Company Representatives’ Experiences of Occupational Health Surveillance for Workers Exposed to Hand-Intensive Work: A Qualitative Study
Abstract
:1. Introduction
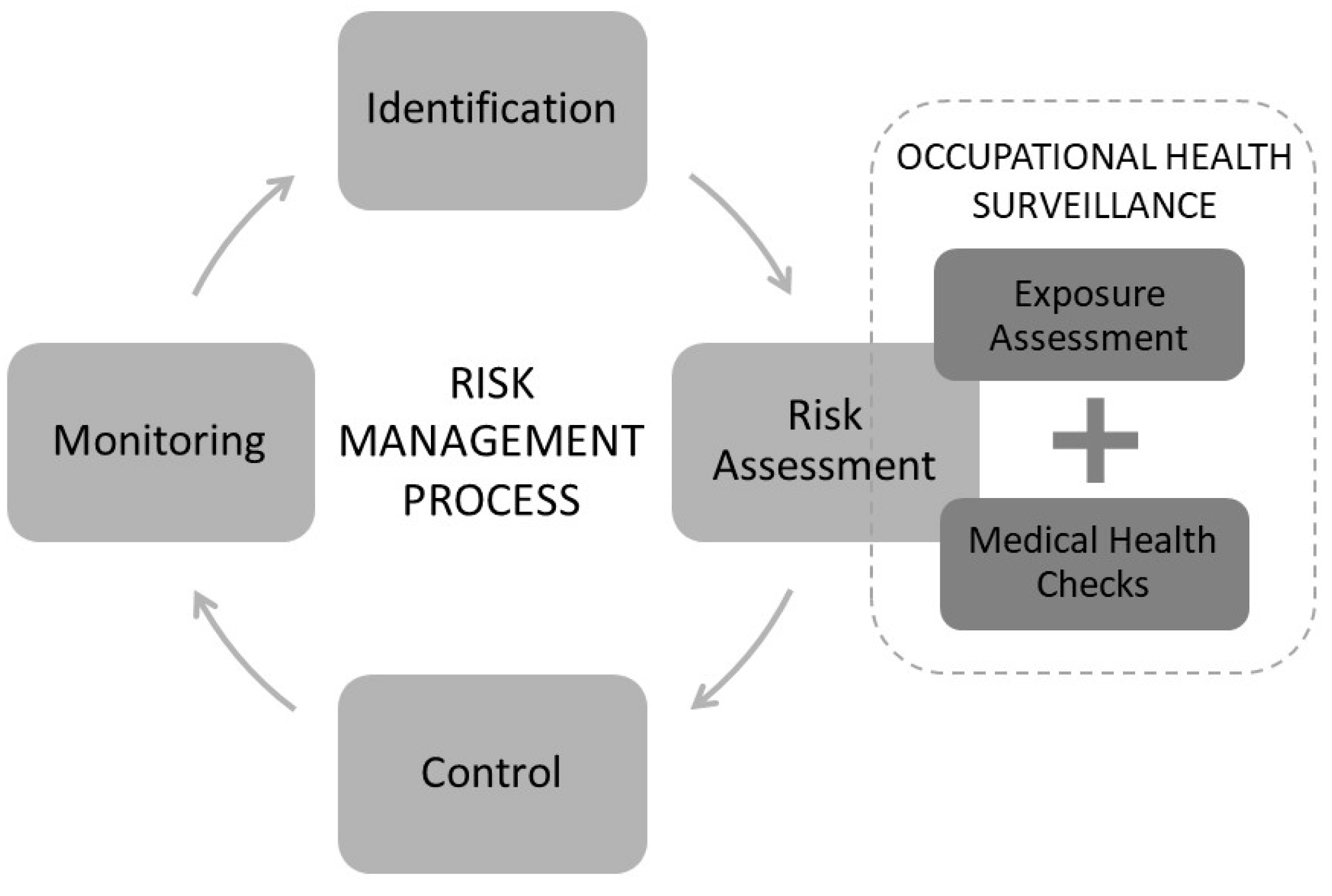
Musculoskeletal Disorders and Occupational Health Surveillance
2. Methods
2.1. Company Selection
2.2. Study Informants
2.3. Study Context
2.4. Data Collection
2.5. Data Analysis
3. Results
3.1. Model Components
3.1.1. Identification of Hand-Intensive Work
3.1.2. Exposure Assessment of Work
The Expert Validity
“It feels good to have the view from an outsider. You easily get blind to flaws at home. One does not really see the risks as an outsider does, so I think it has been valuable.”(Representative from company 9)
Increased Risk Awareness and Workplace Learning
“We never thought that we could get work related disorders in the same way as those with heavier work. But even though we work with lighter products, we have a high risk, and that has not been so obvious until now. And that is really good!”(Representative from company 8)
“Some of these models were new to us; it was the first time so to speak. So, it becomes like an educational part also.”(Representative from company 5)
3.1.3. Screening and Clinical Examination
“The concept hand-intensive is a bit misleading, I think, if you look at the clinical examinations and the discomforts, you do not have immediate pain in your hands.”(Representative from company 5)
“…You find that you have problems there; it is almost too late anyway, but at least it is so that more people will manage in the future... You might find if it is work-related and if so what we should do to avoid it tomorrow...”(Representative from company 7)
3.1.4. Feedback
Structure and Presentation of Feedback
“You do not need to know what all of these assessment tools are called and what numbers they have resulted in. But what is it that they have seen and what are we supposed to do. A little more straight forward!”(Representative from company 3)
Feedback—Valuable for Dissemination
3.2. Facilitating Factors and Barriers for the Execution of the Model
3.2.1. Planning and Preparation
3.2.2. Communication and Roles
“I think [it had been helpful] that steering it up a bit more in the beginning and also, you might have had some regular meetings as well.”(Representative from company 2)
“...in the communication, the language… there was a little to begin with, but when that was resolved, then there was like no weirdness but it worked well after that. So, that was exactly it and it is probably these small cultural differences we have that you have to work a little with.”(Representative from company 9)
“Invest in information before, during, after, get a group that becomes responsible for this, and that it will result in something so that you are willing to take action based on what the results show.”(Representative from company 10)
3.2.3. Collaboration
3.2.4. Outer and Inner Contextual Factors
“It has also obviously made it easier to have a head of department who actually wants to do this, because otherwise it is very difficult to carry out this in different departments.”(Representative from company 10)
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- European Council Directive. Council Directive of 12 June 1989 on the Introduction of Measures to Encourage Improvements in the Safety and Health of Workers at Work; 89/391/EEC; European Council: Brussels, Belgium, 1989. [Google Scholar]
- Arbetsmiljölagen Swedish Work Environmental Law; SFS 1977:1160; Arbetsmarknadsdepartementet: Stockholm, Sweden, 1977.
- Andersen, J.H.; Malmros, P.; Ebbehoej, N.E.; Flachs, E.M.; Bengtsen, E.; Bonde, J.P. Systematic literature review on the effects of occupational safety and health (OSH) interventions at the workplace. Scand. J. Work Environ. Health 2019, 45, 103–113. [Google Scholar] [CrossRef] [Green Version]
- Identifying Ill Health Through Health Surveillance. Available online: https://osha.europa.eu/en/themes/work-related-diseases/health-surveillance (accessed on 11 November 2019).
- International Labour Organization. Technical and Ethical Guidelines for Workers’ Health Surveillance; Occupational Safety and Health Series No. 72. International Labour Organization: Geneva, Switzerland, 1998. [Google Scholar]
- Bergsten, E.; Anundi, H.; Rehfisch, P.; Palm, P. Hälsoeffekter och Förebyggande Arbete vid Vibrationsexponering i Saneringsföretag; 3/2013; Arbets-Och Miljömedicin: Uppsala, Sweden, 2013. (In Swedish) [Google Scholar]
- Gunnarsson, L.-G.; Mölleby, G.; Porat, A.-M. Medicinsk Kontroll vid Användning av Handhållna Vibrerande Verktyg -Enkätstudie om Tillämpningen av Regeler i Företagshälsor och Företag; Center for Occupational and Environmental Medicine: Stockholm, Sweden, 2011. (In Swedish) [Google Scholar]
- Eliasson, K.; Palm, P.; Eriksson, T.; Nyman, T. Medicinska Kontroller—En Underutnyttjad Informationskälla i det Systematiska Arbetsmiljöarbetet; 2/2018; Arbets-Och Miljömedicin: Uppsala, Sweden, 2018. (In Swedish) [Google Scholar]
- Larsson, R.; Akerlind, I.; Sandmark, H. Managing workplace health promotion in municipal organizations: The perspective of senior managers. Work 2015, 53, 485–498. [Google Scholar] [CrossRef]
- Frick, K. The 50/50 Implementation of Sweden’s mandatory systematic work environment management. Policy Pract. Health Saf. 2014, 12. [Google Scholar] [CrossRef]
- Neumann, W.P.; Village, J. Ergonomics action research II: A framework for integrating HF into work system design. Ergonomics 2012, 55, 1140–1156. [Google Scholar] [CrossRef]
- Hasle, P.; Jensen, P.L. Changing the internal health and safety organization through organizational learning and change management. Hum. Factor Ergon. Man. 2006, 16, 269–284. [Google Scholar] [CrossRef]
- Schneider, E.; Irastorza, X.; Copsey, S. OSH in Figures: Work-Related Musculoskeletal Disorders in the EU—Facts and Figures; Publications Office of the European Union: Luxembourg, 2010. [Google Scholar]
- Bevan, S.; Qadrello, T.; McGee, R.; Mahdon, M.; Vavrovsky, A.; Barham, L. Fit for Work? Musculoskeletal Disorders in the European Workforce; The Work Foundation: London, UK, 2009. [Google Scholar]
- Arbetsmiljöverket. Swedish Work Environment Authority. In Arbetsorsakade Besvär 2018. Work-Related Disorders; Arbetsmiljöverket: Stockholm, Sweden, 2018. [Google Scholar]
- Försäkringskassan. Swedish Social Insurance Agency. In Sjukskrivningsdiagnoser i Olika Yrken; Socialförsäkringsrapport no. 2011:17; Försäkringskassan: Stockholm, Sweden, 2011. [Google Scholar]
- Van Rijn, R.M.; Huisstede, B.M.; Koes, B.W.; Burdorf, A. Associations between work-related factors and specific disorders of the shoulder—A systematic review of the literature. Scand. J. Work Environ. Health 2010, 36, 189–201. [Google Scholar] [CrossRef] [Green Version]
- Van Rijn, R.M.; Huisstede, B.M.A.; Koes, B.W.; Burdorf, A. Associations between work-related factors and specific disorders at the elbow: A systematic literature review. Rheumatology 2009, 48, 528–536. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Rijn, R.M.; Huisstede, B.M.; Koes, B.W.; Burdorf, A. Associations between work-related factors and the carpal tunnel syndrome—A systematic review. Scand. J. Work Environ. Health 2009, 35, 19–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palmer, K.T.; Harris, E.C.; Coggon, D. Carpal tunnel syndrome and its relation to occupation: A systematic literature review. Occup. Med. 2007, 57, 57–66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palmer, K.T.; Smedley, J. Work relatedness of chronic neck pain with physical findings—A systematic review. Scand. J. Work Environ. Health 2007, 33, 165–191. [Google Scholar] [CrossRef]
- Nordander, C.; Ohlsson, K.; Akesson, I.; Arvidsson, I.; Balogh, I.; Hansson, G.A.; Stromberg, U.; Rittner, R.; Skerfving, S. Exposure-response relationships in work-related musculoskeletal disorders in elbows and hands—A synthesis of group-level data on exposure and response obtained using uniform methods of data collection. Appl. Ergon. 2013, 44, 241–253. [Google Scholar] [CrossRef] [PubMed]
- Nordander, C.; Ohlsson, K.; Akesson, I.; Arvidsson, I.; Balogh, I.; Hansson, G.A.; Stromberg, U.; Rittner, R.; Skerfving, S. Risk of musculoskeletal disorders among females and males in repetitive/constrained work. Ergonomics 2009, 52, 1226–1239. [Google Scholar] [CrossRef] [PubMed]
- Violante, F.S.; Farioli, A.; Graziosi, F.; Marinelli, F.; Curti, S.; Armstrong, T.J.; Mattioli, S.; Bonfiglioli, R. Carpal tunnel syndrome and manual work: The OCTOPUS cohort, results of a ten-year longitudinal study. Scand. J. Work Environ. Health 2016, 42, 280–290. [Google Scholar] [CrossRef] [Green Version]
- Balogh, I.; Arvidsson, I.; Bjork, J.; Hansson, G.A.; Ohlsson, K.; Skerfving, S.; Nordander, C. Work-related neck and upper limb disorders—Quantitative exposure-response relationships adjusted for personal characteristics and psychosocial conditions. BMC Musculoskelet. Disord. 2019, 20, 139. [Google Scholar] [CrossRef] [Green Version]
- Yung, M.; Dale, A.M.; Kapellusch, J.; Bao, S.; Harris-Adamson, C.; Meyers, A.R.; Hegmann, K.T.; Rempel, D.; Evanoff, B.A. Modeling the effect of the 2018 revised ACGIH hand activity Threshold Limit Value (TLV) at reducing risk for carpal tunnel syndrome. J. Occup. Environ. Hyg. 2019, 16, 628–633. [Google Scholar] [CrossRef] [Green Version]
- May, D.C. Results of an OSHA ergonomic intervention program in New Hampshire. Appl. Occup. Environ. Hyg. 2002, 17, 768–773. [Google Scholar] [CrossRef] [PubMed]
- Foley, M.; Silverstein, B.; Polissar, N.; Neradilek, B. Impact of implementing the Washington State ergonomics rule on employer reported risk factors and hazard reduction activity. Am. J. Ind Med. 2009, 52, 1–16. [Google Scholar] [CrossRef]
- Martinsson, C.; Lohela-Karlsson, M.; Kwak, L.; Bergstrom, G.; Hellman, T. What incentives influence employers to engage in workplace health interventions? BMC Public Health 2016, 16, 854. [Google Scholar] [CrossRef] [Green Version]
- Arbetsmiljöverket. Swedish Work Environment Authority. In Medicinska Kontroller i Arbetslivet. Occupational Health Surveillance; Provision AFS 2019:3.; Arbetsmiljöverket: Stockholm, Sweden, 2019. [Google Scholar]
- Eliasson, K.; Palm, P.; Nordander, C.; Dahlgren, G.; Lewis, C.; Hellman, T.; Svartengren, M.; Nyman, T. Study protocol for a qualitative research project exploring an occupational health surveillance model for workers exposed to hand-intensive work. Int. J. Environ. Res. Public Health 2020, 17, 6400. [Google Scholar] [CrossRef]
- Glendon, I.; Clark, S.; McKenna, E. Human Safety and Risk Management, 2nd ed.; CRC Press Taylor & Francis Group: Boca Raton, FL, USA, 2006. [Google Scholar]
- Arbetsmiljöverket. Swedish Work Environment Authority. In Systematiskt arbetsmiljöarbete. Systematic Work Environment Management; Provision AFS 2001:1; Arbetsmiljöverket: Stockholm, Sweden, 2001. [Google Scholar]
- Roquelaure, Y.; Ha, C.; Leclerc, A.; Touranchet, A.; Sauteron, M.; Melchior, M.; Imbernon, E.; Goldberg, M. Epidemiologic surveillance of upper-extremity musculoskeletal disorders in the working population. Arthritis Rheum. 2006, 55, 765–778. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patton, M.Q. Qualitative Research & Evaluation Methods: Integrating Theory and Practice, 4th ed.; Sage Publications: New York, NY, USA, 2014. [Google Scholar]
- Graneheim, U.H.; Lundman, B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ. Today 2004, 24, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Elo, S.; Kyngas, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Azungah, T. Qualitative research: Deductive and inductive approaches to data analysis. Qual. Res. J. 2018, 18, 383–400. [Google Scholar] [CrossRef]
- Thomas, D.R. A general inductive approach for analyzing qualitative evaluation data. Am. J. Eval. 2006, 27, 237–246. [Google Scholar] [CrossRef]
- Elo, S.; Kääriäinen, M.; Kanste, O.; Pölkki, T.; Utriainen, K.; Kyngäs, H. Qualitative content analysis: A focus on trustworthiness. Sage Open 2014, 4, 1–10. [Google Scholar] [CrossRef]
- Graneheim, U.H.; Lindgren, B.-M.; Lundman, B. Methodological challenges in qualitative content analysis: A discussion paper. Nurse Educ. Today 2017, 56, 29–34. [Google Scholar] [CrossRef]
- Winnemuller, L.L.; Spielholz, P.O.; Daniell, W.E.; Kaufman, J.D. Comparison of ergonomist, supervisor, and worker assessments of work-related musculoskeletal risk factors. J. Occup. Environ. Hyg 2004, 1, 414–422. [Google Scholar] [CrossRef]
- Yazdani, A.; Hilbrecht, M.; Imbeau, D.; Bigelow, P.; Patrick Neumann, W.; Pagell, M.; Wells, R. Integration of musculoskeletal disorders prevention into management systems: A qualitative study of key informants’ perspectives. Saf. Sci. 2018, 104, 110–118. [Google Scholar] [CrossRef]
- Van Dongen, J.M.; Tompa, E.; Clune, L.; Sarnocinska-Hart, A.; Bongers, P.M.; van Tulder, M.W.; van der Beek, A.J.; van Wier, M.F. Bridging the gap between the economic evaluation literature and daily practice in occupational health: A qualitative study among decision-makers in the healthcare sector. Implement. Sci. 2013, 8, 57. [Google Scholar] [CrossRef] [Green Version]
- Miller, P.; Haslam, C. Why employers spend money on employee health: Interviews with occupational health and safety professionals from British Industry. Saf. Sci. 2009, 47, 163–169. [Google Scholar] [CrossRef]
- Eliasson, K.; Forsman, M.; Nyman, T. Exploring ergonomists’ experiences after participation in a theoretical and practical research project in observational risk assessment tools. Int. J. Occup. Saf. Erg. 2021. [Google Scholar] [CrossRef] [PubMed]
- Yazdani, A.; Wells, R. Barriers for implementation of successful change to prevent musculoskeletal disorders and how to systematically address them. Appl. Erg. 2018, 73, 122–140. [Google Scholar] [CrossRef]
- Haines, H.; Wilson, J.R.; Vink, P.; Koningsveld, E. Validating a framework for participatory ergonomics (the PEF). Ergonomics 2002, 45, 309–327. [Google Scholar] [CrossRef]
- Halonen, J.I.; Atkins, S.; Hakulinen, H.; Pesonen, S.; Uitti, J. Collaboration between employers and occupational health service providers: A systematic review of key characteristics. BMC Public Health 2017, 17, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Eerd, D.; King, T.; Keown, K.; Slack, T.; Cole, D.C.; Irvin, E.; Amick, B.C.; Bigelow, P. Dissemination and use of a participatory ergonomics guide for workplaces. Ergonomics 2016, 59, 851–858. [Google Scholar] [CrossRef]
- Van Eerd, D.; Cole, D.; Irvin, E.; Mahood, Q.; Keown, K.; Theberge, N.; Village, J.; Vincent, M.S.; Cullen, K. Process and implementation of participatory ergonomic interventions: A systematic review. Ergonomics 2010, 53, 1153–1166. [Google Scholar] [CrossRef]
- Motamedzade, M.; Shahnavaz, H.; Kazemnejad, A.; Azar, A.; Karimi, H. The impact of participatory ergonomics on working conditions, quality, and productivity. Int. J. Occup. Saf. 2003, 9, 135–147. [Google Scholar] [CrossRef] [PubMed]
- Burgess-Limerick, R.; Straker, L.; Pollock, C.; Dennis, G.; Leveritt, S.; Johnson, S. Implementation of the Participative Ergonomics for Manual tasks (PErforM) programme at four Australian underground coal mines. Int. J. Ind. Erg. 2007, 37, 145–155. [Google Scholar] [CrossRef]
- Burgess-Limerick, R. Participatory ergonomics: Evidence and implementation lessons. Appl. Erg. 2018, 68, 289–293. [Google Scholar] [CrossRef]
- Shenton, A.K. Strategies for ensuring trustworthiness in qualitative research projects. Educ. Inf. 2004, 22, 63–75. [Google Scholar] [CrossRef] [Green Version]
- Nordlof, H.; Wijk, K.; Westergren, K.E. Perceptions of work environment priorities: Are there any differences by company size? An ecological study. Work 2015, 52, 697–706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schmidt, L.; Sjöström, J.; Antonsson, A.-B. Understanding the challenges facing occupational health services in the Swedish Public Sector. Nord. J. Work Life Stud. 2017, 7, 85–104. [Google Scholar] [CrossRef] [Green Version]

| No. | Organization Size (n of Employees) | Intervention Work Group Size (m/f) | Project Group | |||
|---|---|---|---|---|---|---|
| Company Representatives | Ergonomist | |||||
| Title | Work Experience in Current Role (Years) | OHS a-Provider | Work Experience in Ergonomics (Years) | |||
| 1 | Large > 250 | 12 (6/6) | First line manager | 1 | In-house | 27 |
| HSE manager | 2 | |||||
| Safety representative b | 2 | |||||
| 2 | Medium > 50 | 11 (0/11) | Central HSE manager | 3 | External | 5 |
| Local manager | 20 | |||||
| Safety representative | 28 | |||||
| 3 | Large > 250 | 7 (7/0) | First line manager | 20 | External | 9 |
| First-line manager | 20 | |||||
| Manager | 7 | |||||
| 4 | Large > 250 | 26 (10/12) | First line manager | 1 | External | 24 |
| First-line manager b | 12 | |||||
| First-line manager | - | |||||
| HSE manager | - | |||||
| HSE manager | - | |||||
| Safety representatives | - | |||||
| Safety representatives | - | |||||
| Safety representatives | - | |||||
| 5 | Small < 50 | 11 (0/11) | Production manager | 3 | External | 6 |
| First-line manager | 9 | |||||
| First-line manager | 2 | |||||
| Technology manager b | 4 | |||||
| Safety representative | - | |||||
| Safety representative | - | |||||
| 6 | Medium > 50 | 27 (11/16) | Manager | 12 | External | 20 |
| First-line manager | - | |||||
| 7 | Medium > 50 | 22 (12/10) | Production manager | - | External | 14 |
| Safety representative | - | |||||
| 8 | Medium > 50 | 7 (4/3) | Manager | - | External | 12 |
| HR-manager | 24 | |||||
| Safety representative | 34 | |||||
| 9 | Small < 50 | 11 (0/11) | CEO/founder | 4 | External | 34 |
| HSE manager | 2 | |||||
| Central safety representative | 5 | |||||
| 10 | Large > 250 | 21 (0/21) | HR-manager | 3 | External | 14 |
| Production manager | - | |||||
| First-line manager | 8 | |||||
| Model Components |
| Identification of hand intensive work |
| Exposure assessment of work |
| The expert validity |
| Increased risk awareness and workplace learning |
| Screening and clinical examination |
| Feedback |
| Structure and presentation of feedback |
| Valuable for dissemination |
| Facilitating factors and barriers for the execution of the model |
| Planning and preparation |
| Communication and roles |
| Outer and inner contextual factors |
| Collaboration |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eliasson, K.; Dahlgren, G.; Hellman, T.; Lewis, C.; Palm, P.; Svartengren, M.; Nyman, T. Company Representatives’ Experiences of Occupational Health Surveillance for Workers Exposed to Hand-Intensive Work: A Qualitative Study. Int. J. Environ. Res. Public Health 2021, 18, 2018. https://doi.org/10.3390/ijerph18042018
Eliasson K, Dahlgren G, Hellman T, Lewis C, Palm P, Svartengren M, Nyman T. Company Representatives’ Experiences of Occupational Health Surveillance for Workers Exposed to Hand-Intensive Work: A Qualitative Study. International Journal of Environmental Research and Public Health. 2021; 18(4):2018. https://doi.org/10.3390/ijerph18042018
Chicago/Turabian StyleEliasson, Kristina, Gunilla Dahlgren, Therese Hellman, Charlotte Lewis, Peter Palm, Magnus Svartengren, and Teresia Nyman. 2021. "Company Representatives’ Experiences of Occupational Health Surveillance for Workers Exposed to Hand-Intensive Work: A Qualitative Study" International Journal of Environmental Research and Public Health 18, no. 4: 2018. https://doi.org/10.3390/ijerph18042018
APA StyleEliasson, K., Dahlgren, G., Hellman, T., Lewis, C., Palm, P., Svartengren, M., & Nyman, T. (2021). Company Representatives’ Experiences of Occupational Health Surveillance for Workers Exposed to Hand-Intensive Work: A Qualitative Study. International Journal of Environmental Research and Public Health, 18(4), 2018. https://doi.org/10.3390/ijerph18042018








