The Professional and Psycho-Emotional Impact of the COVID-19 Pandemic on Medical Care—A Romanian GPs’ Perspective
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.3. Research Ethics
2.4. Statistical Analysis
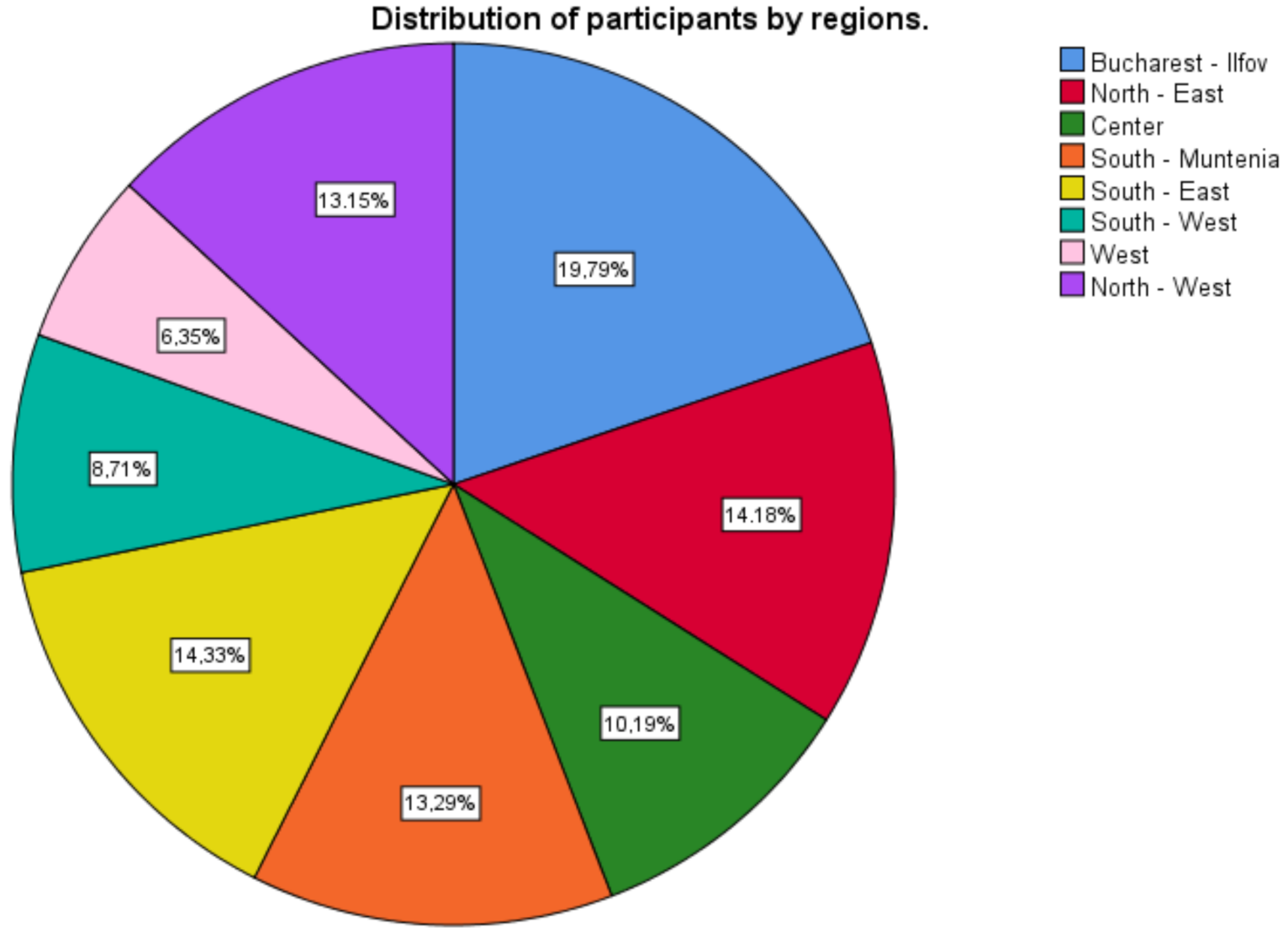
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baddock, K. COVID-19-the frontline (a GP perspective). N. Z. Med. J. 2020, 133, 8–10. [Google Scholar] [PubMed]
- Excerpt from ECDC Rapid Risk Assessment Pandemic with the New Coronavirus (COVID-19): Increased Transmission in EU/EEA and UK, 6th Update, 12 March 2020. National Institute of Public Health, Ministry of Health, Romania. Available online: http://www.cnscbt.ro/index.php/evaluare-de-risc/1511-pandemia-cu-covid-19-a-sasea-evaluare-rapida-de-risc-a-ecdc-rra-12-martie-2020/file (accessed on 25 June 2020).
- Baird, B.; Charles, A.; Honeyman, M.; Maguire, D.; Das, P. Understanding Pressures in General Practice, 1st ed.; The King’s Fund: London, UK, 2016; 100p. [Google Scholar]
- Gonzalez-Padilla, D.A.; Tortolero-Blanco, L. Social Media Influence in the COVID-19 Pandemic. Available online: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1677-55382020000700120&lng=en&nrm=iso (accessed on 10 February 2021).
- Sahni, H.; Sharma, H. Role of social media during the COVID-19 pandemic: Beneficial, destructive, or reconstructive? Int. J. Acad. Med. 2020, 6, 70–75. [Google Scholar]
- Cervino, G.; Oteri, G. COVID-19 Pandemic and Telephone Triage before Attending Medical Office: Problem or Opportunity? Medicina 2020, 56, 250. [Google Scholar] [CrossRef]
- Giorgi, G.; Lecca, L.I.; Alessio, F.; Finstad, G.L.; Bondanini, G.; Lulli, L.G.; Arcangeli, G.; Mucci, N. COVID-19-related mental health effects in the workplace: A narrative review. Int. J. Environ. Res. Public Health 2020, 17, 7857. [Google Scholar] [CrossRef]
- Brooks, S.K.; Dunn, R.; Amlôt, R.; Rubin, G.J.; Greenberg, N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J. Occup. Environ. Med. 2018, 60, 248–257. [Google Scholar] [CrossRef] [PubMed]
- Kang, L.; Ma, S.; Chen, M.; Yang, J.; Wang, Y.; Li, R.; Yao, L.; Bai, H.; Cai, Z.; Yang, B.X.; et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav. Immun. 2020, 87, 11–17. [Google Scholar] [CrossRef]
- Chatzittofis, A.; Karanikola, M.; Michailidou, K.; Constantinidou, A. Impact of the COVID-19 Pandemic on the Mental Health of Healthcare Workers. Int. J. Environ. Res. Public Health 2021, 18, 1435. [Google Scholar] [CrossRef]
- ECRIN—European Clinical Research Infrastructure Network. COVID-19 Trials Registries. Available online: https://ecrin.org/covid-19-trials-registries (accessed on 29 January 2021).
- Shreffler, J.; Petrey, J.; Huecker, M. The impact of COVID-19 on healthcare worker wellness: A scoping review. West. J. Emerg. Med. 2020, 21, 1059–1066. [Google Scholar] [CrossRef] [PubMed]
- Blake, H.; Bermingham, F.; Johnson, G.; Tabner, A. Mitigating the Psychological Impact of COVID-19 on Healthcare Workers: A Digital Learning Package. Int. J. Environ. Res. Public Health 2020, 17, 2997. [Google Scholar] [CrossRef]
- Hameleers, M.; van der Meer, T.G.L.A.; Brosius, A. Feeling “disinformed” lowers compliance with COVID-19 guidelines: Evidence from the US, UK, Netherlands and Germany. Harvard Kennedy Sch. (HKS). Misinformation Rev. 2020. Available online: https://misinforeview.hks.harvard.edu/wp-content/uploads/2020/05/May-27_Michael_misconceptions_compliance_DEF.pdf (accessed on 29 January 2021).
- European Center for Disease Prevention and Control. Interpretation of COVID-19 Data Presented on This Website. Available online: https://www.ecdc.europa.eu/en/interpretation-covid-19-data (accessed on 29 January 2021).
- European Center for Disease Prevention and Control. Data on Testing for COVID-19 by Week and Country. Available online: https://www.ecdc.europa.eu/en/publications-data/covid-19-testing (accessed on 29 January 2021).
- COVID-19 Pandemic in Ukraine. Available online: https://covid19.gov.ua/en (accessed on 31 January 2021).
- Gonzalez-Bernal, J.J.; Rodríguez-Fernández, P.; Santamaría-Peláez, M.; González-Santos, J.; León-del-Barco, B.; Minguez, L.A.; Soto-Cámara, R. Life Satisfaction during Forced Social Distancing and Home Confinement Derived from the COVID-19 Pandemic in Spain. Int. J. Environ. Res. Public Health 2021, 18, 1474. [Google Scholar] [CrossRef] [PubMed]
- The British Medical Association. COVID-19. Available online: https://www.bma.org.uk/advice-and-support/covid-19#your-health-and-wellbeing (accessed on 25 June 2020).
- Kowalczuk, I.; Gębski, J. Impact of Fear of Contracting COVID-19 and Complying with the Rules of Isolation on Nutritional Behaviors of Polish Adults. Int. J. Environ. Res. Public Health 2021, 18, 1631. [Google Scholar] [CrossRef]
- Solar, O.; Irwin, A. A Conceptual Framework for Action on the Social Determinants of Health; Social Determinants of Health Discussion Paper 2 (Policy and Practice); World Health Organization: Geneva, Switzerland, 2010; 76p, Available online: https://apps.who.int/iris/handle/10665/44489 (accessed on 8 February 2021).
- McDowell, I. The Theoretical and Technical Foundations of Health Measurement. In Measuring Health: A Guide to Rating Scales and Questionnaires, 3rd ed.; Oxford University Press: London, UK, 2006; Chapter 2; pp. 10–46. [Google Scholar]
- Havarneanu, C. Psychological Knowledge of the Person: Possibilities of Using the Computer in Applied Psychology, 1st ed.; Polirom Publishing House: Iasi, Romania, 2000; pp. 128–140. [Google Scholar]
- Shadmi, E.; Wong, W.C.W.; Kinder, K.; Heath, I.; Kidd, M. Primary care priorities in addressing health equity: Summary of the WONCA 2013 Health Equity Workshop. Int. J. Equity Health 2014, 13, 104. [Google Scholar] [CrossRef] [PubMed]
- Hasell, J.; Mathieu, E.; Beltekian, D.; Macdonald, B.; Giattino, C.; Ortiz-Ospina, E.; Roser, M.; Ritchie, H. A cross-country database of COVID-19 testing. Sci. Data 2020, 7, 345. [Google Scholar] [CrossRef]
- NUTS II Regions in Romania, 2010 and 2013. Available online: https://ec.europa.eu/eurostat/documents/345175/7451602/nuts-map-RO.pdf (accessed on 29 January 2021).
- National Institute of Statistics. SAN104 Annexes. Available online: http://statistici.insse.ro:8077/tempo-online/#/pages/tables/insse-table (accessed on 25 June 2020).
- The Survey System. Sample Size Calculator. Available online: https://www.surveysystem.com/sscalc.htm (accessed on 25 June 2020).
- Bagcchi, S. Stigma during the COVID-19 pandemic. Lancet Infect. Dis. 2020, 20, 782. [Google Scholar] [CrossRef]
- Kidd, M. (Ed.) The Contribution of Family Medicine to Improving Health Systems: A Guidebook from the World Organization of Family Doctors, 2nd ed.; CRC Press: London, UK, 2013. [Google Scholar]
- Sutter, A.; Llor, C.; Maier, M.; Mallen, C.; Tatsioni, A.; van Weert, H.; Windak, A.; Stoffers, J. Family medicine in times of ‘COVID-19’: A generalists’ voice. Eur. J. Gen. Pract. 2020, 26, 58–60. [Google Scholar] [CrossRef]
- David, D. The Psychology of the Romanian People: The Psychological Profile of the Romanians in a Cognitive-Experimental Monograph; Polirom Publishing House: Iasi, Romania, 2015; 391p. [Google Scholar]
- Lotzin, A.; Acquarini, E.; Ajdukovic, D.; Ardino, V.; Böttche, M.; Bondjers, K.; Bragesjö, M.; Dragan, M.; Grajewski, P.; Figueiredo-Braga, M.; et al. Stressors, coping and symptoms of adjustment disorder in the course of the COVID-19 pandemic—Study protocol of the European Society for Traumatic Stress Studies (ESTSS) pan-European study. Eur. J. Psychotraumatol. 2020, 11, 1780832. [Google Scholar] [CrossRef]
- Chetty, U.J.; O’Donnell, P.; Blane, D.; Willems, S. The role of primary care in improving health equity: Report of a workshop held by the WONCA Health Equity Special Interest Group at the 2015 WONCA Europe Conference in Istanbul, Turkey. Int. J. Equity Health 2016, 15, 128. [Google Scholar] [CrossRef]
- Irwin, R.; Stokes, T.; Marshall, T. Practice-level quality improvement interventions in primary care: A review of systematic reviews. Prim. Health Care Res. Dev. 2015, 16, 556–577. [Google Scholar] [CrossRef]
- Assessment of COVID-19 Surveillance Case Definitions and Data Reporting in the European Union. Available online: https://www.europarl.europa.eu/RegData/etudes/BRIE/2020/652725/IPOL_BRI(2020)652725_EN.pdf (accessed on 31 January 2021).
- David, D.; Comsa, R. Romania’s Modernity Index (IMR)—Is Romania Psychoculturally Modernized? Available online: http://ropsy.granturi.ubbcluj.ro/wp-content/uploads/2020/11/Raport-Profil-Psihocultural-Romania-ROPsy-2020-Site.pdf (accessed on 31 January 2021).
- Research Report: The Psychological and Psychocultural Profile of Romania’s Regions. Available online: http://ropsy.granturi.ubbcluj.ro/2020/11/12/research-report-the-psychological-profile-of-romanias-regions/ (accessed on 31 January 2021).
- El-Hage, W.; Hingray, C.; Lemogne, C.; Yrondi, A.; Brunault, P.; Bienvenu, T.; Etain, B.; Paquet, C.; Gohier, B.; Bennabi, D.; et al. Les professionnels de santé face à la pandémie de la maladie à coronavirus (COVID-19): Quels risques pour leur santé mentale? [Health professionals facing the coronavirus disease 2019 (COVID-19) pandemic: What are the mental health risks?]. Encephale 2020, 46, S73–S80. [Google Scholar] [CrossRef] [PubMed]
- Verhoeven, V.; Tsakitzidis, G.; Philips, H.; Van Royen, P. Impact of the COVID-19 pandemic on the core functions of primary care: Will the cure be worse than the disease? A qualitative interview study in Flemish GPs. BMJ Open 2020, 10, e039674. [Google Scholar] [CrossRef]
- BMA COVID-19 Survey December 2020. Available online: https://www.bma.org.uk/media/3637/bma-covid-survey-results-all-doctors-dec-2020.pdf (accessed on 29 January 2021).
- Conti, C.; Fontanesi, L.; Lanzara, R.; Rosa, I.; Porcelli, P. Fragile heroes. The psychological impact of the COVID-19 pandemic on health-care workers in Italy. PLoS ONE 2020, 15, e0242538. [Google Scholar] [CrossRef] [PubMed]
- Preti, E.; Di Mattei, V.; Perego, G.; Ferrari, F.; Mazzetti, M.; Taranto, P.; Di Pierro, R.; Madeddu, F.; Calati, R. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: Rapid review of the evidence. Curr. Psychiatry Rep. 2020, 22, 43. [Google Scholar] [CrossRef]
- Marina, C.; Geoca-Mutu, D.; Raduca, L.; Avino, A.; Brinduse, L.; Stefan, C.; Scaunasu, R.; Jecan, C. COVID-19 outbreak impact on plastic surgery residents from Romania. J. Mind Med. Sci. 2020, 7, 14. [Google Scholar] [CrossRef]
- COVID Data Tracker. Available online: https://covid.cdc.gov/covid-data-tracker/#datatracker-home (accessed on 2 February 2021).
- Dong, E.; Du, H.; Gardner, L. An Interactive Web-Based Dashboard to Track COVID-19 in Real Time. Lancet Infect. Dis. 2020, 20, 533–534. [Google Scholar] [CrossRef]
- Cabarkapa, S.; Nadjidai, S.E.; Murgier, J.; Ng, C.H. The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: A rapid systematic review. Brain Behav. Immun. Health 2020, 8, 100144. [Google Scholar] [CrossRef]
| Description of Socio- Demographic Characteristics | Gender | Type of Practice | Seniority in the Profession | Age | Region |
|---|---|---|---|---|---|
| Valid | 677 | 677 | 677 | 677 | 677 |
| Missing | 0 | 0 | 0 | 0 | 0 |
| Mean | 1.8715 | 1.5569 | 21.9143 | 51.5790 | 4.05 |
| Std. Deviation | 0.33490 | 0.49712 | 10.83599 | 8.87662 | 2.371 |
| Stage of Disease | Frequency | Percent (%) | Valid % | Cumulative % |
|---|---|---|---|---|
| HBP | 154 | 22.7 | 22.7 | 22.7 |
| COPD | 5 | 0.7 | 0.7 | 23.5 |
| Asthma | 13 | 1.9 | 1.9 | 25.4 |
| Obesity | 112 | 16.5 | 16.5 | 41.9 |
| Diabetes | 36 | 5.3 | 5.3 | 47.3 |
| Chronic hepatitis | 5 | 0.7 | 0.7 | 48.0 |
| Kidney disease | 5 | 0.7 | 0.7 | 48.7 |
| Depression | 9 | 1.3 | 1.3 | 50.1 |
| Anxiety syndrome | 18 | 2.7 | 2.7 | 52.7 |
| Panic attacks | 5 | 0.7 | 0.7 | 53.5 |
| Surgical intervention 1 | 5 | 0.7 | 0.7 | 54.2 |
| Cancer | 10 | 1.5 | 1.5 | 55.7 |
| Without chronic diseases | 115 | 17.0 | 17.0 | 72.7 |
| Other chronic diseases | 185 | 27.3 | 27.3 | 100.0 |
| Total | 677 | 100.0 | 100.0 |
| Correlations | Adjustment to Pandemic | Presence of Stress Symptoms | Burden of Prevention | |
|---|---|---|---|---|
| Adjustment to pandemic | Pearson correlation | 1 | 0.242 ** | 0.242 ** |
| Sig. (2-tailed) | 0.000 | 0.000 | ||
| n | 677 | 677 | 677 | |
| Presence of stress symptoms | Pearson correlation | 0.242 ** | 1 | 1.000 ** |
| Sig. (2-tailed) | 0.000 | 0.000 | ||
| n | 677 | 677 | 677 | |
| Burden of prevention | Pearson correlation | 0.242 ** | 1.000 ** | 1 |
| Sig. (2-tailed) | 0.000 | 0.000 | ||
| n | 677 | 677 | 677 | |
| Model | Sum of Squares | df | Mean Square | F | Sig. |
|---|---|---|---|---|---|
| Regression | 1370.866 | 6 | 228.478 | 5.824 | 0.000 b |
| Residual | 25930.344 | 661 | 39.229 | ||
| Total | 27301.210 | 667 |
| Model | Sum of Squares | df | Mean Square | F | Sig. |
|---|---|---|---|---|---|
| Regression | 1416.461 | 6 | 236.077 | 6.029 | 0.000 b |
| Residual | 25,884.749 | 661 | 39.160 | ||
| Total | 27,301.210 | 667 |
| Model | Sum of Squares | df | Mean Square | F | Sig. |
|---|---|---|---|---|---|
| Regression | 327.857 | 6 | 54.643 | 2.322 | 0.032 b |
| Residual | 15,558.017 | 661 | 23.537 | ||
| Total | 15,885.874 | 667 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stafie, C.S.; Profire, L.; Apostol, M.M.; Costache, I.I. The Professional and Psycho-Emotional Impact of the COVID-19 Pandemic on Medical Care—A Romanian GPs’ Perspective. Int. J. Environ. Res. Public Health 2021, 18, 2031. https://doi.org/10.3390/ijerph18042031
Stafie CS, Profire L, Apostol MM, Costache II. The Professional and Psycho-Emotional Impact of the COVID-19 Pandemic on Medical Care—A Romanian GPs’ Perspective. International Journal of Environmental Research and Public Health. 2021; 18(4):2031. https://doi.org/10.3390/ijerph18042031
Chicago/Turabian StyleStafie, Celina Silvia, Lenuta Profire, Maria Manuela Apostol, and Irina Iuliana Costache. 2021. "The Professional and Psycho-Emotional Impact of the COVID-19 Pandemic on Medical Care—A Romanian GPs’ Perspective" International Journal of Environmental Research and Public Health 18, no. 4: 2031. https://doi.org/10.3390/ijerph18042031
APA StyleStafie, C. S., Profire, L., Apostol, M. M., & Costache, I. I. (2021). The Professional and Psycho-Emotional Impact of the COVID-19 Pandemic on Medical Care—A Romanian GPs’ Perspective. International Journal of Environmental Research and Public Health, 18(4), 2031. https://doi.org/10.3390/ijerph18042031








