How Dentists Face the COVID-19 in Mexico: A Nationwide Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Size Calculation
2.2. Questionnaire Desing
2.3. Sample Selection
2.4. Statistical Analyses
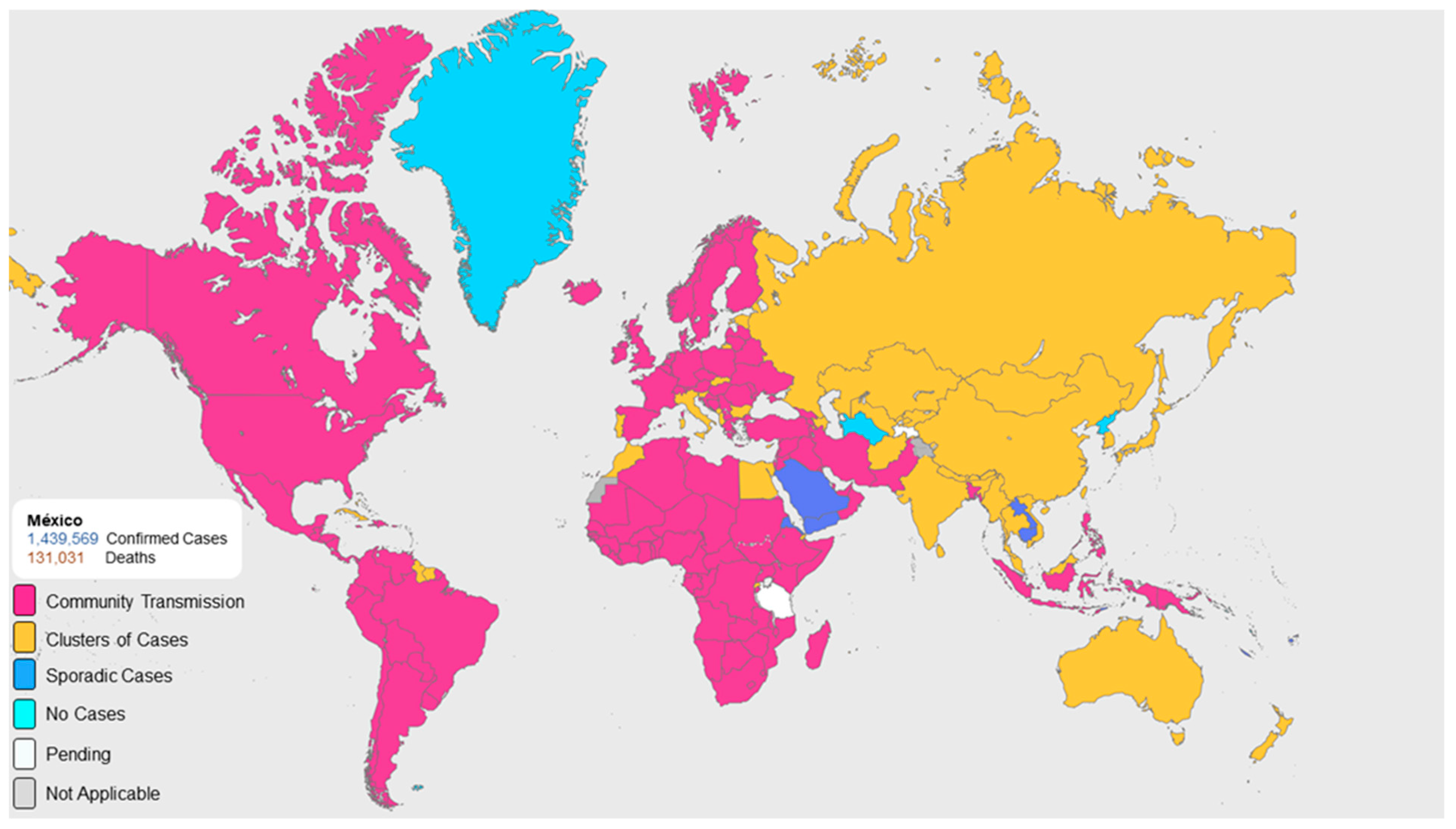
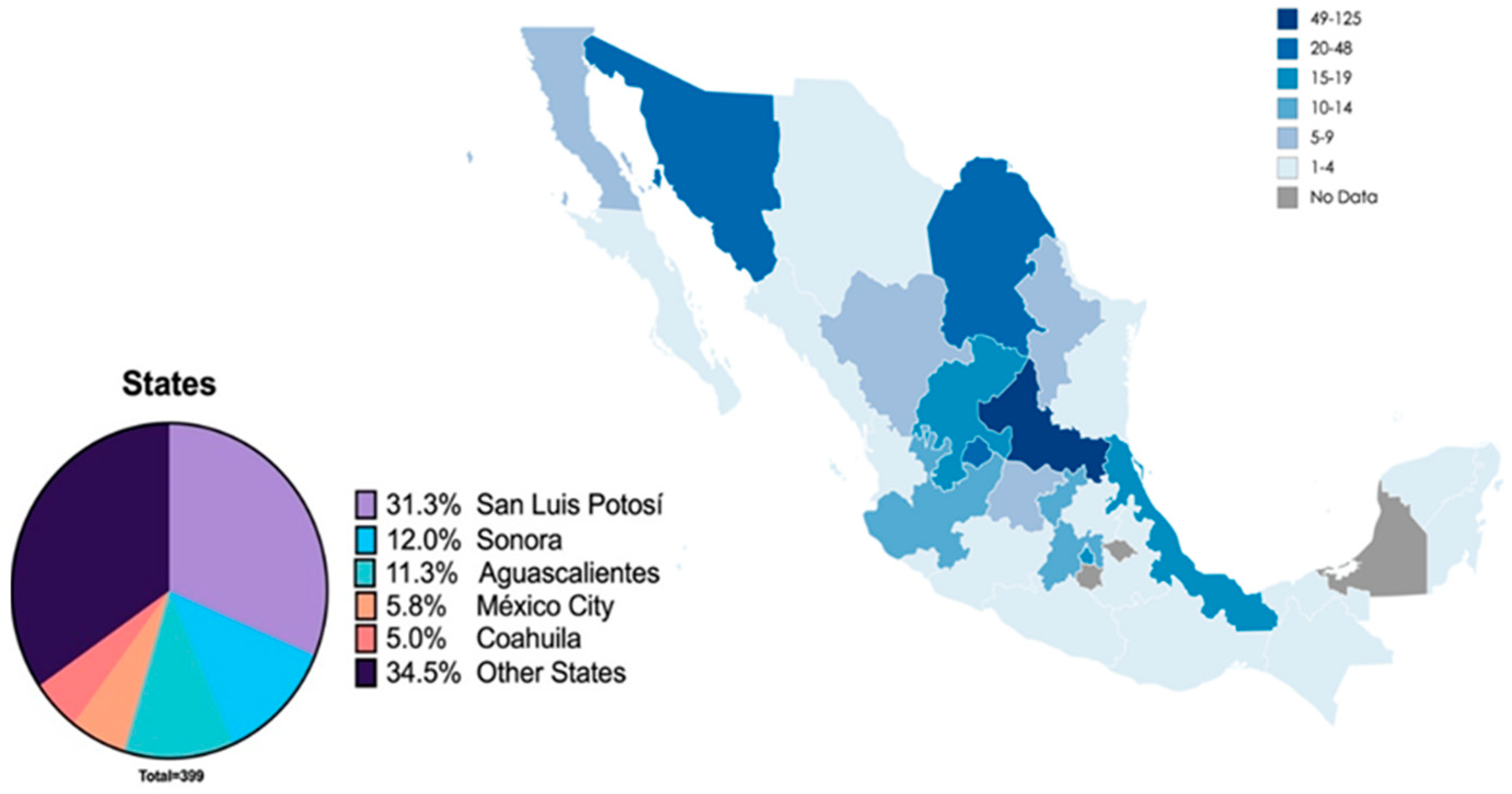
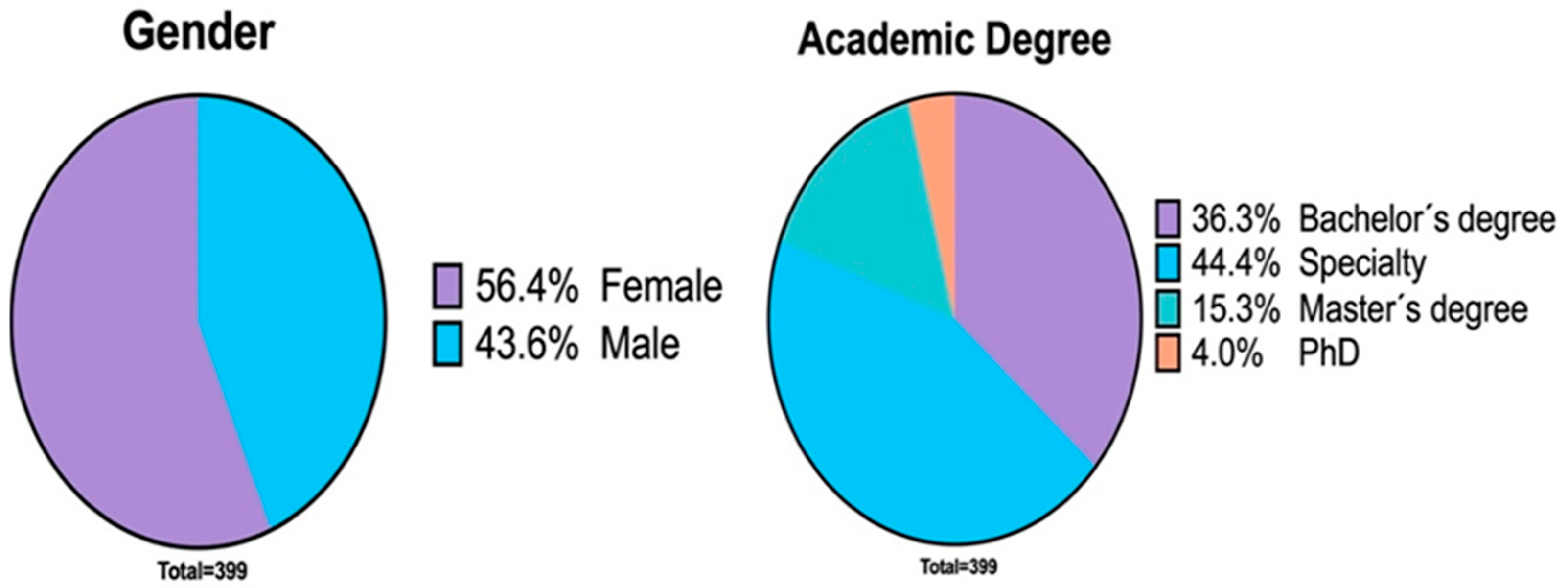
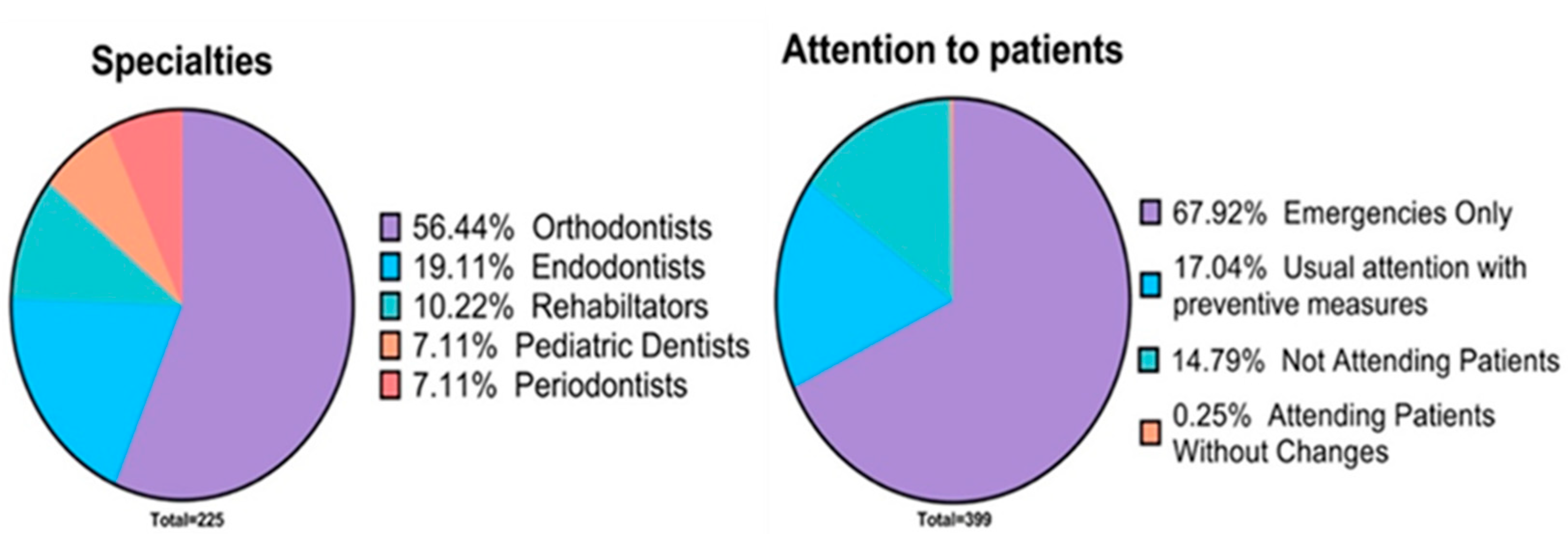
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kamate, S.K.; Sharma, S.; Thakar, S.; Srivastava, D.; Sengupta, K.; Hadi, A.J.; Chaudhary, A.; Joshi, R.; Dhanker, K. Assessing Knowledge, Attitudes and Practices of dental practitioners regarding the COVID-19 pandemic: A multinational study. Dent. Med. Probl. 2020, 57, 11–17. [Google Scholar] [CrossRef]
- Ahmed, M.A.; Jouhar, R.; Ahmed, N.; Adnan, S.; Aftab, M.; Zafar, M.S.; Khurshid, Z. Fear and Practice Modifications among Dentists to Combat Novel Coronavirus Disease (COVID-19) Outbreak. Int. J. Environ. Res. Public Health 2020, 17, 2821. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Zhong, L.; Deng, J.; Peng, J.; Dan, H.; Zeng, X.; Li, T.; Chen, Q. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int. J. Oral Sci. 2020, 12, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Meng, L.; Hua, F.; Bian, Z. Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine. J. Dent. Res. 2020, 99, 481–487. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Coronavirus Disease (COVID-2019) Situation Reports. Available online: https://covid19.who.int/region/amro/country/mx (accessed on 11 February 2020).
- Gobierno de México Documentos de Consulta Para el Personal de Salud. Recomendaciones Para la Práctica Odontológica. Available online: http://https://coronavirus.gob.mx/personal-de-salud/documentos-de-consulta/ (accessed on 10 February 2020).
- Peng, X.; Xu, X.; Li, Y.; Cheng, L.; Zhou, X.; Ren, B. Transmission routes of 2019-nCoV and controls in dental practice. Int. J. Oral Sci. 2020, 12, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Zhao, J.; Peng, J.; Li, X.; Deng, X.; Geng, Z.; Shen, Z.; Guo, F.; Zhang, Q.; Jin, Y. Detection of 2019-nCoV in Saliva and Characterization of Oral Symptoms in COVID-19 Patients. Cell Prolif. 2020, 53, e12923. [Google Scholar]
- Patini, R. How to face the post-SARS-CoV-2 outbreak era in private dental practice: Current evidence for avoiding cross-infections. Commun. Dent. 2020, 10, 237. [Google Scholar] [CrossRef]
- Sivaraman, K.; Chopra, A.; Narayana, A.; Radhakrishnan, R.A.J.G. A five-step risk management process for geriatric dental practice during SARS-CoV-2 pandemic. Gerodontology 2020. [Google Scholar] [CrossRef]
- Spagnuolo, G.; De Vito, D.; Rengo, S.; Tatullo, M. COVID-19 Outbreak: An Overview on Dentistry. Int. J. Environ. Res. Public Health 2020, 17, 2094. [Google Scholar] [CrossRef]
- ADA. ADA Coronavirus (COVID-19) Center for Dentists; ADA: Bengaluru, India, 2020. [Google Scholar]
- Martina, S.; Amato, A.; Rongo, R.; Caggiano, M.; Amato, M. The Perception of COVID-19 among Italian Dentists: An Orthodontic Point of View. Int. J. Environ. Res. Public Health 2020, 17, 4384. [Google Scholar] [CrossRef]
- Khader, Y.; Al Nsour, M.; Al-Batayneh, O.B.; Saadeh, R.; Bashier, H.; Alfaqih, M.; Al-Azzam, S.; Alshurman, B.A. Dentists’ Awareness, Perception, and Attitude Regarding COVID-19 and Infection Control: Cross-Sectional Study Among Jordanian Dentists. JMIR Public Health Surveill. 2020, 6, e18798. [Google Scholar] [CrossRef] [PubMed]
- Duruk, G.; Gümüşboğa, Z.Ş.; Çolak, C. Investigation of Turkish dentists’ clinical attitudes and behaviors towards the COVID-19 pandemic: A survey study. Braz. Oral Res. 2020, 34, e054. [Google Scholar] [CrossRef] [PubMed]
- Gambhir, R.S.; Dhaliwal, J.S.; Aggarwal, A.; Anand, S.; Anand, V.; Bhangu, A.K. Covid-19: A survey on knowledge, awareness and hygiene practices among dental health professionals in an Indian scenario. Rocz. Państw. Zakładu Hig. 2020, 71, 223–229. [Google Scholar]
- Quadri, M.F.A.; Jafer, M.A.; Alqahtani, A.S.; Al Mutahar, S.A.; Odabi, N.I.; Daghriri, A.A.; Tadakamadla, S.K. Novel corona virus disease (COVID-19) awareness among the dental interns, dental auxiliaries and dental specialists in Saudi Arabia: A nationwide study. J. Infect. Public Health 2020, 13, 856–864. [Google Scholar] [CrossRef]
- Brug, J.; Aro, A.R.; Oenema, A.; De Zwart, O.; Richardus, J.H.; Bishop, G.D. SARS Risk Perception, Knowledge, Precautions, and Information Sources, the Netherlands. Emerg. Infect. Dis. 2004, 10, 1486–1489. [Google Scholar] [CrossRef]
- Yu, J.; Zhang, T.; Zhao, D.; Haapasalo, M.; Shen, Y. Characteristics of Endodontic Emergencies during COVID-19 Outbreak in Wuhan. J. Endod. 2020, 46, 730–735. [Google Scholar] [CrossRef] [PubMed]
- Soltani, P.; Patini, R. Retracted COVID-19 articles: A side-effect of the hot race to publication. Science 2020, 125, 819–822. [Google Scholar] [CrossRef]
- Cagetti, M.G.; Cairoli, J.L.; Senna, A. Guglielmo Campus COVID-19 Outbreak in North Italy: An Overview on Dentistry. A Questionnaire Survey. Int. J. Environ. Res. Public Health 2020, 17, 3835. [Google Scholar] [CrossRef]
- Srivastava, K.C.; Shrivastava, D.; Sghaireen, M.G.; AlSharari, A.F.; Alduraywish, A.A.; Al-Johani, K.; Alam, M.K.; Khader, Y.; AlZarea, B.K. Knowledge, attitudes and practices regarding COVID-19 among dental health care professionals: A cross-sectional study in Saudi Arabia. J. Int. Med. Res. 2020, 48, 0300060520977593. [Google Scholar] [CrossRef]
- Yang, Y.; Zhou, Y.; Liu, X.; Tan, J. Health services provision of 48 public tertiary dental hospitals during the COVID-19 epidemic in China. Clin. Oral Investig. 2020, 24, 1861–1864. [Google Scholar] [CrossRef]
- Tysiąc-Miśta, M.; Dziedzic, A. The Attitudes and Professional Approaches of Dental Practitioners during the COVID-19 Outbreak in Poland: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2020, 17, 4703. [Google Scholar] [CrossRef]
- Farooq, I.; Ali, S. COVID-19 outbreak and its monetary implications for dental practices, hospitals and healthcare workers. Postgrad. Med. J. 2020, 96, 791–792. [Google Scholar] [CrossRef]
- Schwendicke, F.; Krois, J.; Gomez, J. Impact of SARS-CoV2 (Covid-19) on dental practices: Economic analysis. J. Dent. 2020, 99, 103387. [Google Scholar] [CrossRef] [PubMed]
- Basu, S. Non-communicable disease management in vulnerable patients during Covid-19. Indian J. Med. Ethic- 2020, 5, 103–105. [Google Scholar] [CrossRef] [PubMed]
- Patini, R. Management of special needs patients in dentistry during the SARS-CoV-2 pandemic. J. Int. Oral Health 2020, 12, 53. [Google Scholar] [CrossRef]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef] [PubMed]
- Aguilera-Galaviz, L.; Gaitán-Fonseca, C.; Bermúdez-Jiménez, C. Patient management in dental care and staff biosecurity during the SARS-CoV-2 coronavirus outbreak (COVID-19). Rev. Asoc. Dent. Mexic. 2020, 77, 88–95. [Google Scholar]
- World Health Organization. Advice on the Use of Masks in the Community, during Home Care, and in Health Care Settings in the Context of COVID-19: Interim Guidance, 19 March 2020; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- European Centre for Disease Prevention and Control. Personal Protective Equipment (PPE) Needs in Healthcare Settings for the Care of Patients with Suspected or Confirmed 2019-nCoV; ECDC Stockholm: Solna, Sweden, 2020.
- Lo Giudice, R. The Severe Acute Respiratory Syndrome Coronavirus-2 (SARS CoV-2) in Dentistry. Management of Biological Risk in Dental Practice. Int. J. Environ. Res. Public Health 2020, 17, 3067. [Google Scholar] [CrossRef]
- Card, K.J.; Crozier, D.; Dhawan, A.; Dinh, M.; Dolson, E.; Farrokhian, N.; Gopalakrishnan, V.; Ho, E.; Jagdish, T.; King, E.S. UV sterilization of personal protective equipment with idle laboratory biosafety cabinets during the Covid-19 pandemic. MedRxiv 2020. [Google Scholar] [CrossRef]
- Rubio-Romero, J.C.; del Carmen Pardo-Ferreira, M.; García, J.A.T.; Calero-Castro, S. Disposable masks: Disinfection and sterilization for reuse, and non-certified manufacturing, in the face of shortages during the COVID-19 pandemic. Saf. Sci. 2020, 129, 104830. [Google Scholar] [CrossRef]
- Hadi, J.; Dunowska, M.; Wu, S.; Brightwell, G.J.P. Control Measures for SARS-CoV-2: A Review on Light-Based Inactivation of Single-Stranded RNA Viruses. Pathogens 2020, 9, 737. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Zhang, X.; Zhang, X.; Wei, Z.; Zhang, L.; Xu, J.; Liang, P.; Xu, Y.; Zhang, C.; Xu, A. Rapid asymptomatic transmission of COVID-19 during the incubation period demonstrating strong infectivity in a cluster of youngsters aged 16–23 years outside Wuhan and characteristics of young patients with COVID-19: A prospective contact-tracing study. J. Infect. 2020, 80, e1–e13. [Google Scholar] [CrossRef] [PubMed]
- Martín Carreras-Presas, C.; Amaro Sánchez, J.; López-Sánchez, A.F.; Jané-Salas, E.; Pérez, M.L.S. Oral vesiculobullous lesions associated with SARS-CoV-2 infection. Oral. Dis. 2020. [Google Scholar] [CrossRef]
- Jia, J.L.; Kamceva, M.; Rao, S.A.; Linos, E. Cutaneous manifestations of COVID-19: A preliminary review. J. Am. Acad. Dermatol. 2020, 83, 687–690. [Google Scholar] [CrossRef] [PubMed]
| 1. Gender | Male |
| Female | |
| 2. Age | |
| 3. In which state of the country do you reside? | |
| 4. Level of study: | Bachelor’s degree |
| Specialty | |
| Master’s degree | |
| PhD | |
| 5. What specialty or master’s degree do you have? | |
| 6. What decision did you make regarding your daily consultation during the pandemic? | Not attending patients |
| Only attending emergencies | |
| Continue with the same amount of patients, following the measures of prevention. | |
| I did not make any changes. | |
| 7. If you continue seeing patients, what preventive measures have you implemented in your practice? | Phone triage |
| Shoe disinfection mat | |
| Infrared thermometer | |
| Handwashing | |
| Face-to-face questionnaire on patient health | |
| Space of at least one meter between patients | |
| Use of personal protective equipment | |
| Pre-operative rinse with mouthwash | |
| Chlorination of dental unit water | |
| Use of techniques that avoid the generation of aerosols | |
| Use of rubber dam | |
| 8. Which of the following personal protection barriers (PPE) do you use in your practice? | N95 face mask |
| Face mask other than N95 | |
| Gloves | |
| Googles or glasses | |
| Disposable gown | |
| Disposable surgical cap | |
| Face shield | |
| 9. Do you know the correct sequence of PPE placement and removal? | Yes |
| No | |
| 10. Do you know the disinfectant solutions for the dental office? | Yes |
| No | |
| 11. What disinfection solutions do you use in the disinfection of the dental office? | |
| 12. Do you know the main symptoms in patients suspected of COVID-19? | Yes |
| No | |
| 13. Do you know the skin symptoms that may be present in patients suspected of COVID-19? | Yes |
| No | |
| 14. Do you know the oral symptoms that can occur in a patient with COVID 19? | Yes |
| No | |
| 15. Do you carry out any type of disinfection of the material immediately after caring for a patient? | Yes |
| No | |
| 16. When do you thoroughly disinfect the dental office? | At the beginning of the day |
| At the end of the day | |
| At the end of the morning and evening consultation | |
| Weekly | |
| Between each patient | |
| 17. If you suspect a patient has COVID 19, do you know where to refer him/her? | Yes |
| No | |
| 18. What sterilization method do you use in your dental office? | Dry heat |
| Humid heat | |
| Chemical substances | |
| UV light | |
| 19. Have you verified the effectiveness of the sterilization methods you use? | Yes |
| No | |
| 20. Do dental office staff know and use PPE? | Yes |
| No | |
| 21. Do you have a sanitation filter at the entrance of your dental clinic or office? | Yes |
| No | |
| 22. Have you recently read scientific evidence about COVID-19 dental care? | Yes |
| No | |
| 23. Do you use any special equipment (in addition to the ejectors) for the elimination of the aerosols generated during the dental consultation? | Yes |
| No |
| Prevention Measures | Total of Dentists Who Answered the Question | n (%) |
|---|---|---|
| Phone triage | 280 (82.6) | |
| Shoe disinfection mat | 280 (82.6) | |
| Infrared thermometer | 169 (49.9) | |
| Handwashing | 326 (96.2) | |
| Face-to-face questionnaire on patient health | 257 (75.8) | |
| Space of at least one meter between patients | 339 | 310 (91.5) |
| Use of personal protective equipment | 329 (97) | |
| Pre-operative rinse with mouthwash | 252 (74.3) | |
| Chlorination of dental unit water | 134 (39.5) | |
| Use of techniques that avoid the generation of aerosols | 194 (57.2) | |
| Use of Rubber dam | 218 (64.3) |
| Protective Barriers | Total of Dentists Who Answered the Question | n (%) |
|---|---|---|
| N95 face mask | 238 (70.2) | |
| Face mask other than N95 | 140 (41.3) | |
| Gloves | 331 (97.6) | |
| Googles or glasses | 339 | 309 (91.1) |
| Disposable gown | 310 (91.5) | |
| Disposable surgical cap | 280 (82.6) | |
| Face shield | 326 (96.2) |
| Sterilization Method | Total of Dentists | n (%) |
|---|---|---|
| Humid heat sterilization | 293 (86.4) | |
| Sterilization by chemical substances | 339 | 167 (49.5) |
| Dry heat sterilization | 78 (23) | |
| UV light | 36 (10.6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Casillas Santana, M.Á.; Martínez Zumarán, A.; Patiño Marín, N.; Castillo Silva, B.E.; Sámano Valencia, C.; Salas Orozco, M.F. How Dentists Face the COVID-19 in Mexico: A Nationwide Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 1750. https://doi.org/10.3390/ijerph18041750
Casillas Santana MÁ, Martínez Zumarán A, Patiño Marín N, Castillo Silva BE, Sámano Valencia C, Salas Orozco MF. How Dentists Face the COVID-19 in Mexico: A Nationwide Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2021; 18(4):1750. https://doi.org/10.3390/ijerph18041750
Chicago/Turabian StyleCasillas Santana, Miguel Ángel, Alan Martínez Zumarán, Nuria Patiño Marín, Brenda Eréndida Castillo Silva, Carolina Sámano Valencia, and Marco Felipe Salas Orozco. 2021. "How Dentists Face the COVID-19 in Mexico: A Nationwide Cross-Sectional Study" International Journal of Environmental Research and Public Health 18, no. 4: 1750. https://doi.org/10.3390/ijerph18041750
APA StyleCasillas Santana, M. Á., Martínez Zumarán, A., Patiño Marín, N., Castillo Silva, B. E., Sámano Valencia, C., & Salas Orozco, M. F. (2021). How Dentists Face the COVID-19 in Mexico: A Nationwide Cross-Sectional Study. International Journal of Environmental Research and Public Health, 18(4), 1750. https://doi.org/10.3390/ijerph18041750








