Malaria in Cambodia: A Retrospective Analysis of a Changing Epidemiology 2006–2019
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources
2.1.1. Malaria Data
2.1.2. Population Data and Maps
2.1.3. Untoward Events
2.2. Inclusion Criteria and Setting
2.3. Case Definition
- −
- had fever, chills, or sweats or two of the following: headache, nausea, vomiting, diarrhea, AND
- −
- any of the following: traveled to the forest in the previous month, had confirmed malaria in the past 28 days, traveled to a malaria-endemic area from a non-endemic area, or lived or worked around others with a recently confirmed malaria diagnosis [47].
2.4. Data Analysis
3. Results
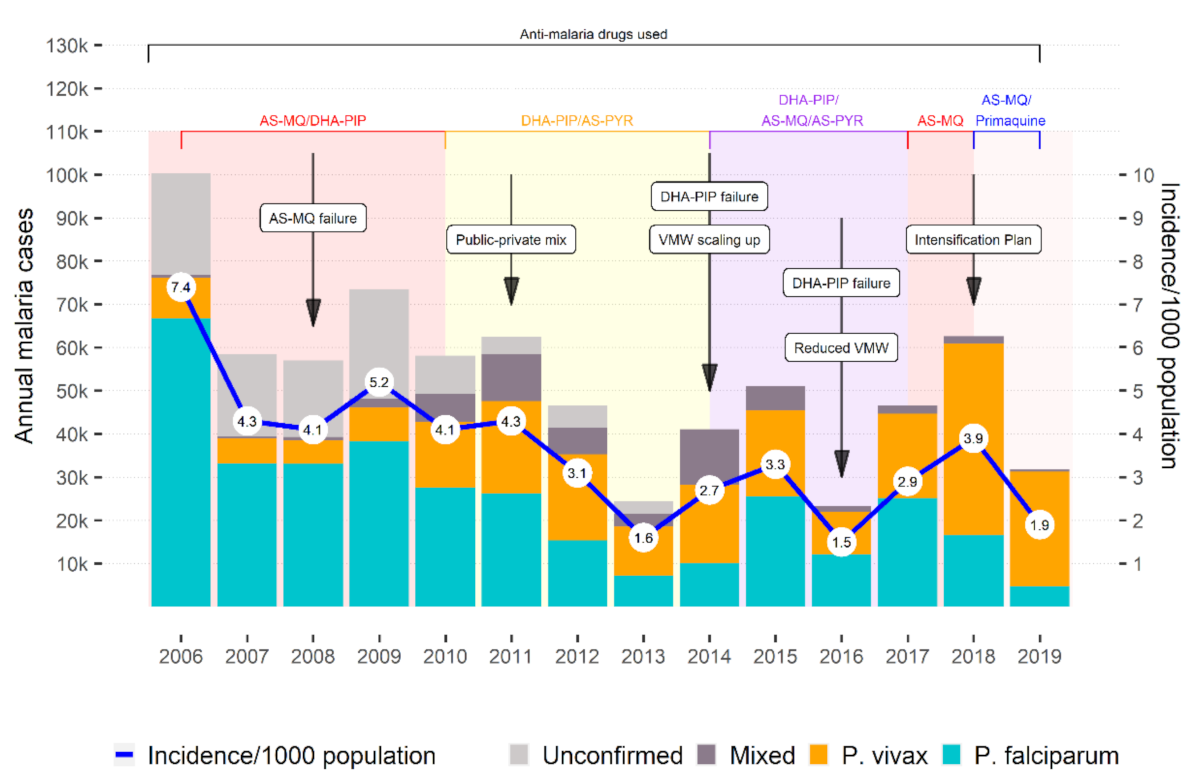
3.1. Overall Malaria Cases and Incidence Rate
3.2. Incidence by Sex
3.3. Incidence by Age Group
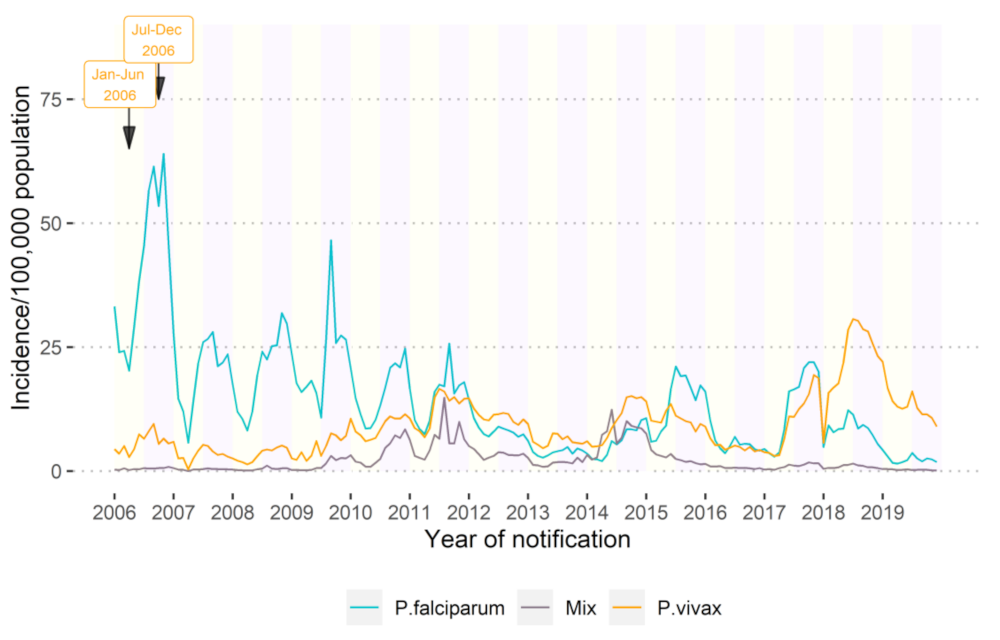
3.4. Seasonality
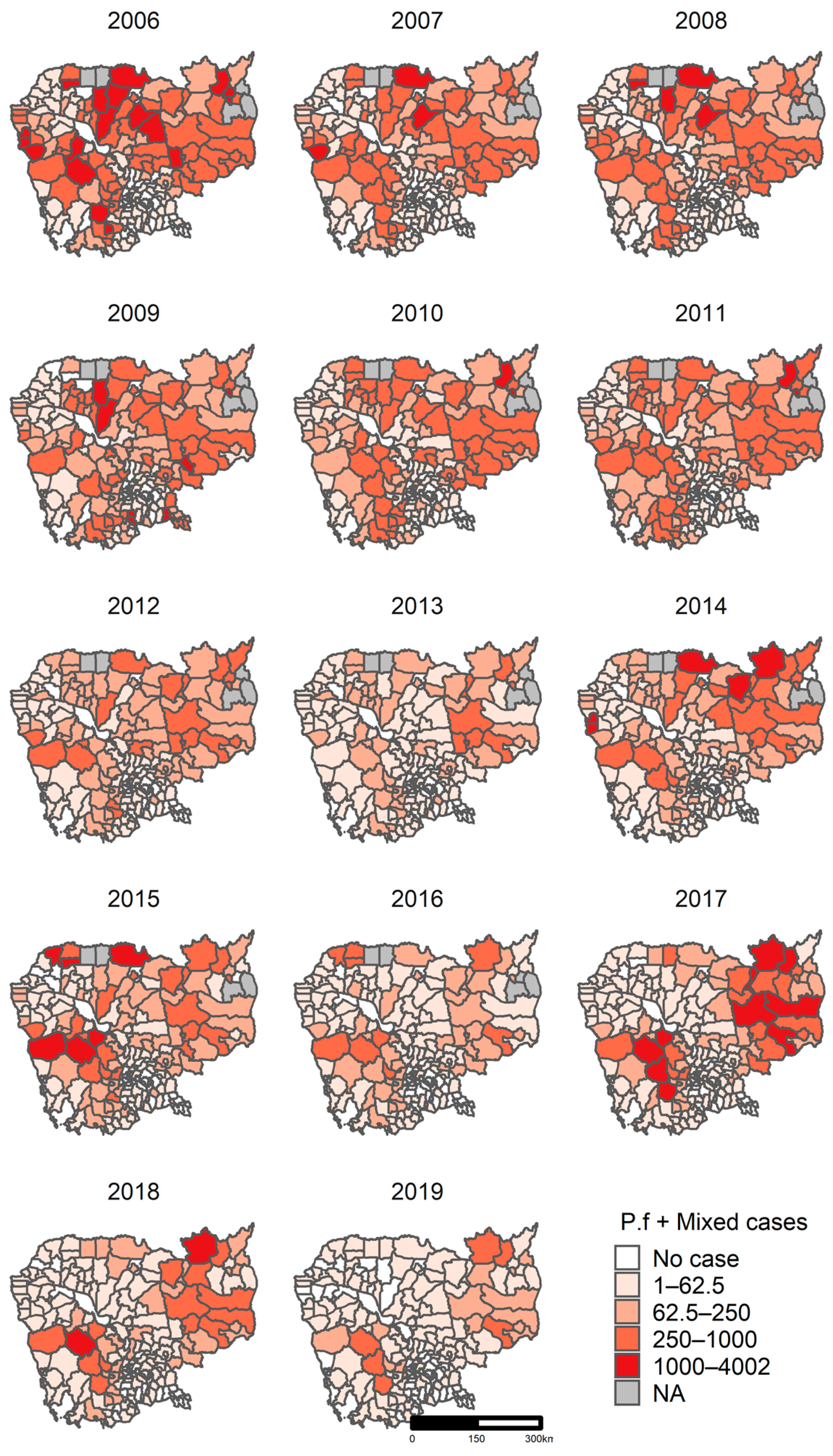
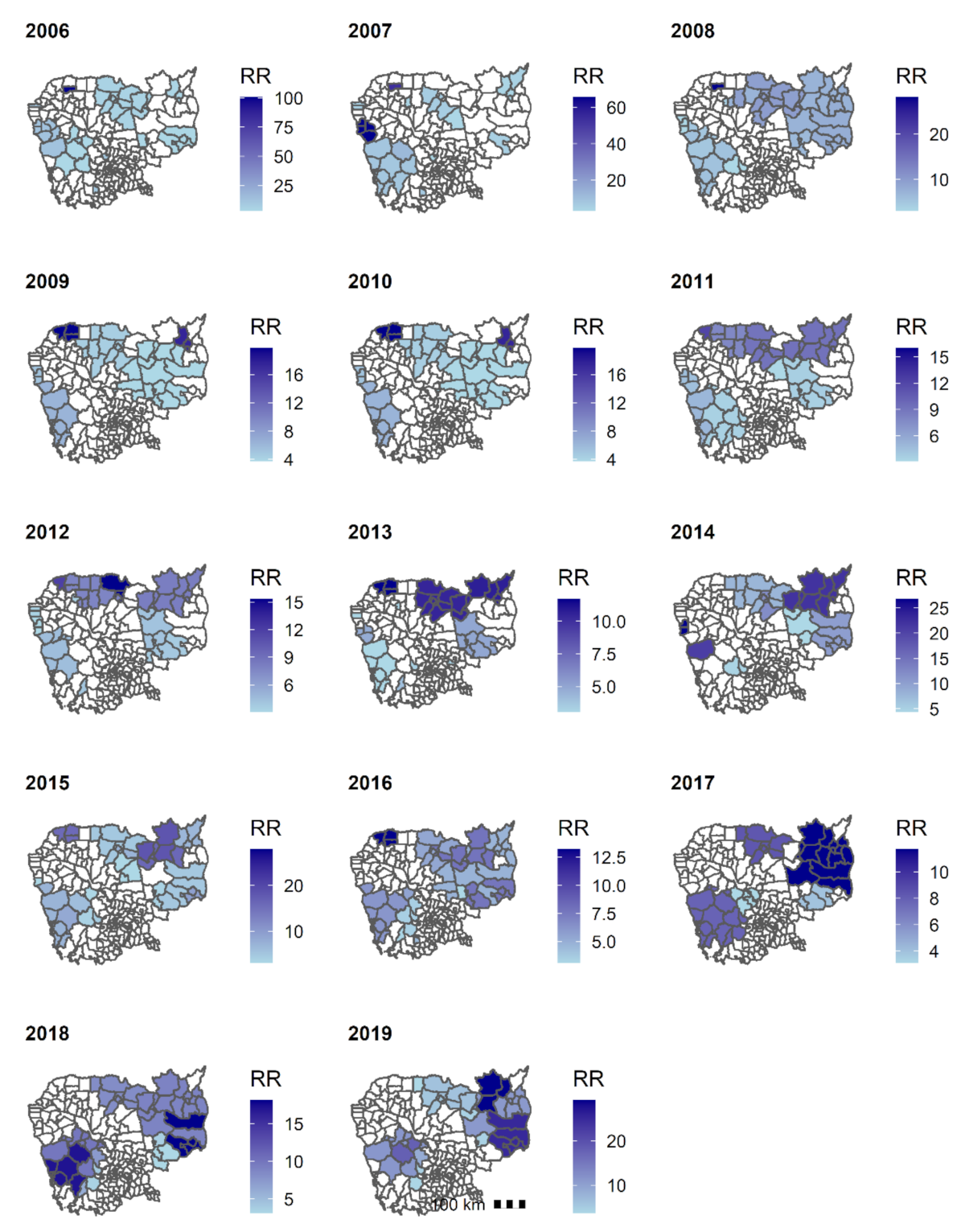
3.5. Geographical Distribution
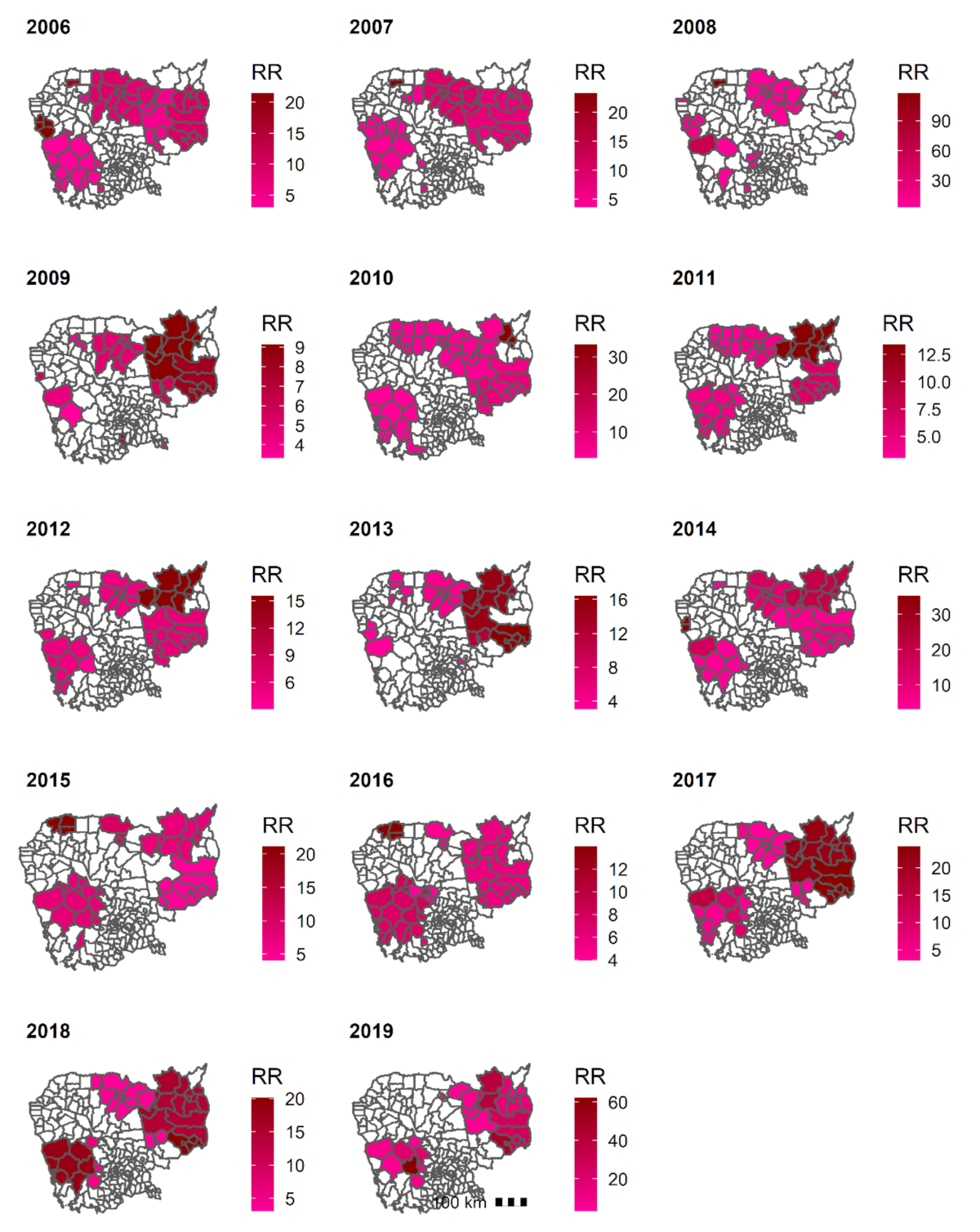
3.5.1. Clusters of P. falciparum + Mixed
3.5.2. Clusters of P. vivax + Mixed
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Centers for Disease Control and Prevention (CDC) Malaria. Available online: https://www.cdc.gov/malaria/about/faqs.html (accessed on 15 August 2020).
- WHO. World Malaria Report; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- World Health Organization (WHO). WHO African Region. Available online: https://www.who.int/immunization/monitoring_surveillance/data/AFR/en/ (accessed on 28 August 2020).
- World Health Organization (WHO). WHO Western Pacific Region. Available online: https://www.who.int/westernpacific (accessed on 28 August 2020).
- World Health Organization (WHO). Region of the Americas. Available online: https://www.who.int/choice/demography/american_region/en/ (accessed on 29 August 2020).
- National Centre for Parasitology Entomology and Malaria Control (CNM). Cambodia Malaria Elimination Action Framework (2016–2020); CNM: Phnom Penh, Cambodia, 2016.
- National Centre for Parasitology Entomology and Malaria Control (CNM). National Malaria Porgram Review; CNM: Phnom Penh, Cambodia, 2019.
- St. Laurent, B.; Oy, K.; Miller, B.; Gasteiger, E.B.; Lee, E.; Sovannaroth, S.; Gwadz, R.W.; Anderson, J.M.; Fairhurst, R.M. Cow-baited tents are highly effective in sampling diverse Anopheles malaria vectors in Cambodia. Malar. J. 2016, 15, 440. [Google Scholar] [CrossRef]
- Durnez, L.; Mao, S.; Denis, L.; Roelants, P.; Sochantha, T.; Coosemans, M. Outdoor malaria transmission in forested villages of Cambodia. Malar. J. 2013, 12, 329. [Google Scholar] [CrossRef]
- Hii, J.; Rueda, L.M. Malaria vectors in the Greater Mekong Subregion: Overview of malaria vectors and remaining challenges. Southeast Asian J. Trop. Med. Public Health 2013, 44, 73–165, discussion 306–307. [Google Scholar]
- Bannister-Tyrrell, M.; Gryseels, C.; Sokha, S.; Dara, L.; Sereiboth, N.; James, N.; Thavrin, B.; Ly, P.; Soy Ty, K.; Peeters Grietens, K.; et al. Forest Goers and Multidrug-Resistant Malaria in Cambodia: An Ethnographic Study. Am. J. Trop. Med. Hyg. 2019, 100, 1170–1178. [Google Scholar] [CrossRef]
- Incardona, S.; Vong, S.; Chiv, L.; Lim, P.; Nhem, S.; Sem, R.; Khim, N.; Doung, S.; Mercereau-Puijalon, O.; Fandeur, T. Large-scale malaria survey in Cambodia: Novel insights on species distribution and risk factors. Malar. J. 2007, 6, 37. [Google Scholar] [CrossRef] [PubMed]
- National Centre for Parasitology Entomology and Malaria Control (CNM). The National Strategic Plan for Elimination of Malaria in the Kingdom of Cambodia 2011–2025; CNM: Phnom Penh, Cambodia, 2011.
- WHO. World Malaria Report; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- ACTwatch Cambodia 2009–2015 Reference Document. Available online: http://www.actwatch.info/projects/actwatch/cambodia (accessed on 21 November 2019).
- Group, A.C.; Phok, S.; Phanalasy, S.; Thein, S.T.; Likhitsup, A. Private sector opportunities and threats to achieving malaria elimination in the Greater Mekong Subregion: Results from malaria outlet surveys in Cambodia, the Lao PDR, Myanmar, and Thailand. Malar. J. 2017, 16, 180. [Google Scholar]
- Dondorp, A.M.; Fairhurst, R.M.; Slutsker, L.; Macarthur, J.R.; Breman, J.G.; Guerin, P.J.; Wellems, T.E.; Ringwald, P.; Newman, R.D.; Plowe, C.V. The threat of artemisinin-resistant malaria. N. Engl. J. Med. 2011, 365, 1073–1075. [Google Scholar] [CrossRef]
- Mahase, E. Malaria drugs left ineffective by spread of multidrug resistant parasites in southeast Asia. BMJ 2019, 366, l4807. [Google Scholar] [CrossRef]
- van der Pluijm, R.W.; Imwong, M.; Chau, N.H.; Hoa, N.T.; Thuy-Nhien, N.T.; Thanh, N.V.; Jittamala, P.; Hanboonkunupakarn, B.; Chutasmit, K.; Saelow, C.; et al. Determinants of dihydroartemisinin-piperaquine treatment failure in Plasmodium falciparum malaria in Cambodia, Thailand, and Vietnam: A prospective clinical, pharmacological, and genetic study. Lancet Infect. Dis. 2019, 19, 952–961. [Google Scholar] [CrossRef]
- Hamilton, W.L.; Amato, R.; van der Pluijm, R.W.; Jacob, C.G.; Quang, H.H.; Thuy-Nhien, N.T.; Hien, T.T.; Hongvanthong, B.; Chindavongsa, K.; Mayxay, M.; et al. Evolution and expansion of multidrug-resistant malaria in southeast Asia: A genomic epidemiology study. Lancet Infect. Dis. 2019, 19, 943–951. [Google Scholar] [CrossRef]
- Imwong, M.; Hien, T.T.; Thuy-Nhien, N.T.; Dondorp, A.M.; White, N.J. Spread of a single multidrug resistant malaria parasite lineage (PfPailin) to Vietnam. Lancet Infect. Dis. 2017, 17, 1022–1023. [Google Scholar] [CrossRef]
- Imwong, M.; Suwannasin, K.; Kunasol, C.; Sutawong, K.; Mayxay, M.; Rekol, H.; Smithuis, F.M.; Hlaing, T.M.; Tun, K.M.; van der Pluijm, R.W.; et al. The spread of artemisinin-resistant Plasmodium falciparum in the Greater Mekong subregion: A molecular epidemiology observational study. Lancet Infect. Dis. 2017, 17, 491–497. [Google Scholar] [CrossRef]
- Denis, M.B.; Tsuyuoka, R.; Poravuth, Y.; Narann, T.S.; Seila, S.; Lim, C.; Incardona, S.; Lim, P.; Sem, R.; Socheat, D.; et al. Surveillance of the efficacy of artesunate and mefloquine combination for the treatment of uncomplicated falciparum malaria in Cambodia. Trop. Med. Int. Health TM IH 2006, 11, 1360–1366. [Google Scholar] [CrossRef] [PubMed]
- Noedl, H.; Se, Y.; Schaecher, K.; Smith, B.L.; Socheat, D.; Fukuda, M.M. Evidence of artemisinin-resistant malaria in western Cambodia. N. Engl. J. Med. 2008, 359, 2619–2620. [Google Scholar] [CrossRef]
- Lim, P.; Chim, P.; Sem, R.; Nemh, S.; Poravuth, Y.; Lim, C.; Seila, S.; Tsuyuoka, R.; Denis, M.B.; Socheat, D.; et al. In vitro monitoring of Plasmodium falciparum susceptibility to artesunate, mefloquine, quinine and chloroquine in Cambodia: 2001–2002. Acta Trop. 2005, 93, 31–40. [Google Scholar] [CrossRef]
- Bustos, M.D.; Wongsrichanalai, C.; Delacollette, C.; Burkholder, B. Monitoring antimalarial drug efficacy in the Greater Mekong Subregion: An overview of in vivo results from 2008 to 2010. Southeast Asian J. Trop. Med. Public Health 2013, 44, 201–230, discussion 306–307. [Google Scholar]
- Amaratunga, C.; Lim, P.; Suon, S.; Sreng, S.; Mao, S.; Sopha, C.; Sam, B.; Dek, D.; Try, V.; Amato, R.; et al. Dihydroartemisinin—piperaquine resistance in Plasmodium falciparum malaria in Cambodia: A multisite prospective cohort study. Lancet Infect. Dis. 2016, 16, 357–365. [Google Scholar] [CrossRef]
- Spring, M.D.; Lin, J.T.; Manning, J.E.; Vanachayangkul, P.; Somethy, S.; Bun, R.; Se, Y.; Chann, S.; Ittiverakul, M.; Sia-ngam, P.; et al. Dihydroartemisinin-piperaquine failure associated with a triple mutant including kelch13 C580Y in Cambodia: An observational cohort study. Lancet Infect. Dis. 2015, 15, 683–691. [Google Scholar] [CrossRef]
- Lon, C.; Manning, J.E.; Vanachayangkul, P.; So, M.; Sea, D.; Se, Y.; Gosi, P.; Lanteri, C.; Chaorattanakawee, S.; Sriwichai, S.; et al. Efficacy of two versus three-day regimens of dihydroartemisinin-piperaquine for uncomplicated malaria in military personnel in northern Cambodia: An open-label randomized trial. PLoS ONE 2014, 9, e93138. [Google Scholar] [CrossRef] [PubMed]
- Boyle, D. Dispute delays release of malaria money in Cambodia. Lancet 2015, 386, 1811. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Global Technical Strategy for Malaria 2016–2030; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Thacker, S.B.; Choi, K.; Brachman, P.S. The Surveillance of Infectious Diseases. JAMA 1983, 249, 1181–1185. [Google Scholar] [CrossRef]
- Aregawi, M.; Lynch, M.; Bekele, W.; Kebede, H.; Jima, D.; Taffese, H.S.; Yenehun, M.A.; Lilay, A.; Williams, R.; Thomson, M.; et al. Time series analysis of trends in malaria cases and deaths at hospitals and the effect of antimalarial interventions, 2001–2011, Ethiopia. PLoS ONE 2014, 9, e106359. [Google Scholar] [CrossRef] [PubMed]
- Comfort, A.B.; van Dijk, J.H.; Mharakurwa, S.; Stillman, K.; Gabert, R.; Korde, S.; Nachbar, N.; Derriennic, Y.; Musau, S.; Hamazakaza, P.; et al. Hospitalizations and costs incurred at the facility level after scale-up of malaria control: Pre-post comparisons from two hospitals in Zambia. Am. J. Trop. Med. Hyg. 2014, 90, 20–32. [Google Scholar] [CrossRef]
- Cissé, B.; Ba, E.H.; Sokhna, C.; Ndiaye, J.L.; Gomis, J.F.; Dial, Y.; Pitt, C.; Ndiaye, M.; Cairns, M.; Faye, E.; et al. Effectiveness of Seasonal Malaria Chemoprevention in Children under Ten Years of Age in Senegal: A Stepped-Wedge Cluster-Randomised Trial. PLoS Med. 2016, 13, e1002175. [Google Scholar] [CrossRef]
- Katureebe, A.; Zinszer, K.; Arinaitwe, E.; Rek, J.; Kakande, E.; Charland, K.; Kigozi, R.; Kilama, M.; Nankabirwa, J.; Yeka, A.; et al. Measures of Malaria Burden after Long-Lasting Insecticidal Net Distribution and Indoor Residual Spraying at Three Sites in Uganda: A Prospective Observational Study. PLoS Med. 2016, 13, e1002167. [Google Scholar] [CrossRef]
- Aregawi, M.; Malm, K.L.; Wahjib, M.; Kofi, O.; Allotey, N.K.; Yaw, P.N.; Abba-Baffoe, W.; Segbaya, S.; Owusu-Antwi, F.; Kharchi, A.T.; et al. Effect of anti-malarial interventions on trends of malaria cases, hospital admissions and deaths, 2005–2015, Ghana. Malar. J. 2017, 16, 177. [Google Scholar] [CrossRef]
- Ssempiira, J.; Kissa, J.; Nambuusi, B.; Kyozira, C.; Rutazaana, D.; Mukooyo, E.; Opigo, J.; Makumbi, F.; Kasasa, S.; Vounatsou, P. The effect of case management and vector-control interventions on space-time patterns of malaria incidence in Uganda. Malar. J. 2018, 17, 162. [Google Scholar] [CrossRef]
- Kenangalem, E.; Poespoprodjo, J.R.; Douglas, N.M.; Burdam, F.H.; Gdeumana, K.; Chalfein, F.; Prayoga; Thio, F.; Devine, A.; Marfurt, J.; et al. Malaria morbidity and mortality following introduction of a universal policy of artemisinin-based treatment for malaria in Papua, Indonesia: A longitudinal surveillance study. PLoS Med. 2019, 16, e1002815. [Google Scholar] [CrossRef] [PubMed]
- Lechthaler, F.; Matthys, B.; Lechthaler-Felber, G.; Likwela, J.L.; Mavoko, H.M.; Rika, J.M.; Mutombo, M.M.; Ruckstuhl, L.; Barczyk, J.; Shargie, E.; et al. Trends in reported malaria cases and the effects of malaria control in the Democratic Republic of the Congo. PLoS ONE 2019, 14, e0219853. [Google Scholar] [CrossRef] [PubMed]
- Tugume, A.; Muneza, F.; Oporia, F.; Kiconco, A.; Kihembo, C.; Kisakye, A.N.; Nsubuga, P.; Deogratias, S.; Yeka, A. Effects and factors associated with indoor residual spraying with Actellic 300 CS on malaria morbidity in Lira District, Northern Uganda. Malar. J. 2019, 18, 44. [Google Scholar] [CrossRef]
- Department of Planning and Health Information (DPHI). Health Information System Master Plan 2016–2020; DPHI: Phnom Penh, Cambodia, 2017. [Google Scholar]
- National Centre for Parasitology Entomology and Malaria Control (CNM). Malaria Information System; CNM: Phnom Penh, Cambodia, 2020.
- World Health Organization (WHO). WHO Malaria Terminology; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- OCHA. Cambodia Administrative Level 0–3 Population Statistics; OCHA: New York, NY, USA, 2019. [Google Scholar]
- National Institute of Statistics (NIS). Population Projections for Cambodia, 2008–2030; NIS: Phnom Penh, Cambodia, 2008.
- National Center for Parasitology Entomology and Malaria Control (CNM). National Treatment Guidelines for Malaria in Cambodia; CNM: Phnom Penh, Cambodia, 2014.
- Kulldorff, M. A spatial scan statistic. Commun. Stat. Theory Methods 1997, 26, 1481–1496. [Google Scholar] [CrossRef]
- Martin, K. SaTScan™, a Free Software That Analyzes Spatial, Temporal and Space-Time Data Using the Spatial, Temporal, or Space-Time Scan Statistics. Available online: https://www.satscan.org/ (accessed on 20 March 2019).
- Maude, R.J.; Nguon, C.; Ly, P.; Bunkea, T.; Ngor, P.; Canavati de la Torre, S.E.; White, N.J.; Dondorp, A.M.; Day, N.P.J.; White, L.J.; et al. Spatial and temporal epidemiology of clinical malaria in Cambodia 2004–2013. Malar. J. 2014, 13, 385. [Google Scholar] [CrossRef] [PubMed]
- Gao, H.-W.; Wang, L.-P.; Liang, S.; Liu, Y.-X.; Tong, S.-L.; Wang, J.-J.; Li, Y.-P.; Wang, X.-F.; Yang, H.; Ma, J.-Q.; et al. Change in Rainfall Drives Malaria Re-Emergence in Anhui Province, China. PLoS ONE 2012, 7, e43686. [Google Scholar] [CrossRef]
- Wardrop, N.A.; Barnett, A.G.; Atkinson, J.-A.; Clements, A.C.A. Plasmodium vivax malaria incidence over time and its association with temperature and rainfall in four counties of Yunnan Province, China. Malar. J. 2013, 12, 452. [Google Scholar] [CrossRef]
- Huang, F.; Zhou, S.; Zhang, S.; Wang, H.; Tang, L. Temporal correlation analysis between malaria and meteorological factors in Motuo County, Tibet. Malar. J. 2011, 10, 54. [Google Scholar] [CrossRef]
- Bomblies, A. Modeling the role of rainfall patterns in seasonal malaria transmission. Clim. Chang. 2012, 112, 673–685. [Google Scholar] [CrossRef]
- US Department of Interior. United States Geological Survey (USGS); U.S. Department of Interior: Washington, DC, USA, 2020.
- Sluydts, V.; Somony, H.; Coosemans, M.; Van Roey, K.; Gryseels, C.; Canier, L.; Kim, S.; Khim, N.; Sovannaroth, S.; Mean, V.; et al. Spatial clustering and risk factors of malaria infections in Ratanakiri Province, Cambodia. Malar. J. 2014, 13, 387. [Google Scholar] [CrossRef] [PubMed]
- An, U.S.; Mao, B.; Saphonn, V.; Bruce, J.; Meek, S.; Lines, J.; Cox, J. Cambodia Malaria Survey 2007; National Centre for Parasitology, Entomology and Malaria Control (CNM): Phnom Penh, Cambodia, 2007.
- Dysoley, L.; Rithea, L.; Bunkea, T.; Babu, S.; Sim, K.; Nguon, C.; Socheat, D.; Thompson, M.; Bruce, J.; de Beyl, C.Z.; et al. Cambodia Malaria Survey 2010; National Centre for Parasitology, Entomology and Malaria Control (CNM): Phnom Penh, Cambodia, 2010.
- Rekol, H.; Sovannaroth, S.; Dysoley, L.; Vanna, C.; Sokun, C.; Yeang, O.; Thavrin, B.K.; Montha, M.; Yom, Y.; Theasy, H.C.; et al. Cambodia Malaria Survey 2013; National Centre for Parasitology, Entomology and Malaria Control (CNM): Phnom Penh, Cambodia, 2013.
- National Centre for Parasitology, Entomology and Malaria Control (CNM). Cambodia Malaria Survey 2017; CNM: Phnom Penh, Cambodia, 2017.
- Jambou, R.; Legrand, E.; Niang, M.; Khim, N.; Lim, P.; Volney, B.; Ekala, M.T.; Bouchier, C.; Esterre, P.; Fandeur, T.; et al. Resistance of Plasmodium falciparum field isolates to in-vitro artemether and point mutations of the SERCA-type PfATPase6. Lancet 2005, 366, 1960–1963. [Google Scholar] [CrossRef]
- Khim, N.; Bouchier, C.; Ekala, M.T.; Incardona, S.; Lim, P.; Legrand, E.; Jambou, R.; Doung, S.; Puijalon, O.M.; Fandeur, T. Countrywide survey shows very high prevalence of Plasmodium falciparum multilocus resistance genotypes in Cambodia. Antimicrob. Agents Chemother. 2005, 49, 3147–3152. [Google Scholar] [CrossRef]
- Denis, M.B.; Tsuyuoka, R.; Lim, P.; Lindegardh, N.; Yi, P.; Top, S.N.; Socheat, D.; Fandeur, T.; Annerberg, A.; Christophel, E.M.; et al. Efficacy of artemether-lumefantrine for the treatment of uncomplicated falciparum malaria in northwest Cambodia. Trop. Med. Int. Health TM IH 2006, 11, 1800–1807. [Google Scholar] [CrossRef] [PubMed]
- Resistance to artemisinin derivatives along the Thai-Cambodian border. Relev. Epidemiol. Hebd. 2007, 82, 360.
- Shah, N.K.; Alker, A.P.; Sem, R.; Susanti, A.I.; Muth, S.; Maguire, J.D.; Duong, S.; Ariey, F.; Meshnick, S.R.; Wongsrichanalai, C. Molecular surveillance for multidrug-resistant Plasmodium falciparum, Cambodia. Emerg. Infect. Dis. 2008, 14, 1637–1640. [Google Scholar] [CrossRef]
- Wongsrichanalai, C.; Meshnick, S.R. Declining artesunate-mefloquine efficacy against falciparum malaria on the Cambodia-Thailand border. Emerg. Infect. Dis. 2008, 14, 716–719. [Google Scholar] [CrossRef] [PubMed]
- Antimalarial drug resistance, Thai-Cambodian border. Relev. Epidemiol. Hebd. 2009, 84, 94–95.
- Dondorp, A.M.; Nosten, F.; Yi, P.; Das, D.; Phyo, A.P.; Tarning, J.; Lwin, K.M.; Ariey, F.; Hanpithakpong, W.; Lee, S.J.; et al. Artemisinin resistance in Plasmodium falciparum malaria. N. Engl. J. Med. 2009, 361, 455–467. [Google Scholar] [CrossRef] [PubMed]
- Müller, O.; Sié, A.; Meissner, P.; Schirmer, R.H.; Kouyaté, B. Artemisinin resistance on the Thai-Cambodian border. Lancet 2009, 374, 1419. [Google Scholar] [CrossRef]
- Rogers, W.O.; Sem, R.; Tero, T.; Chim, P.; Lim, P.; Muth, S.; Socheat, D.; Ariey, F.; Wongsrichanalai, C. Failure of artesunate-mefloquine combination therapy for uncomplicated Plasmodium falciparum malaria in southern Cambodia. Malar. J. 2009, 8, 10. [Google Scholar] [CrossRef]
- Yeung, S.; Socheat, D.; Moorthy, V.S.; Mills, A.J. Artemisinin resistance on the Thai-Cambodian border. Lancet 2009, 374, 1418–1419. [Google Scholar] [CrossRef]
- Duru, V.; Witkowski, B.; Ménard, D. Plasmodium falciparum Resistance to Artemisinin Derivatives and Piperaquine: A Major Challenge for Malaria Elimination in Cambodia. Am. J. Trop. Med. Hyg. 2016, 95, 1228–1238. [Google Scholar] [CrossRef]
- Population Services International and ACTwatch. Actwatch Outlet Survey Results: Cambodia 2009–2015; Population Services International and ACTwatch: Phnom Penh, Cambodia, 2016. [Google Scholar]
- Siv, S.; Roca-Feltrer, A.; Vinjamuri, S.B.; Bouth, D.M.; Lek, D.; Rashid, M.A.; By, N.P.; Popovici, J.; Huy, R.; Menard, D. Plasmodium vivax Malaria in Cambodia. Am. J. Trop. Med. Hyg. 2016, 95, 97–107. [Google Scholar] [CrossRef][Green Version]
- Office of the Inspector General (OIG). Investigation Report: Global Fund Grants to CambodiaNational Centre for Parasitology Entomology and Malaria Control (CNM); OIG: Geneva, Switzerland, 2017. Available online: https://www.theglobalfund.org/media/5433/oig_gf-oig-17-004_report_en.pdf?u=637278311890000000 (accessed on 5 May 2020).
- Titthara, M. Mondulkiri logging crackdowns stun illegal industry. Khmer Times, 31 July 2019. [Google Scholar]
- Akulayi, L.; Alum, A.; Andrada, A.; Archer, J.; Arogundade, E.D.; Auko, E.; Badru, A.R.; Bates, K.; Bouanchaud, P.; Bruce, M.; et al. Evidence on anti-malarial and diagnostic markets in Cambodia to guide malaria elimination strategies and policies. Malar. J. 2017, 16, 171. [Google Scholar]
- Abba, K.; Kirkham, A.J.; Olliaro, P.L.; Deeks, J.J.; Donegan, S.; Garner, P.; Takwoingi, Y. Rapid diagnostic tests for diagnosing uncomplicated non-falciparum or Plasmodium vivax malaria in endemic countries. Cochrane Database System. Rev. 2014, 2014, Cd011431. [Google Scholar] [CrossRef]
- Chu, C.S.; White, N.J. Management of relapsing Plasmodium vivax malaria. Expert Rev. Anti Infect. Ther. 2016, 14, 885–900. [Google Scholar] [CrossRef]
- Taylor, A.R.; Watson, J.A.; Chu, C.S.; Puaprasert, K.; Duanguppama, J.; Day, N.P.J.; Nosten, F.; Neafsey, D.E.; Buckee, C.O.; Imwong, M.; et al. Resolving the cause of recurrent Plasmodium vivax malaria probabilistically. Nat. Commun. 2019, 10, 5595. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Control and Elimination of Plasmodium Vivax Malaria: Technical Brief; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Lu, G.; Liu, Y.; Beiersmann, C.; Feng, Y.; Cao, J.; Müller, O. Challenges in and lessons learned during the implementation of the 1-3-7 malaria surveillance and response strategy in China: A qualitative study. Infect. Dis. Poverty 2016, 5, 94. [Google Scholar] [CrossRef] [PubMed]
- Kheang, S.T.; Sovannaroth, S.; Barat, L.M.; Dysoley, L.; Kapella, B.K.; Po, L.; Nguon, S.; Gimnig, J.; Slot, R.; Samphornarann, T.; et al. Malaria elimination using the 1-3-7 approach: Lessons from Sampov Loun, Cambodia. BMC Public Health 2020, 20, 544. [Google Scholar] [CrossRef] [PubMed]
- Bruce, M.C.; Donnelly, C.A.; Alpers, M.P.; Galinski, M.R.; Barnwell, J.W.; Walliker, D.; Day, K.P. Cross-Species Interactions Between Malaria Parasites in Humans. Science 2000, 287, 845. [Google Scholar] [CrossRef]
- Nagao, Y.; Kimura-Sato, M.; Chavalitshewinkoon-Petmitr, P.; Thongrungkiat, S.; Wilairatana, P.; Ishida, T.; Tan-Ariya, P.; de Souza, J.B.; Krudsood, S.; Looareesuwan, S. Suppression of Plasmodium falciparum by serum collected from a case of Plasmodium vivax infection. Malar. J. 2008, 7, 113. Available online: http://europepmc.org/abstract/MED/18582375; https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/18582375/pdf/?tool=EBI (accessed on 30 August 2020). [CrossRef] [PubMed][Green Version]
- Whitehorn, J.; Coltart, C.; Manser, D.; Doherty, T. A mixed malaria infection: Is Plasmodium vivax good for you? Trans. R. Soc. Trop. Med. Hyg. 2010, 104, 240–241. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Haghdoost, A.A.; Alexander, N. Systematic review and meta-analysis of the interaction between Plasmodium falciparum and Plasmodium vivax in humans. J. Vector Borne Dis. 2007, 44, 33–43. [Google Scholar]



| Year | Number of Health Centers | Number of Hospitals | Total Malaria Case Notifications | Population (a) |
|---|---|---|---|---|
| 2006 | 1087 | 96 | 1183 | 13,474,489 |
| 2007 | 1087 | 96 | 1183 | 13,676,693 |
| 2008 | 1087 | 96 | 1183 | 13,880,509 |
| 2009 | 1087 | 96 | 1183 | 14,090,208 |
| 2010 | 1087 | 96 | 1183 | 14,308,740 |
| 2011 | 1087 | 96 | 1183 | 14,537,886 |
| 2012 | 1087 | 96 | 1183 | 14,776,866 |
| 2013 | 1087 | 96 | 1183 | 15,022,692 |
| 2014 | 1138 | 104 | 1242 | 15,270,790 |
| 2015 | 1148 | 107 | 1255 | 15,517,635 |
| 2016 | 1168 | 111 | 1279 | 15,762,370 |
| 2017 | 1195 | 116 | 1311 | 16,005,373 |
| 2018 | 1213 | 121 | 1334 | 16,245,454 |
| 2019 | 1225 | 125 | 1350 | 16,489,135 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chhim, S.; Piola, P.; Housen, T.; Herbreteau, V.; Tol, B. Malaria in Cambodia: A Retrospective Analysis of a Changing Epidemiology 2006–2019. Int. J. Environ. Res. Public Health 2021, 18, 1960. https://doi.org/10.3390/ijerph18041960
Chhim S, Piola P, Housen T, Herbreteau V, Tol B. Malaria in Cambodia: A Retrospective Analysis of a Changing Epidemiology 2006–2019. International Journal of Environmental Research and Public Health. 2021; 18(4):1960. https://doi.org/10.3390/ijerph18041960
Chicago/Turabian StyleChhim, Srean, Patrice Piola, Tambri Housen, Vincent Herbreteau, and Bunkea Tol. 2021. "Malaria in Cambodia: A Retrospective Analysis of a Changing Epidemiology 2006–2019" International Journal of Environmental Research and Public Health 18, no. 4: 1960. https://doi.org/10.3390/ijerph18041960
APA StyleChhim, S., Piola, P., Housen, T., Herbreteau, V., & Tol, B. (2021). Malaria in Cambodia: A Retrospective Analysis of a Changing Epidemiology 2006–2019. International Journal of Environmental Research and Public Health, 18(4), 1960. https://doi.org/10.3390/ijerph18041960







