The Role of Traditional Acupuncture in Patients with Fecal Incontinence—Mini-Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature Search and Inclusion Criteria
2.2. Definition of Fecal Incontinence
3. Results
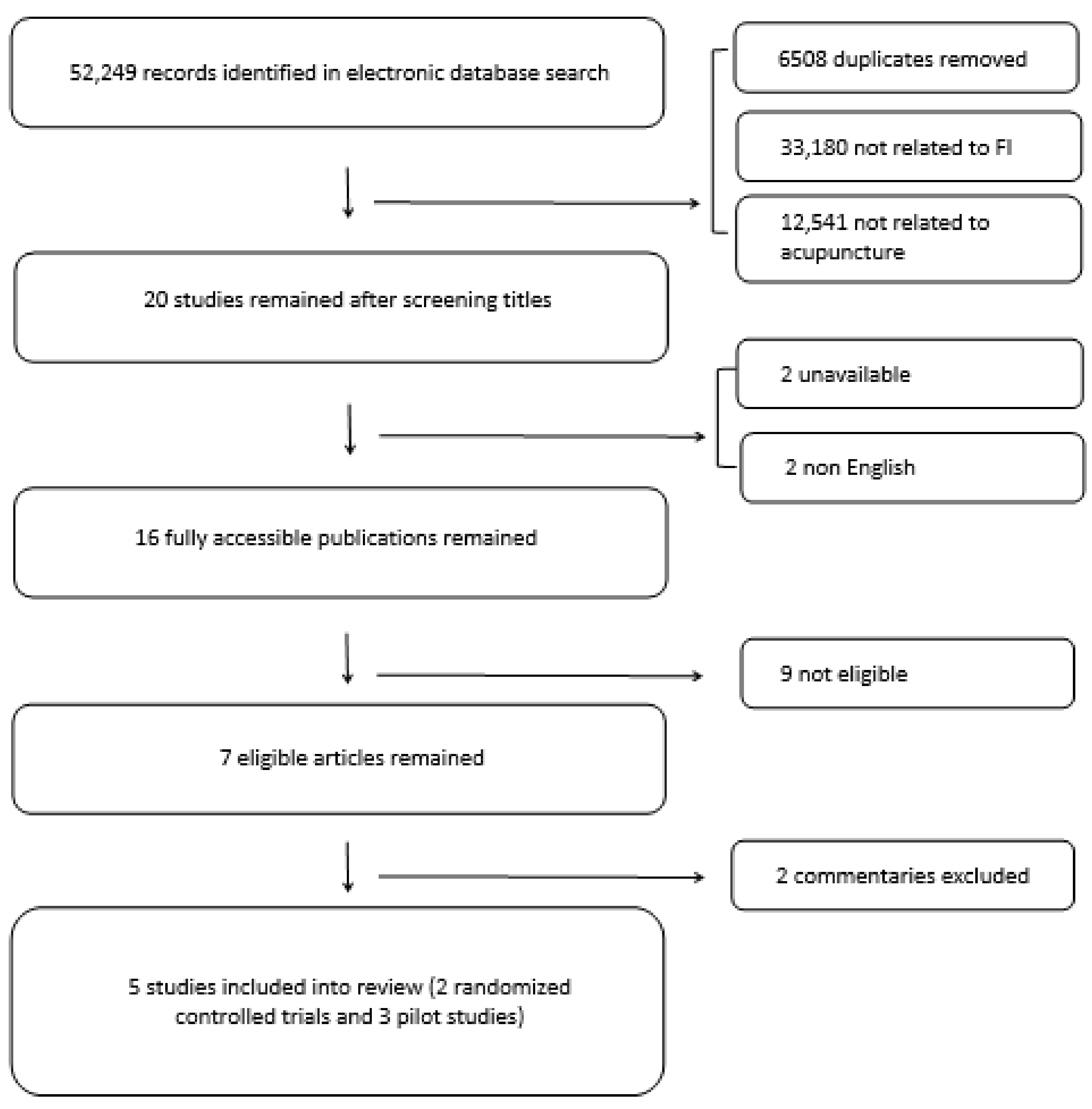
3.1. Search Results
3.2. Effect of Acupuncture Treatment
3.3. Evaluation According to the Criteria
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Benezech, A.; Bouvier, M.; Vitton, V. Faecal incontinence: Current knowledges and perspectives. World J. Gastrointest. Pathophysiol. 2016, 7, 59–71. [Google Scholar] [CrossRef]
- Lamm, S.; Rosenberg, R. Anale Inkontinenz [Fecal incontinence]. Umsch 2019, 73, 559–564. [Google Scholar]
- Whitehead, W.E.; Wald, A.; Norton, N.J. Treatment options for fecal incontinence. Dis. Colon Rectum 2001, 44, 131–144. [Google Scholar] [CrossRef]
- Yang, T.; Liu, Z.; Liu, Y. Electroacupuncture at ciliao and huiyang for treating neuropathic incontinence of defecation and urination in 30 cases. J. Tradit. Chin. Med. 2003, 23, 53–54. [Google Scholar]
- Takahashi, T. Mechanism of acupuncture on neuromodulation in the gut a review. Neuromodulation 2011, 14, 8–12. [Google Scholar] [CrossRef]
- Washabau, R.J.; Fudge, M.; Price, W.J.; Barone, F.C. GABA receptors in the dorsal motor nucleus of the vagus influence feline lower esophageal sphincter and gastric function. Brain Res. Bull. 1995, 38, 587–594. [Google Scholar] [CrossRef]
- Kantzides, A.; Owens, N.C.; De Matteo, R.; Badoer, E. Right atrial stretch activates neurons in autonomic brain regions that project to the rostral ventrolateral medulla in the rat. Neuroscience 2005, 133, 775–786. [Google Scholar] [CrossRef]
- Lin, Y.; Zhou, Z.; Shen, W. Clinical and experimental studies on shallow needling technique for treating childhood diarrhea. J. Tradit. Chin. Med. 1993, 13, 107–114. [Google Scholar] [PubMed]
- Zhou, S.; Zeng, F.; Liu, J.; Zheng, H.; Huang, W.; Liu, T.; Chen, D.; Qin, W.; Gong, Q.; Tian, J.; et al. Influence of acupuncture stimulation on cerebral network in functional diarrhea. Evid. Based Complement Altern. Med. 2013, 2013, 975769. [Google Scholar] [CrossRef]
- Hultén, L.; Angerås, U.; Scaglia, M.; Delbro, D. Sacral nerve stimulation (SNS), posterior tibial nerve stimulation (PTNS) or acupuncture for the treatment for fecal incontinence: A clinical commentary. Tech. Coloproctol. 2013, 17, 589–592. [Google Scholar] [CrossRef] [PubMed]
- Dulskas, A.; Aukstikalnis, T.; Kavaliauskas, P.; Samalavicius, N.E. The role of traditional acupuncture in low anterior resection syndrome treatment a pilot study. Dis. Colon Rectum 2021. accepted for publication. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Whitehead, W.E.; Wald, A.; Diamant, N.E.; Enck, P.; Pemberton, J.H.; Rao, S.S. Functional disorders of the anus and rectum. Gut 1999, 45, II55–II59. [Google Scholar] [CrossRef]
- Treatments for Fecal Incontinence [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US). Available online: https://pubmed.ncbi.nlm.nih.gov/27099893 (accessed on 15 January 2020).
- Rockwood, T.H.; Church, J.M.; Fleshman, J.W.; Kane, R.L.; Mavrantonis, C.; Thorson, A.G.; Wexner, S.D.; Bliss, D.; Lowry, A.C. Patient and surgeon ranking of the severity of symptoms associated with fecal incontinence: The fecal incontinence severity index. Dis. Colon Rectum 1999, 42, 1525–1532. [Google Scholar] [CrossRef] [PubMed]
- Jorge, M.J.N.; Wexner, S.D. Etiology and management of fecal incontinence. Dis. Colon Rectum 1993, 36, 77–97. [Google Scholar] [CrossRef] [PubMed]
- Franco, J.T.; Agulhon, A.M.; Viani, F.C.; Viebig, R.G. Systemic acupuncture in patients with faecal incontinence. Complement Clin. Pr. 2016, 24, 162–166. [Google Scholar] [CrossRef] [PubMed]
- Rockwood, T.H.; Church, J.M.; Fleshman, J.W.; Kane, R.L.; Mavrantonis, C.; Thorson, A.G.; Wexner, S.D.; Bliss, D.N.R.; Lowry, A.C. Fecal Incontinence Quality of Life Scale: Quality of life instrument for patients with fecal incontinence. Dis. Colon Rectum 2000, 43, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.; Azpiroz, F.; Diamant, N.; Enck, P.; Tou-Gas, G.; Wald, A. Minimum standards of anorectal manometry. Neurogastroenterol. Motil. 2002, 14, 553–559. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomized studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J.; GRADE Working Group. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Zhao, Y.; Luo, Y.; Yan, J.; Wu, J.; Liu, M.; Li, N. Zhongguo Zhen Jiu. Chin. Acupunct. Moxibustion 2015, 35, 665–669. [Google Scholar]
- Allam, N.; Mogahed, H. Effect of laser acupuncture on fecal; incontinence after anorectal surgery. Bull. Fac. Phys. Ther. 2018, 23, 60. [Google Scholar]
- Scaglia, M.; Delaini, G.; Destefano, I.; Hultén, L. Fecal incontinence treated with acupuncture—A pilot study. Auton. Neurosci. 2009, 145, 89–92. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Wang, L.; Cooper, E.; Zhang, M.; Manheimer, E.; Berman, B.; Shen, X.; Lao, L. Adverse events of acupuncture: A systematic review of case reports. Evid. Based Complement Altern. Med. 2013, 2013, 581203. [Google Scholar] [CrossRef] [PubMed]
| No. | Author and Year | Type | Patients Included | Follow-up | Inclusion Criteria | Exclusion Criteria | Treatment Technique | Acupoints | Diagnostic Tools for Incontinence Assessment | Results |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Allam N. et al. 2018 | Randomized controlled trial | N = 40 M = 17 F = 23 | - | Patients with moderate FI after anorectal surgery. | Patients with severe FI, damage to the rectovaginal fascia, spinal cord injury, neurological disorders, pregnancy, inflammatory bowel disease, idiopathic FI, history of FI before surgery, intake of photosensitive drugs, injury or active infection in the area of treatment, and unstable medical conditions. | Experimental group: laser acupuncture + pelvic floor exercises LA (infrared laser, 905nm, 15 W, 225 mJ, 60 s/point)—3 sessions per week for 4 weeks (1 month after the surgery). Control group: sham laser acupuncture + pelvic floor exercises | RN3, RN6, BL23, BL32, BL35, ST36, KI3 | Anorectal manometry | 18.55% increase in resting anal pressure and 11.87% increase in squeeze anal pressure after treatment in the experimental group (p > 0.001). 10.49% increase in resting anal pressure and 6.62% increase in squeeze anal pressure after treatment in the control group (p > 0.001). Significant increase in the experimental group compared to the control group after the treatment (p > 0.001). |
| FISI | 26.44% decrease in FISI in the experimental group after the treatment (p > 0.001). 13.90% decrease in FISI in the control group after the treatment (p > 0.001). Significant decrease in FISI in the experimental group compared to the control group after the treatment (p > 0.001). | |||||||||
| 2. | Franco J. et al. 2016 | Pilot study | N = 18 M = 2 F = 16 | - | Adult patients diagnosed with FI for more than 6 months and lack of continence function shown by anorectal manometry. | Patients younger than 21 years of age; prior muscle injury caused by surgical episiotomy or accident, neurological disorders, metabolic diseases, cognitive deficits, or other factors that could influence the incontinence, such as chronic diarrhea. | Traditional acupuncture, 10 weekly sessions. First session—seeds attached for 3 days on preselected points. Follow up sessions—needles applied to the dorsal area and held for 20 min, then to the ventral area for 15 min. | LI11, PC6, ST37, SP9, BL54, KI7, CV9 CV6, CV3, LV13, BL23, BL25, BL32, LU9, TH5, SP6, BL67, SP2, GB41 | VAS | Statistically significant improvement (p < 0.0001). |
| FIQL | Statistically significant improvement in each domain (p < 0.05). | |||||||||
| Adverse effects not reported. | ||||||||||
| 3. | Scaglia M. et al. 2009 | Pilot study | N = 15 M = 0 F = 15 | 18 months | Patients diagnosed with FI for longer than a year. | Manual acupuncture Once a week for 10 weeks, and once a month for 7 months for 6 patients. | 3RM, 6RM, 4DM, 23BL, 32BL, 4LI, 36ST, 3K | Anorectal manometry | Resting anal pressure increased from 25 mmHg to 36 mmHG (p = 0.05); maximal sphincter squeeze pressure, rectal volume, and sensory function remained unchanged; the ability to sustain the squeeze pressure improved from 41 mmHg to 60 mmHg (p < 0.05) and returned to the pre-treatment values after the follow-up period. | |
| Cleveland clinic continence score/Wexner score | Significant improvement (p < 0.05) after treatment and at the final assessment in overall and mean scores. | |||||||||
| 4. | Yang T. et al. 2003 | Pilot study | N = 30 M = 16 F = 14 | - | Patients with at least one-time urinary incontinence plus FI episode per day caused by cerebral or spinal injury. | NA | Electroacupuncture (EA) 5 daily sessions with 2 free days between 2 courses + 2 more courses for uncured patients. | BL32, BL35 | Effectiveness: Decrease of incontinence by over 50%. Failure: Decrease of incontinence by less than 50% or without improvement. | 76.7% of FI patients were cured; for 6.7% of participants, the treatment was effective, while for 16.6% of patients, the treatment failed. No significant difference was found when comparing patients with a spinal injury and patients with cerebrovascular diseases, with a cured rate for FI being 66.7% and 80%, respectively. |
| 5. | Zhao Y. et al. 2015 | Randomized controlled trial | N = 40 | NA | Patients with copracrasia. | Acupuncture-moxibustion group Acupuncture-moxibustion 3 times a week for 8 weeks, then 2 times a week for 4 weeks. Medication group. Symptomatic treatment, support therapy, prevention, and treatment of complications. | BL32, GV1, ST25, CV6 | Vaizey incontinence score | Vaizey incontinence’ scores both statistically significantly decreased (both p P < 0.05) in acupuncture group after treatment and in the follow-up period compared to medication group. | |
| Effective rate | The effective rate of the acupuncture-moxibustion group was 80.0% (16/20), which was statistically different from 50.0% (10/20) in the medication group (p < 0.05). The effective rate in the follow-up period of the acupuncture-moxibustion group was 90.0% (18/20), which was not statistically different from 80.0% (16/20) in the medication group (p > 0. 05). | |||||||||
| Self-rating score for satisfaction | The self-rating scores for satisfaction in the acupuncture-moxibustion group were superior. |
| Domain | Allam N. et al. | Franco J. et al. | Scaglia M. et al. | Yang T. et al. | Zhao Y. et al. |
|---|---|---|---|---|---|
| Bias due to confounding | Serious | Serious | Moderate | Serious | Serious |
| Bias in selection of participants into the study | Low | Moderate | Moderate | Moderate | Low |
| Bias in classification of interventions | Low | Low | Low | Low | Low |
| Bias due to deviations from intended interventions | Low | Moderate | Moderate | Low | Moderate |
| Bias due to missing data | Low | Low | Low | Low | Low |
| Bias in measurement of outcomes | Low | Serious | Low | Serious | Serious |
| Bias in selection of the reported result | Low | Low | Low | Low | No information |
| Overall Risk | Serious | Serious | Moderate | Serious | Serious |
| Quality Assessment | Summary of Findings | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No of Patients | Effect | Quality | ||||||||
| No. of Studies | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Acupuncture | No Intervention | |||
| Incontinence | ||||||||||
| 5 | RCT and Pilot | Serious | Not serious | Not serious | Not serious | 103 | 40 | Statistically significant improvement | Moderate | Important |
| Quality of life | ||||||||||
| 2 | RCT and Pilot | Serious | Not serious | Not serious | Not serious | 38 | 20 | Statistically significant improvement | Moderate | Important |
| Anorectal manometry | ||||||||||
| 2 | RCT and Pilot | Moderate | Not serious | Not serious | Not serious | 38 | 20 | Statistically significant improvement | Moderate | Important |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sipaviciute, A.; Aukstikalnis, T.; Samalavicius, N.E.; Dulskas, A. The Role of Traditional Acupuncture in Patients with Fecal Incontinence—Mini-Review. Int. J. Environ. Res. Public Health 2021, 18, 2112. https://doi.org/10.3390/ijerph18042112
Sipaviciute A, Aukstikalnis T, Samalavicius NE, Dulskas A. The Role of Traditional Acupuncture in Patients with Fecal Incontinence—Mini-Review. International Journal of Environmental Research and Public Health. 2021; 18(4):2112. https://doi.org/10.3390/ijerph18042112
Chicago/Turabian StyleSipaviciute, Agne, Tomas Aukstikalnis, Narimantas E. Samalavicius, and Audrius Dulskas. 2021. "The Role of Traditional Acupuncture in Patients with Fecal Incontinence—Mini-Review" International Journal of Environmental Research and Public Health 18, no. 4: 2112. https://doi.org/10.3390/ijerph18042112
APA StyleSipaviciute, A., Aukstikalnis, T., Samalavicius, N. E., & Dulskas, A. (2021). The Role of Traditional Acupuncture in Patients with Fecal Incontinence—Mini-Review. International Journal of Environmental Research and Public Health, 18(4), 2112. https://doi.org/10.3390/ijerph18042112







