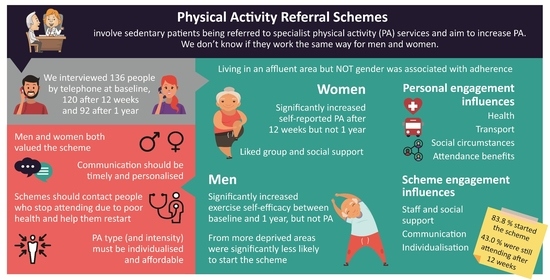
Gender Differences in Uptake, Adherence and Experiences: A Longitudinal, Mixed-Methods Study of a Physical Activity Referral Scheme in Scotland, UK
Abstract
1. Introduction
2. Materials and Methods
2.1. Scheme Context
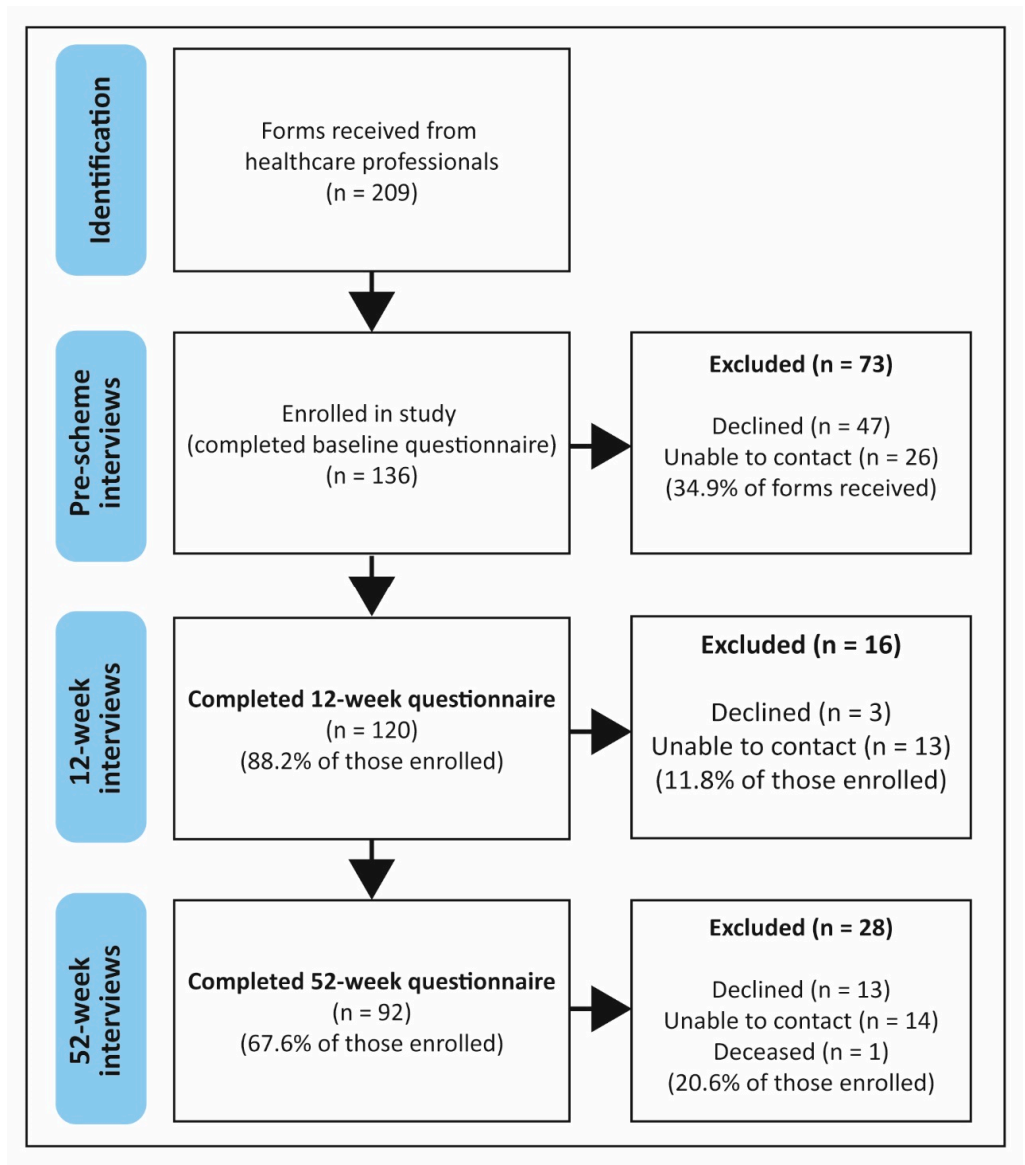
2.2. Sample
2.3. Data Collection
2.4. Quantitative Analysis
2.5. Qualitative Analysis
2.6. Data Integration
3. Results
3.1. Quantitative Findings
3.1.1. Participant Characteristics
3.1.2. Attendance, Drop out and Adherence
3.1.3. Behaviour Change for Study Completers
3.2. Qualitative Analysis
3.2.1. Gender Perspectives
“It is lots of fun and there are nice people there. The main thing has been meeting other people and getting out of the house. This has made me feel a lot happier. I just chat on with whoever happens to be there”(Participant 109, female, 60–69 years, 12-week dropout)
3.2.2. Personal Factors
Previous Physical Activity Levels
Health
Social Circumstances
Transport
Physical and Mental Benefits of Attendance
3.2.3. Scheme Process Factors
Communication with the PARS
Social and Staff Support
“It’s Not for Me”
4. Discussion
4.1. Uptake
4.2. Adherence
4.3. Change in Behaviour
4.4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef]
- Scottish Public Health Observatory. Physical Activity: Adults. Available online: https://www.scotpho.org.uk/behaviour/physical-activity/data/adults/#:~:text=In%202018%2C%2021%25%20of%20adults%20in%20Scotland%20reported,physical%20activity%2C%20or%20an%20equivalent%20combination%20of%20these%29 (accessed on 16 October 2020).
- Martín-Borràs, C.; Giné-Garriga, M.; Puig-Ribera, A.; Martín, C.; Solà, M.; Cuesta-Vargas, A.I. A new model of exercise referral scheme in primary care: Is the effect on adherence to physical activity sustainable in the long term? A 15-month randomised controlled trial. BMJ Open 2018, 8, e017211. [Google Scholar] [CrossRef]
- Onerup, A.; Arvidsson, D.; Blomqvist, Å.; Daxberg, E.-L.; Jivegård, L.; Jonsdottir, I.H.; Lundqvist, S.; Mellén, A.; Persson, J.; Sjögren, P.; et al. Physical activity on prescription in accordance with the Swedish model increases physical activity: A systematic review. Br. J. Sports Med. 2019, 53, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Craike, M.; Britt, H.; Parker, A.; Harrison, C. General practitioner referrals to exercise physiologists during routine practice: A prospective study. J. Sci. Med. Sport 2019, 22, 478–483. [Google Scholar] [CrossRef]
- American College of Sports Medicine. Exercise is Medicine, Health Care Providers. Available online: https://www.exerciseismedicine.org/support_page.php/health-care-providers/ (accessed on 21 September 2020).
- National Institute for Health and Care Excellence. Exercise Referral Schemes to Promote Physical Activity; NICE Public Health Guidance 54; National Institute for Health and Care Excellence: London, UK, 2014. [Google Scholar]
- British Heart Foundation National Centre. A Tool Kit for the Design, Implementation & Evaluation of Exercise Referral Schemes; British Heart Foundation National Centre for Physical Activity and Health: Loughborough, UK, 2010. [Google Scholar]
- Wade, M.; Mann, S.; Copeland, R.J.; Steele, J. Effect of exercise referral schemes upon health and well-being: Initial observational insights using individual patient data meta-analysis from the National Referral Database. J. Epidemiol. Community Health 2020, 74, 32. [Google Scholar] [CrossRef] [PubMed]
- Pavey, T.G.; Anokye, N.; Taylor, A.; Trueman, P.; Moxham, T.; Fox, K.; Hillsdon, M.; Green, C.; Campbell, J.; Foster, C. The clinical effectiveness and cost-effectiveness of exercise referral schemes: A systematic review and economic evaluation. Health Technol. Assess. 2011, 15, 1. [Google Scholar] [CrossRef] [PubMed]
- Campbell, F.; Holmes, M.; Everson-Hock, E.; Davis, S.; Buckley Woods, H.; Anokye, N.; Tappenden, P.; Kaltenthaler, E. A systematic review and economic evaluation of exercise referral schemes in primary care: A short report. Health Technol. Assess. 2015, 19, 1–87. [Google Scholar] [CrossRef] [PubMed]
- Pavey, T.G.; Taylor, A.; Hillsdon, M.; Fox, K.; Campbell, J.; Foster, C.; Moxham, T.; Mutrie, N.; Searle, J.; Taylor, R. Levels and predictors of exercise referral scheme uptake and adherence: A systematic review. J. Epidemiol. Community Health 2012, 66, 737–744. [Google Scholar] [CrossRef]
- Hanson, C.L.; Oliver, E.; Dodd-Reynolds, C.; Pearsons, A.; Kelly, P. A modified Delphi study to gain consensus for a taxonomy to report and classify Physical Activity Referral Schemes (PARS). Int. J. Behav. Nutr. Phys. Act. 2020, 17, 6832. [Google Scholar] [CrossRef]
- Oliver, E.J.; Hanson, C.L.; Lindsey, I.A.; Dodd-Reynolds, C.J. Exercise on referral: Evidence and complexity at the nexus of public health and sport policy. Int. J. Sport Policy Politics 2016, 8, 731–736. [Google Scholar] [CrossRef]
- Sowden, S.; Breeze, E.; Barber, J.; Raine, R. Do general practices provide equitable access to physical activity interventions? Brit. J. Gen. Pract. 2008, 58, e1–e8. [Google Scholar] [CrossRef]
- Hanson, C.L.; Allin, L.J.; Ellis, J.G.; Dodd-Reynolds, C.J. An evaluation of the efficacy of the exercise on referral scheme in Northumberland, UK: Association with physical activity and predictors of engagement. A naturalistic observation study. BMJ Open 2013, 3, e002849. [Google Scholar] [CrossRef] [PubMed]
- Dugdill, L.; Graham, R.; McNair, F. Exercise referral: The public health panacea for physical activity promotion? A critical perspective of exercise referral schemes; their development and evaluation. Ergonomics 2005, 48, 1390–1410. [Google Scholar] [CrossRef] [PubMed]
- Gidlow, C.; Johnston, L.H.; Crone, D.; Morris, C.; Smith, A.; Foster, C.; James, D.V.B. Socio-demographic patterning of referral, uptake and attendance in Physical Activity Referral Schemes. J. Public Health 2007, 29, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Kelly, M.C.; Rae, G.C.; Walker, D.; Partington, S.; Dodd-Reynolds, C.J.; Caplan, N. Retrospective cohort study of the South Tyneside Exercise Referral Scheme 2009–14: Predictors of dropout and barriers to adherence. J. Public Health 2017, 39, e257–e264. [Google Scholar] [CrossRef]
- Murphy, S.M.; Edwards, R.T.; Williams, N.; Raisanen, L.; Moore, G.; Linck, P.; Hounsome, N.; Din, N.U.; Moore, L. An evaluation of the effectiveness and cost effectiveness of the National Exercise Referral Scheme in Wales, UK: A randomised controlled trial of a public health policy initiative. J. Epidemiol. Community Health 2012, 66, 745–753. [Google Scholar] [CrossRef]
- Harrison, R.A.; Roberts, C.; Elton, P.J. Does primary care referral to an exercise programme increase physical activity one year later? A randomized controlled trial. J. Public Health 2005, 27, 25–32. [Google Scholar] [CrossRef]
- Isaacs, A.J.; Critchley, J.A.; Tai, S.S.; Buckingham, K.; Westley, D.; Harridge, S.D.; Smith, C.; Gottlieb, J.M. Exercise evaluation randomised trial (EXERT): A randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only. Health Technol. Assess. 2007, 11, 1–185. [Google Scholar] [CrossRef]
- James, D.; Mills, H.; Crone, D.; Johnston, L.H.; Morris, C.; Gidlow, C.J. Factors associated with physical activity referral completion and health outcomes. J. Sports Sci. 2009, 27, 1007–1017. [Google Scholar] [CrossRef] [PubMed]
- Morgan, K.; Rahman, M.; Moore, G. Patterning in Patient Referral to and Uptake of a National Exercise Referral Scheme (NERS) in Wales from 2008 to 2017: A Data Linkage Study. Int. J. Environ. Res. Public Health 2020, 17, 3942. [Google Scholar] [CrossRef] [PubMed]
- Harrison, R.A.; McNair, F.; Dugdill, L. Access to exercise referral schemes; a population based analysis. J. Public Health 2005, 27, 326–330. [Google Scholar] [CrossRef] [PubMed]
- Moore, G.F.; Raisanen, L.; Moore, L.; Din, N.U.; Murphy, S. Mixed-method process evaluation of the Welsh National Exercise Referral Scheme. Health Educ. 2013, 113, 476–501. [Google Scholar] [CrossRef]
- Pentecost, C.; Taket, A. Understanding exercise uptake and adherence for people with chronic conditions: A new model demonstrating the importance of exercise identity, benefits of attending and support. Health Educ. Res. 2011, 26, 908–922. [Google Scholar] [CrossRef] [PubMed]
- Buxton, K.; McGeorge, S. Audit of Exercise Referral Schemes in Scotland: A Snapshot of Current Practice; National Centre for Sport and Exercise Medicine: Loughborough, UK, 2018; p. 37. [Google Scholar]
- Stewart, L.; Dolan, E.; Carver, P.; Swinton, P.A. Per-protocol investigation of a best practice exercise referral scheme. Public Health 2017, 150, 26–33. [Google Scholar] [CrossRef]
- Eynon, M.J.; O’Donnell, C.; Williams, L. Gaining qualitative insight into the subjective experiences of adherers to an exercise referral scheme: A thematic analysis. J. Health Psychol. 2018, 23, 1476–1487. [Google Scholar] [CrossRef]
- Leech, N.L.; Onwuegbuzie, A.J. A typology of mixed methods research designs. Qual. Quant. 2009, 43, 265–275. [Google Scholar] [CrossRef]
- World Health Organisation. WHO STEPS Surveillance Manual: The WHO STEPwise Approach to Chronic Disease Risk Factor Surveillance; World Health Organisation: Geneva, Switzerland, 2005. [Google Scholar]
- Sallis, J.F.; Pinski, R.B.; Grossman, R.M.; Patterson, T.L.; Nader, P.R. The development of self-efficacy scales for health related diet and exercise behaviors. Health Educ. Res. 1988, 3, 283–292. [Google Scholar] [CrossRef]
- NHS Scotland. NHS Scotland Caldicott Guardian’s Principles into Practice; Scottish Government: Edinburgh, UK, 2010. Available online: https://www.gov.scot/publications/nhsscotland-caldicott-guardians-principles-practice/ (accessed on 8 February 2021).
- Braun, V.; Clarke, V.; Hayfield, N.; Terry, G. Thematic Analysis. In Handbook of Research Methods in Health Social Sciences; Springer: Singapore, 2019; pp. 843–860. [Google Scholar] [CrossRef]
- Ritchie, J.; Lewis, J.; O’Connor, W. Carrying out Qualitative Analysis. In Qualitative Research Practice: A Guide for Social Science Students and Researchers; Ritchie, J., Lewis, J., Eds.; Sage: London, UK, 2003; pp. 220–262. [Google Scholar]
- Prendergast, F. Service Evaluation of Exercise Referral Scheme Performance 2018–2019; Fife Sports and Leisure Trust: Fife, UK, 2020. [Google Scholar]
- Hanson, C.L.; Oliver, E.J.; Dodd-Reynolds, C.J.; Allin, L.J. How do participant experiences and characteristics influence engagement in exercise referral? A qualitative longitudinal study of a scheme in Northumberland, UK. BMJ Open 2019, 9, e024370. [Google Scholar] [CrossRef]
- McHale, S.; Astin, F.; Neubeck, L.; Dawkes, S.; Hanson, C.L. A systematic review and thematic synthesis exploring how a previous experience of physical activity influences engagement with cardiac rehabilitation. Eur. J. Cardiovasc. Nurs. 2019, 19, 31–43. [Google Scholar] [CrossRef]
- Bäck, M.; Öberg, B.; Krevers, B. Important aspects in relation to patients’ attendance at exercise-based cardiac rehabilitation—Facilitators, barriers and physiotherapist’s role: A qualitative study. BMC Cardiovasc. Disord. 2017, 17, 77. [Google Scholar] [CrossRef] [PubMed]
- Herber, O.R.; Smith, K.; White, M.; Jones, M.C. ‘Just not for me’—Contributing factors to nonattendance/noncompletion at phase III cardiac rehabilitation in acute coronary syndrome patients: A qualitative enquiry. J. Clin. Nurs. 2017, 26, 3529–3542. [Google Scholar] [CrossRef]
- Douglas, F.; Teijlingen, E.; Torrance, N.; Fearn, P.; Kerr, A.; Meloni, S. Promoting physical activity in primary care settings: Health visitors’ and practice nurses’ views and experiences. J. Adv. Nurs. 2006, 55, 159–168. [Google Scholar] [CrossRef]
- Graham, R.C.; Dugdill, L.; Cable, N.T. Health professionals’ perspectives in exercise referral: Implications for the referral process. Ergonomics 2005, 48, 1411–1422. [Google Scholar] [CrossRef] [PubMed]
- Bélanger, M.; Couturier, E.; Dion, N.; Girouard, V.; Phillips, J.; Brunet, J. Family Physicians’ Perceptions Toward Writing Physical Activity Prescriptions: Contrasting Prescribers And Non-prescribers Perceptions. Med. Sci. Sports Exerc. 2015, 47, 69. [Google Scholar] [CrossRef]
- Ribera, A.P.; McKenna, J.; Riddoch, C. Attitudes and practices of physicians and nurses regarding physical activity promotion in the Catalan primary health-care system. Eur. J. Public Health 2005, 15, 569–575. [Google Scholar] [CrossRef] [PubMed]
- Tobi, P.; Estacio, E.V.; Yu, G.; Renton, A.; Foster, N. Who stays, who drops out? Biosocial predictors of longer-term adherence in participants attending an exercise referral scheme in the UK. BMC Public Health 2012, 12, 347. [Google Scholar] [CrossRef]
- Department of Health and Social Care. UK Chief Medical Officers’ Physical Activity Guidelines. 2019. Available online: https://www.gov.uk/government/publications/physical-activity-guidelines-uk-chief-medical-officers-report (accessed on 8 February 2021).
| Functional Level | Description |
|---|---|
| Level 1 | Limited standing, balance and require mobility aid |
| Level 2 | Mobile (without aid) but have difficulty with movement or activities of daily living |
| Level 3 | Independently mobile |
| Level 4 | Independently mobile and physically active |
| Characteristic | Baseline | 12 Weeks | 52 Weeks | |||
|---|---|---|---|---|---|---|
| n (136) | % | n (120) | % | n (92) | % | |
| Gender | ||||||
| Female | 65 | 47.8 | 59 | 49.2 | 42 | 45.7 |
| Male | 71 | 52.2 | 61 | 50.8 | 50 | 54.3 |
| Age group | ||||||
| <50 | 21 | 15.4 | 15 | 12.5 | 7 | 7.6 |
| 50–59 | 23 | 16.9 | 20 | 16.7 | 17 | 18.5 |
| 60–69 | 40 | 29.4 | 37 | 30.8 | 32 | 34.8 |
| 70+ | 52 | 38.2 | 48 | 40.0 | 36 | 9.1 |
| SIMD * | ||||||
| 1 (most deprived) | 16 | 11.8 | 15 | 12.5 | 9 | 9.8 |
| 2 | 25 | 18.4 | 19 | 15.8 | 16 | 17.4 |
| 3 | 19 | 14.0 | 16 | 13.3 | 12 | 13.0 |
| 4 | 31 | 22.8 | 27 | 22.5 | 23 | 25.0 |
| 5 (least deprived) | 45 | 33.1 | 43 | 35.8 | 32 | 34.8 |
| Education Level | ||||||
| Primary | 8 | 5.9 | 7 | 5.8 | 5 | 5.4 |
| Secondary | 73 | 53.7 | 63 | 52.5 | 50 | 54.4 |
| Post-secondary further education | 18 | 13.2 | 23 | 19.2 | 16 | 17.4 |
| Bachelor degree or higher | 29 | 21.4 | 27 | 22.5 | 21 | 13.0 |
| Employment status | ||||||
| Employed/self-employed | 28 | 20.6 | 26 | 21.7 | 19 | 20.7 |
| Retired | 84 | 61.8 | 76 | 63.3 | 60 | 65.2 |
| Claiming incapacity benefit/other | 24 | 17.6 | 18 | 15.0 | 13 | 14.1 |
| Reason for referral | ||||||
| COPD | 15 | 11 | 14 | 11.7 | 9 | 9.8 |
| CVD secondary prevention | 35 | 25.7 | 33 | 27.5 | 30 | 32.6 |
| Falls | 16 | 11.8 | 13 | 10.8 | 9 | 9.8 |
| Stroke | 13 | 9.6 | 12 | 10.0 | 11 | 12.0 |
| Type 1 or 2 diabetes | 8 | 5.9 | 6 | 5.0 | 5 | 5.4 |
| Obesity | 29 | 21.3 | 25 | 20.8 | 17 | 18.5 |
| Multiple sclerosis/rheumatic disease | 20 | 14.7 | 17 | 14.2 | 11 | 11.9 |
| No. of co-morbidities | ||||||
| 0–1 | 31 | 22.8 | 27 | 22.5 | 17 | 18.5 |
| 2 | 35 | 25.7 | 29 | 24.2 | 21 | 22.8 |
| 3+ | 70 | 51.5 | 64 | 53.3 | 54 | 58.7 |
| Transport to sessions | ||||||
| Private car | 100 | 73.5 | 89 | 74.1 | 68 | 73.9 |
| Public transport | 19 | 14 | 16 | 13.3 | 13 | 14.1 |
| Other (walking, cycling) | 17 | 12.5 | 15 | 12.5 | 11 | 11.9 |
| Type of session attended | ||||||
| Circuit class | N/A | 61 | 50.8 | 52 | 56.5 | |
| Gym | 14 | 11.7 | 12 | 13 | ||
| Gym circuit | 11 | 9.2 | 8 | 8.7 | ||
| Seated exercise/aqua aerobics | 12 | 10.0 | 10 | 10.9 | ||
| Did not attend any sessions | 22 | 18.3 | 10 | 10.9 | ||
| Characteristic | Baseline (n = 136) | 12-Week Study Completers (n = 120) | 52-Week Study Completers (n = 92) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Female | Male | Female | Male | Female | Male | |||||||
| n (65) | % | n (71) | % | n (59) | % | n (61) | % | n (42) | % | n (50) | % | |
| Age group | ||||||||||||
| <59 | 24 | 36.3 | 20 | 28.2 | 19 | 32.2 | 16 | 26.2 | 10 | 23.8 | 14 | 28 |
| 60–69 | 19 | 29.2 | 21 | 29.6 | 18 | 30.5 | 19 | 31.1 | 17 | 40.5 | 15 | 30 |
| 70+ | 22 | 33.8 | 30 | 42.3 | 22 | 37.3 | 26 | 42.6 | 15 | 35.7 | 21 | 42 |
| SIMD * | ||||||||||||
| 1 (most deprived) and 2 | 22 | 33.8 | 19 | 26.8 | 18 | 30.5 | 16 | 26.2 | 10 | 23.8 | 15 | 30 |
| 3 | 8 | 12.3 | 11 | 15.5 | 7 | 11.9 | 9 | 14.8 | 6 | 14.3 | 6 | 12 |
| 4 | 13 | 20 | 18 | 25.4 | 12 | 20.3 | 15 | 24.6 | 10 | 23.8 | 13 | 26 |
| 5 (least deprived) | 22 | 33.8 | 23 | 32.4 | 22 | 37.3 | 21 | 34.4 | 16 | 38.1 | 16 | 32 |
| Education Level | ||||||||||||
| Primary/secondary/further education | 50 | 76.9 | 57 | 80.3 | 44 | 75.6 | 49 | 80.3 | 30 | 71.4 | 41 | 82 |
| Bachelor degree or higher | 15 | 23.1 | 16 | 19.7 | 15 | 25.4 | 12 | 19.7 | 12 | 28.6 | 9 | 18 |
| Employment status | ||||||||||||
| Employed/self-employed | 12 | 18.5 | 16 | 22.5 | 11 | 18.6 | 15 | 24.6 | 5 | 11.9 | 14 | 28 |
| Retired | 39 | 60 | 45 | 63.4 | 38 | 64.4 | 38 | 62.3 | 30 | 71.4 | 30 | 60 |
| Claiming incapacity benefit/other | 14 | 21.5 | 10 | 14.1 | 10 | 16.9 | 8 | 13.1 | 7 | 16.7 | 6 | 12 |
| Reason for referral | ||||||||||||
| CVD secondary prevention | 7 | 10.8 | 28 | 39.4 | 7 | 11.9 | 26 | 42.6 | 7 | 16.7 | 23 | 46 |
| COPD and falls prevention | 19 | 29.2 | 12 | 16.9 | 18 | 30.5 | 9 | 14.8 | 13 | 31 | 5 | 10 |
| Obesity | 20 | 30.8 | 9 | 12.7 | 17 | 28.8 | 7 | 11.5 | 10 | 23.8 | 7 | 14 |
| Other ** | 19 | 29.2 | 22 | 31 | 11 | 32.2 | 18 | 29.5 | 12 | 28.6 | 15 | 30 |
| No. of co-morbidities | ||||||||||||
| 0–1 | 14 | 21.5 | 17 | 23.9 | 14 | 23.7 | 13 | 21.3 | 7 | 16.7 | 10 | 20 |
| 2 | 17 | 26.2 | 18 | 25.4 | 13 | 22 | 16 | 26.2 | 7 | 16.7 | 14 | 28 |
| 3+ | 34 | 52.3 | 36 | 50.7 | 32 | 54.2 | 32 | 52.5 | 28 | 66.7 | 26 | 52 |
| Transport to sessions | ||||||||||||
| Private car | 68 | 73.9 | 53 | 74.6 | 43 | 74.1 | 46 | 75.4 | 30 | 71.4 | 38 | 77.6 |
| Public transport, walking or cycling | 24 | 26 | 16 | 22.4 | 15 | 25.9 | 12 | 19.7 | 12 | 28.6 | 11 | 22.4 |
| Type of session attended | ||||||||||||
| Exercise class (circuit/seated/aqua) | N/A | 37 | 62.8 | 36 | 59.1 | 31 | 73.8 | 31 | 62 | |||
| Gym/gym circuit | 10 | 16.9 | 15 | 24.6 | 6 | 14.3 | 14 | 28 | ||||
| Did not attend any sessions | 12 | 20.3 | 10 | 16.4 | 5 | 11.9 | 5 | 10 | ||||
| All Participants | Females | Males | ||||
|---|---|---|---|---|---|---|
| (n = 136) | % | (n = 65) | % | (n = 71) | % | |
| Did not start | 22 | 16.2 | 11 | 16.9 | 11 | 15.5 |
| Uptake (attended at least one session) | 114 | 83.8 | 54 | 83.1 | 60 | 84.5 |
| Dropout (of those who started, those who attended 1–7 sessions) | 65 | 57.0 | 30 | 55.6 | 35 | 58.3 |
| Adherence (of those who started, those who attended ≥ 8 sessions) | 49 | 43.0 | 24 | 44.4 | 25 | 41.7 |
| Overall scheme adherence (of those referred, those who attended ≥ 8 sessions) | 49 | 36.0 | 24 | 36.9 | 25 | 35.2 |
| Completers (n = 92) * | 12 Weeks | 52 Weeks | ||
|---|---|---|---|---|
| n | % | n | % | |
| Did not start | 11 | 12.2 | 10 | 10.9 |
| Uptake (attended at least one session after referral) | 81 | 88.0 | 82 | 89.1 |
| Dropout (of those who started, those who attended 1–7 sessions in previous 12 weeks) | 38 | 57.0 | 40 | 43.5 |
| Adherence (of those who started, those who attended ≥ 8 sessions in previous 12 weeks) | 43 | 53.1 | 34 | 41.5 |
| Overall scheme adherence (of those referred, those who attended ≥ 8 sessions in previous 12 weeks) | 43 | 46.7 | 34 | 37.0 |
| Measure | Classification | Attendance Status | Baseline | 12 Weeks | 52 Weeks | Significance | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | Median | IQR | Overall α < 0.05 | a α < 0.0167 | b α < 0.0167 | |||
| Global Physical Activity Questionnaire | Total weekly PA (MET-Min/Week) | All study completers (n = 92) | 900.0 | 210.0–1980.0 | 960.0 | 480.0–2175.0 | 780.0 | 360.0–1440.0 | 0.057 | ||
| Female study completers (n = 42) | 520.00 a | 0.0–1140.0 | 760.0 a | 340.0–1800.0 | 620.0 | 240.0–1095.0 | 0.004 | 0.001 | |||
| Male study completers (n = 50) | 1440.0 | 465.0–2400.0 | 1220.0 | 590–2450.0 | 980.0 | 405.0–1710.0 | 0.214 | ||||
| 12-week adherers (n = 43) | 720.0 | 240.0–2040.0 | 960.0 | 400.0–2180.0 | 720.0 | 360.0–1440.0 | 0.105 | ||||
| Female 12-week adherers (19) | 360.0 a | 0.0–960.0 | 720.0 a | 280.0–2160.0 | 440.0 | 240.0–720.0 | 0.008 | 0.005 | |||
| Male 12-week adherers (n = 24) | 1410.0 | 450.0–2370.0 | 1340.0 | 695.0–2250.0 | 960.0 | 435.0–1950.0 | 0.740 | ||||
| 12-week dropouts (n = 38) | 1200.0 | 230.0–2520.0 | 1000.0 | 240.0–2040.0 | 880.0 | 230.0–1500.0 | 0.055 | ||||
| Non-starter (n = 11) | 480.0 a | 0.0–1440.0 | 880.0 | 623.0–1320.0 | 720.0 a | 560.0–1680.0 | 0.045 | 0.014 | |||
| Sedentary behaviour (Min/day) | All study completers (n = 92) | 540.0 a | 360.0–682.5 | 540.0 b | 420.0–660.0 | 480.0 a b | 300.0–600.0 | <0.0005 | 0.002 | 0.001 | |
| Female study completers (n = 42) | 600.0 | 360.0–720.0 | 555.0 | 420.0–660.0 | 480.0 | 322.5–607.5 | 0.027 | not sig. in post hoc tests | |||
| Male study completers (n = 50) | 480.0 a | 360.0–7.20.0 | 540.0 b | 442.5–660.0 | 450.0 a b | 300.0–600.0 | 0.001 | 0.009 | 0.003 | ||
| 12-week adherers (n = 43) | 480.0 a | 360.0–660.0 | 510.0 b | 420.0–660.0 | 420.0 a b | 300.0–600.0 | 0.001 | 0.007 | 0.002 | ||
| Female 12-week adherers (n = 19) | 540.0 | 360.0–660.0 | 510.0 | 420.0–660.0 | 480.0 | 300.0–600.0 | 0.060 | ||||
| Male 12-week adherers (n = 24) | 465.0 | 410.0–780.0 | 525.0 a | 427.5–682.5 | 360.0 a | 300.0–600.0 | 0.006 | 0.004 | |||
| 12-week dropouts (n = 38) | 570.0 a | 345.0–720.0 | 592.5 | 360.0–675.0 | 480.0 a | 322.5–615.0 | 0.017 | 0.016 | |||
| Non-starter (n = 11) | 600.0 | 360.0–780.0 | 600.0 | 540.0–780.0 | 600.0 | 360.0–720.0 | 0.562 | ||||
| Measure | Attendance Status | Baseline | 12 Weeks | 52 Weeks | Significance | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | Median | IQR | Overall | a | b | |||
| α < 0.05 | α < 0.0167 | α < 0.0167 | |||||||||
| Self-Efficacy and Exercise Habits Survey | Making time for PA | All study completers (n = 92) | 3.7 b | 3.0–4.3 | 3.7 a | 3.0–4.3 | 4.3 a b | 3.3–5.0 | <0.0005 | 0.001 | <0.0005 |
| Female study completers (n = 42) | 3.2 | 2.7–3.8 | 3.4 | 2.8–4.3 | 3.7 | 2.7–4.4 | 0.642 | ||||
| Male study completers (n = 50) | 3.9 a | 3.5–4.7 | 3.7 b | 3.0–4.4 | 5.0 a b | 4.3–5.0 | <0.05 | 0.001 | <0.0005 | ||
| 12-week adherers (n = 43) | 3.7 | 3.0–4.0 | 3.7 a | 3.0–4.3 | 4.3 a | 3.3–5.0 | 0.046 | not sig. in post hoc tests | |||
| Female 12-week adherers (n = 19) | 3.0 | 2.7–3.7 | 3.0 | 2.5–4.3 | 3.3 | 2.3–4.3 | 0.678 | ||||
| Male 12-week adherers (n = 24) | 3.9 a | 3.5–4.7 | 3.7 b | 3.7–4.6 | 5.0 a b | 4.4–5.0 | <0.0005 | 0.009 | <0.0005 | ||
| 12-week dropouts (n = 38) | 3.7 a | 3.0–4.4 | 3.6 b | 2.8–4.3 | 4.5 a b | 3.7–5.0 | 0.001 | 0.014 | <0.0005 | ||
| Non-starter (n = 11) | 3.3 | 2.7–4.7 | 3.3 | 3.0–4.3 | 4.1 | 3.0–5.0 | 0.218 | ||||
| Sticking to PA | All study completers (n = 92) | 3.7 a | 3.2–4.2 | 3.8 b | 3.2–4.3 | 4.5 a b | 3.5–5.0 | <0.0005 | <0.0005 | <0.0005 | |
| Female study completers (n = 42) | 3.5 a | 3.0–4.3 | 3.8 | 3.0–4.3 | 4.0 a | 3.3–4.8 | 0.019 | 0.006 | |||
| Male study completers (n = 50) | 3.7 a | 3.3–4.3 | 3.6 b | 3.3–4.3 | 4.7 a b | 3.8–5.0 | <0.0005 | <0.0005 | <0.0005 | ||
| 12-week adherers (n = 43) | 3.8 a | 3.3–4.0 | 4.0 b | 3.5–4.0 | 4.6 a b | 3.8–5.0 | <0.0005 | <0.0005 | 0.001 | ||
| Female 12-week adherers (n = 19) | 3.7 | 3.0–4.2 | 3.8 | 3.4–4.5 | 4.0 | 3.5–4.8 | 0.171 | ||||
| Male 12-week adherers (n = 24) | 3.9 a | 3.4–4.6 | 4.3 b | 3.5–4.8 | 4.8 a b | 4.5–5.1 | 0.001 | 0.004 | 0.005 | ||
| 12-week dropouts (n = 38) | 3.4 a | 3.1–4.1 | 3.6 b | 3.1–4.1 | 4.2 a b | 3.3–4.9 | <0.0005 | <0.0005 | 0.010 | ||
| Non-starter (n = 11) | 3.4 | 2.5–3.8 | 3.0 | 2.8–3.8 | 3.6 | 3.3–5.0 | 0.202 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hanson, C.L.; Neubeck, L.; Kyle, R.G.; Brown, N.; Gallagher, R.; Clark, R.A.; McHale, S.; Dawkes, S. Gender Differences in Uptake, Adherence and Experiences: A Longitudinal, Mixed-Methods Study of a Physical Activity Referral Scheme in Scotland, UK. Int. J. Environ. Res. Public Health 2021, 18, 1700. https://doi.org/10.3390/ijerph18041700
Hanson CL, Neubeck L, Kyle RG, Brown N, Gallagher R, Clark RA, McHale S, Dawkes S. Gender Differences in Uptake, Adherence and Experiences: A Longitudinal, Mixed-Methods Study of a Physical Activity Referral Scheme in Scotland, UK. International Journal of Environmental Research and Public Health. 2021; 18(4):1700. https://doi.org/10.3390/ijerph18041700
Chicago/Turabian StyleHanson, Coral L., Lis Neubeck, Richard G. Kyle, Norrie Brown, Robyn Gallagher, Robyn A. Clark, Sheona McHale, and Susan Dawkes. 2021. "Gender Differences in Uptake, Adherence and Experiences: A Longitudinal, Mixed-Methods Study of a Physical Activity Referral Scheme in Scotland, UK" International Journal of Environmental Research and Public Health 18, no. 4: 1700. https://doi.org/10.3390/ijerph18041700
APA StyleHanson, C. L., Neubeck, L., Kyle, R. G., Brown, N., Gallagher, R., Clark, R. A., McHale, S., & Dawkes, S. (2021). Gender Differences in Uptake, Adherence and Experiences: A Longitudinal, Mixed-Methods Study of a Physical Activity Referral Scheme in Scotland, UK. International Journal of Environmental Research and Public Health, 18(4), 1700. https://doi.org/10.3390/ijerph18041700