Objectively Measured Built Environments and Cardiovascular Diseases in Middle-Aged and Older Korean Adults
Abstract
1. Introduction
2. Methods
Study Participants
3. Measures
3.1. Cardiovascular Disease
3.2. Built Environment
3.3. Covariates
4. Statistical Analyses
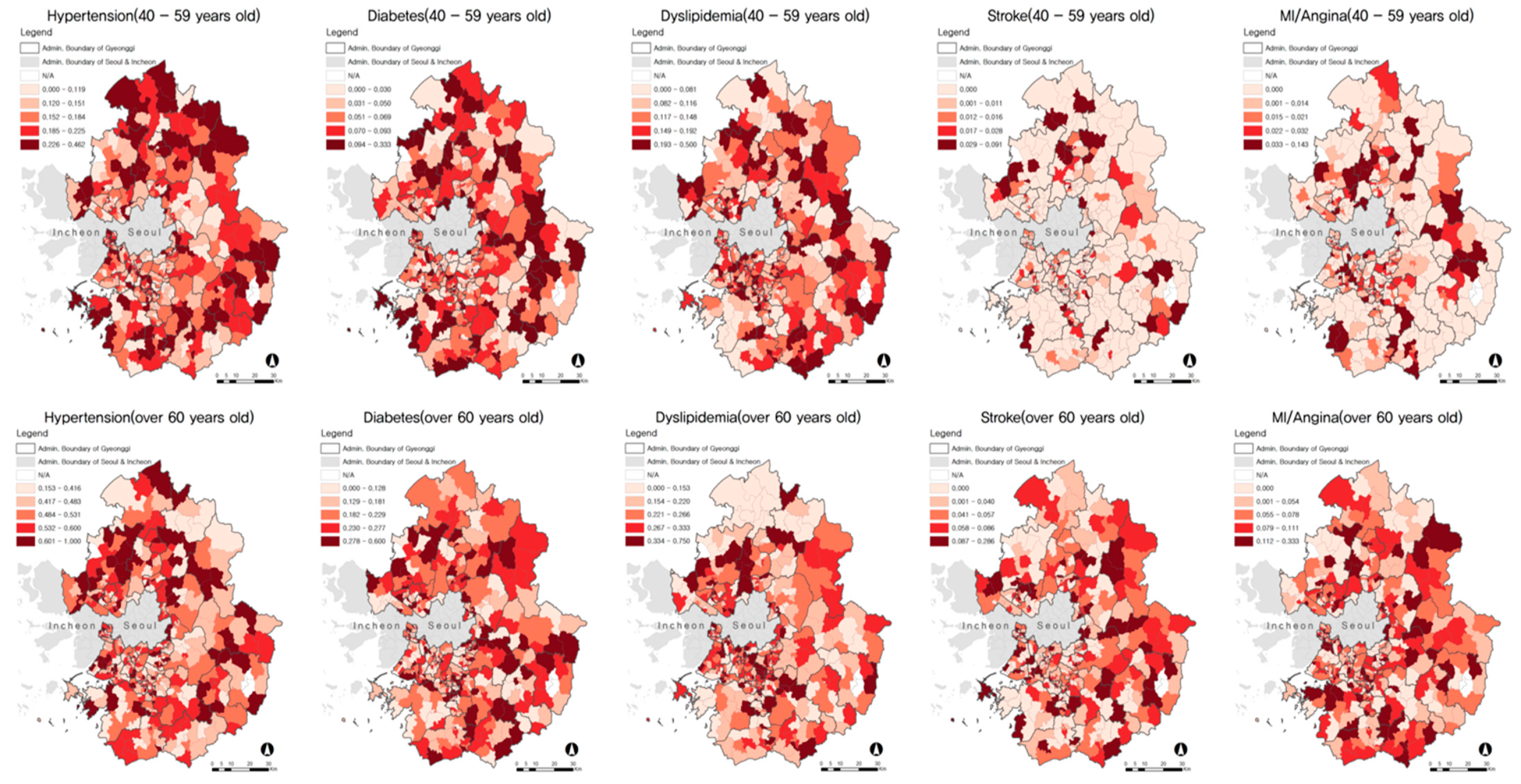
5. Results
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- GBD 2017 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1859–1922. [Google Scholar] [CrossRef]
- World Health Organination. Cardiovascular Diseases (CVDs). 2017. Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 13 August 2020).
- Statistics Korea. Cause of Death in 2018; Statistics Korea: Daejeon, Korea, 2018.
- Kim, Y.E.; Park, H.; Jo, M.W.; Oh, I.H.; Go, D.S.; Jung, J.; Yoon, S.J. Trends and patterns of burden of disease and injuries in Korea using disability-adjusted life years. J. Korean Med. Sci. 2019, 34, e75. [Google Scholar] [CrossRef]
- Diez Roux, A.V.; Mujahid, M.S.; Hirsch, J.A.; Moore, K.; Moore, L.V. The impact of neighborhoods on CV Risk. Glob. Heart 2016, 11, 353–363. [Google Scholar] [CrossRef]
- Clark, C.; Sbihi, H.; Tamburic, L.; Brauer, M.; Frank, L.D.; Davies, H.W. Association of Long-Term Exposure to Transportation Noise and Traffic-Related Air Pollution with the Incidence of Diabetes: A Prospective Cohort Study. Environ. Health Perspect. 2017, 125, 087025. [Google Scholar] [CrossRef] [PubMed]
- Leal, C.; Chaix, B. The influence of geographic life environments on cardiometabolic risk factors: A systematic review, a mehtodological assessment and a research agenda. Obes. Rev. 2011, 12, 217–230. [Google Scholar] [CrossRef] [PubMed]
- Malambo, P.; Kengne, A.P.; De Villiers, A.; Lambert, E.V.; Puoane, T. Built Environment, Selected Risk Factors and Major Cardiovascular Disease Outcomes: A Systematic Review. PLoS ONE 2016, 11, e0166846. [Google Scholar] [CrossRef]
- Chandrabose, M.; Chandrabose, M.; Rachele, J.N.; Gunn, L.; Kavanagh, A.; Owen, N.; Turrell, G.; Giles-Corti, B.; Sugiyama, T. Built environment and cardio-metabolic health: Systematic review and meta-analysis of longitudinal studies. Obes. Rev. 2019, 20, 41–54. [Google Scholar] [CrossRef]
- Loo, C.K.; Greiver, M.; Aliarzadeh, B.; Lewis, D. Association between neighbourhood walkability and metabolic risk factors influenced by physical activity: A cross-sectional study of adults in Toronto, Canada. BMJ Open 2017, 7, e013889. [Google Scholar] [CrossRef]
- Dendup, T.; Feng, X.; Clingan, S.; Astell-Burt, T. Environmental Risk Factors for Developing Type 2 Diabetes Mellitus: A Systematic Review. Int. J. Environ. Res. Public Health 2018, 15, 78. [Google Scholar] [CrossRef]
- Hamano, T.; Kawakami, N.; Li, X.; Sundquist, K. Neighborhood environment and stroke: A follow-up study in Sweden. PLoS ONE 2013, 8, e56680. [Google Scholar] [CrossRef]
- Chum, A.; O’Campo, P. Cross-sectional associations between residential environmental exposures and cardiovascular diseases. BMC Public Health 2015, 15, 438. [Google Scholar] [CrossRef]
- Kang, Y.W.; Ko, Y.S.; Kim, Y.J.; Sung, K.M.; Kim, H.J.; Choi, H.Y.; Sung, C.; Jeong, E. Korea Community Health Survey Data Profiles. Osong Public Health Res. Perspect. 2015, 6, 211–217. [Google Scholar] [CrossRef]
- Choe, S.; Lee, J.; Lee, J.; Kang, D.; Lee, J.; Shin, A. Validity of self-reported stroke and myocardial infarction in Korea: The Health Examinees study. J. Prev. Med. Public Health 2019, 52, 377–383. [Google Scholar] [CrossRef]
- Kehoe, R.; Wu, S.; Leske, M.; Chylack, L. Comparing self-reported and physician-reported medical history. Am. J. Epidemiol. 1994, 139, 813–818. [Google Scholar] [CrossRef]
- Frank, L.D.; Pivo, G. Relationship Between Land Use and Travel Behavior in the Puget Sound Region; Washington State Department of Transportation: Olympia, WA, USA, 1994.
- Lee, E.Y.; Lee, S.; Choi, B.Y.; Choi, J. Influence of Neighborhood Environment on Korean Adult Obesity Using a Bayesian Spatial Multilevel Model. Int. J. Environ. Res. Public Health 2019, 16, 3991. [Google Scholar] [CrossRef] [PubMed]
- Eastwood, J.G.; Jalaludin, B.B.; Kemp, L.A.; Phung, H.N.; Barnett, B.E.W. Immigrant maternal depression and social networks. A multilevel Bayesian spatial logistic regression in South Western Sydney, Australia. Spat. Spatio Temporal Epidemiol. 2013, 6, 49–58. [Google Scholar] [CrossRef]
- Wang, X.; Shao, C.; Yin, C.; Zhuge, C. Exploring the Influence of Built Environment on Car Ownership and Use with a Spatial Multilevel Model: A Case Study of Changchun, China. Int. J. Environ. Res. Public Health 2018, 15, 1868. [Google Scholar] [CrossRef]
- Besag, J. Spatial Interaction and the Statistical Analysis of Lattice Systems. J. R. Stat. Soc. 1974, 36, 192–236. [Google Scholar] [CrossRef]
- Rue, H.; Martino, S.; Lindgren, F.; Simpson, D.; Riebler, A.; Krainski, E. INLA: Functions Which Allow to Perform Full Bayesian Analysis of Latent Gaussian Models Using Integrated Nested Laplace Approximation. 2014. Available online: http://www.r-inla.org (accessed on 19 March 2020).
- Spiegelhalter, D.J.; Best, N.G.; Carlin, B.P.; Van Der Linde, A. Bayesian measures of model complexity and fit. J. R. Stat. Soc. 2002, 64, 583–639. [Google Scholar] [CrossRef]
- Dasgupta, P.; Cramb, S.M.; Aitken, J.F.; Turrell, G.; Baade, P.D. Comparing multilevel and Bayesian spatial random effects survival models to assess geographical inequalities in colorectal cancer survival: A case study. Int. J. Health Geogr. 2014, 13, 36. [Google Scholar] [CrossRef]
- Djurhuus, S.; Hansen, H.S.; Aadahl, M.; Glümer, C. The Association between Access to Public Transportation and Self-Reported Active Commuting. Int. J. Environ. Res. Public Health 2014, 11, 12632–12651. [Google Scholar] [CrossRef]
- Patterson, R.; Webb, E.; Hone, T.; Millett, C.; Laverty, A.A. Associations of public transportation use with cardiometabolic health: A systematic review and meta-analysis. Am. J. Epidemiol. 2019, 188, 785–795. [Google Scholar] [CrossRef]
- Patterson, R.; Panter, J.; Vamos, E.P.; Cummins, S.; Millett, C.; Laverty, A.A. Associations between commute mode and cardiovascular disease, cancer, and all-cause mortality, and cancer incidence, using linked Census data over 25 years in England and Wales: A cohort study. Lancet Planet. Health 2020, 4, e186–e194. [Google Scholar] [CrossRef]
- Paquet, C.; Coffee, N.T.; Haren, M.T.; Howard, N.J.; Adams, R.J.; Taylor, A.W.; Daniel, M. Food environment, walkability, and public open spaces are associated with incident development of cardio-metabolic risk factors in a biomedical cohort. Health Place 2014, 28, 173–176. [Google Scholar] [CrossRef]
- Muller-Riemenschneider, F.; Pereira, G.; Villanueva, K.; Christian, H.; Knuiman, M.; Giles-Corti, B.; Bull, F.C. Neighborhood walkability and cardiometabolic risk factors in Australian adults: An observational study. BMC Public Health 2013, 13, 755. [Google Scholar] [CrossRef]
- Mazidi, M.; Speakman, J.R. Association of fast-food and full-service restaurant densities with mortality from cardiovascular disease and stroke, and the prevalence of diabetes mellitus. J. Am. Heart Assoc. 2018, 7, e007651. [Google Scholar] [CrossRef]
- Briggs, A.C.; Black, A.W.; Lucas, F.L.; Siewers, A.E.; Fairfield, K.M. Association between the food and physical activity environment, obesity, and cardiovascular health across Maine counties. BMC Public Health 2019, 19, 374. [Google Scholar] [CrossRef] [PubMed]
- Sharkey, J.R.; Johnson, C.M.; Dean, W.R.; Horel, S.A. Association between proximity to and coverage of traditional fast-food restaurants and non-traditional fast-food outlets and fast-food consumption among rural adults. Int. J. Health Geogr. 2011, 10, 37. [Google Scholar] [CrossRef]
- Amuda, A.T.; Berkowitz, S.A. Diabetes and the built environment: Evidence and policies. Curr. Diabetes Rep. 2019, 19, 35. [Google Scholar] [CrossRef]
- Kärmeniemi, M.; Lankila, T.; Ikäheimo, T.; Puhakka, S.; Niemelä, M.; Jämsä, T.; Koivumaa-Honkanen, H.; Korpelainen, R. Residential relocation trajectories and neighborhood density, mixed land use and access networks as predictors of walking and bicycling in the Northern Finland Birth Cohort 1966. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 88. [Google Scholar] [CrossRef] [PubMed]
- Bonaccorsi, G.; Manzi, F.; Del Riccio, M.; Setola, N.; Naldi, E.; Milani, C.; Giorgetti, D.; Dellisanti, C.; Lorini, C. Impact of the Built Environment and the Neighborhood in Promoting the Physical Activity and the Healthy Aging in Older People: An Umbrella Review. Int. J. Environ. Res. Public Health 2020, 17, 6127. [Google Scholar] [CrossRef] [PubMed]
- Grant, M.; Braubach, M. Evidence review on the spatial determinants of health in urban settings: Land use pattern. In Annex 2 in Urban Planning, Environment and Health: From Evidence to Policy Action; Meeting repot, 22-97; WHO Regional Office for Europe: Copenhagen, Denmark, 2010. [Google Scholar]
- Wu, Y.; Prina, A.M.; Jones, A.; Barnes, L.E.; Mattews, F.E.; Brayne, C.; MRC CFAS. Land use mix and five-year mortality in later life: Results from the Cognitive Function and Ageing Study. Health Place 2016, 38, 54–60. [Google Scholar] [CrossRef] [PubMed]
| Variables | Definitions | Data Sources | Mean (±SD) | Min-Max |
|---|---|---|---|---|
| Population density | Number of people per sq. km of urbanized area | 2013 Population Census of Statistics Korea | 227.6 (±398.5) | 4.2–8067.8 |
| Density of physical activity facilities | Areas of physical activity facility per population | 2013 Public Physical Activity Facility Database of the Ministry of Culture, Sports, and Tourism | 23,145.9 (±55,203.8) | 0.0–513,250.7 |
| Density of public parks | Area of public park per population | 451,898.2 (±3008,972.2) | 0.0–76,659,160.8 | |
| Density of fast-food restaurants | Number of fast-food restaurant per urbanized area | 2013 Building Database of the Ministry of Land, Infrastructure and Transport | 0.0 (±0.2) | 0.0–3.5 |
| Proximity to public physical activity facilities | Average distance between the 100 × 100 m grid center of urbanized areas and public physical activity facilities | 2013 Public Physical Activity Facility Database of the Ministry of Culture, Sports, and Tourism | 1444.6 (±1216.1) | 205.3–9783.6 |
| Proximity to public parks | Average distance between the 100 × 100 m grid center of urbanized areas and public parks | 709.3 (± 991.6) | 39.9–6183.3 | |
| Proximity to public transit | Average distance between the 100 × 100 m grid center of urbanized areas and bus stops or subway stations | 2013 Transport Database of the Ministry of Land, Infrastructure and Transport | 282.2 (±206.4) | 85.1–1751.6 |
| Street connectivity | Number of three- or four-way intersections per urbanized area | 0.2 (±0.3) | 0.0–2.9 | |
| Residential density | Residential building floor areas per urbanized area | 2013 Building Database of the Ministry of Land, Infrastructure and Transport | 11,734.0 (±53,103.4) | 148.7–1,044,944.0 |
| Commercial density | Commercial building floor areas per urbanized area | 2750.3 (±7652.3) | 49.9–137,521.9 | |
| Industrial density | Industrial building floor areas per urbanized area | 2305.9 (±6849.8) | 49.7–128,049.5 | |
| Land-use mix | Residential, commercial, and industrial building floor areas per urbanized area | 0.7 (±0.2) | 0.0–1.0 |
| Variables | Total | Hypertension | Diabetes | Dyslipidemia | Stroke | MI/Angina |
|---|---|---|---|---|---|---|
| Total, n | 50,741 (100) | 14,438 (28.5) | 5725 (11.3) | 8644 (17.0) | 1006 (2.0) | 1649 (3.2) |
| Male sex, n (%) | 23,549 (46.4) | 6923 (47.9) | 3013 (52.6) | 3717 (43.0) | 540 (53.7) | 906 (54.9) |
| 40–59 years old, n (%) | 33,433 (65.9) | 5601 (38.8) | 2083 (36.4) | 4434 (51.3) | 186 (18.5) | 418 (25.3) |
| Education, ≤high school, n (%) | 35,632 (70.2) | 11,654 (80.7) | 4673 (81.6) | 6431 (74.4) | 861 (85.6) | 1344 (81.5) |
| Household income, <3 million won/month, n (%) | 23,482 (46.3) | 8672 (60.1) | 3580 (62.5) | 4649 (53.8) | 745 (74.1) | 1123 (68.1) |
| Job, non-manual job, n (%) | 10,674 (21.0) | 1721 (11.9) | 634 (11.1) | 1425 (16.5) | 45 (4.5) | 154 (9.3) |
| Job, manual job, n (%) | 20,264 (39.9) | 4977 (34.5) | 1865 (32.6) | 3043 (35.2) | 193 (19.2) | 459 (27.8) |
| Living alone (yes), n (%) | 4139 (8.2) | 1720 (11.9) | 670 (11.7) | 954 (11.0) | 133 (13.2) | 216 (13.1) |
| Residence period, <20 years, n (%) | 27,153 (53.5) | 6497 (45.0) | 2516 (43.9) | 4309 (49.8) | 464 (46.1) | 736 (44.8) |
| Former smokers, n (%) | 9693 (19.1) | 3417 (23.7) | 1448 (25.3) | 1874 (21.7) | 325 (32.3) | 505 (30.6) |
| Current smokers, n (%) | 10,509 (20.7) | 2414 (16.7) | 1123 (19.6) | 1479 (17.1) | 143 (14.2) | 292 (17.7) |
| Former drinkers, n (%) | 6790 (13.4) | 2392 (16.6) | 1152 (20.1) | 1347 (15.6) | 279 (27.7) | 379 (23.0) |
| Current drinkers, n (%) | 34,807 (68.6) | 8572 (59.4) | 3119 (54.5) | 5452 (63.1) | 442 (43.9) | 829 (50.3) |
| Sleeping duration, ≥7 h/day, n (%) | 24,906 (49.1) | 6974 (48.3) | 2897 (50.6) | 3938 (45.8) | 510 (50.7) | 783 (47.5) |
| Moderate or vigorous physical activity (yes), n (%) | 32,589 (64.2) | 9204 (63.7) | 3537 (61.8) | 5460 (63.2) | 590 (58.6) | 991 (60.1) |
| Low-sodium diet, n (%) | 13,583 (26.8) | 4012 (27.8) | 1670 (29.2) | 2398 (27.7) | 299 (29.7) | 469 (28.4) |
| High-sodium diet, n (%) | 12,054 (23.8) | 3890 (26.9) | 1488 (26.0) | 2209 (25.6) | 270 (26.8) | 485 (29.4) |
| Subjective health (good), n (%) | 40,841 (80.5) | 9535 (66.0) | 3108 (54.3) | 5926 (68.6) | 335 (33.3) | 783 (47.5) |
| Stress perception (yes), n (%) | 13,469 (26.5) | 3819 (26.5) | 1570 (27.4) | 2500 (28.9) | 314 (31.2) | 453 (27.5) |
| Depressive symptom (yes), n (%) | 3600 (7.1) | 1172 (8.1) | 549 (9.6) | 855 (9.9) | 132 (13.1) | 197 (11.9) |
| Obesity (≥25.0 kg/m2), n (%) | 13,917 (27.4) | 5563 (38.5) | 2197 (38.4) | 3420 (39.6) | 337 (33.5) | 565 (34.3) |
| Diabetes (yes), n (%) | 5725 (11.3) | 3479 (24.1) | 2095 (24.2) | 294 (29.2) | 516 (31.3) | |
| Hypertension (yes), n (%) | 14,438 (28.5) | 712 (4.9) | 972 (6.7) | |||
| Dyslipidemia (yes), n (%) | 8644 (17.0) | 331 (3.8) | 713 (8.2) |
| Built Environments | Hypertension a | Diabetes b | Dyslipidemia c | Stroke d | MI/angina e | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Univariable | Multivariable | Univariable | Multivariable | Univariable | Multivariable | Univariable | Multivariable | Univariable | Multivariable | |
| OR 95%CI | OR 95%CI | OR 95%CI | OR 95%CI | OR 95%CI | OR 95%CI | OR 95%CI | OR 95%CI | OR 95%CI | OR 95%CI | |
| Population density | ||||||||||
| T1 (lowest) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||
| T2 | 0.97 (0.90, 1.05) | 0.83 (0.74, 0.93) | 0.87 (0.71, 1.06) | 1.10 (1.01, 1.19) | 1.03 (0.89, 1.21) | 0.79 (0.55, 1.15) | 0.90 (0.71, 1.16) | |||
| T3 (highest) | 0.97 (0.90, 1.05) | 0.90 (0.80, 1.01) | 0.98 (0.77, 1.26) | 1.05 (0.96, 1.14) | 0.96 (0.80, 1.15) | 0.96 (0.67, 1.39) | 0.87 (0.68, 1.12) | |||
| Density of physical activity facilities | ||||||||||
| T1 (lowest) | 1 | 1 | 1 | 1 | 1 | |||||
| T2 | 0.94 (0.87, 1.01) | 0.91 (0.81, 1.03) | 1.00 (0.92, 1.09) | 0.97 (0.64, 1.44) | 1.12 (0.87, 1.43) | |||||
| T3 (highest) | 1.03 (0.96, 1.11) | 1.01 (0.90, 1.12) | 0.99 (0.91, 1.07) | 1.38 (0.98, 1.96) | 1.10 (0.86, 1.39) | |||||
| Density of public parks | ||||||||||
| T1 (lowest) | 1 | 1 | 1 | 1 | 1 | |||||
| T2 | 0.99 (0.92, 1.07) | 0.96 (0.86, 1.08) | 0.99 (0.91, 1.07) | 1.01 (0.71, 1.45) | 1.04 (0.82, 1.33) | |||||
| T3 (highest) | 0.99 (0.91, 1.06) | 1.04 (0.93, 1.17) | 1.00 (0.92, 1.09) | 0.89 (0.62, 1.30) | 1.05 (0.82, 1.35) | |||||
| Density of fast-food restaurants | ||||||||||
| T1 (lowest) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| T2 | 0.91 (0.84, 0.98) | 0.91 (0.84, 0.99) | 0.95 (0.84, 1.06) | 1.04 (0.95, 1.13) | 1.02 (0.90, 1.16) | 0.58 (0.41, 0.83) | 0.58 (0.41, 0.83) | 1.12 (0.87, 1.44) | ||
| T3 (highest) | 0.92 (0.85, 1.00) | 0.93 (0.86, 1.02) | 0.98 (0.87, 1.11) | 1.10 (1.01, 1.20) | 1.08 (0.94, 1.25) | 0.64 (0.44, 0.92) | 0.64 (0.44, 0.92) | 1.03 (0.79, 1.35) | ||
| Proximity to public physical activity facilities | ||||||||||
| T1 (nearest) | 1 | 1 | 1 | 1 | 1 | 1 | ||||
| T2 | 1.00 (0.93, 1.08) | 1.02 (0.92, 1.14) | 0.95 (0.88, 1.02) | 0.96 (0.86, 1.08) | 0.99 (0.70, 1.40) | 0.98 (0.78, 1.24) | ||||
| T3 (farthest) | 1.01 (0.93, 1.09) | 1.08 (0.96, 1.22) | 0.91 (0.84, 0.99) | 0.92 (0.78, 1.08) | 1.01 (0.70, 1.47) | 1.03 (0.80, 1.33) | ||||
| Proximity to public parks | ||||||||||
| T1 (nearest) | 1 | 1 | 1 | 1 | 1 | 1 | ||||
| T2 | 0.98 (0.92, 1.06) | 0.99 (0.88, 1.11) | 1.01 (0.89, 1.13) | 0.98 (0.91, 1.06) | 0.78 (0.54, 1.12) | 1.11 (0.88, 1.41) | ||||
| T3 (farthest) | 1.03 (0.95, 1.11) | 1.13 (1.00, 1.26) | 1.05 (0.85, 1.28) | 0.93 (0.86, 1.02) | 1.05 (0.74, 1.50) | 1.11 (0.86, 1.43) | ||||
| Proximity to public transit | ||||||||||
| T1 (nearest) | 1 | 1 | 1 | 1 | 1 | 1 | ||||
| T2 | 1.00 (0.94, 1.08) | 1.00 (0.90, 1.11) | 1.01 (0.94, 1.09) | 0.98 (0.70, 1.39) | 1.41 (1.11, 1.80) | 1.36 (1.07, 1.74) | ||||
| T3 (farthest) | 0.99 (0.92, 1.07) | 1.01 (0.90, 1.14) | 0.99 (0.91, 1.08) | 0.95 (0.65, 1.38) | 1.22 (0.94, 1.60) | 1.09 (0.81, 1.46) | ||||
| Street connectivity | ||||||||||
| T1 (lowest) | 1 | 1 | 1 | 1 | 1 | 1 | ||||
| T2 | 0.95 (0.88, 1.03) | 1.00 (0.89, 1.12) | 1.01 (0.93, 1.10) | 0.91 (0.64, 1.31) | 0.92 (0.72, 1.17) | 0.93 (0.72, 1.20) | ||||
| T3 (highest) | 0.95 (0.88, 1.02) | 0.94 (0.83, 1.06) | 1.06 (0.97, 1.15) | 0.83 (0.57, 1.21) | 0.75 (0.58, 0.97) | 0.77 (0.58, 1.02) | ||||
| Residential density | ||||||||||
| T1 (lowest) | 1 | 1 | 1 | 1 | 1 | 1 | ||||
| T2 | 0.98 (0.91, 1.05) | 0.86 (0.77, 0.97) | 0.98 (0.79, 122) | 1.05 (0.97, 1.14) | 0.73 (0.51, 1.05) | 0.93 (0.74, 1.18) | ||||
| T3 (highest) | 0.96 (0.89, 1.04) | 0.90 (0.80, 1.01) | 0.95 (0.73, 1.22) | 1.06 (0.97, 1.16) | 0.96 (0.66, 1.38) | 0.86 (0.66, 1.11) | ||||
| Commercial density | ||||||||||
| T1 (lowest) | 1 | 1 | 1 | 1 | 1 | |||||
| T2 | 0.97 (0.90, 1.04) | 0.91 (0.81, 1.02) | 1.06 (0.98, 1.15) | 0.79 (0.55, 1.12) | 1.01 (0.80, 1.29) | |||||
| T3 (highest) | 0.99 (0.92, 1.07) | 0.90 (0.80, 1.01) | 1.04 (0.95, 1.13) | 0.86 (0.60, 1.25) | 0.87 (0.67, 1.13) | |||||
| Industrial density | ||||||||||
| T1 (lowest) | 1 | 1 | 1 | 1 | 1 | |||||
| T2 | 0.99 (0.92, 1.07) | 0.90 (0.81, 1.01) | 1.07 (0.99, 1.16) | 1.02 (0.71, 1.46) | 0.95 (0.75, 1.20) | |||||
| T3 (highest) | 1.01 (0.93, 1.09) | 0.93 (0.83, 1.05) | 1.08 (0.99, 1.18) | 1.14 (0.79, 1.65) | 0.79 (0.61, 1.02) | |||||
| Land-use mix | ||||||||||
| T1 (lowest) | 1 | 1 | 1 | 1 | 1 | 1 | ||||
| T2 | 1.02 (0.95, 1.10) | 1.02 (0.95, 1.10) | 0.98 (0.88, 1.10) | 1.05 (0.97, 1.14) | 0.89 (0.61, 1.30) | 0.88 (0.69, 1.13) | ||||
| T3 (highest) | 1.08 (1.00, 1.16) | 1.07 (0.99, 1.16) | 1.11 (0.99, 1.25) | 1.01 (0.93, 1.10) | 1.15 (0.81, 1.65) | 1.07 (0.84, 1.36) | ||||
| Spatial fraction | 0.515 | 0.473 | 0.651 | 0.487 | 0.518 | |||||
| Built Environments | Hypertension a | Diabetes b | Dyslipidemia c | Stroke d | MI/angina e | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Univariable | Multivariable | Univariable | Multivariable | Univariable | Multivariable | Univariable | Multivariable | Univariable | Multivariable | |
| OR 95%CI | OR 95%CI | OR 95%CI | OR 95%CI | OR 95%CI | OR 95%CI | OR 95%CI | OR 95%CI | OR 95%CI | OR 95%CI | |
| Population density | ||||||||||
| T1 (lowest) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||
| T2 | 0.96 (0.89, 1.03) | 0.95 (0.86, 1.03) | 1.12 (1.02, 1.22) | 0.89 (0.73, 1.10) | 0.79 (0.66, 0.94) | 0.83 (0.67, 1.04) | 0.99 (0.86, 1.14) | |||
| T3 (highest) | 0.95 (0.88, 1.03) | 0.98 (0.89, 1.08) | 1.20 (1.10, 1.31) | 0.90 (0.70, 1.16) | 1.03 (0.87, 1.23) | 1.02 (0.78, 1.32) | 0.95 (0.82, 1.10) | |||
| Density of physical activity facilities | ||||||||||
| T1 (lowest) | 1 | 1 | 1 | 1 | 1 | |||||
| T2 | 0.96 (0.89, 1.03) | 1.01 (0.91, 1.11) | 1.01 (0.92, 1.10) | 1.19 (0.99, 1.44) | 0.97 (0.83, 1.13) | |||||
| T3 (highest) | 1.02 (0.96, 1.10) | 1.02 (0.93, 1.11) | 0.93 (0.85, 1.01) | 1.05 (0.88, 1.25) | 0.93 (0.81, 1.07) | |||||
| Density of public parks | ||||||||||
| T1 (lowest) | 1 | 1 | 1 | 1 | 1 | |||||
| T2 | 1.01 (0.93, 1.09) | 0.98 (0.89, 1.08) | 1.07 (0.98, 1.17) | 1.01 (0.84, 1.20) | 1.01 (0.88, 1.17) | |||||
| T3 (highest) | 1.00 (0.93, 1.08) | 1.00 (0.91, 1.09) | 1.05 (0.96, 1.15) | 0.99 (0.83, 1.18) | 1.03 (0.89, 1.19) | |||||
| Density of fast-food restaurants | ||||||||||
| T1 (lowest) | 1 | 1 | 1 | 1 | 1 | 1 | ||||
| T2 | 1.05 (0.97, 1.13) | 1.04 (0.95, 1.13) | 1.10 (1.01, 1.21) | 1.00 (0.88, 1.14) | 0.89 (0.75, 1.06) | 0.95 (0.82, 1.09) | ||||
| T3 (highest) | 0.96 (0.88, 1.04) | 1.01 (0.92, 1.11) | 1.20 (1.09, 1.32) | 1.05 (0.90, 1.23) | 0.86 (0.72, 1.04) | 1.05 (0.91, 1.22) | ||||
| Proximity to public physical activity facilities | ||||||||||
| T1 (nearest) | 1 | 1 | 1 | 1 | 1 | 1 | ||||
| T2 | 1.08 (1.00, 1.17) | 1.04 (0.94, 1.14) | 1.02 (0.94, 1.12) | 1.15 (1.01, 1.30) | 0.88 (0.73, 1.05) | 1.08 (0.93, 1.26) | ||||
| T3 (farthest) | 1.05 (0.97, 1.13) | 1.04 (0.94, 1.14) | 0.88 (0.80, 0.96) | 1.09 (0.90, 1.31) | 1.04 (0.87, 1.25) | 1.10 (0.95, 1.28) | ||||
| Proximity to public parks | ||||||||||
| T1 (nearest) | 1 | 1 | 1 | 1 | 1 | 1 | ||||
| T2 | 1.01 (0.93, 1.09) | 0.98 (0.89, 1.08) | 0.94 (0.86, 1.03) | 0.98 (0.86, 1.11) | 0.87 (0.72, 1.05) | 1.05 (0.90, 1.23) | ||||
| T3 (farthest) | 1.03 (0.95, 1.11) | 1.03 (0.94, 1.13) | 0.82 (0.75, 0.90) | 0.97 (0.78, 1.20) | 1.03 (0.87, 1.23) | 1.12 (0.97, 1.30) | ||||
| Proximity to public transit | ||||||||||
| T1 (nearest) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||
| T2 | 0.96 (0.89, 1.04) | 0.99 (0.90, 1.08) | 0.99 (0.90, 1.08) | 1.03 (0.89, 1.18) | 0.83 (0.69, 0.99) | 0.85 (0.68, 1.06) | 1.00 (0.86, 1.16) | |||
| T3 (farthest) | 1.03 (0.96, 1.12) | 0.99 (0.90, 1.09) | 0.87 (0.79, 0.95) | 0.95 (0.79, 1.14) | 0.96 (0.81, 1.15) | 0.91 (0.70, 1.18) | 1.06 (0.91, 1.23) | |||
| Street connectivity | 1 | |||||||||
| T1 (lowest) | 1 | 1 | 1 | 1 | 1 | 1 | ||||
| T2 | 1.04 (0.97, 1.12) | 0.97 (0.89, 1.06) | 1.12 (1.03, 1.22) | 1.08 (0.94, 1.23) | 0.81 (0.68, 0.96) | 0.83 (0.68, 1.01) | 0.91 (0.79, 1.05) | |||
| T3 (highest) | 1.01 (0.94, 1.10) | 0.96 (0.88, 1.06) | 1.20 (1.10, 1.32) | 1.11 (0.95, 1.30) | 0.90 (0.75, 1.07) | 0.93 (0.74, 1.16) | 0.98 (0.85, 1.14) | |||
| Residential density | ||||||||||
| T1 (lowest) | 1 | 1 | 1 | 1 | 1 | 1 | ||||
| T2 | 0.97 (0.91, 1.05) | 0.96 (0.88, 1.05) | 1.13 (1.04, 1.24) | 1.19 (0.88, 1.60) | 0.87 (0.74, 1.04) | 0.98 (0.85, 1.12) | ||||
| T3 (highest) | 0.93 (0.86, 1.00) | 0.96 (0.89, 1.08) | 1.24 (1.13, 1.36) | 1.33 (0.94, 1.87) | 0.99 (0.82, 1.18) | 0.92 (0.79, 1.07) | ||||
| Commercial density | ||||||||||
| T1 (lowest) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||
| T2 | 0.96 (0.89, 1.03) | 0.97 (0.89, 1.05) | 0.95 (0.87, 1.04) | 1.15 (1.06, 1.26) | 0.82 (0.63, 1.08) | 0.92 (0.78, 1.09) | 0.99 (0.86, 1.14) | |||
| T3 (highest) | 0.92 (0.85, 1.00) | 0.94 (0.86, 1.03) | 1.02 (0.93, 1.12) | 1.18 (1.08, 1.29) | 0.81 (0.60, 1.10) | 0.94 (0.79, 1.13) | 0.94 (0.81, 1.10) | |||
| Industrial density | ||||||||||
| T1 (lowest) | 1 | 1 | 1 | 1 | 1 | 1 | ||||
| T2 | 0.99 (0.92, 1.07) | 0.99 (0.91, 1.08) | 1.17 (1.07, 1.27) | 1.05 (0.87, 1.27) | 0.85 (0.71, 1.01) | 0.99 (0.86, 1.13) | ||||
| T3 (highest) | 0.93 (0.86, 1.01) | 0.95 (0.87, 1.05) | 1.21 (1.10, 1.32) | 1.05 (0.83, 1.31) | 1.06 (0.88, 1.26) | 0.96 (0.83, 1.12) | ||||
| Land-use mix | ||||||||||
| T1 (lowest) | 1 | 1 | 1 | 1 | 1 | 1 | ||||
| T2 | 0.98 (0.91, 1.06) | 1.11 (1.01, 1.23) | 1.11 (1.01, 1.23) | 0.96 (0.88, 1.05) | 1.07 (0.89, 1.29) | 1.05 (0.91, 1.23) | ||||
| T3 (highest) | 1.03 (0.96, 1.12) | 1.13 (1.03, 1.24) | 1.13 (1.02, 1.24) | 0.92 (0.84, 1.01) | 1.14 (0.95, 1.36) | 1.02 (0.88, 1.18) | ||||
| Spatial fraction | 0.706 | 0.473 | 0.938 | 0.491 | 0.488 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, E.Y.; Choi, J.; Lee, S.; Choi, B.Y. Objectively Measured Built Environments and Cardiovascular Diseases in Middle-Aged and Older Korean Adults. Int. J. Environ. Res. Public Health 2021, 18, 1861. https://doi.org/10.3390/ijerph18041861
Lee EY, Choi J, Lee S, Choi BY. Objectively Measured Built Environments and Cardiovascular Diseases in Middle-Aged and Older Korean Adults. International Journal of Environmental Research and Public Health. 2021; 18(4):1861. https://doi.org/10.3390/ijerph18041861
Chicago/Turabian StyleLee, Eun Young, Jungsoon Choi, Sugie Lee, and Bo Youl Choi. 2021. "Objectively Measured Built Environments and Cardiovascular Diseases in Middle-Aged and Older Korean Adults" International Journal of Environmental Research and Public Health 18, no. 4: 1861. https://doi.org/10.3390/ijerph18041861
APA StyleLee, E. Y., Choi, J., Lee, S., & Choi, B. Y. (2021). Objectively Measured Built Environments and Cardiovascular Diseases in Middle-Aged and Older Korean Adults. International Journal of Environmental Research and Public Health, 18(4), 1861. https://doi.org/10.3390/ijerph18041861






