Personal identification number: | |||
| Address: | |||
| Mail diagnosis at discharge: | |||
| Hospitalization department: | File number: | ||
| Period: | From: | To: | |
| Hospitalization days: | |||
| Insurance status: | |||
| 1. Hospitalization costs (number of hospitalization days x cost/day): | |||
| 2. Food costs (food cost/one hospitalization day x number of days): | |||
| 3. Cost of drugs during hospitalization (art.3 from order 1100/2005): | |||
| - Cost of drugs from the national health program: | |||
| 4. Cost of sanitary materials (art.3 from order 1100/2005): | |||
| 5. Cost of medical tests (art.3 from order 1100/2005): | |||
| 6. Other investigations (art.3 from order 1100/2005): | |||
| - Cost of drugs in the Emergency Room: | |||
| - Other medical services: | |||
| TOTAL COSTS: | |||
| Cost of drugs from the national health program: | |||
| Written by: | |||
| Date: | |||
| Medical office: | |||
| Parameter | Group 1 (With Ulcerations) N = 682 | Group 2 (Without Ulcerations) N = 194 | p |
|---|---|---|---|
| Male, n (%) | 532 (78.0) | 102 (52.6) | <0.001 |
| Age, years 1 | 64 (58–70) | 62.5 (50–71) | 0.004 |
| Type 2 diabetes, n (%) | 629 (92.2) | 161 (83.0) | <0.001 |
| Diabetes duration, years 1 | 14 (8–21) | 8 (1–16) | <0.001 |
| BMI, kg/m2 1 | 28.63 (25.4–32.72) | 28.41 (24.39–34.45) | 0.068 |
| Abdominal circumference, cm 1 | 110 (101–122) | 110 (100.5–119) | 0.091 |
| Hypertension, n (%) | 503 (73.8) | 133 (70.0) | 0.303 |
| HbA1c, % | 8.70 (7.50–10.25) | 9.76 (8.00–12.00) | <0.001 |
| Peripheral arteriopathy, n (%) | 250 (36.7) | 24 (12.4) | <0.001 |
| Diabetic neuropathy, n (%) | 682 (100) | 133 (68.6) | <0.001 |
| Retinopathy, n (%) | 322 (47.2) | 46 (23.7) | <0.001 |
| Nephropathy, n (%) | 108 (15.8) | 10 (5.2) | <0.001 |
| End-stage renal disease, n (%) | 207 (30.4) | 41 (21.1) | 0.012 |
| Amputations, n (%) | 323 (47.4) | 0 (0) | <0.001 |
| Hospitalization duration, days 1 | 7 (5–12) | 6 (4–8) | <0.001 |
| Treatment for diabetes | <0.001 | ||
| Diet, n (%) 1 | 9 (1.3) | 2 (1.0) | |
| Insulin, n (%) 1 | 308 (45.2) | 72 (37.3) | |
| GLAO, n (%) 1 | 187 (24.7) | 19 (9.8) | |
| GLAO+GLAI, n (%) 1 | 5 (0.7) | 2 (1.0) | |
| Insulin+GLAO, n (%) 1 | 169 (24.8) | 91 (47.2) | |
| Insulin+GLAI, n (%) 1 | 2 (0.3) | 1 (0.5) | |
| Insulin+GLAO+GLAI, n (%) 1 | 2 (0.3) | 6 (3.1) |
| Parameter | Category | Total Costs/Person, Euro (median [25th–75th percentile]) | p ** | |
|---|---|---|---|---|
| Group 1 (with Ulcerations) N = 682 | Group 2 (without Ulcerations) N = 194 | |||
| Sex | Men | 716.35 (503.79; 1141.15) | 500.85 (319.21; 631.7) | <0.001 |
| Women | 768.04 (507.96; 1307.76) | 520.61 (370.69; 644.52) | <0.001 | |
| p * | 0.627 | 0.142 | - | |
| Diabetes type | Type 1 | 609.64 (495.3; 1086.53) | 457.31 (319.21; 572.98) | 0.001 |
| Type 2 | 739.11 (505.81; 1211.43) | 520.61 (368.84; 652.58) | <0.001 | |
| p * | 0.322 | 0.268 | - | |
| Hypertension | Present | 722.62 (503.79; 1154.82) | 536.53 (372.1; 641.81) | <0.001 |
| Absent | 734.82 (516.84; 1289.88) | 465.82 (327.91; 660.63) | <0.001 | |
| p * | 0.317 | 0.458 | - | |
| Peripheral arteriopathy | Present | 823.89 (546.35; 1376.01) | 524.12 (366.2; 600.05) | <0.001 |
| Absent | 664.79 (497.06; 1067.8) | 517.01 (353.44; 664.32) | <0.001 | |
| p * | 0.003 | 0.590 | - | |
| Diabetic neuropathy | Present | 723.51 (504.02; 1186.36) | 501.52 (367.68; 630.33) | <0.001 |
| Absent | - | 560.53 (326.11; 729.14) | - | |
| p * | - | 0.312 | - | |
| Retinopathy | Present | 668.52 (502.66; 1131.18) | 471.52 (349.49; 579.57) | <0.001 |
| Absent | 769 (505.15; 1241.86) | 536.98 (368.84; 672.07) | <0.001 | |
| p * | 0.293 | 0.095 | - | |
| Nephropathy | Present | 863.4 (555.84; 1615.88) | 643.17 (454.53; 779.94) | 0.031 |
| Absent | 682.39 (502.66; 1131.18) | 512.25 (357.5; 632.49) | <0.001 | |
| p * | 0.231 | 0.172 | - | |
| End-stage renal disease | Present | 683.14 (503.2; 1256.8) | 556.77 (394.14; 695.2) | 0.001 |
| Absent | 735.81 (505.37; 1136.98) | 501.2 (361.57; 633.28) | <0.001 | |
| p * | 0.503 | 0.220 | - | |
| Amputations | Present | 812.05 (529.05; 1323.55) | - | - |
| Absent | 648.59 (485.38; 1076.33) | - | - | |
| p * | 0.308 | - | - | |
| Treatment for diabetes | Diet | 705.4 (630.82; 873.79) | 514.68 (195.7; 833.66) | 0.582 |
| Insulin | 755.11 (515.97; 1320.3) | 539.99 (366.2; 712.13) | <0.001 | |
| GLAO | 681.65 (497.84; 1049.87) | 556.77 (214.48; 642.29) | 0.102 | |
| GLAO+GLAI | 809.17 (775.47; 988.1) | 386.47 (257.98; 514.95) | 0.190 | |
| Insulin+GLAO | 650.78 (498.45; 1100) | 519.07 (394.15; 624.44) | <0.001 | |
| Insulin+GLAI | 731.22 (707.38; 755.06) | - | - | |
| Insulin+GLAO+GLAI | 982.07 (656.38; 1307.76) | 379.09 (348.32; 480.15) | 0.071 | |
| p * | 0.685 | 0.449 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sima, D.I.; Bondor, C.I.; Vereşiu, I.A.; Gâvan, N.A.; Borzan, C.M. Hospitalization Costs of Lower Limb Ulcerations and Amputations in Patients with Diabetes in Romania. Int. J. Environ. Res. Public Health 2021, 18, 2230. https://doi.org/10.3390/ijerph18052230
Sima DI, Bondor CI, Vereşiu IA, Gâvan NA, Borzan CM. Hospitalization Costs of Lower Limb Ulcerations and Amputations in Patients with Diabetes in Romania. International Journal of Environmental Research and Public Health. 2021; 18(5):2230. https://doi.org/10.3390/ijerph18052230
Chicago/Turabian StyleSima, Diana I., Cosmina I. Bondor, Ioan A. Vereşiu, Norina A. Gâvan, and Cristina M. Borzan. 2021. "Hospitalization Costs of Lower Limb Ulcerations and Amputations in Patients with Diabetes in Romania" International Journal of Environmental Research and Public Health 18, no. 5: 2230. https://doi.org/10.3390/ijerph18052230
APA StyleSima, D. I., Bondor, C. I., Vereşiu, I. A., Gâvan, N. A., & Borzan, C. M. (2021). Hospitalization Costs of Lower Limb Ulcerations and Amputations in Patients with Diabetes in Romania. International Journal of Environmental Research and Public Health, 18(5), 2230. https://doi.org/10.3390/ijerph18052230