The Psychological and Physical Effects of Forests on Human Health: A Systematic Review of Systematic Reviews and Meta-Analyses
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature Search
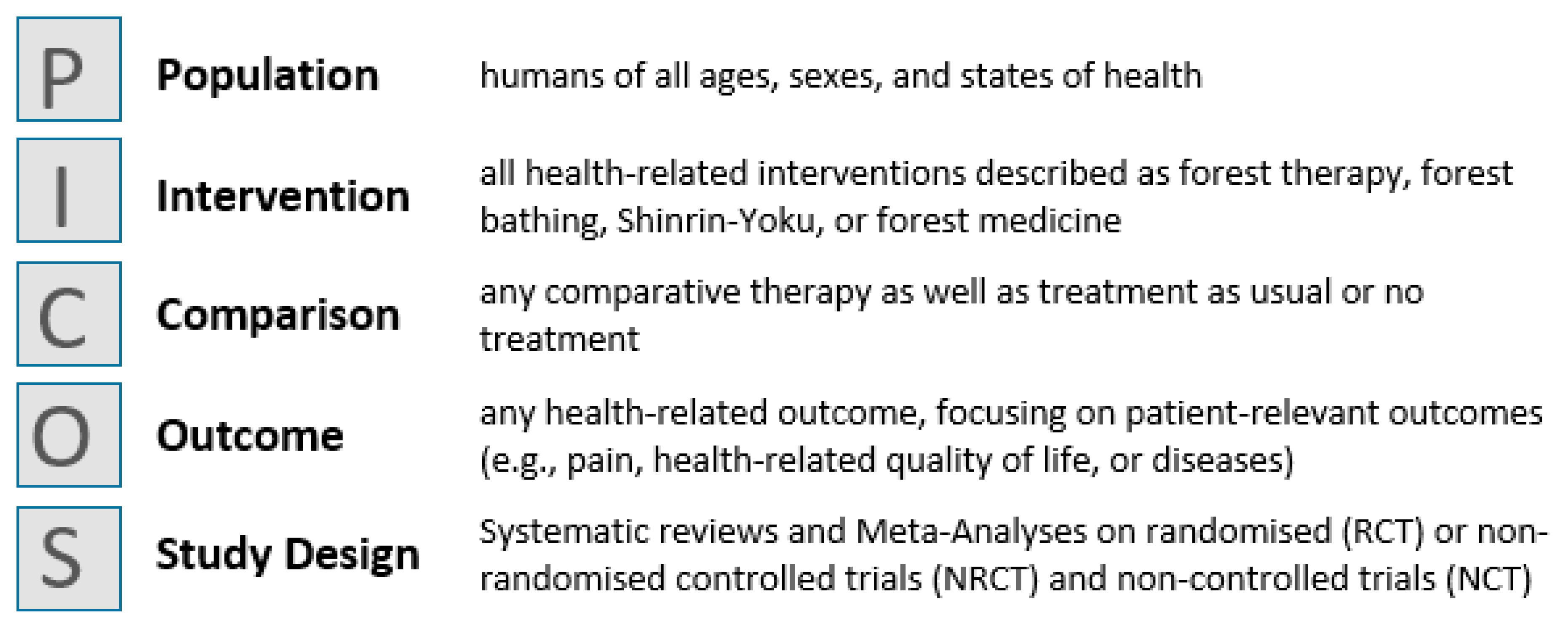
2.2. Inclusion and Exclusion Criteria
2.3. Deviation from the Study Protocol
2.4. Selection of Studies
2.5. Quality Assessment
2.6. Data Extraction
3. Results
3.1. Search Results
3.2. Characteristics of Included Studies
3.3. Methodological Quality of Included Reviews
3.4. Summary of Main Findings
3.4.1. Cardiovascular System
3.4.2. Immune and/or Inflammatory Parameters
3.4.3. Metabolic Parameters
3.4.4. Atopic Dermatitis
3.4.5. Mental Health
Stress
Anxiety and Depression
Negative Emotions
Quality of Life/Well-Being
Mental Health—Conclusion
3.4.6. Sociality
4. Discussion
4.1. Key Findings from the Review—Summary of Evidence
4.2. Latest Work on the Topic
4.3. Mechanisms of Action
4.4. Strengths and Limitations
4.4.1. Strengths
4.4.2. Limitations at the Primary Study Level
4.4.3. Limitations at the Review Level
4.4.4. Limitations at the Overview Level
4.5. Implications for Practice and Future Research
4.5.1. Interventions
4.5.2. Selection of Control Groups for the Investigation of the Effects of Forest-Based Interventions
4.5.3. Recommendations for Practice and Future Research
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A. Search Strings
| No. | Search Strings | Hits |
|---|---|---|
| 1 | “forest therap*”.ab,ti. | 30 |
| 2 | “forest bath*”.ab,ti. | 27 |
| 3 | forest medicine.ab,ti. | 4 |
| 4 | Shinrin-yoku.ab,ti. | 18 |
| 5 | forest healing.ab,ti. | 1 |
| 6 | “review*”.ab,ti. | 1,732,382 |
| 7 | “systematic*”.ab,ti. | 360,076 |
| 8 | “overview*”.ab,ti. | 133,772 |
| 9 | “Meta-Analys*”.ab,ti. | 133,384 |
| 10 | 1 or 2 or 3 or 4 or 5 | 63 |
| 11 | 6 or 7 or 8 or 9 | 2,052,748 |
| 12 | 10 and 11 | 12 |
| No. | Search Strings | Hits |
|---|---|---|
| 1 | “forest therap*”.ab,ti. | 39 |
| 2 | “forest bath*”.ab,ti. | 45 |
| 3 | forest medicine.ab,ti. | 4 |
| 4 | Shinrin-yoku.ab,ti. | 21 |
| 5 | forest healing.ab,ti. | 4 |
| 6 | “review*”.ab,ti. | 2,679,607 |
| 7 | “systematic*”.ab,ti. | 565,832 |
| 8 | “overview*”.ab,ti. | 198,810 |
| 9 | “Meta-Analys*”.ab,ti. | 217,515 |
| 10 | 1 or 2 or 3 or 4 or 5 | 90 |
| 11 | 6 or 7 or 8 or 9 | 3,173,197 |
| 12 | 10 and 11 | 22 |
| No. | Search Strings | Hits |
|---|---|---|
| # 12 | #11AND#10 | 64 |
| # 11 | #9OR#8OR#7OR#6 | 3,453,809 |
| # 10 | #5OR#4OR#3OR#2OR#1 | 470 |
| # 9 | TOPIC: (Meta-Analys*) | 196,262 |
| # 8 | TOPIC: (overview*) | 331,638 |
| # 7 | TOPIC: (systematic*) | 889,313 |
| # 6 | TOPIC: (review*) | 2,509,712 |
| # 5 | TOPIC: (forest healing) | 287 |
| # 4 | TOPIC: (“Shinrin-yoku”) | 112 |
| # 3 | TOPIC: (“forest medicine”) | 3 |
| # 2 | TOPIC: (“forest bath*”) | 70 |
| # 1 | TOPIC: (“forest therap*”) | 68 |
| No. | Search Strings | Hits |
|---|---|---|
| #1 | (review*):ti,ab,kw OR (systematic*):ti,ab,kw OR (overview*):ti,ab,kw OR (Meta-Analys*):ti,ab,kw (Word variations have been searched) | 91,743 |
| #2 | (forest NEXT therap*):ti,ab,kw OR (forest NEXT bath*):ti,ab,kw OR (Forest NEXT medicine):ti,ab,kw OR (Shinrin-Yoku):ti,ab,kw OR (forest NEXT healing):ti,ab,kw (Word variations have been searched) | 27 |
| #3 | #1 AND #2 | 0 |
| No. | Search Strings | Hits |
|---|---|---|
| S3 | (S1 AND S2) | 2 |
| S2 | review* OR systematic* OR overview* OR Meta-Analys* | 776,703 |
| S1 | “forest therap*” OR “forest bath*” OR “forest medicine” OR “shinrin-yoku” OR “forest healing” | 12 |
| No. | Search Strings | Hits |
|---|---|---|
| S3 | (S1 AND S2) | 2 |
| S2 | review* OR systematic* OR overview* OR Meta-Analys* | 776,703 |
| S1 | “forest therap*” OR “forest bath*” OR “forest medicine” OR “shinrin-yoku” OR “forest healing” | 12 |
| No. | Search Strings | Hits |
|---|---|---|
| 1 | (forest therap* OR forest bath* OR forest medicine OR Shinrin-Yoku OR forest healing) AND (review* OR systematic* OR overview* OR Meta-Analys*) | 21 |
| No. | Search Strings | Hits |
|---|---|---|
| 1 | (TITLE-ABS-KEY(“forest therap*” OR “forest bath*” OR “forest medicine” OR “shinrin-yoku” OR “forest healing”)AND TITLE-ABS-KEY(review* OR systematic* OR overview* OR meta-analys*)) | 31 |
| No. | Search Strings | Hits |
|---|---|---|
| 1 | review AND [“forest therapy” OR “forest bathing” OR “forest medicine” OR “shinrin-yoku” OR “forest healing” -doi] | 1090 |
| No. | Search Strings | Hits |
|---|---|---|
| 1 | (“forest therap*” or “forest bath*” or “forest medicine” or “shinrin-Yoku” or “forest healing”) AND (review* or systematic* or overview* or “Meta-Analys*”) | 8 |
Appendix B
| Reference | Reason for Exclusion |
|---|---|
| Ambrose-Oji, B. Mindfulness Practice in Woods and Forests: An Evidence Review. Research Report for The Mersey Forest, Forest Research. Alice Holt Lodge Farnham, Surrey; 2013. Available from: https://infta.net/files/references/Mindfulness%20and%20Woods%20Evidence%20Review%20%202013.pdf [Access Date: 6 October 2020]. | No systematic review |
| Cho, K. S.; Lim, Y. R.; Lee, K.; Lee, J.; Lee, J. H.; Lee, I. S. Terpenes from Forests and Human Health. Toxicol. Res. 2017;33(2):97–106. | No systematic review |
| Cho, Y.-M.; Kim, D.-J.; Lee, K. H.; Lee, H. E.; Lee, Y. J. A Study on Effect of Forest Related Programs based on the Meta-Analysis. Journal of the Korean Institute of Forest Recreation, 2015. 19(1): 1–13. | No systematic review |
| Karjalainen, E., Sarjala, T. & Raitio, H. Promoting human health through forests: overview and major challenges. Environ Health Prev Med. 2010;15:1–8. | No systematic review |
| Li, Q. Effect of forest bathing trips on human immune function. Environ Health Prev Med. 2010;15:9–17. | No systematic review |
| Li, Q. Effect of forest bathing (shinrin-yoku) on human health: A review of the literature. Santé Publique. 2019;31:135–143. | No systematic review |
| Li, Q.; Kawada, T. Possibility of Clinical Applications of Forest Medicine. Japanese Journal of Hygiene. 2014;69(2):117–121. | No systematic review |
| Meyer, K.; Burger-Arndt, R. How forests foster human health—Present state of research-based knowledge (in the field of Forests and Human Health). International Forestry Review. 2014;16(4):421–446. | No systematic review |
| Meyer-Schulz, K.; Burger-Arndt, R. Une revue de la littérature scientifique Reviewing the psychological and physical health effects of forests. Santé Publique. 2019; 31:115–134. | No systematic review |
| Miyazaki, Y.; Ikei, H.; Song, C. Forest medicine research in Japan. Japanese Journal of Hygiene. 2014; 69(2):122–135. | No systematic review |
| Payne, M.; Delphinus, E. The most natural of natural therapies: A review of the health benefits derived from Shinrin-Yoku (Forest Bathing). The International Journal of Health, Wellness, and Society. 2019;9:19–30. | No systematic review |
| Shin, W. S.; Yeoun, P. S.; Yoo, R. W.; Shin, C. S. Forest experience and psychological health benefits: The state of the art and future prospect in Korea. Environ Health Prev Med. 2010; 15:38–47. | No systematic review |
| Zhang, Z. Y.; Wang, P.; Gao, Y.; Ye, B. Current Development Status of Forest Therapy in China. Healthcare (Basel). 2020;8(1):61. | No systematic review |
| Corazon, S. S.; Sidenius, U.; Poulsen, D. V.; Gramkow, M. C.; Stigsdotter, U. K. Psycho-Physiological Stress Recovery in Outdoor Nature-Based Interventions: A Systematic Review of the Past Eight Years of Research. Int. J. Environ. Res. Public Health. 2019; 16, 1711. | Non-predominant forest (≥80% of the studies) |
| Haluza, D.; Schonbauer, R.; Cervinka, R. Green Perspectives for Public Health: A Narrative Review on the Physiological Effects of Experiencing Outdoor Nature. Int. J. Environ. Res. Public Health. 2014;11,:5445–5461. | Non-predominant forest (≥80% of the studies) |
| Hansen, M. M.; Jones, R.; Tocchini, K. Shinrin-Yoku (Forest Bathing) and Nature Therapy: A State-of-the-Art Review. Int. J. Environ. Res. Public Health. 2017;14 (8):851. | Non-predominant forest (≥80% of the studies) |
| Hossain, M., Sultana, A., Ma, P., Fan, Q., Sharma, R., Purohit, N., & Sharmin, D. F. (2020, January 8). Effects of natural environment on mental health: an umbrella review of systematic reviews and meta-analyses. Available from: https://psyarxiv.com/4r3mh/ [Access Date: 6 October 2020]. | Non-predominant forest (≥80% of the studies) |
| Kamioka H, Tsutani K, Mutoh Y, Honda T, Shiozawa N, Okada S, Park SJ, Kitayuguchi J, Kamada M, Okuizumi H, Handa S. A systematic review of randomized controlled trials on curative and health enhancement effects of forest therapy. Psychol Res Behav Manag. 2012;5:85–95. | Non-predominant forest (≥80% of the studies) |
| Poulsen, D. V. (2015). How war veterans with post-traumatic stress disorder experience nature-based therapy in a forest therapy garden. Københavns Universitet: Department of Geosciences and Natural Resource Management, Faculty of Science, University of Copenhagen. Available from: https://ign.ku.dk/phd-forsvar/2015/phd-defence-dorthe-varning-poulsen/ [Access Date: 6 October 2020]. | Non-predominant forest (≥80% of the studies) |
| Kim T, Song B, Cho KS, Lee IS. Therapeutic Potential of Volatile Terpenes and Terpenoids from Forests for Inflammatory Diseases. Int J Mol Sci. 2020;21(6):2187. | Non-predominant forest (≥80% of the studies) |
| Mathias, S., Daigle, P., Dancause, K. N., & Gadais, T. (2019, December 5). Forest bathing: a narrative review of the effects on health for outdoor and environmental education use in Canada. Available from: https://doi.org/10.31236/osf.io/j6mq3 [Access Date: 6 October 2020]. | Non-predominant forest (≥80% of the studies) |
| McMahan, E. A.; Estes, D. The effect of contact with natural environments on positive and negative affect: A meta-analysis. The Journal of Positive Psychology. 2015;10(6): 507–519. | Non-predominant forest (≥80% of the studies) |
| Meredith Genevive R., Rakow Donald A., Eldermire Erin R. B., Madsen Cecelia G., Shelley Steven P., Sachs Naomi A. Minimum Time Dose in Nature to Positively Impact the Mental Health of College-Aged Students, and How to Measure It: A Scoping Review. 2020;10:2942 Available from: https://doi.org/10.3389/fpsyg.2019.02942 [Access Date: 6 October 2020]. | Non-predominant forest (≥80% of the studies) |
| Muranen, Anni-Tuulia; Alihanka, Karoliina. Green Exercise in Supportin the Mental Health of Cardiac patients. Thesis. 2019. Available from: https://www.theseus.fi/bitstream/handle/10024/265719/Muranen_Anni-Tuulia%2C%20Alihanka_Karoliina.pdf?sequence=2&isAllowed=y [Access Date: 6 October 2020]. | Non-predominant forest (≥80% of the studies) |
| Mygind L, Kjeldsted E, Hartmeyer R, et al.. Effects of Public Green Space on Acute Psychophysiological Stress Response: A Systematic Review and Meta-Analysis of the Experimental and Quasi-Experimental Evidence. Environment and Behavior. 2019. | Non-predominant forest (≥80% of the studies) |
| Mygind L, Kjeldsted E, Hartmeyer RD, Mygind E, Bølling M, Bentsen P. Immersive Nature-Experiences as Health Promotion Interventions for Healthy, Vulnerable, and Sick Populations? A Systematic Review and Appraisal of Controlled Studies. Front Psychol. 2019;10:943. | Non-predominant forest (≥80% of the studies) |
| Nilsson K, Bentsen P, Grahn P, Mygind L. De quelles preuves scientifiques disposons-nous concernant les effets des forêts et des arbres sur la santé et le bien-être humains ? [What is the scientific evidence with regard to the effects of forests, trees on human health and well-being?]. Sante Publique. 2019;S1(HS):219–240. French. | Non-predominant forest (≥80% of the studies) |
| Roberts H, van Lissa C, Hagedoorn P, Kellar I, Helbich M. The effect of short-term exposure to the natural environment on depressive mood: A systematic review and meta-analysis. Environ Res. 2019;177:108606. | Non-predominant forest (≥80% of the studies) |
| Roth, A.-S. (2011). Naturen—En resurs för stressåterhämtning: En systematisk litteraturstudie (Dissertation). Available from: http://urn.kb.se/resolve?urn=urn:nbn:se:his:diva-5342 [Access Date: 6 October 2020]. | Non-predominant forest (≥80% of the studies) |
| Sun, Seung-Ho; Lee, Seon-Goo. Systemic review on forest healing journals. Korean J. Oriental Physiology & Pathology 2010; 24(4): 566–570. | Non-predominant forest (≥80% of the studies) |
| Twohig-Bennett, Caoimhe; Jones, Andy. The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. Environmental Research. 2018, 166:628–637. | Non-predominant forest (≥80% of the studies) |
| Vibholm, A. P.; Christensen, J. R.; Pallesen, H. Nature-based rehabilitation for adults with acquired brain injury: a scoping review. International Journal of Environmental Health Research, 30:6, 661–676. | Non-predominant forest (≥80% of the studies) |
Appendix C. Deviation from the AMSTAR-2 Guidance Document
- Many items in the AMSTAR-2 can be answered with “Partial Yes” or “Yes”. Several criteria must usually be met for a “Partial Yes”. The criteria for “Partial Yes” and several additional criteria must be met for a “Yes”. This is usually formulated as “For Yes should also have...” or “For Yes must also have...”. We have interpreted and applied these rules as follows: for a formulation with “should”, at least one of the following criteria had to be met for a “Yes”, and all the criteria listed had to be met for a formulation with “must”.
- Item 4: “Did the review authors use a comprehensive literature search strategy?” Three criteria must be met for a “Partial Yes” to this question. One of them is “justified publication restrictions (e.g., language)”. Since the restrictions for the literature search are usually described, but only very rarely justified, we did not take this criterion into account in the evaluation.
- Item 7: “Did the review authors provide a list of excluded studies and justify the exclusions?” For a “Yes” to this question, a list of the excluded studies must be available, and the exclusion of every potentially relevant study from the review must be justified. The evaluation was modified as follows: for a “Yes”, it was sufficient if the number of excluded studies and information about how many studies had been excluded for what reasons in the paper (e.g., in PRISMA Flow Chart) were listed.
References
- United Nations. Department of Economic and Social Affairs (UN/DESA): World Urbanization Prospects: The 2018 Revision. Available online: https://population.un.org/wup/Publications/Files/WUP2018-KeyFacts.pdf (accessed on 27 November 2020).
- Corazon, S.S.; Sidenius, U.; Poulsen, D.V.; Gramkow, M.C.; Stigsdotter, U.K. Psycho-Physiological Stress Recovery in Outdoor Nature-Based Interventions: A Systematic Review of the Past Eight Years of Research. Int. J. Environ. Res. Public Health 2019, 16, 1711. [Google Scholar] [CrossRef]
- Hansen, M.M.; Jones, R.; Tocchini, K. Shinrin-yoku (forest bathing) and nature therapy: A state of the art review. Int. J. Environ. Res. Public Health 2017, 14, 851. [Google Scholar] [CrossRef]
- Twohig-Bennett, C.; Jones, A. The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. Environ. Res. 2018, 166, 628–637. [Google Scholar] [CrossRef] [PubMed]
- Bowler, D.E.; Buyung-Ali, L.M.; Knight, T.M.; Pullin, A.S. A systematic review of evidence for the added benefits to health of exposure to natural environments. BMC Public Health 2010, 10. [Google Scholar] [CrossRef]
- Li, Q. Effect of forest bathing trips on human immune function. Environ. Health Prev. Med. 2010, 15, 9. [Google Scholar] [CrossRef] [PubMed]
- Markov, S.; Steckenbauer, G.C.; Pillmayer, M.; Herntrei, M. Austria: The Forest as a Touristic Landscape. In International Handbook of Forest Therapy; Kotte, D., Li, Q., Shin, W.S., Michalsen, A., Eds.; Cambridge Scholars Publishing: Newcastle, UK, 2019; pp. 337–355. [Google Scholar]
- Li, Q. Forest Medicine—Public Health in the 21st Century; Nova Science Publisher: New York, NY, USA, 2012. [Google Scholar]
- Kotte, D.; Li, Q.; Shin, W.S.; Michalsen, A. International Handbook of Forest Therapy; Cambridge Scholars Publishing: Newcastle, UK, 2019. [Google Scholar]
- Li, Q. What is Forest Medicine? In Forest Medicine; Nova Science Publisher: New York, NY, USA, 2013. [Google Scholar]
- Schuh, A.; Immich, G. Waldtherapie—Das Potential des Waldes für Ihre Gesundheit; Springer-Verlag: Berlin/Heidelberg, Germany, 2019. [Google Scholar]
- Kaiserbaeder Usedom. Cure and Healing Forests. 2002. Available online: https://www.kur-und-heilwald.de/?lang=en (accessed on 12 December 2002).
- Karim, A.; Khalil, R.; Schmitt, M. Wald reloaded—Die Neuentdeckung des Waldes aus gesundheitspsychologischer Sicht. Z. Komplementärmedizin 2020, 2, 24–30. [Google Scholar] [CrossRef]
- Vukin, M.; Isailović, G. A Cure and Healing Foest of Goč Mountain—A New Approach to Health Tourism in Serbia. Available online: https://de.calameo.com/read/00586528821d0b12eaa9b (accessed on 22 November 2020).
- Berman, M.G.; Jonides, J.; Kaplan, S. The cognitive benefits of interacting with nature. Psychol. Sci. 2008, 19, 1207–1212. [Google Scholar] [CrossRef]
- Peen, J.; Schoevers, R.A.; Beekman, A.T.; Dekker, J. The current status of urban-rural differences in psychiatric disorders. Acta Psychiatr. Scand. 2010, 121, 84–93. [Google Scholar] [CrossRef]
- Van Den Berg, A.E.; Maas, J.; Verheij, R.A.; Groenewegen, P.P. Green space as a buffer between stressful life events and health. Soc. Sci. Med. 2010, 70, 1203–1210. [Google Scholar] [CrossRef]
- Müllner, M. Epidemiologie der Zivilisationskrankheiten. In Bewegung als Therapie: Gezielte Schritte zum Wohlbefinden; Zwick, H., Ed.; Springer Verlag: Wien, Austria, 2007; pp. 13–31. [Google Scholar]
- Oh, B.; Lee, K.J.; Zaslawski, C.; Yeung, A.; Rosenthal, D.; Larkey, L.; Back, M. Health and well-being benefits of spending time in forests: Systematic review. Environ. Health Prev. Med. 2017, 22. [Google Scholar] [CrossRef] [PubMed]
- Vibholm, A.P.; Christensen, J.R.; Pallesen, H. Nature-based rehabilitation for adults with acquired brain injury: A scoping review. Int. J. Environ. Health Res. 2020, 30, 661–676. [Google Scholar] [CrossRef]
- Meyer, K.; Burger-Arndt, R. How forests foster human health—Present state of research-based knowledge (in the field of Forests and Human Health). Int. For. Rev. 2014, 16, 421–446. [Google Scholar] [CrossRef]
- Meyer-Schulz, K.; Burger-Arndt, R. Reviewing the Psychological and Physical Health Effects of Forests. Santé Publique 2019, 31 (Suppl. S1), 115–134. [Google Scholar] [CrossRef]
- Stier-Jarmer, M.; Throner, V.; Kirschneck, M.; Frisch, D.; Schuh, A. Psychological and Physical Effects of Forests on Human Health—A Systematic Review of Systematic Reviews and Meta-Analyses; 2020; Available online: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020190649 (accessed on 11 February 2021).
- Stern, C.; Jordan, Z.; McArthur, A. Developing the Review Question and Inclusion Criteria. Am. J. Nurs. 2014, 114, 53–56. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed]
- Cochrane Deutschland Stiftung, Institut für Evidenz in der Medizin, Institut für Medizinische Biometrie und Statistik, Freiburg, Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften, Institut für Medizinisches Wissensmanagement, Ärztliches Zentrum für Qualität in der Medizin. Manual Systematische Recherche für Evidenzsynthesen und Leitlinien. 2019. Available online: https://freidok.uni-freiburg.de/data/149324 (accessed on 20 November 2020). [CrossRef]
- Antonelli, M.; Barbieri, G.; Donelli, D. Effects of forest bathing (shinrin-yoku) on levels of cortisol as a stress biomarker: A systematic review and meta-analysis. Int. J. Biometeorol. 2019, 63, 1117–1134. [Google Scholar] [CrossRef] [PubMed]
- Ideno, Y.; Hayashi, K.; Abe, Y.; Ueda, K.; Iso, H.; Noda, M.; Lee, J.S.; Suzuki, S. Blood pressure-lowering effect of Shinrin-yoku (Forest bathing): A systematic review and meta-analysis. BMC Complement. Altern. Med. 2017, 17, 409. [Google Scholar] [CrossRef] [PubMed]
- Kotera, Y.; Richardson, M.; Sheffield, D. Effects of Shinrin-Yoku (Forest Bathing) and Nature Therapy on Mental Health: A Systematic Review and Meta-Analysis. Int. J. Ment. Health Addict. 2020. [Google Scholar] [CrossRef]
- Farrow, M.R.; Washburn, K.A. Review of Field Experiments on the Effect of Forest Bathing on Anxiety and Heart Rate Variability. Glob. Adv. Health Med. 2019, 8. [Google Scholar] [CrossRef]
- Lee, I.; Bang, K.S.; Kim, S.; Choi, H.; Lee, B.; Song, M. Effect of Forest Program on Atopic Dermatitis in Children—A Systematic Review. J. Korean Inst. For. Recreat. 2016, 20, 1–13. [Google Scholar] [CrossRef][Green Version]
- Lee, I.; Choi, H.; Bang, K.S.; Kim, S.; Song, M.; Lee, B. Effects of forest therapy on depressive symptoms among adults: A systematic review. Int. J. Environ. Res. Public Health 2017, 14, 321. [Google Scholar] [CrossRef]
- Putra, R.R.F.A.; Veridianti, D.D.; Nathalia, E.; Brilliant, D.; Rosellinny, G.; Suarez, C.G.; Sumarpo, A. Immunostimulant Effect from Phytoncide of Forest Bathing to Prevent the Development of Cancer. Adv. Sci. Lett. 2018, 24, 6653–6659. [Google Scholar] [CrossRef]
- Song, M.K.; Bang, K.-S. A systematic review of forest therapy programs for elementary school students. Child Health Nurs. Res. 2017, 23, 300–311. [Google Scholar] [CrossRef]
- Chae, Y.R.; Kim, J.H.; Kang, H. Literature Review of Forest Healing Therapy on Korean Adults. J. Korean Biol. Nurs. Sci. 2018, 20, 122–131. [Google Scholar] [CrossRef]
- Wen, Y.; Yan, Q.; Pan, Y.; Gu, X.; Liu, Y. Medical empirical research on forest bathing (Shinrin-yoku): A systematic review. Environ. Health Prev. Med. 2019, 24, 70. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Pieper, D.; Antoine, S.-L.; Mathes, T.; Neugebauer, E.A.M.; Eikermann, M. Systematic review finds overlapping reviews were not mentioned in every other overview. J. Clin. Epidemiol. 2014, 67, 368–375. [Google Scholar] [CrossRef] [PubMed]
- Yau, K.K.-Y.; Loke, A.Y. Effects of forest bathing on pre-hypertensive and hypertensive adults: A review of the literature. Environ. Health Prev. Med. 2020, 25, 23. [Google Scholar] [CrossRef] [PubMed]
- Grilli, G.; Sacchelli, S. Health Benefits Derived from Forest: A Review. Int. J. Environ. Res. Public Health 2020, 17, 6125. [Google Scholar] [CrossRef] [PubMed]
- Hansen, M.M.; Jones, R. The Interrelationship of Shinrin-Yoku and Spirituality: A Scoping Review. J. Altern. Complement. Med. 2020, 26, 1093–1104. [Google Scholar] [CrossRef] [PubMed]
- Rajoo, K.S.; Karamb, D.S.; Abdullaha, M.Z. The physiological and psychosocial effects of forest therapy: A systematic review. Urban For. Urban Green. 2020, 54, 126744. [Google Scholar] [CrossRef]
- Kang, M.-J.; Myung, S.-K. Effects of Forest-Based Interventions on Mental Health; A Meta-Analysis of Randomized Controlled Trials. 2020. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020202489 (accessed on 11 February 2021).
- Ioannou, S.; Patterson, L.; Whittaker, P. The Health Benefits of Forest Therapy: An Umbrella Review. 2019. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42019136586 (accessed on 11 February 2021).
- Kemper, H. Waldbaden: Der Wald Wirkt Entschleunigend; ZEIT Wissen: Hamburg, Germany, 2018; p. 3. [Google Scholar]
- Markert, R. Alternative Medizin. Waldtherapie—Gesund durch Natur? 2019. Available online: https://www.zdf.de/nachrichten/heute/alternative-medizin-heilung-durch-waldtherapie-100.html (accessed on 28 October 2020).
- Abe, T.; Hisama, M.; Tanimoto, S.; Shibayama, H.; Mihara, Y.; Nomura, M. Antioxidant effects and antimicrobial activites of phytoncide. Biocontrol. Sci. 2008, 13, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Morimoto, K.; Kobayashi, M.; Inagaki, H.; Katsumata, M.; Hirata, Y.; Hirata, K.; Suzuki, H.; Li, Y.J.; Wakayama, Y.; et al. Visiting a forest, but not a city, increases human natural killer activity and expression of anti-cancer proteins. Int. J. Immunopathol. Pharmacol. 2008, 21, 117–127. [Google Scholar] [CrossRef]
- Šimpraga, M.; Ghimire, R.P.; Van Der Straeten, D.; Blande, J.D.; Kasurinen, A.; Sorvari, J.; Holopainen, T.; Adriaenssens, S.; Holopainen, J.K.; Kivimaenpaa, M. Unravelling the functions of biogenic volatiles in boreal and temperate forest ecosystems. Eur. J. For. Res. 2019, 138, 763–787. [Google Scholar] [CrossRef]
- Antonelli, M.; Donelli, D.; Barbieri, G.; Valussi, M.; Maggini, V.; Firenzuoli, F. Forest Volatile Organic Compounds and Their Effects on Human Health: A State-of-the-Art Review. Int. J. Environ. Res. Public Health 2020, 17, 6506. [Google Scholar] [CrossRef]
- Park, B.J. Forest Welfare Policy in South Korea. Poster Präsentation am 2. In Proceedings of the Internationalen Kongress „Gesundheitspotential Wald“, Krems, Austria, 6–7 November 2018. [Google Scholar]
- Clifford, A. Your Guide to Forest Bathing; Conari Press: Newburyport, MA, USA, 2018. [Google Scholar]
- Imai, M. An introduction to the Forest Therapy Society of Japan, Forest Therapy and Forest Therapist. In Forest Medicine; Li, Q., Ed.; Nova Science Publishers: Hauppauge, NY, USA, 2012. [Google Scholar]
- Kang, B.; Kim, T.; Kim, M.J.; Lee, K.H.; Choi, S.; Lee, D.H.; Kim, H.R.; Jun, B.; Park, S.Y.; Lee, S.J.; et al. Relief of chronic posterior neck pain depending on the type of forest therapy: Comparison of the therapeutic effect of forest bathing alone versus forest bathing with exercise. Ann. Rehabil. Med. 2015, 39, 957–963. [Google Scholar] [CrossRef] [PubMed]


| First Author (Date); Country | Search Details | Objective; | Assessment of Risk of Bias and/or Study Quality: | Number (Type) of Studies Included; | Study Population; | Interventions: Intervention Group (IG) and Control Group (CG); |
|---|---|---|---|---|---|---|
| Meta-Analysis: Yes/No | Total Number (Range) | |||||
| Country of Study Implementation | Intervention Duration | |||||
| Lee (2016); | 6 DBs, from inception to Nov. 2015; | Effects of forest programs on atopic dermatitis; | RoBANS | N = 5 (5 NCT); | Children, adolescents with atopic dermatitis; | IG: forest experience, forest trip; forest camp; physical therapy; forest-camp swimming; forest activities, disease education |
| SB: confounder and selection of participants—high, comparability—predominantly low | ||||||
| South Korea [31] | GL: unpublished dissertations considered | |||||
| PB: high | ||||||
| 184 (12–64) | ||||||
| CG: n. a.; | ||||||
| No | DB: high | Korea | Durations: 1–3 days (3–4 nights) | |||
| LR: n. a. | ||||||
| AB: predominantly low | ||||||
| RB: predominantly low | ||||||
| Ideno (2017); | 4 DBs, from inception to May 2016; | Effects of the forest environment on blood pressure; | RoB | N = 20 (2 RCT, 15 NRCT cross-over, 3 NRCT); | Healthy adults, adults with hypertension; | IG: walking in/sitting in and viewing forest area |
| SB: high (with 50%) | CG: walking in/sitting in and viewing in non-forest environment, such as city areas, sitting in a room, measuring blood pressure in daily life; | |||||
| GL: was searched | PB: high | |||||
| Japan | DB: high | Japan (n = 17) | 732 (6–268) | |||
| [28] | LR: English and Japanese language only | AB: low | Korea (n = 2) | |||
| Yes | RB: low | China (n = 1) | ||||
| Durations: 15 min to 2 h; 1 × 3 days, 1 × 7 days | ||||||
| Lee (2017); South Korea [32] | 7 DBs, from inception to July 2016; GL: n. a. LR: English and Korean language only | Effects of forest therapy on depressive symptoms; No | SIGN checklist 18 studies low and 10 acceptable quality | N = 28 (17 RCT, 11 NRCT); Korea (n = 17) Japan (n = 7) China (n = 3) Great Britain (n = 1) | Healthy adults, adults with health conditions: alcoholism, COPD, chronic stroke, hypertension, cancer, mental-health conditions, psychiatric out- and inpatients, major depression disorder; 1090 (11–92) | IG: forest therapy: walking as a key component in the forest, other therapeutic activities (experiencing the forest through all five senses: seeing, hearing, touching, smelling, tasting), viewing the forest/meditation, Qi-Qong, aromatherapy, herbal tea therapy, handicrafts with natural items CG: normal daily routine; conducted same activities in the room/city area/urban forest/hospital/stay in a hotel; regular diet and exercise program in the forest; one-day trip for urban walking; Durations: 12 min to 3 days for 1 day to 12 weeks |
| Oh (2017); Australia [19] | 5 DBs, from inception to Dec. 2016; GL: was searched LR: English language only | Effects of forest bathing on health; No | RoB SB: high (with 66%) PB: high DB: high (with 30%) AB: unclear or low RB: low | N = 6 (6 RCT); China (n = 3) Korea (n = 2) Sweden (n = 1) | Healthy adults, adults with health conditions: chronic alcoholic, high blood pressure, exhaustion disorders, COPD; 323 (18–99) | IG: forest-healing camp (interaction with nature; mountain climbing und trekking; self-introspection, including mediation and counselling); mountain-forest walks; forest-rehabilitation group (with subsequent cognitive behavioural rehabilitation for all participants) CG: normal daily routine; walking/hiking/interventions in urban area/city; waiting list group with cognitive behavioural rehabilitation; Durations: 1 h to 2× week for 11 weeks (22 visits each with 4 h) |
| Song (2017); South Korea [34] | 6 DBs, from inception to Dec. 2016; GL: n. a. LR: English and Korean language only | Effects of forest therapy programs for elementary-school students; No | RoBANS SB: confounder high (with 50%); comparability—predominantly low; selection of participants—low PB: high DB: high AB: predominantly low RB: predominantly low | N = 17 (two of them without forest intervention; 10 NRCT, 7 NCT); South Korea | Healthy children; 1491 (16–308) | IG: walks; forest athletic meetings; getting along with neighbours; forest-ecology exploration; making something with natural materials; psychotherapy; climate therapy; exercise therapy; diet therapy; water therapy CG: normal daily routine; traditional learning methods, reduced forest program at school; Durations: 5 h to 8 months |
| Chae (2018); South Korea [35] | 5 DBs, from inception to March 2018; GL: n. a. LR: English and Korean language only | Effects of forest healing therapy; No | n. a. | N = 25 (5 of them without forest intervention; 13 NRCT, 12 NCT; Korea | Nurses, healthcare worker, healthy adults, adults with health conditions: alcoholism, Hwa-Byung, depression, mild cognitive impairment, cancer; 1141 (10–221) | IG: nature-experiencing physical activities; forest (healing) program; meditation; hiking CG: interventions conducted indoors; other settings (ambulatory treatment); comparator duration of intervention; no intervention; Durations: 1 day to 12 weeks |
| Putra (2018); Indonesia[33] | 2 DBs, from 2007 to July 2017; GL: n. a. LR: English language only | Effects of phytoncides when forest bathing; No | n. a. | N = 10 (n. a.); Japan | Healthy adults; 126 (12–17) | IG: walking, sitting and watching in the forest; physical activity; stay in the hotel for 3 days and 3 nights and giving aromatic volatile substances (phytoncides produced by vaporising Chamaecyparis obtusa stem oil) with a humidifier in the hotel room for 3 nights CG: city trips: walking, sitting and watching; normal physical activity; Durations: 4.5 h to 2–3 days |
| Antonelli, (2019); Italy[27] | 6 DBs, from inception to Feb. 2019;GL: was searched LR: English, French, Spanish, and Italian only | Effects of forest bathing on levels of salivary or serum cortisol as stress biomarkers; Yes | NIH; RoB SB: low or unclear PB: high DB: low AB: low or unclear RB: low | N = 22 (3 RCT, 8 RCT cross-over, 5 NRCT, 3 NRCT cross-over,3 NCT);Japan (n = 12) South Korea (n = 4)China (n = 2) Germany (n = 1) Iceland (n = 1), Finland (n = 1) Spain (n = 1) | Healthy children and adults, adults with health conditions: COPD, high risk of stress/burnout, major depressive disorder, hypertension, post-menopausal women; 2165 (9–348) | IG: forest bathing: spending time in a forest, walking, resting, watching, and deep breathing in forest; psychological program; cognitive behaviour therapy CG: walking and/or watching an urban area/-park; spending time on beach; no intervention; indoor; psychological program; comparator age; Durations: 15 min to half a day |
| Farrow (2019); USA [30] | 2 DBs, from 2008 to 2018; GL: n. a. LR: n. a. | Effects of forest bathing on reducing anxiety and heart rate variability (activation of parasympathetic nervous system); No | n. a. | N = 10 (2 RCT, 3 RCT cross-over, 1 NRCT cross-over, 1 NRCT, 3 NCT); Japan (n = 8) Taiwan (n = 1) Finland (n = 1) | Healthy adults, hypertensive adults; 1667 (9–625) | IG: walking, sitting in forest environment, viewing a forest landscape CG: walking, sitting in urban environment, viewing an urban landscape; Durations: 15 mint half a day (4–4.5h); 15 min on 2 days in a row |
| Wen (2019); China [36] | 3 DBs from 2015 to April 2019; GL: was searched LR: English language only | Effects of forest environment exposure on human health; No | Downs and Black Checklist 16 studies high- and 12 studies low-quality; RoB relatively high overall | N = 28 (7 RCT, 10 RCT cross-over, 1 NRCT cross-over,3 NRCT, 7 NCT); Japan (n = 13) China (n = 6) South Korea (n = 5) Taiwan (n = 3) Poland (n = 1) | Healthy children, adults, adults with health conditions: high blood pressure, COPD, chronic stroke, chronic heart failure; 924 (6–128) | IG: exposed to forest (urban forest park), walking, meditation, “five sense experience”, activities and rest, watching the scenery—forest environment, handicrafts, sitting quietly in a dense/sparse forest environment; taking a tree-measuring course; enjoying private time CG: exposed to urban environment/walking and meditating; watching the scenery—urban environment; sitting quietly in a dense/sparse forest environment; indoor classes; Durations: 15 min to 5 days |
| Kotera (2020); United Kingdom [29] | 4 DBs from inception to Oct. 2019; GL: was searched LR: English language only | Effects of Shinrin-Yoku (forest bathing) and nature therapy on mental health; Yes | 1. NOS 2. Quality Assessment Table of Randomised Controlled Trials RCTs high to medium; RoB in 6 studies low and in 2 studies high | N = 20 (11 RCT, 2 NRCT, 7 NCT); Japan (n = 10) Korea (n = 4) Taiwan (n = 2) Poland (n = 2) China (n = 1) Serbia (n = 1) | Healthy adults, adults with health conditons: metabolic syndrome, chronic stroke, psychiatric disorders (depression), chronic diseases, chronic pain, alcoholism; 2257 (12–585) | IG: Walk in forest and meditation CG: Crossover (forest vs. city); groups with different forest types (birch, maple, and oak); Durations: 15 min to 9 days |
| Author | AMSTAR-2 Rating | Study Population | Indications | Outcomes | Results |
|---|---|---|---|---|---|
| Ideno, Y. et al. (2017) [28] | moderate | Healthy adults, adults with health conditions: hypertension | Cardiovascular System | Blood pressure: systolic (SBP)/diastolic (DBP) | SBP (20 studies): ↓↓ in forest group DBP (17 studies): ↓↓ in forest group |
| Healthy adults, adults with health conditions: hypertension | Cardiovascular system | Heart Rate and Pulse Rate | HR (5 studies)/PR (8 studies): ↓↓ in forest group | ||
| Kotera, Y. et al. (2020) [29] | moderate | Healthy adults, adults with health conditions: metabolic syndrome, chronic stroke, psychiatric disorders (depressions), chronic diseases, chronic pains, alcoholism | Mental health | Depression: POMS; BDI; HDR; DASS; EQVAS; MMS Anxiety: POMS; STAI; AAQ; DASS; EQVAS | Depression (20 studies): ↓↓ forest vs. city Anxiety: (5 studies) ↓ after forest intervention, (16 studies) ↓↓ after forest intervention |
| Healthy adults, adults with health conditions: metabolic syndrome, depressive tendencies, chronic diseases | Mental health | Anger: POMS | Anger (14 studies): ↓↓ after forest intervention | ||
| Lee, I. et al. (2016) [31] | low | Children/adolescents with atopic dermatitis | Atopic dermatitis | Atopic Dermatitis: SCORAD Index (subjective/objective) Child Anxiety-Test Immunology blood test: TARC, MDC,Serum immune cytokine levels | Atopic Dermatitis SCORAD Index (subjective/objective) (all studies): all ↓↓ Child-Anxiety-Test (1 study): ↓ Immunology blood test (1 study): WBC + CD8+ T cells ↑↑; Haemoglobin+ N cells ↓↓, all other ; TARC (1 study): ↓; MDC (1 study): ↓↓; serum immune cytokine levels (1 study): IL-5 ↓↓; IL-2, IL-4, IFN-y |
| Lee, I. et al. (2017) [32] | low | Healthy adults, adults with health conditions: alcoholism, COPD, chronic stroke, hypertension, cancer, mental disorders, psychiatric inpatients or outpatients, severe depression | Mental health | Physical activity: HPLP II Health promotion behaviour: HPLP II Quality of life: EQ-VAS; GHQ/QL-12, SF-36, WHOQOL-BREF, POMS | Physical activity (1 study): ## Health promotion behaviour (1 study): ## Quality of life (5 studies): ## POMS (15 studies): 14 studies ##, 1 study # |
| Healthy adults, adults with health conditions: alcoholism, COPD, chronic stroke, hypertension, cancer, mental disorders, psychiatric inpatients or outpatients, severe depression | Mental health | Depression: BDI; MADRS; HDR-D17; Zung Self-Rating Depression Scale Anxiety: STAI | Depression (15 studies): 14 ##, 1 study # Anxiety (6 studies): 5 studies ##, 1 study # | ||
| Healthy adults, adults with health conditions: alcoholism, COPD, chronic stroke, hypertension, cancer, mental disorders, psychiatric inpatients or outpatients, severe depression | Mental health | Stress: Stress response, inventory measuring self-reported stress and arousal Hwa-Byung-Syndrome: The Instrument of Oriental Medical Evaluation for Hwa-Byung | Stress:(2 studies): ## Hwa-Byung-Syndrome (1 study): ## | ||
| Healthy adults, adults with health conditions: alcoholism, COPD, chronic stroke, hypertension, cancer, mental disorders, psychiatric inpatients or outpatients, severe depression | Mental health | Anger: STAXI Emotion: SD -Method | Anger (2 studies): Emotion (4 studies): 3 studies ##, 1 study # | ||
| Healthy adults, adults with health conditions: alcoholism, COPD, chronic stroke, hypertension, cancer, mental disorders, psychiatric inpatients or outpatients, severe depression | Mental health | Self-esteem: Self-esteem, The Rosenberg Self-Esteem Scale Spirituality: SHI, The Spiritual Assessment Scale Resilience: Self-regulation Resilience Pos./Neg. Effects: PANAS, ROS | Self-esteem (3 studies): ## Spirituality (1 study): ## Resilience (1 study): ## Pos./Neg. Effects (1 study): ## | ||
| Healthy adults, adults with health conditions: alcoholism, COPD, chronic stroke, hypertension, cancer, mental disorders, psychiatric inpatients or outpatients, severe depression | Mental health | NK cells Blood pressure Salivary amylase (Saliva/Serum) Cortisol Pulse rate or Heart rate (PR/HR) HRV/(In LF/HF) Cytokine: IL-6 Enzyme-bonded Immunoassay | NK cells (1 study): ## Blood pressure (6 studies): 3 studies ##, 1 study #, 1 study n.a. Salivary amylase (2 studies): 1 study ##, 1 study # (Saliva/Serum) Cortisol (4 studies): ## PR Or HR (7 studies): 5 studies ##, 1 study #, 1 study n.a. HRV (In LF/HF) (8 studies): 5 studies ##, 2 studies #, 1 study n.a. Cytokine (1 study) IL-6: ## Enzyme-bonded Immunoassay (1 study): ## | ||
| Oh, B. et al. (2017) [19] | low | Adults with health conditions: hypertension | Cardiovascular system | Blood pressure Heart function: Cardio Ankle Vascular Index (CAVI) | Blood pressure (2 studies): ↓↓ in forest group Heart function (1 study): ↑↑ in forest group |
| Healthy adults, adults with health conditions: COPD | Immune and/or inflammatory indices | Immune function: Expression von Perforin (NK cells, NK-similar cells, CD8 + T cells) and granzyme B Inflammation: Proinflammatory cytokines (IFN-y, IL-6, IL-8, IL-1ß); C-reactive protein (CRP) Inflammation/Tumor: Tumor necrosis factor α | Immune function (1 study): ↓↓ Perforin and granzyme B in forest groupInflammation: Proinflammatory cytokines (3 studies): ↓↓ in forest group; CRP (1 study): ↓ in forest group Inflammation/Tumor (2 studies): 1 study ↓↓ in forest group, 1 study | ||
| Healthy adults | Immune and/or inflammatory indices | Antioxidants: Biomarkers for malondialdehyde (MDA) and superoxide dismutase (SOD) | Antioxidants (1 study): ↓↓ MDA in forest group, SOD | ||
| Older women | Lung function | Lung function: FEV1 (in 1 s) and FEV6 (in 6 s) | Lung function: FEV (in 1s) and FEV (in 6s) (1 study): ↑↑ in forest group | ||
| Adults with chronic health conditions: alcoholism, fatigue syndrome | Mental health | Anxiety and Depression: BDI HADS | Anxiety and Depression: BDI (1 study): ↓↓ forest group HADS (1 study): both groups ↓↓, between groups | ||
| Adults with health conditions: fatigue syndrome, COPD | Mental health | Stress: PSQserum cortisol | Stress: PSQ (1 study): ↓ in forest group cortisol (1 study): ↓↓ in forest group | ||
| Healthy adults, adults with health conditions: hypertension, COPD | Mental health | Mood: POMS | Mood (3 studies): all ↑↑ in forest group | ||
| Song, M. K. and Bang, K. -S. (2017) [34] | low | Healthy children | Mental health | Depression: CDI; Scale for Mental Health Measurement Anxiety: STAI-C; Scale for Mental Health measurement | Depression (4 studies): 2 studies ##, 2 studies # Anxiety (3 studies): 2 studies ##, 1 studies # |
| Healthy children | Mental health | Stress: Stress Recognition Inventory for School-aged Children; saliva cortisol level; AMHI | Stress (3 studies): 1 study stress recognition ##; 1 study salivary cortisol ##; 1 study AMHI stress level # | ||
| Healthy children | Mental health | Self-esteem: Self-esteem scale/self-esteem | Self-esteem (3 studies): ## | ||
| Healthy children | Mental health | Negative Emotions: Draw a Story (DAS); scale for emotional and social development test Anger: Novaco Anger Scale Impulsiveness: Scale for mental-health measurement Aggression: Scale for aggression; scale for mental health measurement Attack: Scale for mental health measurement | Negative Emotions (2 studies): ## Anger (1 study): ## Impulsiveness (2 studies): 1 study ##; 1 study # Aggression (2 studies): ## Attack (1 study): # | ||
| Healthy children | Mental health | Mental health: AMHI; scale for mental-health measurement; scale for psychological, social, moral, and physical level | Mental health (4 studies): 2 studies #; 1 study mental health quotient ##; 1 study psychological level ## | ||
| Healthy children | Mental health | Subject Well-being: Subject Well-being Scale | Subject Well-being (1 study): # | ||
| Healthy children | Mental health | Psychological skills: Emotional Intelligence Test; AMHI; Ergo-Resilience Scale | Psychological skills (3 studies): 1 study Ergo-Resilience Scale: interpersonal relationship and curiosity ##.; 1 study emotional intelligence ##; 1 study possibility of problem behaviour (chronic fatigue) and psychological resources ## | ||
| Healthy children | Mental health | Physical skills: Scale for psychological, social, moral, and physical level | Physical skills (1 study): ## | ||
| Healthy children | Sociality | Sociality: Korean Personality Inventory: sociality Social competence: Social Competence Scale; scale for emotional and social development test; scale for psychological, social, moral, and physical level | Sociality (2 studies): ## Social competence (3 studies): ## | ||
| Healthy children | Sociality | School violence attitude: Scale for school violence attitude School adjustment: Scale for school adjustment; multiple life satisfaction scaleLife respect: Scale for life respect | School violence attitude (1 study): ## School adjustment: (2 studies): both in parts ## Life respect (1 study): ## | ||
| Antonelli, M. et al. (2019) [27] | low | Healthy children, adults with health conditions: COPD, high risk for stress/burnout, severe depression, hypertension, postmenopausal women | Mental health | Stress: salivary/serum cortisol | Stress (22 studies): 20 studies ↓↓ forest vs. non-forest within group: 13 studies ↓↓, 1 study ↑↑, 5 n.a. between groups: 13 studies ↓↓ forest vs. non-forest, 1 ↑↑ forest vs. non-forest, 4 , 3 n. a. |
| Wen, Y. et al. (2019) [36] | low | Healthy children/adults, adults with health conditions: hypertension, COPD, chronic stroke, chronic heart failure | Cardiovascular system | Blood pressure: systolic/diastolic Heart rate Pulse rate HRV | Blood pressure (8 studies): ↓↓ in 5 studies in forest group, 1 study ↓↓ between groups, 1 study ↑↑ between groups, 1 study irregular index Heart rate (3 studies): all ↓↓ between groups Pulse rate (5 studies): ↓↓ in 4 studies, 1 study ↓; HRV (6 studies): lnHF ↑↑ in 4 studies, 1 study ↓; lnLF/lnHF ↓↓ in 2 studies, 1 study ↓, 2 studies ↑ |
| Healthy adults, adults with health conditions: hypertension | Metabolic parameters | Triglyceride Adiponectin | Triglyceride (2 studies): ↓↓ Adiponectin (1 study): ↑↑ | ||
| Healthy adults, adults with health conditions: hypertension, COPD, chronic heart failure | Immune and/or inflammatory indices | NK cells NKT cells Interleukin (IL-6, IL-8) Tumor necrosis factor CRP | NK cells (2 studies): ↓↓ NKT cells (1 study): ↓↓; Interleukin (4 studies): in 3 studies ↓↓ Tumor necrosis factor (3 studies): 2 studies ↓↓ CRP (3 studies): 1 study ↓↓ | ||
| Adults with health conditions: chronic heart failure | Immune and/or inflammatory indices | Antioxidants: Glutathione peroxidase biological antioxidant potential; peroxides (8-hydroxy-2’-deoxyguanosine and hydrogen); MDAHyperventilation | Antioxidants: Glutathione peroxidase (1 study): ↑↑, biological antioxidant potential (1 study): ↑↑, Peroxides (1 study): ↓↓, MDA (2 studies): ↓↓ Hyperventilation (2 studies): ↓↓ | ||
| Healthy adults, adults with health conditions: hypertension, COPD | Mental health | Stress: Stress management; stress reaction; cortisol; adrenaline; norepinephrine; dopamine | Stress (6 studies): management 1 study ↑↑ between groups; reaction 1 study ↓↓ between groups; hormones (5 studies): 2 studies ↓↓ within group, 3 studies ↓↓ between groups | ||
| Healthy adults | Mental health | Electrophysiological indices:EEG, high alpha brain waves and high beta brain waves | Electrophysiological indices (1 study): ↑↑ | ||
| Healthy adults, adults with health conditions: hypertension, COPD, chronic heart failure | Mental health | POMS | POMS (14 studies): in 11 studies ↓↓ negative emotions, 10 studies ↑↑ tension, 2 studies ↑↑ positive emotions | ||
| Healthy adults, adults with health conditions: hypertension | Mental health | Attitudes and feelings about things: SD method | Attitudes and feelings about things (6 studies): in 5 studies ↑↑; 1 study n.a. | ||
| Healthy children/adults, adults with health conditions: chronic stroke | Mental health | Anxiety and Depression: BDI, HDR, CDI, STAI | Anxiety (6 studies): 4 studies ↓↓ within group, 3 studies ↓↓ between groups Depression (3 studies): 2 studies ↓↓ within group, 2 studies ↓↓ between groups | ||
| Healthy adults | Mental health | Degree of phys./psych. regeneration: Somatic Quality of Life: EQ-5D-3L; somatic symptoms; psychological regeneration; mental health | Degree of phys./psych. regeneration: Somatic Quality of life (1 study): ↑↑ within group somatic symptoms (2 studies): ↓↓ psychological regeneration, mental health (2 studies): ↑↑ | ||
| Healthy children/adults | Mental health | Adaptive Behaviour:Self-esteem; health-promoting behaviour | Adaptive Behaviour: self-esteem (1 study): ↑↑ health-promoting behaviour (1 study): ↑↑ | ||
| Chae, Y. R. et al. (2018) [35] | critically low | Healthy adults | Metabolic parameters | Triglycerid Level | Triglycerid Level (1 study): ↓↓ |
| Healthy adults | Menopausal symptoms | Menopausal Complaints: Menopausal symptoms | Menopausal Complaints: Menopausal symptoms (1 study): ↓ | ||
| Healthy adults: adults with health conditions: alcohol dependency | Mental health | Stress: Employment/job stress; psychosocial stress | Stress (8 studies): all ↓ | ||
| Healthy adults: adults with health conditions: alcohol dependency; Hwa-Byung; depression; cancer; mild cognitive impairment | Mental health | Depression: BDI; HDR; MADRS Anxiety: n.a. | Depression (9 studies): all ↓ Anxiety (7 studies): 4 studies ↓, 2 studies | ||
| Healthy adults: adults with health conditions: Hwa-Byung; depression; mild cognitive impairment | Quality of Life | Quality of life: SF-36; QoL | Quality of life (4 studies): all ↑ | ||
| Healthy adults: adults with health conditions: alcohol dependency | Mental health | Emotion: POMS | Emotion (2 studies): ↑↑ | ||
| Healthy adults: adults with health conditions: Hwa-Byung; depression; mild cognitive impairment | Mental health | Heart Rate Variability (HRV) | HRV (2 studies): ↑ | ||
| Putra, R. et al. (2018) [33] | critically low | Healthy adults | Immune and/or inflammatory indices | Immune function: NK activity; adrenaline concentration in urine; salivary/serum cortisol Blood pressure Pulse rate (PR) HRV WBC POMS | Immune function: NK activity (4 studies): all ↑↑ in forest group, adrenaline (4 studies): 2 studies ↓↓ in forest group, 1 study , 1 study ↑↑; cortisol (5 studies): 3 studies ↓↓, 1 study in forest group, 1 study ↓ in both groups Blood pressure (4 studies): 1 study , 2 studies ↓↓ in forest group, 1 study n.a. Pulse rate (5 studies): 3 studies ↓↓, 1 study unchanged, 1 study ↑↑ in forest group HRV (3 studies): 1 study ↑↑, 1 study ↓↓, 1 study in forest group WBC (4 studies): 2 studies , 2 studies n. a. POMS (4 studies): all ↑↑ in forest group |
| Farrow, M. R. and Washburn, K. (2019) [30] | critically low | Healthy adults | Mental health | Activity of the parasympathetic nervous system: HRV (InLF/HF, InHF) | Activity of the parasympathetic nervous system: ↑↑ InHF, ↓↓ lnLF/HF |
| Healthy adults, adults with health conditions: hypertension | Mental health | Blood pressure Pulse rate Salivary cortisol level Dopamine/Adrenaline/Noradrenalin in Urine Anxiety (POMS subscale values, SD Method) | Blood pressure (2 studies): ↓ Pulse rate (6 studies): ↑ Salivary cortisol (3 studies): ↓ Adrenaline in urine (1 study): ↓ Anxiety (8 studies): ↓ |
| Health Effects/Outcomes | Forest-Based Interventions | Reference of Association (+) | Reference of Association (+/−) | |
|---|---|---|---|---|
| Cardiovascular system | Blood pressure | Walking/sitting in and viewing forest area | Ideno, Y. et al. (2017) [28] | |
| Walking in forest area | Oh, B. et al. (2017) [19] | |||
| Walking/activity/rest in forest area | Wen, Y. et al. (2019) [36] | |||
| Heart and pulse rate | Walking/activity/rest in forest area | Wen, Y. et al. (2019) [36] | ||
| Sitting in and viewing forest area/walking and activities in the forest | Ideno, Y. et al. (2017) [28] | |||
| Cardio Ankle Vascular Index (CAVI) | Walking in forest area | Oh, B. et al. (2017) [19] | ||
| HRV | Walking/activity/rest in forest area | Wen, Y. et al. (2019) [36] |
| Health Effects/ Outcomes | Forest-Based Interventions | Reference of Association (+) | Reference of Association (+/−) | |
|---|---|---|---|---|
| Immune and/orinflammatory parameters | NK/NKT cells | Walking in forest area | Oh, B. et al. (2017) [19] | |
| Walking in forest area | Wen, Y. et al. (2019) [36] | |||
| Cytokines | Walking in forest area | Oh, B. et al. (2017) [19] | ||
| Walking in forest area; exposed to forest | Wen, Y. et al. (2019) [36] | |||
| CRP | Walking in forest area | Oh, B. et al. (2017) [19] | ||
| Walking in forest area | Wen, Y. et al. (2019) [36] | |||
| Tumour necrosis factor | Walking in forest area | Oh, B. et al. (2017) [19] | ||
| Walking in forest area; exposed to forest | Wen, Y. et al. (2019) [36] | |||
| Antioxidants | Walking in forest area | Oh, B. et al. (2017) [19] | ||
| Walking and meditation in forest area; exposed to forest | Wen, Y. et al. (2019) [36] |
| Health Effects/ Outcomes | Forest-Based Interventions | Reference of Association (+) | Reference of Association (+/–) | |
|---|---|---|---|---|
| Metabolic Parameters | Triglyceride level | Walking in forest area | Wen, Y. et al. (2019) [36] | |
| Adiponectin level | Walking in forest area | Wen, Y. et al. (2019) [36] |
| Health Effects/ Outcomes | Forest-Based Interventions | Reference of Association (+) | Reference of Association (+/–) | |
|---|---|---|---|---|
| Skin Diseases (Atopic Dermatitis) | SCORAD Index | Forest experience, forest trip; forest activity; forest camp; forest camp swimming | Lee, I. et al. (2016) [31] | |
| Forest trip; forest activity; forest camp | Lee, I et al. (2016) [31] |
| Health Effects/ Outcomes | Forest-Based Interventions | Reference of Association (+) | Reference of Association (+/−) | |
|---|---|---|---|---|
| Mental Health | Stress(cortisol level/PROs) | Walking in forest area; forest healing program | Lee, I. et al. (2017) [32] | |
| Forest healing program (with cognitive behavioural rehabilitation) | Oh, B. et al. (2017) [19] | |||
| Forest activity; forest healing program | Song, M. K. and Bang, K. -S. (2017) [34] | |||
| Walking/activity/rest in forest area | Wen, Y et al. (2019) [36] | |||
| Forest bathing: spending time in a forest, walking, resting, watching, and deep breathing for a limited time in forest | Antonelli, M. et al. (2019) [27] | |||
| Anxiety and depression (PROs) | Walking in forest area, resting in the forest, forest healing program, forest therapy | Lee, I. et al. (2017) [32] | ||
| Forest healing program (with cognitive behavioural rehabilitation) | Oh, B. et al. (2017) [19] | |||
| Activity in forest area, forest experience program | Song, M. K. and Bang, K. -S. (2017) [34] | |||
| Walking/activity/mediation/rest in forest area | Wen, Y. et al. (2019) [36] | |||
| Waking, mediation in forest area, forest therapy program | Kotera, Y. et al. (2020) [29] | |||
| Walking, activity, resting in forest area, forest experience program | Lee, I. et al. (2017) [32] | |||
| Negative emotions(PROs) | Walking in forest area | Oh, B. et al. (2017) [19] | ||
| Activity in forest area, forest experience program, forest ecology exploration | Song, M. K. and Bang, K. -S. (2017) [34] | |||
| Walking/activity/rest in forest area | Wen, Y. et al. (2019) [36] | |||
| Walking, resting/breathing in forest area, recreation program, forest therapy program, forest bathing program | Kotera, Y. et al. (2020) [29] | |||
| Quality of life/well-being(PROs) | Walking in the forest; forest-healing program, forest therapy | Lee, I. et al. (2017) [32] | ||
| Activities in the forest | Song, M. K. and Bang, K. -S. (2017) [34] | |||
| Walking/activities in the forest | Wen, Y. et al. (2019) [36] |
| Health Effects / Outcomes | Forest-based Interventions | Reference of Association (+) | Reference of Association (+/–) | |
|---|---|---|---|---|
| Sociality | Sociality(PRO) | Forest-experience program, forest-therapy program | Song, M. K. & Bang, K.-S. (2017) [32] | |
| Social Competence (PROs) | Forest-healing program, ecology exploration | Song, M. K. & Bang, K.-S. (2017) [32] | ||
| School Violence Attitude (PRO) | Forest-ecology exploration | Song, M. K. & Bang, K.-S. (2017) [32] | ||
| School Adjustment (PROs) | Activities in the forest; forest-experience program | Song, M. K. & Bang, K.-S. (2017) [32] | ||
| Life Respect (PRO) | Forest-therapy program | Song, M. K. & Bang, K.-S. (2017) [32] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stier-Jarmer, M.; Throner, V.; Kirschneck, M.; Immich, G.; Frisch, D.; Schuh, A. The Psychological and Physical Effects of Forests on Human Health: A Systematic Review of Systematic Reviews and Meta-Analyses. Int. J. Environ. Res. Public Health 2021, 18, 1770. https://doi.org/10.3390/ijerph18041770
Stier-Jarmer M, Throner V, Kirschneck M, Immich G, Frisch D, Schuh A. The Psychological and Physical Effects of Forests on Human Health: A Systematic Review of Systematic Reviews and Meta-Analyses. International Journal of Environmental Research and Public Health. 2021; 18(4):1770. https://doi.org/10.3390/ijerph18041770
Chicago/Turabian StyleStier-Jarmer, Marita, Veronika Throner, Michaela Kirschneck, Gisela Immich, Dieter Frisch, and Angela Schuh. 2021. "The Psychological and Physical Effects of Forests on Human Health: A Systematic Review of Systematic Reviews and Meta-Analyses" International Journal of Environmental Research and Public Health 18, no. 4: 1770. https://doi.org/10.3390/ijerph18041770
APA StyleStier-Jarmer, M., Throner, V., Kirschneck, M., Immich, G., Frisch, D., & Schuh, A. (2021). The Psychological and Physical Effects of Forests on Human Health: A Systematic Review of Systematic Reviews and Meta-Analyses. International Journal of Environmental Research and Public Health, 18(4), 1770. https://doi.org/10.3390/ijerph18041770






