Pulmonary Hypertension in Acute and Chronic High Altitude Maladaptation Disorders
Abstract
1. Introduction
2. Hypoxic Pulmonary Vasoconstriction
3. Pulmonary Circulation in Sea Level Residents upon Acute Exposure to High Altitude
3.1. Factors Modulating the Magnitude of the Hypoxic Pulmonary Vascular Responses
3.2. Pulmonary Hypertension in HIgh Altitude Pulmonary Edema
3.3. Prevention and Treatment of Pulmonary Hypertension in High Altitude Pulmonary Edema
3.3.1. Non-Pharmacological Prevention of Pulmonary Hypertension in High Altitude Pulmonary Edema
3.3.2. Pharmacological Prevention of Pulmonary Hypertension in High Altitude Pulmonary Edema
3.4. Treatment of Pulmonary Hypertension in High Altitude Pulmonary Edema
4. Pulmonary Circulation in Sea Level Residents Chronically Exposed to High Altitude
5. Pulmonary Circulation in Healthy High Altitude Residents
6. High Altitude Pulmonary Hypertension and Chronic Mountain Sickness
6.1. Hypoxia Inducible Factors (HIFs)–Prolyl Hydroxylase Domain (PHD) Enzymes–von Hippel–Lindau Tumor Suppressor (VHL) Protein System
6.2. Variability in Hypoxic Pulmonary Vasoconstriction
6.3. Erythrocytosis
6.4. Fetal Programming
6.5. Iron Deficiency
7. Other Clinical Forms of Pulmonary Hypertension at High Altitude
8. Prevention and Treatment of Pulmonary Hypertension in High Altitude Dwellers
8.1. Potential of Drugs Approved for Treatment of Pulmonary Arterial Hypertension
8.2. Drug Repurposing
8.3. Novel Potential Therapeutic Targets
9. Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- West, J.B. High-altitude medicine. Am. J. Respir. Crit. Care Med. 2012, 186, 1229–1237. [Google Scholar] [CrossRef] [PubMed]
- Burtscher, M.; Gatterer, H.; Burtscher, J.; Mairbaurl, H. Extreme Terrestrial Environments: Life in Thermal Stress and Hypoxia. A Narrative Review. Front. Physiol. 2018, 9, 572. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, M.R.; Ghofrani, H.A.; Weissmann, N.; Aldashev, A.; Zhao, L. Pathophysiology and treatment of high-altitude pulmonary vascular disease. Circulation 2015, 131, 582–590. [Google Scholar] [CrossRef]
- Luks, A.M.; Swenson, E.R.; Bartsch, P. Acute high-altitude sickness. Eur. Respir. Rev. Off. J. Eur. Respir. Soc. 2017, 26, 160096. [Google Scholar] [CrossRef]
- Penaloza, D.; Arias-Stella, J. The heart and pulmonary circulation at high altitudes: Healthy highlanders and chronic mountain sickness. Circulation 2007, 115, 1132–1146. [Google Scholar] [CrossRef]
- Rhodes, J. Comparative physiology of hypoxic pulmonary hypertension: Historical clues from brisket disease. J. Appl. Physiol. 2005, 98, 1092–1100. [Google Scholar] [CrossRef]
- Sylvester, J.T.; Shimoda, L.A.; Aaronson, P.I.; Ward, J.P. Hypoxic pulmonary vasoconstriction. Physiol. Rev. 2012, 92, 367–520. [Google Scholar] [CrossRef]
- Waypa, G.B.; Schumacker, P.T. Oxygen sensing in hypoxic pulmonary vasoconstriction: Using new tools to answer an age-old question. Exp. Physiol. 2008, 93, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Sommer, N.; Strielkov, I.; Pak, O.; Weissmann, N. Oxygen sensing and signal transduction in hypoxic pulmonary vasoconstriction. Eur. Respir. J. 2016, 47, 288–303. [Google Scholar] [CrossRef]
- Waypa, G.B.; Schumacker, P.T. Hypoxia-induced changes in pulmonary and systemic vascular resistance: Where is the O2 sensor? Respir. Physiol. Neurobiol. 2010, 174, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Strielkov, I.; Pak, O.; Sommer, N.; Weissmann, N. Recent advances in oxygen sensing and signal transduction in hypoxic pulmonary vasoconstriction. J. Appl. Physiol. 2017, 123, 1647–1656. [Google Scholar] [CrossRef]
- Weissmann, N.; Akkayagil, E.; Quanz, K.; Schermuly, R.T.; Ghofrani, H.A.; Fink, L.; Hanze, J.; Rose, F.; Seeger, W.; Grimminger, F. Basic features of hypoxic pulmonary vasoconstriction in mice. Respir. Physiol. Neurobiol. 2004, 139, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Talbot, N.P.; Balanos, G.M.; Dorrington, K.L.; Robbins, P.A. Two temporal components within the human pulmonary vascular response to approximately 2 h of isocapnic hypoxia. J. Appl. Physiol. 2005, 98, 1125–1139. [Google Scholar] [CrossRef] [PubMed]
- Dorrington, K.L.; Clar, C.; Young, J.D.; Jonas, M.; Tansley, J.G.; Robbins, P.A. Time course of the human pulmonary vascular response to 8 hours of isocapnic hypoxia. Am. J. Physiol. 1997, 273 Pt 2, H1126–H1134. [Google Scholar] [CrossRef]
- Grover, R.F.; Vogel, J.H.; Averill, K.H.; Blount, S.G., Jr. Pulmonary hypertension. individual and species variability relative to vascular reactivity. Am. Heart J. 1963, 66, 1–3. [Google Scholar] [CrossRef]
- Westcott, R.N.; Fowler, N.O.; Scott, R.C.; Hauenstein, V.D.; Mc, G.J. Anoxia and human pulmonary vascular resistance. J. Clin. Investig. 1951, 30, 957–970. [Google Scholar] [CrossRef]
- Vogel, J.H.; Weaver, W.F.; Rose, R.L.; Blount, S.G., Jr.; Grover, R.F. Pulmonary hypertension on exertion in normal man living at 10,150 feet (Leadville, Colorado). Med. Thorac. 1962, 19, 461–477. [Google Scholar] [CrossRef]
- Jaenke, R.S.; Alexander, A.F. Fine structural alterations of bovine peripheral pulmonary arteries in hypoxia-induced hypertension. Am. J. Pathol. 1973, 73, 377–398. [Google Scholar] [PubMed]
- Boos, C.J.; Hodkinson, P.; Mellor, A.; Green, N.P.; Woods, D.R. The effects of acute hypobaric hypoxia on arterial stiffness and endothelial function and its relationship to changes in pulmonary artery pressure and left ventricular diastolic function. High Alt. Med. Biol. 2012, 13, 105–111. [Google Scholar] [CrossRef]
- Zhao, L.; Mason, N.A.; Morrell, N.W.; Kojonazarov, B.; Sadykov, A.; Maripov, A.; Mirrakhimov, M.M.; Aldashev, A.; Wilkins, M.R. Sildenafil inhibits hypoxia-induced pulmonary hypertension. Circulation 2001, 104, 424–428. [Google Scholar] [CrossRef]
- Beard, J.T., 2nd; Newman, J.H.; Loyd, J.E.; Byrd, B.F., 3rd. Doppler estimation of changes in pulmonary artery pressure during hypoxic breathing. J. Am. Soc. Echocardiogr. Off. Publ. Am. Soc. Echocardiogr. 1991, 4, 121–130. [Google Scholar] [CrossRef]
- Reichenberger, F.; Kohstall, M.G.; Seeger, T.; Olschewski, H.; Grimminger, F.; Seeger, W.; Ghofrani, H.A. Effect of sildenafil on hypoxia-induced changes in pulmonary circulation and right ventricular function. Respir. Physiol. Neurobiol. 2007, 159, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Mason, N.P.; Petersen, M.; Melot, C.; Imanow, B.; Matveykine, O.; Gautier, M.T.; Sarybaev, A.; Aldashev, A.; Mirrakhimov, M.M.; Brown, B.H.; et al. Serial changes in nasal potential difference and lung electrical impedance tomography at high altitude. J. Appl. Physiol. 2003, 94, 2043–2050. [Google Scholar] [CrossRef] [PubMed]
- Maggiorini, M.; Melot, C.; Pierre, S.; Pfeiffer, F.; Greve, I.; Sartori, C.; Lepori, M.; Hauser, M.; Scherrer, U.; Naeije, R. High-altitude pulmonary edema is initially caused by an increase in capillary pressure. Circulation 2001, 103, 2078–2083. [Google Scholar] [CrossRef] [PubMed]
- Kronenberg, R.S.; Safar, P.; Lee, J.; Wright, F.; Noble, W.; Wahrenbrock, E.; Hickey, R.; Nemoto, E.; Severinghaus, J.W. Pulmonary artery pressure and alveolar gas exchange in man during acclimatization to 12,470 ft. J. Clin. Investig. 1971, 50, 827–837. [Google Scholar] [CrossRef]
- Dubowitz, G.; Peacock, A.J. Pulmonary artery pressure in healthy subjects at 4250 m measured by Doppler echocardiography. Wilderness Environ. Med. 2007, 18, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Dehnert, C.; Grunig, E.; Mereles, D.; von Lennep, N.; Bartsch, P. Identification of individuals susceptible to high-altitude pulmonary oedema at low altitude. Eur. Respir. J. 2005, 25, 545–551. [Google Scholar] [CrossRef]
- Grunig, E.; Mereles, D.; Hildebrandt, W.; Swenson, E.R.; Kubler, W.; Kuecherer, H.; Bartsch, P. Stress Doppler echocardiography for identification of susceptibility to high altitude pulmonary edema. J. Am. Coll. Cardiol. 2000, 35, 980–987. [Google Scholar] [CrossRef]
- Scherrer, U.; Rimoldi, S.F.; Rexhaj, E.; Stuber, T.; Duplain, H.; Garcin, S.; de Marchi, S.F.; Nicod, P.; Germond, M.; Allemann, Y.; et al. Systemic and pulmonary vascular dysfunction in children conceived by assisted reproductive technologies. Circulation 2012, 125, 1890–1896. [Google Scholar] [CrossRef] [PubMed]
- von Arx, R.; Allemann, Y.; Sartori, C.; Rexhaj, E.; Cerny, D.; de Marchi, S.F.; Soria, R.; Germond, M.; Scherrer, U.; Rimoldi, S.F. Right ventricular dysfunction in children and adolescents conceived by assisted reproductive technologies. J. Appl. Physiol. 2015, 118, 1200–1206. [Google Scholar] [CrossRef]
- Sartori, C.; Allemann, Y.; Trueb, L.; Delabays, A.; Nicod, P.; Scherrer, U. Augmented vasoreactivity in adult life associated with perinatal vascular insult. Lancet 1999, 353, 2205–2207. [Google Scholar] [CrossRef]
- Balanos, G.M.; Pugh, K.; Frise, M.C.; Dorrington, K.L. Exaggerated pulmonary vascular response to acute hypoxia in older men. Exp. Physiol. 2015, 100, 1187–1198. [Google Scholar] [CrossRef]
- Fatemian, M.; Herigstad, M.; Croft, Q.P.; Formenti, F.; Cardenas, R.; Wheeler, C.; Smith, T.G.; Friedmannova, M.; Dorrington, K.L.; Robbins, P.A. Determinants of ventilation and pulmonary artery pressure during early acclimatization to hypoxia in humans. J. Physiol. 2016, 594, 1197–1213. [Google Scholar] [CrossRef]
- Boos, C.J.; Mellor, A.; O’Hara, J.P.; Tsakirides, C.; Woods, D.R. The effects of sex on cardiopulmonary responses to acute normobaric hypoxia. High Alt. Med. Biol. 2016, 17, 108–115. [Google Scholar] [CrossRef]
- Muza, S.R.; Beidleman, B.A.; Fulco, C.S. Altitude preexposure recommendations for inducing acclimatization. High Alt. Med. Biol. 2010, 11, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Foster, G.P.; Westerdahl, D.E.; Foster, L.A.; Hsu, J.V.; Anholm, J.D. Ischemic preconditioning of the lower extremity attenuates the normal hypoxic increase in pulmonary artery systolic pressure. Respir. Physiol. Neurobiol. 2011, 179, 248–253. [Google Scholar] [CrossRef]
- Foster, G.P.; Giri, P.C.; Rogers, D.M.; Larson, S.R.; Anholm, J.D. Ischemic preconditioning improves oxygen saturation and attenuates hypoxic pulmonary vasoconstriction at high altitude. High Alt. Med. Biol. 2014, 15, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.M.; Macholz, F.; Lehmann, L.; Dankl, D.; Hochreiter, M.; Bacher, B.; Bärtsch, P.; Mairbäurl, H. Remote ischemic preconditioning does not prevent acute mountain sickness after rapid ascent to 3450 m. J. Appl. Physiol. 2017, 123, 1228–1234. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Baggish, A.L.; Fulco, C.S.; Muza, S.; Rock, P.B.; Beidleman, B.; Cymerman, A.; Yared, K.; Fagenholz, P.; Systrom, D.; Wood, M.J.; et al. The impact of moderate-altitude staging on pulmonary arterial hemodynamics after ascent to high altitude. High Alt. Med. Biol. 2010, 11, 139–145. [Google Scholar] [CrossRef]
- Balanos, G.M.; Dorrington, K.L.; Robbins, P.A. Desferrioxamine elevates pulmonary vascular resistance in humans: Potential for involvement of HIF-1. J. Appl. Physiol. 2002, 92, 2501–2507. [Google Scholar] [CrossRef]
- Smith, T.G.; Balanos, G.M.; Croft, Q.P.; Talbot, N.P.; Dorrington, K.L.; Ratcliffe, P.J.; Robbins, P.A. The increase in pulmonary arterial pressure caused by hypoxia depends on iron status. J. Physiol. 2008, 586 Pt 24, 5999–6005. [Google Scholar] [CrossRef]
- Frise, M.C.; Cheng, H.Y.; Nickol, A.H.; Curtis, M.K.; Pollard, K.A.; Roberts, D.J.; Ratcliffe, P.J.; Dorrington, K.L.; Robbins, P.A. Clinical iron deficiency disturbs normal human responses to hypoxia. J. Clin. Investig. 2016, 126, 2139–2150. [Google Scholar] [CrossRef] [PubMed]
- Talbot, N.P.; Croft, Q.P.; Curtis, M.K.; Turner, B.E.; Dorrington, K.L.; Robbins, P.A.; Smith, T.G. Contrasting effects of ascorbate and iron on the pulmonary vascular response to hypoxia in humans. Physiol. Rep. 2014, 2, e12220. [Google Scholar] [CrossRef]
- Bart, N.K.; Curtis, M.K.; Cheng, H.Y.; Hungerford, S.L.; McLaren, R.; Petousi, N.; Dorrington, K.L.; Robbins, P.A. Elevation of iron storage in humans attenuates the pulmonary vascular response to hypoxia. J. Appl. Physiol. 2016, 121, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.G.; Talbot, N.P.; Privat, C.; Rivera-Ch, M.; Nickol, A.H.; Ratcliffe, P.J.; Dorrington, K.L.; Leon-Velarde, F.; Robbins, P.A. Effects of iron supplementation and depletion on hypoxic pulmonary hypertension: Two randomized controlled trials. JAMA J. Am. Med. Assoc. 2009, 302, 1444–1450. [Google Scholar] [CrossRef]
- Holdsworth, D.A.; Frise, M.C.; Bakker-Dyos, J.; Boos, C.; Dorrington, K.L.; Woods, D.; Mellor, A.; Robbins, P.A. Iron bioavailability and cardiopulmonary function during ascent to very high altitude. Eur. Respir. J. 2020, 56, 1902285. [Google Scholar] [CrossRef]
- Basnyat, B.; Murdoch, D.R. High-altitude illness. Lancet 2003, 361, 1967–1974. [Google Scholar] [CrossRef]
- Bartsch, P. High altitude pulmonary edema. Med. Sci. Sports Exerc. 1999, 31 (Suppl. 1), S23–S27. [Google Scholar] [CrossRef]
- West, J.B. The physiologic basis of high-altitude diseases. Ann. Intern. Med. 2004, 141, 789–800. [Google Scholar] [CrossRef]
- Bartsch, P.; Maggiorini, M.; Mairbaurl, H.; Vock, P.; Swenson, E.R. Pulmonary extravascular fluid accumulation in climbers. Lancet 2002, 360, 571–572. [Google Scholar] [CrossRef]
- Bartsch, P.; Mairbaurl, H.; Maggiorini, M.; Swenson, E.R. Physiological aspects of high-altitude pulmonary edema. J. Appl. Physiol. 2005, 98, 1101–1110. [Google Scholar] [CrossRef] [PubMed]
- Viswanathan, R.; Jain, S.K.; Subramanian, S.; Subramanian, T.A.; Dua, G.L.; Giri, J. Pulmonary edema of high altitude. II. Clinical, aerohemodynamic, and biochemical studies in a group with history of pulmonary edema of high altitude. Am. Rev. Respir. Dis. 1969, 100, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Hultgren, H.N.; Grover, R.F.; Hartley, L.H. Abnormal circulatory responses to high altitude in subjects with a previous history of high-altitude pulmonary edema. Circulation 1971, 44, 759–770. [Google Scholar] [CrossRef]
- Kawashima, A.; Kubo, K.; Kobayashi, T.; Sekiguchi, M. Hemodynamic responses to acute hypoxia, hypobaria, and exercise in subjects susceptible to high-altitude pulmonary edema. J. Appl. Physiol. 1989, 67, 1982–1989. [Google Scholar] [CrossRef]
- Yagi, H.; Yamada, H.; Kobayashi, T.; Sekiguchi, M. Doppler assessment of pulmonary hypertension induced by hypoxic breathing in subjects susceptible to high altitude pulmonary edema. Am. Rev. Respir. Dis. 1990, 142, 796–801. [Google Scholar] [CrossRef]
- Vachiery, J.L.; McDonagh, T.; Moraine, J.J.; Berre, J.; Naeije, R.; Dargie, H.; Peacock, A.J. Doppler assessment of hypoxic pulmonary vasoconstriction and susceptibility to high altitude pulmonary oedema. Thorax 1995, 50, 22–27. [Google Scholar] [CrossRef]
- Grunig, E.; Weissmann, S.; Ehlken, N.; Fijalkowska, A.; Fischer, C.; Fourme, T.; Galie, N.; Ghofrani, A.; Harrison, R.E.; Huez, S.; et al. Stress Doppler echocardiography in relatives of patients with idiopathic and familial pulmonary arterial hypertension: Results of a multicenter European analysis of pulmonary artery pressure response to exercise and hypoxia. Circulation 2009, 119, 1747–1757. [Google Scholar] [CrossRef] [PubMed]
- Hultgren, H.N.; Lopez, C.E.; Lundberg, E.; Miller, H. Physiologic studies of pulmonary edema at high altitude. Circulation 1964, 29, 393–408. [Google Scholar] [CrossRef]
- Penaloza, D.; Sime, F. Circulatory dynamics during high altitude pulmonary edema. Am. J. Cardiol. 1969, 23, 369–378. [Google Scholar] [CrossRef]
- Roy, S.B.; Guleria, J.S.; Khanna, P.K.; Manchanda, S.C.; Pande, J.N.; Subba, P.S. Haemodynamic studies in high altitude pulmonary oedema. Br. Heart J. 1969, 31, 52–58. [Google Scholar] [CrossRef]
- Scherrer, U.; Sartori, C.; Lepori, M.; Allemann, Y.; Duplain, H.; Trueb, L.; Nicod, P. High-altitude pulmonary edema: From exaggerated pulmonary hypertension to a defect in transepithelial sodium transport. Adv. Exp. Med. Biol. 1999, 474, 93–107. [Google Scholar]
- Hultgren, H.N.; Honigman, B.; Theis, K.; Nicholas, D. High-altitude pulmonary edema at a ski resort. West. J. Med. 1996, 164, 222–227. [Google Scholar] [PubMed]
- Bartsch, P.; Maggiorini, M.; Ritter, M.; Noti, C.; Vock, P.; Oelz, O. Prevention of high-altitude pulmonary edema by nifedipine. N. Engl. J. Med. 1991, 325, 1284–1289. [Google Scholar] [CrossRef] [PubMed]
- Maggiorini, M.; Brunner-La Rocca, H.P.; Peth, S.; Fischler, M.; Bohm, T.; Bernheim, A.; Kiencke, S.; Bloch, K.E.; Dehnert, C.; Naeije, R.; et al. Both tadalafil and dexamethasone may reduce the incidence of high-altitude pulmonary edema: A randomized trial. Ann. Intern. Med. 2006, 145, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Hackett, P.H.; Roach, R.C.; Hartig, G.S.; Greene, E.R.; Levine, B.D. The effect of vasodilators on pulmonary hemodynamics in high altitude pulmonary edema: A comparison. Int. J. Sports Med. 1992, 13 (Suppl. 1), S68–S71. [Google Scholar] [CrossRef]
- Oelz, O.; Maggiorini, M.; Ritter, M.; Waber, U.; Jenni, R.; Vock, P.; Bartsch, P. Nifedipine for high altitude pulmonary oedema. Lancet 1989, 2, 1241–1244. [Google Scholar] [CrossRef]
- Robertson, J.A.; Shlim, D.R. Treatment of Moderate Acute Mountain-Sickness with Pressurization in a Portable Hyperbaric (Gamow) Bag. J. Wilderness Med. 1991, 2, 268–273. [Google Scholar] [CrossRef]
- Bartsch, P. Treatment of high altitude diseases without drugs. Int. J. Sports Med. 1992, 13 (Suppl. 1), S71–S74. [Google Scholar] [CrossRef]
- Rios, B.; Driscoll, D.J.; McNamara, D.G. High-altitude pulmonary edema with absent right pulmonary artery. Pediatrics 1985, 75, 314–317. [Google Scholar]
- Schoene, R.B. Fatal high altitude pulmonary edema associated with absence of the left pulmonary artery. High Alt. Med. Biol. 2001, 2, 405–406. [Google Scholar] [CrossRef]
- Scherrer, U.; Turini, P.; Thalmann, S.; Hutter, D.; Salmon, C.S.; Stuber, T.; Shaw, S.; Jayet, P.Y.; Sartori-Cucchial, C.; Villena, M.; et al. Pulmonary hypertension in high-altitude dwellers: Novel mechanisms, unsuspected predisposing factors. Adv. Exp. Med. Biol. 2006, 588, 277–291. [Google Scholar]
- Durmowicz, A.G. Pulmonary edema in 6 children with Down syndrome during travel to moderate altitudes. Pediatrics 2001, 108, 443–447. [Google Scholar] [CrossRef]
- Hlastala, M.P.; Lamm, W.J.; Karp, A.; Polissar, N.L.; Starr, I.R.; Glenny, R.W. Spatial distribution of hypoxic pulmonary vasoconstriction in the supine pig. J. Appl. Physiol. 2004, 96, 1589–1599. [Google Scholar] [CrossRef] [PubMed]
- Lamm, W.J.; Starr, I.R.; Neradilek, B.; Polissar, N.L.; Glenny, R.W.; Hlastala, M.P. Hypoxic pulmonary vasoconstriction is heterogeneously distributed in the prone dog. Respir. Physiol. Neurobiol. 2004, 144, 281–294. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, S.R.; Garg, J.; Bolar, D.S.; Balouch, J.; Levin, D.L. Pulmonary blood flow heterogeneity during hypoxia and high-altitude pulmonary edema. Am. J. Respir. Crit. Care Med. 2005, 171, 83–87. [Google Scholar] [CrossRef] [PubMed]
- Viswanathan, R.; Subramanian, S.; Radha, T.G. Effect of hypoxia on regional lung perfusion, by scanning. Respiration 1979, 37, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Dehnert, C.; Risse, F.; Ley, S.; Kuder, T.A.; Buhmann, R.; Puderbach, M.; Menold, E.; Mereles, D.; Kauczor, H.U.; Bartsch, P.; et al. Magnetic resonance imaging of uneven pulmonary perfusion in hypoxia in humans. Am. J. Respir. Crit. Care Med. 2006, 174, 1132–1138. [Google Scholar] [CrossRef]
- Visscher, M.B. Studies on embolization of lung vessels. Med. Thorac. 1962, 19, 334–340. [Google Scholar] [CrossRef]
- Hyers, T.M.; Fowler, A.A.; Wicks, A.B. Focal pulmonary edema after massive pulmonary embolism. Am. Rev. Respir. Dis. 1981, 123, 232–233. [Google Scholar]
- West, J.B.; Tsukimoto, K.; Mathieu-Costello, O.; Prediletto, R. Stress failure in pulmonary capillaries. J. Appl. Physiol. 1991, 70, 1731–1742. [Google Scholar] [CrossRef]
- West, J.B.; Mathieu-Costello, O. High altitude pulmonary edema is caused by stress failure of pulmonary capillaries. Int. J. Sports Med. 1992, 13 (Suppl. 1), S54–S58. [Google Scholar] [CrossRef] [PubMed]
- West, J.B.; Colice, G.L.; Lee, Y.J.; Namba, Y.; Kurdak, S.S.; Fu, Z.; Ou, L.C.; Mathieu-Costello, O. Pathogenesis of high-altitude pulmonary oedema: Direct evidence of stress failure of pulmonary capillaries. Eur. Respir. J. 1995, 8, 523–529. [Google Scholar] [PubMed]
- Tsukimoto, K.; Mathieu-Costello, O.; Prediletto, R.; Elliott, A.R.; West, J.B. Ultrastructural appearances of pulmonary capillaries at high transmural pressures. J. Appl. Physiol. 1991, 71, 573–582. [Google Scholar] [CrossRef] [PubMed]
- Schoene, R.B.; Swenson, E.R.; Pizzo, C.J.; Hackett, P.H.; Roach, R.C.; Mills, W.J., Jr.; Henderson, W.R., Jr.; Martin, T.R. The lung at high altitude: Bronchoalveolar lavage in acute mountain sickness and pulmonary edema. J. Appl. Physiol. 1988, 64, 2605–2613. [Google Scholar] [CrossRef]
- Elliott, A.R.; Fu, Z.; Tsukimoto, K.; Prediletto, R.; Mathieu-Costello, O.; West, J.B. Short-term reversibility of ultrastructural changes in pulmonary capillaries caused by stress failure. J. Appl. Physiol. 1992, 73, 1150–1158. [Google Scholar] [CrossRef]
- Swenson, E.R.; Maggiorini, M.; Mongovin, S.; Gibbs, J.S.; Greve, I.; Mairbaurl, H.; Bartsch, P. Pathogenesis of high-altitude pulmonary edema: Inflammation is not an etiologic factor. JAMA J. Am. Med. Assoc. 2002, 287, 2228–2235. [Google Scholar] [CrossRef]
- Sartori, C.; Allemann, Y.; Trueb, L.; Lepori, M.; Maggiorini, M.; Nicod, P.; Scherrer, U. Exaggerated pulmonary hypertension is not sufficient to trigger high-altitude pulmonary oedema in humans. Schweiz. Med. Wochenschr. 2000, 130, 385–389. [Google Scholar] [PubMed]
- Dehnert, C.; Mereles, D.; Greiner, S.; Albers, D.; Scheurlen, F.; Zugel, S.; Bohm, T.; Vock, P.; Maggiorini, M.; Grunig, E.; et al. Exaggerated hypoxic pulmonary vasoconstriction without susceptibility to high altitude pulmonary edema. High Alt. Med. Biol. 2015, 16, 11–17. [Google Scholar] [CrossRef]
- Taylor, A.T. High-altitude illnesses: Physiology, risk factors, prevention, and treatment. Rambam Maimonides Med. J. 2011, 2, e0022. [Google Scholar] [CrossRef] [PubMed]
- Akunov, A.C.; Sartmyrzaeva, M.A.; Maripov, A.M.; Muratali Uulu, K.; Mamazhakypov, A.T.; Sydykov, A.S.; Sarybaev, A.S. High Altitude Pulmonary Edema in a Mining Worker With an Abnormal Rise in Pulmonary Artery Pressure in Response to Acute Hypoxia Without Prior History of High Altitude Pulmonary Edema. Wilderness Environ. Med. 2017, 28, 234–238. [Google Scholar] [CrossRef]
- Masud ul Hasan Nuri, M.; Khan, M.Z.; Quraishi, M.S. High altitude pulmonary oedema—Response to exercise and cold on systemic and pulmonary vascular beds. JPMA J. Pak. Med. Assoc. 1988, 38, 211–217. [Google Scholar] [PubMed]
- Sophocles, A.M., Jr. High-altitude pulmonary edema in Vail, Colorado, 1975–1982. West. J. Med. 1986, 144, 569–573. [Google Scholar]
- Luks, A.M.; McIntosh, S.E.; Grissom, C.K.; Auerbach, P.S.; Rodway, G.W.; Schoene, R.B.; Zafren, K.; Hackett, P.H. Wilderness Medical Society consensus guidelines for the prevention and treatment of acute altitude illness. Wilderness Environ. Med. 2010, 21, 146–155. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, S.R.; Schoene, R.B.; Henderson, W.R.; Spragg, R.G.; Martin, T.R.; West, J.B. Intense exercise impairs the integrity of the pulmonary blood-gas barrier in elite athletes. Am. J. Respir. Crit. Care Med. 1997, 155, 1090–1094. [Google Scholar] [CrossRef]
- Whitwell, K.E.; Greet, T.R. Collection and evaluation of tracheobronchial washes in the horse. Equine Vet. J. 1984, 16, 499–508. [Google Scholar] [CrossRef] [PubMed]
- McKechnie, J.K.; Leary, W.P.; Noakes, T.D.; Kallmeyer, J.C.; MacSearraigh, E.T.; Olivier, L.R. Acute pulmonary oedema in two athletes during a 90-km running race. S. Afr. Med. J. 1979, 56, 261–265. [Google Scholar] [PubMed]
- Bai, C.; She, J.; Goolaerts, A.; Song, Y.; Shen, C.; Shen, J.; Hong, Q. Stress failure plays a major role in the development of high-altitude pulmonary oedema in rats. Eur. Respir. J. 2010, 35, 584–591. [Google Scholar] [CrossRef]
- Bloch, K.E.; Turk, A.J.; Maggiorini, M.; Hess, T.; Merz, T.; Bosch, M.M.; Barthelmes, D.; Hefti, U.; Pichler, J.; Senn, O.; et al. Effect of ascent protocol on acute mountain sickness and success at Muztagh Ata, 7546 m. High Alt. Med. Biol. 2009, 10, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Beidleman, B.A.; Fulco, C.S.; Muza, S.R.; Rock, P.B.; Staab, J.E.; Forte, V.A.; Brothers, M.D.; Cymerman, A. Effect of six days of staging on physiologic adjustments and acute mountain sickness during ascent to 4300 meters. High Alt. Med. Biol. 2009, 10, 253–260. [Google Scholar] [CrossRef]
- Muza, S.R. Military applications of hypoxic training for high-altitude operations. Med. Sci. Sports Exerc. 2007, 39, 1625–1631. [Google Scholar] [CrossRef]
- Shaul, P.W.; Wells, L.B.; Horning, K.M. Acute and prolonged hypoxia attenuate endothelial nitric oxide production in rat pulmonary arteries by different mechanisms. J. Cardiovasc. Pharmacol. 1993, 22, 819–827. [Google Scholar] [CrossRef] [PubMed]
- Johns, R.A.; Linden, J.M.; Peach, M.J. Endothelium-dependent relaxation and cyclic GMP accumulation in rabbit pulmonary artery are selectively impaired by moderate hypoxia. Circ. Res. 1989, 65, 1508–1515. [Google Scholar] [CrossRef]
- Rodman, D.M.; Yamaguchi, T.; Hasunuma, K.; O’Brien, R.F.; McMurtry, I.F. Effects of hypoxia on endothelium-dependent relaxation of rat pulmonary artery. Am. J. Physiol. 1990, 258 Pt 1, L207–L214. [Google Scholar] [CrossRef]
- Blitzer, M.L.; Loh, E.; Roddy, M.A.; Stamler, J.S.; Creager, M.A. Endothelium-derived nitric oxide regulates systemic and pulmonary vascular resistance during acute hypoxia in humans. J. Am. Coll. Cardiol. 1996, 28, 591–596. [Google Scholar] [CrossRef]
- Frostell, C.; Fratacci, M.D.; Wain, J.C.; Jones, R.; Zapol, W.M. Inhaled nitric oxide. A selective pulmonary vasodilator reversing hypoxic pulmonary vasoconstriction. Circulation 1991, 83, 2038–2047. [Google Scholar] [CrossRef] [PubMed]
- Fagan, K.A.; Fouty, B.W.; Tyler, R.C.; Morris, K.G., Jr.; Hepler, L.K.; Sato, K.; LeCras, T.D.; Abman, S.H.; Weinberger, H.D.; Huang, P.L.; et al. The pulmonary circulation of homozygous or heterozygous eNOS-null mice is hyperresponsive to mild hypoxia. J. Clin. Investig. 1999, 103, 291–299. [Google Scholar] [CrossRef]
- Busch, T.; Bartsch, P.; Pappert, D.; Grunig, E.; Hildebrandt, W.; Elser, H.; Falke, K.J.; Swenson, E.R. Hypoxia decreases exhaled nitric oxide in mountaineers susceptible to high-altitude pulmonary edema. Am. J. Respir. Crit. Care Med. 2001, 163, 368–373. [Google Scholar] [CrossRef] [PubMed]
- Duplain, H.; Sartori, C.; Lepori, M.; Egli, M.; Allemann, Y.; Nicod, P.; Scherrer, U. Exhaled nitric oxide in high-altitude pulmonary edema: Role in the regulation of pulmonary vascular tone and evidence for a role against inflammation. Am. J. Respir. Crit. Care Med. 2000, 162, 221–224. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.M.; Dehnert, C.; Bailey, D.M.; Luks, A.M.; Menold, E.; Castell, C.; Schendler, G.; Faoro, V.; Mairbaurl, H.; Bartsch, P.; et al. Transpulmonary plasma ET-1 and nitrite differences in high altitude pulmonary hypertension. High Alt. Med. Biol. 2009, 10, 17–24. [Google Scholar] [CrossRef]
- Schneider, J.C.; Blazy, I.; Dechaux, M.; Rabier, D.; Mason, N.P.; Richalet, J.P. Response of nitric oxide pathway to L-arginine infusion at the altitude of 4350 m. Eur. Respir. J. 2001, 18, 286–292. [Google Scholar] [CrossRef]
- Bailey, D.M.; Dehnert, C.; Luks, A.M.; Menold, E.; Castell, C.; Schendler, G.; Faoro, V.; Gutowski, M.; Evans, K.A.; Taudorf, S.; et al. High-altitude pulmonary hypertension is associated with a free radical-mediated reduction in pulmonary nitric oxide bioavailability. J. Physiol. 2010, 588 Pt 23, 4837–4847. [Google Scholar] [CrossRef]
- Scherrer, U.; Vollenweider, L.; Delabays, A.; Savcic, M.; Eichenberger, U.; Kleger, G.R.; Fikrle, A.; Ballmer, P.E.; Nicod, P.; Bartsch, P. Inhaled nitric oxide for high-altitude pulmonary edema. N. Engl. J. Med. 1996, 334, 624–629. [Google Scholar] [CrossRef] [PubMed]
- Anand, I.S.; Prasad, B.A.; Chugh, S.S.; Rao, K.R.; Cornfield, D.N.; Milla, C.E.; Singh, N.; Singh, S.; Selvamurthy, W. Effects of inhaled nitric oxide and oxygen in high-altitude pulmonary edema. Circulation 1998, 98, 2441–2445. [Google Scholar] [CrossRef]
- Ghofrani, H.A.; Reichenberger, F.; Kohstall, M.G.; Mrosek, E.H.; Seeger, T.; Olschewski, H.; Seeger, W.; Grimminger, F. Sildenafil increased exercise capacity during hypoxia at low altitudes and at Mount Everest base camp: A randomized, double-blind, placebo-controlled crossover trial. Ann. Intern. Med. 2004, 141, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Ricart, A.; Maristany, J.; Fort, N.; Leal, C.; Pages, T.; Viscor, G. Effects of sildenafil on the human response to acute hypoxia and exercise. High Alt. Med. Biol. 2005, 6, 43–49. [Google Scholar] [CrossRef]
- Faoro, V.; Lamotte, M.; Deboeck, G.; Pavelescu, A.; Huez, S.; Guenard, H.; Martinot, J.B.; Naeije, R. Effects of sildenafil on exercise capacity in hypoxic normal subjects. High Alt. Med. Biol. 2007, 8, 155–163. [Google Scholar] [CrossRef]
- Richalet, J.P.; Gratadour, P.; Robach, P.; Pham, I.; Dechaux, M.; Joncquiert-Latarjet, A.; Mollard, P.; Brugniaux, J.; Cornolo, J. Sildenafil inhibits altitude-induced hypoxemia and pulmonary hypertension. Am. J. Respir. Crit. Care Med. 2005, 171, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Yanagisawa, M.; Kurihara, H.; Kimura, S.; Tomobe, Y.; Kobayashi, M.; Mitsui, Y.; Yazaki, Y.; Goto, K.; Masaki, T. A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature 1988, 332, 411–415. [Google Scholar] [CrossRef]
- Wiley, K.E.; Davenport, A.P. Nitric oxide-mediated modulation of the endothelin-1 signalling pathway in the human cardiovascular system. Br. J. Pharmacol. 2001, 132, 213–220. [Google Scholar] [CrossRef]
- Morganti, A.; Giussani, M.; Sala, C.; Gazzano, G.; Marana, I.; Pierini, A.; Savoia, M.T.; Ghio, F.; Cogo, A.; Zanchetti, A. Effects of exposure to high altitude on plasma endothelin-1 levels in normal subjects. J. Hypertens. 1995, 13, 859–865. [Google Scholar] [CrossRef]
- Goerre, S.; Wenk, M.; Bartsch, P.; Luscher, T.F.; Niroomand, F.; Hohenhaus, E.; Oelz, O.; Reinhart, W.H. Endothelin-1 in pulmonary hypertension associated with high-altitude exposure. Circulation 1995, 91, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Modesti, P.A.; Vanni, S.; Morabito, M.; Modesti, A.; Marchetta, M.; Gamberi, T.; Sofi, F.; Savia, G.; Mancia, G.; Gensini, G.F.; et al. Role of endothelin-1 in exposure to high altitude: Acute Mountain Sickness and Endothelin-1 (ACME-1) study. Circulation 2006, 114, 1410–1416. [Google Scholar] [CrossRef] [PubMed]
- Droma, Y.; Hayano, T.; Takabayashi, Y.; Koizumi, T.; Kubo, K.; Kobayashi, T.; Sekiguchi, M. Endothelin-1 and interleukin-8 in high altitude pulmonary oedema. Eur. Respir. J. 1996, 9, 1947–1949. [Google Scholar] [CrossRef] [PubMed]
- Sartori, C.; Vollenweider, L.; Loffler, B.M.; Delabays, A.; Nicod, P.; Bartsch, P.; Scherrer, U. Exaggerated endothelin release in high-altitude pulmonary edema. Circulation 1999, 99, 2665–2668. [Google Scholar] [CrossRef] [PubMed]
- Pham, I.; Wuerzner, G.; Richalet, J.P.; Peyrard, S.; Azizi, M. Endothelin receptors blockade blunts hypoxia-induced increase in PAP in humans. Eur. J. Clin. Investig. 2010, 40, 195–202. [Google Scholar] [CrossRef]
- Pham, I.; Wuerzner, G.; Richalet, J.P.; Peyrard, S.; Azizi, M. Bosentan effects in hypoxic pulmonary vasoconstriction: Preliminary study in subjects with or without high altitude pulmonary edema-history. Pulm. Circ. 2012, 2, 28–33. [Google Scholar] [CrossRef]
- Faoro, V.; Boldingh, S.; Moreels, M.; Martinez, S.; Lamotte, M.; Unger, P.; Brimioulle, S.; Huez, S.; Naeije, R. Bosentan decreases pulmonary vascular resistance and improves exercise capacity in acute hypoxia. Chest 2009, 135, 1215–1222. [Google Scholar] [CrossRef]
- Seheult, R.D.; Ruh, K.; Foster, G.P.; Anholm, J.D. Prophylactic bosentan does not improve exercise capacity or lower pulmonary artery systolic pressure at high altitude. Respir. Physiol. Neurobiol. 2009, 165, 123–130. [Google Scholar] [CrossRef]
- Naeije, R.; Huez, S.; Lamotte, M.; Retailleau, K.; Neupane, S.; Abramowicz, D.; Faoro, V. Pulmonary artery pressure limits exercise capacity at high altitude. Eur. Respir. J. 2010, 36, 1049–1055. [Google Scholar] [CrossRef]
- Murata, T.; Hori, M.; Sakamoto, K.; Karaki, H.; Ozaki, H. Dexamethasone blocks hypoxia-induced endothelial dysfunction in organ-cultured pulmonary arteries. Am. J. Respir. Crit. Care Med. 2004, 170, 647–655. [Google Scholar] [CrossRef]
- Stelzner, T.J.; O’Brien, R.F.; Sato, K.; Weil, J.V. Hypoxia-induced increases in pulmonary transvascular protein escape in rats. Modulation by glucocorticoids. J. Clin. Investig. 1988, 82, 1840–1847. [Google Scholar] [CrossRef]
- Noda, M.; Suzuki, S.; Tsubochi, H.; Sugita, M.; Maeda, S.; Kobayashi, S.; Kubo, H.; Kondo, T. Single dexamethasone injection increases alveolar fluid clearance in adult rats. Crit. Care Med. 2003, 31, 1183–1189. [Google Scholar] [CrossRef]
- Guney, S.; Schuler, A.; Ott, A.; Hoschele, S.; Zugel, S.; Baloglu, E.; Bartsch, P.; Mairbaurl, H. Dexamethasone prevents transport inhibition by hypoxia in rat lung and alveolar epithelial cells by stimulating activity and expression of Na+-K+-ATPase and epithelial Na+ channels. Am. J. Physiol. Lung Cell Mol. Physiol. 2007, 293, L1332–L1338. [Google Scholar] [CrossRef]
- Swenson, E.R. Carbonic anhydrase inhibitors and hypoxic pulmonary vasoconstriction. Respir. Physiol. Neurobiol. 2006, 151, 209–216. [Google Scholar] [CrossRef]
- Swenson, E.R. Carbonic anhydrase inhibitors and ventilation: A complex interplay of stimulation and suppression. Eur. Respir. J. 1998, 12, 1242–1247. [Google Scholar] [CrossRef] [PubMed]
- Teppema, L.J.; Balanos, G.M.; Steinback, C.D.; Brown, A.D.; Foster, G.E.; Duff, H.J.; Leigh, R.; Poulin, M.J. Effects of acetazolamide on ventilatory, cerebrovascular, and pulmonary vascular responses to hypoxia. Am. J. Respir. Crit. Care Med. 2007, 175, 277–281. [Google Scholar] [CrossRef] [PubMed]
- Hohne, C.; Pickerodt, P.A.; Francis, R.C.; Boemke, W.; Swenson, E.R. Pulmonary vasodilation by acetazolamide during hypoxia is unrelated to carbonic anhydrase inhibition. Am. J. Physiol. Lung Cell Mol. Physiol. 2007, 292, L178–L184. [Google Scholar] [CrossRef] [PubMed]
- Luks, A.M.; McIntosh, S.E.; Grissom, C.K.; Auerbach, P.S.; Rodway, G.W.; Schoene, R.B.; Zafren, K.; Hackett, P.H. Wilderness medical society practice guidelines for the prevention and treatment of acute altitude illness: 2014 update. Wilderness Environ. Med. 2014, 25 (Suppl. 4), S4–S14. [Google Scholar] [CrossRef]
- Fesler, P.; Pagnamenta, A.; Rondelet, B.; Kerbaul, F.; Naeije, R. Effects of sildenafil on hypoxic pulmonary vascular function in dogs. J. Appl. Physiol. 2006, 101, 1085–1090. [Google Scholar] [CrossRef]
- Omura, A.; Roy, R.; Jennings, T. Inhaled nitric oxide improves survival in the rat model of high-altitude pulmonary edema. Wilderness Environ. Med. 2000, 11, 251–256. [Google Scholar] [CrossRef]
- Roberts, J.D., Jr.; Chen, T.Y.; Kawai, N.; Wain, J.; Dupuy, P.; Shimouchi, A.; Bloch, K.; Polaner, D.; Zapol, W.M. Inhaled nitric oxide reverses pulmonary vasoconstriction in the hypoxic and acidotic newborn lamb. Circ. Res. 1993, 72, 246–254. [Google Scholar] [CrossRef]
- Chamorro, V.; Morales-Cano, D.; Milara, J.; Barreira, B.; Moreno, L.; Callejo, M.; Mondejar-Parreño, G.; Esquivel-Ruiz, S.; Cortijo, J.; Cogolludo, Á.; et al. Riociguat versus sildenafil on hypoxic pulmonary vasoconstriction and ventilation/perfusion matching. PLoS ONE 2018, 13, e0191239. [Google Scholar] [CrossRef]
- Preston, I.R.; Hill, N.S.; Gambardella, L.S.; Warburton, R.R.; Klinger, J.R. Synergistic effects of ANP and sildenafil on cGMP levels and amelioration of acute hypoxic pulmonary hypertension. Exp. Biol. Med. 2004, 229, 920–925. [Google Scholar] [CrossRef]
- Tsai, B.M.; Turrentine, M.W.; Sheridan, B.C.; Wang, M.; Fiore, A.C.; Brown, J.W.; Meldrum, D.R. Differential effects of phosphodiesterase-5 inhibitors on hypoxic pulmonary vasoconstriction and pulmonary artery cytokine expression. Ann. Thorac. Surg. 2006, 81, 272–278. [Google Scholar] [CrossRef]
- Rashid, M.; Kotwani, A.; Fahim, M. Long-acting phosphodiesterase 5 inhibitor, tadalafil, and superoxide dismutase mimetic, tempol, protect against acute hypoxia-induced pulmonary hypertension in rats. Hum. Exp. Toxicol. 2012, 31, 626–636. [Google Scholar] [CrossRef] [PubMed]
- Goirand, F.; Bardou, M.; Guerard, P.; Dumas, J.P.; Rochette, L.; Dumas, M. ETA, mixed ETA/ETB receptor antagonists, and protein kinase C inhibitor prevent acute hypoxic pulmonary vasoconstriction: Influence of potassium channels. J. Cardiovasc. Pharmacol. 2003, 41, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.J.; Chen, Y.F.; Meng, Q.C.; Durand, J.; Dicarlo, V.S.; Oparil, S. Endothelin-receptor antagonist bosentan prevents and reverses hypoxic pulmonary hypertension in rats. J. Appl. Physiol. 1995, 79, 2122–2231. [Google Scholar] [CrossRef]
- Redding, G.J.; Tuck, R.; Escourrou, P. Nifedipine attenuates acute hypoxic pulmonary vasoconstriction in awake piglets. Am. Rev. Respir. Dis. 1984, 129, 785–789. [Google Scholar] [CrossRef] [PubMed]
- Hohne, C.; Krebs, M.O.; Seiferheld, M.; Boemke, W.; Kaczmarczyk, G.; Swenson, E.R. Acetazolamide prevents hypoxic pulmonary vasoconstriction in conscious dogs. J. Appl. Physiol. 2004, 97, 515–521. [Google Scholar] [CrossRef]
- Shimoda, L.A.; Luke, T.; Sylvester, J.T.; Shih, H.W.; Jain, A.; Swenson, E.R. Inhibition of hypoxia-induced calcium responses in pulmonary arterial smooth muscle by acetazolamide is independent of carbonic anhydrase inhibition. Am. J. Physiol. Lung Cell Mol. Physiol. 2007, 292, L1002–L1012. [Google Scholar] [CrossRef]
- Pavelescu, A.; Naeije, R. Effects of epoprostenol and sildenafil on right ventricular function in hypoxic volunteers: A tissue Doppler imaging study. Eur. J. Appl. Physiol. 2012, 112, 1285–1294. [Google Scholar] [CrossRef]
- de Bisschop, C.; Martinot, J.B.; Leurquin-Sterk, G.; Faoro, V.; Guénard, H.; Naeije, R. Improvement in lung diffusion by endothelin A receptor blockade at high altitude. J. Appl. Physiol. 2012, 112, 20–25. [Google Scholar] [CrossRef]
- Lichtblau, M.; Furian, M.; Aeschbacher, S.S.; Bisang, M.; Ulrich, S.; Saxer, S.; Sheraliev, U.; Marazhapov, N.H.; Osmonov, B.; Estebesova, B.; et al. Dexamethasone improves pulmonary hemodynamics in COPD-patients going to altitude: A randomized trial. Int. J. Cardiol. 2019, 283, 159–164. [Google Scholar] [CrossRef]
- Fischler, M.; Maggiorini, M.; Dorschner, L.; Debrunner, J.; Bernheim, A.; Kiencke, S.; Mairbäurl, H.; Bloch, K.E.; Naeije, R.; Brunner-La Rocca, H.P. Dexamethasone but not tadalafil improves exercise capacity in adults prone to high-altitude pulmonary edema. Am. J. Respir. Crit. Care Med. 2009, 180, 346–352. [Google Scholar] [CrossRef]
- Zafren, K.; Reeves, J.T.; Schoene, R. Treatment of high-altitude pulmonary edema by bed rest and supplemental oxygen. Wilderness Environ. Med. 1996, 7, 127–132. [Google Scholar] [CrossRef]
- Marticorena, E.; Hultgren, H.N. Evaluation of therapeutic methods in high altitude pulmonary edema. Am. J. Cardiol. 1979, 43, 307–312. [Google Scholar] [CrossRef]
- Luks, A.M.; Auerbach, P.S.; Freer, L.; Grissom, C.K.; Keyes, L.E.; McIntosh, S.E.; Rodway, G.W.; Schoene, R.B.; Zafren, K.; Hackett, P.H. Wilderness Medical Society Clinical Practice Guidelines for the Prevention and Treatment of Acute Altitude Illness: 2019 Update. Wilderness Environ. Med. 2019, 30, S3–S18. [Google Scholar] [CrossRef] [PubMed]
- Freeman, K.; Shalit, M.; Stroh, G. Use of the Gamow Bag by EMT-basic park rangers for treatment of high-altitude pulmonary edema and high-altitude cerebral edema. Wilderness Environ. Med. 2004, 15, 198–201. [Google Scholar] [CrossRef]
- Taber, R.L. Protocols for the use of a portable hyperbaric chamber for the treatment of high altitude disorders. J. Wilderness Med. 1990, 1, 181–192. [Google Scholar] [CrossRef]
- Frostell, C.G.; Blomqvist, H.; Hedenstierna, G.; Lundberg, J.; Zapol, W.M. Inhaled nitric oxide selectively reverses human hypoxic pulmonary vasoconstriction without causing systemic vasodilation. Anesthesiology 1993, 78, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Fagenholz, P.J.; Gutman, J.A.; Murray, A.F.; Harris, N.S. Treatment of high altitude pulmonary edema at 4240 m in Nepal. High Alt. Med. Biol. 2007, 8, 139–146. [Google Scholar] [CrossRef]
- Jones, B.E.; Stokes, S.; McKenzie, S.; Nilles, E.; Stoddard, G.J. Management of high altitude pulmonary edema in the Himalaya: A review of 56 cases presenting at Pheriche medical aid post (4240 m). Wilderness Environ. Med. 2013, 24, 32–36. [Google Scholar] [CrossRef]
- Davis, C.; Hackett, P. Advances in the Prevention and Treatment of High Altitude Illness. Emerg. Med. Clin. N. Am. 2017, 35, 241–260. [Google Scholar] [CrossRef]
- Deshwal, R.; Iqbal, M.; Basnet, S. Nifedipine for the treatment of high altitude pulmonary edema. Wilderness Environ. Med. 2012, 23, 7–10. [Google Scholar] [CrossRef]
- Joyce, K.E.; Lucas, S.J.E.; Imray, C.H.E.; Balanos, G.M.; Wright, A.D. Advances in the available non-biological pharmacotherapy prevention and treatment of acute mountain sickness and high altitude cerebral and pulmonary oedema. Expert Opin. Pharmacother. 2018, 19, 1891–1902. [Google Scholar] [CrossRef]
- Groves, B.M.; Reeves, J.T.; Sutton, J.R.; Wagner, P.D.; Cymerman, A.; Malconian, M.K.; Rock, P.B.; Young, P.M.; Houston, C.S. Operation Everest II: Elevated high-altitude pulmonary resistance unresponsive to oxygen. J. Appl. Physiol. 1987, 63, 521–530. [Google Scholar] [CrossRef] [PubMed]
- Luks, A.M.; Levett, D.; Martin, D.S.; Goss, C.H.; Mitchell, K.; Fernandez, B.O.; Feelisch, M.; Grocott, M.P.; Swenson, E.R. Changes in acute pulmonary vascular responsiveness to hypoxia during a progressive ascent to high altitude (5300 m). Exp. Physiol. 2017, 102, 711–724. [Google Scholar] [CrossRef] [PubMed]
- Hilty, M.P.; Müller, A.; Flück, D.; Siebenmann, C.; Rasmussen, P.; Keiser, S.; Auinger, K.; Lundby, C.; Maggiorini, M. Effect of increased blood flow on pulmonary circulation before and during high altitude acclimatization. High Alt. Med. Biol. 2016, 17, 305–314. [Google Scholar] [CrossRef]
- Kosanovic, D.; Platzek, S.M.; Petrovic, A.; Sydykov, A.; Maripov, A.; Mamazhakypov, A.; Sartmyrzaeva, M.; Muratali Uulu, K.; Cholponbaeva, M.; Toktosunova, A.; et al. Circulating Apoptotic Signals During Acute and Chronic Exposure to High Altitude in Kyrgyz Population. Front. Physiol. 2019, 10, 54. [Google Scholar] [CrossRef]
- Yang, T.; Li, X.; Qin, J.; Li, S.; Yu, J.; Zhang, J.; Yu, S.; Wu, X.; Huang, L. High altitude-induced borderline pulmonary hypertension impaired cardiorespiratory fitness in healthy young men. Int. J. Cardiol. 2015, 181, 382–388. [Google Scholar] [CrossRef] [PubMed]
- Faoro, V.; Huez, S.; Vanderpool, R.; Groepenhoff, H.; de Bisschop, C.; Martinot, J.B.; Lamotte, M.; Pavelescu, A.; Guenard, H.; Naeije, R. Pulmonary circulation and gas exchange at exercise in Sherpas at high altitude. J. Appl. Physiol. 2014, 116, 919–926. [Google Scholar] [CrossRef] [PubMed]
- Foster, G.E.; Ainslie, P.N.; Stembridge, M.; Day, T.A.; Bakker, A.; Lucas, S.J.; Lewis, N.C.; MacLeod, D.B.; Lovering, A.T. Resting pulmonary haemodynamics and shunting: A comparison of sea-level inhabitants to high altitude Sherpas. J. Physiol. 2014, 592 Pt 6, 1397–1409. [Google Scholar] [CrossRef]
- Schwab, M.; Jayet, P.Y.; Stuber, T.; Salinas, C.E.; Bloch, J.; Spielvogel, H.; Villena, M.; Allemann, Y.; Sartori, C.; Scherrer, U. Pulmonary-artery pressure and exhaled nitric oxide in Bolivian and Caucasian high altitude dwellers. High Alt. Med. Biol. 2008, 9, 295–299. [Google Scholar] [CrossRef]
- Singh, I.; Khanna, P.K.; Lal, M.; Hoon, R.S.; Rao, B.D. High-altitude pulmonary hypertension. Lancet 1965, 1, 146–150. [Google Scholar] [CrossRef]
- Sui, G.J.; Liu, Y.H.; Cheng, X.S.; Anand, I.S.; Harris, E.; Harris, P.; Heath, D. Subacute infantile mountain sickness. J. Pathol. 1988, 155, 161–170. [Google Scholar] [CrossRef]
- Wu, T.; Miao, C. High altitude heart disease in children in Tibet. High Alt. Med. Biol. 2002, 3, 323–325. [Google Scholar] [CrossRef]
- Muratali Uulu, K.; Cholponbaeva, M.; Duishobaev, M.; Toktosunova, A.; Maripov, A.; Sydykov, A.; Sarybaev, A. A Case of Subacute Infantile Mountain Sickness in a Kyrgyz Child. High Alt. Med. Biol. 2018, 19, 208–210. [Google Scholar] [CrossRef] [PubMed]
- Heath, D.; Harris, P.; Sui, G.J.; Liu, Y.H.; Gosney, J.; Harris, E.; Anand, I.S. Pulmonary blood vessels and endocrine cells in subacute infantile mountain sickness. Respir. Med. 1989, 83, 77–81. [Google Scholar] [CrossRef]
- Anand, I.S.; Wu, T. Syndromes of subacute mountain sickness. High Alt. Med. Biol. 2004, 5, 156–170. [Google Scholar] [CrossRef]
- Anand, I.S. Hypoxia and the pulmonary circulation. Thorax 1994, 49, S19–S24. [Google Scholar] [CrossRef] [PubMed]
- Poduval, R.G. Adult subacute mountain sickness--a syndrome at extremes of high altitude. J. Assoc. Physicians India 2000, 48, 511–513. [Google Scholar] [PubMed]
- Anand, I.S.; Malhotra, R.M.; Chandrashekhar, Y.; Bali, H.K.; Chauhan, S.S.; Jindal, S.K.; Bhandari, R.K.; Wahi, P.L. Adult subacute mountain sickness—A syndrome of congestive heart failure in man at very high altitude. Lancet 1990, 335, 561–565. [Google Scholar] [CrossRef]
- Canepa, A.; Chavez, R.; Hurtado, A.; Rotta, A.; Velasquez, T. Pulmonary circulation at sea level and at high altitudes. J. Appl. Physiol. 1956, 9, 328–336. [Google Scholar]
- Sime, F.; Banchero, N.; Penaloza, D.; Gamboa, R.; Cruz, J.; Marticorena, E. Pulmonary hypertension in children born and living at high altitudes. Am. J. Cardiol. 1963, 11, 143–149. [Google Scholar] [CrossRef]
- Peñaloza, D.; Sime, F.; Banchero, N.; Gamboa, R.; Cruz, J.; Marticorena, E. Pulmonary hypertension in healthy men born and living at high altitudes. Am. J. Cardiol. 1963, 11, 150–157. [Google Scholar] [CrossRef]
- Arias-Stella, J.; Saldana, M. The muscular pulmonary arteries in people native to high altitude. Med. Thorac. 1962, 19, 484–493. [Google Scholar] [CrossRef]
- Rowan, S.C.; McLoughlin, P. Hypoxic pulmonary hypertension: The paradigm is changing. Exp. Physiol. 2014, 99, 837–838. [Google Scholar] [CrossRef]
- Cahill, E.; Rowan, S.C.; Sands, M.; Banahan, M.; Ryan, D.; Howell, K.; McLoughlin, P. The pathophysiological basis of chronic hypoxic pulmonary hypertension in the mouse: Vasoconstrictor and structural mechanisms contribute equally. Exp. Physiol. 2012, 97, 796–806. [Google Scholar] [CrossRef] [PubMed]
- van Suylen, R.J.; Smits, J.F.; Daemen, M.J. Pulmonary artery remodeling differs in hypoxia- and monocrotaline-induced pulmonary hypertension. Am. J. Respir. Crit. Care Med. 1998, 157 Pt 1, 1423–1428. [Google Scholar] [CrossRef]
- Hyvelin, J.M.; Howell, K.; Nichol, A.; Costello, C.M.; Preston, R.J.; McLoughlin, P. Inhibition of Rho-kinase attenuates hypoxia-induced angiogenesis in the pulmonary circulation. Circ. Res. 2005, 97, 185–191. [Google Scholar] [CrossRef]
- Will, D.H.; Alexander, A.F.; Reeves, J.T.; Grover, R.F. High altitude-induced pulmonary hypertension in normal cattle. Circ. Res. 1962, 10, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jibaja, J.; Banchero, N.; Sime, F.; Penaloza, D.; Gamboa, R.; Marticorena, E. Correlation between pulmonary artery pressure and level of altitude. Dis. Chest 1964, 46, 446–451. [Google Scholar] [CrossRef] [PubMed]
- De Micheli, A.; Villacis, E.; Guzzydela Mora, P.; Rubio Alvarez, V. Observations on the hemodynamic and respiratory measurements obtained in normal subjects. Arch. Del Inst. De Cardiol. De Mex. 1960, 30, 507–520. [Google Scholar]
- Ordonez, J.H. Physiological observations in residents of Bogota, Colombia, altitude 8700 feet. Rocky Mt. Med. J. 1969, 66, 33–36. [Google Scholar]
- Grover, R.F. Chronic hypoxic pulmonary hypertension. In The Pulmonary Circulation: Normal and Abnormal: Mechanisms, Management, and the National Registry; Fishman, A.P., Ed.; University of Pennsylvania Press: Philadelphia, PA, USA, 1990; pp. 283–299. [Google Scholar]
- Soria, R.; Egger, M.; Scherrer, U.; Bender, N.; Rimoldi, S.F. Pulmonary artery pressure and arterial oxygen saturation in people living at high or low altitude: Systematic review and meta-analysis. J. Appl. Physiol. 2016, 121, 1151–1159. [Google Scholar] [CrossRef] [PubMed]
- Banchero, N.; Sime, F.; Penaloza, D.; Cruz, J.; Gamboa, R.; Marticorena, E. Pulmonary pressure, cardiac output, and arterial oxygen saturation during exercise at high altitude and at sea level. Circulation 1966, 33, 249–262. [Google Scholar] [CrossRef]
- Antezana, A.M.; Antezana, G.; Aparicio, O.; Noriega, I.; Velarde, F.L.; Richalet, J.P. Pulmonary hypertension in high-altitude chronic hypoxia: Response to nifedipine. Eur. Respir. J. 1998, 12, 1181–1185. [Google Scholar] [CrossRef]
- Heath, D.; Smith, P.; Rios Dalenz, J.; Williams, D.; Harris, P. Small pulmonary arteries in some natives of La Paz, Bolivia. Thorax 1981, 36, 599–604. [Google Scholar] [CrossRef]
- Wagenvoort, C.A.; Wagenvoort, N. Hypoxic pulmonary vascular lesions in man at high altitude and in patients with chronic respiratory disease. Pathol. Et Microbiol. 1973, 39, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Gupta, M.L.; Rao, K.S.; Anand, I.S.; Banerjee, A.K.; Boparai, M.S. Lack of smooth muscle in the small pulmonary arteries of the native Ladakhi. Is the Himalayan highlander adapted? Am. Rev. Respir. Dis. 1992, 145, 1201–1204. [Google Scholar] [CrossRef]
- Heath, D.; Williams, D.; Rios-Dalenz, J.; Calderon, M.; Gosney, J. Small pulmonary arterial vessels of Aymara Indians from the Bolivian Andes. Histopathology 1990, 16, 565–571. [Google Scholar] [CrossRef]
- Wagenvoort, C.A. Pathology of Pulmonary Hypertension; Wiley: New York, NY, USA, 1977. [Google Scholar]
- Durmowicz, A.G.; Hofmeister, S.; Kadyraliev, T.K.; Aldashev, A.A.; Stenmark, K.R. Functional and structural adaptation of the yak pulmonary circulation to residence at high altitude. J. Appl. Physiol. 1993, 74, 2276–2285. [Google Scholar] [CrossRef]
- Kadyraliev, T.K. The morphological changes in the pulmonary resistive vessels in the development of high-altitude pulmonary arterial hypertension. Arkhiv Patol. 1990, 52, 36–40. [Google Scholar]
- Kadyraliev, T.K.; Mirrakhimov, M.M. Functional morphology of resistant pulmonary vessels and capillaries in individual and species adaptation to high altitude. Biulleten ‘Eksperimental’noi Biol. I Meditsiny 1992, 114, 100–104. [Google Scholar]
- Heath, D.; Castillo, Y.; Arias-Stella, J.; Harris, P. The small pulmonary arteries of the llama and other domestic animals native to high altitudes. Cardiovasc. Res. 1969, 3, 75–78. [Google Scholar] [CrossRef]
- Heath, D.; Smith, P.; Williams, D.; Harris, P.; Arias-Stella, J.; Kruger, H. The heart and pulmonary vasculature of the llama (Lama glama). Thorax 1974, 29, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Groves, B.M.; Droma, T.; Sutton, J.R.; McCullough, R.G.; McCullough, R.E.; Zhuang, J.; Rapmund, G.; Sun, S.; Janes, C.; Moore, L.G. Minimal hypoxic pulmonary hypertension in normal Tibetans at 3,658 m. J. Appl. Physiol. 1993, 74, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Roy, S.B.; Sciences, A.-I.I.O.M.; Services, I.A.F.M.; Research, I.C.O.M. Circulatory and Ventilatory Effects of High Altitude-Acclimatization and Deacclimatization of Indian Soldiers: A Prospective Study, 1964–1972; Indian Council of Medical Research: New-Delhi, India, 1972.
- Pang, Y.; Ma, R.Y.; Qi, H.Y.; Sun, K. Comparitive study of the indexes of pulmonary arterial pressure of healthy children at different altitudes by Doppler echocardiography. Zhonghua Er Ke Za Zhi/Chin. J. Pediatr. 2004, 42, 595–599. [Google Scholar]
- Hoit, B.D.; Dalton, N.D.; Erzurum, S.C.; Laskowski, D.; Strohl, K.P.; Beall, C.M. Nitric oxide and cardiopulmonary hemodynamics in Tibetan highlanders. J. Appl. Physiol. 2005, 99, 1796–1801. [Google Scholar] [CrossRef] [PubMed]
- Huez, S.; Faoro, V.; Guenard, H.; Martinot, J.B.; Naeije, R. Echocardiographic and tissue Doppler imaging of cardiac adaptation to high altitude in native highlanders versus acclimatized lowlanders. Am. J. Cardiol. 2009, 103, 1605–1609. [Google Scholar] [CrossRef]
- Maignan, M.; Rivera-Ch, M.; Privat, C.; Leon-Velarde, F.; Richalet, J.P.; Pham, I. Pulmonary pressure and cardiac function in chronic mountain sickness patients. Chest 2009, 135, 499–504. [Google Scholar] [CrossRef]
- Petousi, N.; Croft, Q.P.; Cavalleri, G.L.; Cheng, H.Y.; Formenti, F.; Ishida, K.; Lunn, D.; McCormack, M.; Shianna, K.V.; Talbot, N.P.; et al. Tibetans living at sea level have a hyporesponsive hypoxia-inducible factor system and blunted physiological responses to hypoxia. J. Appl. Physiol. 2014, 116, 893–904. [Google Scholar] [CrossRef]
- Beall, C.M.; Laskowski, D.; Strohl, K.P.; Soria, R.; Villena, M.; Vargas, E.; Alarcon, A.M.; Gonzales, C.; Erzurum, S.C. Pulmonary nitric oxide in mountain dwellers. Nature 2001, 414, 411–412. [Google Scholar] [CrossRef] [PubMed]
- Erzurum, S.C.; Ghosh, S.; Janocha, A.J.; Xu, W.; Bauer, S.; Bryan, N.S.; Tejero, J.; Hemann, C.; Hille, R.; Stuehr, D.J.; et al. Higher blood flow and circulating NO products offset high-altitude hypoxia among Tibetans. Proc. Natl. Acad. Sci. USA 2007, 104, 17593–17598. [Google Scholar] [CrossRef] [PubMed]
- Maripov, A.; Mamazhakypov, A.; Karagulova, G.; Sydykov, A.; Sarybaev, A. High altitude pulmonary hypertension with severe right ventricular dysfunction. Int. J. Cardiol. 2013, 168, e89–e90. [Google Scholar] [CrossRef]
- Villafuerte, F.C.; Corante, N. Chronic Mountain Sickness: Clinical Aspects, Etiology, Management, and Treatment. High Alt. Med. Biol. 2016, 17, 61–69. [Google Scholar] [CrossRef] [PubMed]
- De Ferrari, A.; Miranda, J.J.; Gilman, R.H.; Dávila-Román, V.G.; León-Velarde, F.; Rivera-Ch, M.; Huicho, L.; Bernabé-Ortiz, A.; Wise, R.A.; Checkley, W. Prevalence, clinical profile, iron status, and subject-specific traits for excessive erythrocytosis in andean adults living permanently at 3,825 meters above sea level. Chest 2014, 146, 1327–1336. [Google Scholar] [CrossRef]
- Leon-Velarde, F.; Ramos, M.A.; Hernandez, J.A.; De Idiaquez, D.; Munoz, L.S.; Gaffo, A.; Cordova, S.; Durand, D.; Monge, C. The role of menopause in the development of chronic mountain sickness. Am. J. Physiol. 1997, 272 Pt 2, R90–R94. [Google Scholar] [CrossRef]
- Gou, Q.; Shi, R.; Zhang, X.; Meng, Q.; Li, X.; Rong, X.; Gawa, Z.; Zhuoma, N.; Chen, X. The Prevalence and Risk Factors of High-Altitude Pulmonary Hypertension Among Native Tibetans in Sichuan Province, China. High Alt. Med. Biol. 2020, 21, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Semenza, G.L. Regulation of oxygen homeostasis by hypoxia-inducible factor 1. Physiology 2009, 24, 97–106. [Google Scholar] [CrossRef]
- Salceda, S.; Caro, J. Hypoxia-inducible factor 1alpha (HIF-1alpha) protein is rapidly degraded by the ubiquitin-proteasome system under normoxic conditions. Its stabilization by hypoxia depends on redox-induced changes. J. Biol. Chem. 1997, 272, 22642–22647. [Google Scholar] [CrossRef]
- Semenza, G.L. The Genomics and Genetics of Oxygen Homeostasis. Annu. Rev. Genom. Hum. Genet. 2020, 21, 183–204. [Google Scholar] [CrossRef]
- Gale, D.P.; Harten, S.K.; Reid, C.D.; Tuddenham, E.G.; Maxwell, P.H. Autosomal dominant erythrocytosis and pulmonary arterial hypertension associated with an activating HIF2 alpha mutation. Blood 2008, 112, 919–921. [Google Scholar] [CrossRef]
- Formenti, F.; Beer, P.A.; Croft, Q.P.; Dorrington, K.L.; Gale, D.P.; Lappin, T.R.; Lucas, G.S.; Maher, E.R.; Maxwell, P.H.; McMullin, M.F.; et al. Cardiopulmonary function in two human disorders of the hypoxia-inducible factor (HIF) pathway: Von Hippel-Lindau disease and HIF-2alpha gain-of-function mutation. Faseb J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2011, 25, 2001–2011. [Google Scholar] [CrossRef]
- Talbot, N.P.; Smith, T.G.; Balanos, G.M.; Dorrington, K.L.; Maxwell, P.H.; Robbins, P.A. Cardiopulmonary phenotype associated with human PHD2 mutation. Physiol. Rep. 2017, 5, e13224. [Google Scholar] [CrossRef] [PubMed]
- Sergeyeva, A.; Gordeuk, V.R.; Tokarev, Y.N.; Sokol, L.; Prchal, J.F.; Prchal, J.T. Congenital polycythemia in Chuvashia. Blood 1997, 89, 2148–2154. [Google Scholar] [CrossRef] [PubMed]
- Ang, S.O.; Chen, H.; Gordeuk, V.R.; Sergueeva, A.I.; Polyakova, L.A.; Miasnikova, G.Y.; Kralovics, R.; Stockton, D.W.; Prchal, J.T. Endemic polycythemia in Russia: Mutation in the VHL gene. Blood Cells Mol. Dis. 2002, 28, 57–62. [Google Scholar] [CrossRef]
- Ang, S.O.; Chen, H.; Hirota, K.; Gordeuk, V.R.; Jelinek, J.; Guan, Y.; Liu, E.; Sergueeva, A.I.; Miasnikova, G.Y.; Mole, D.; et al. Disruption of oxygen homeostasis underlies congenital Chuvash polycythemia. Nat. Genet. 2002, 32, 614–621. [Google Scholar] [CrossRef]
- Perrotta, S.; Nobili, B.; Ferraro, M.; Migliaccio, C.; Borriello, A.; Cucciolla, V.; Martinelli, V.; Rossi, F.; Punzo, F.; Cirillo, P.; et al. Von Hippel-Lindau-dependent polycythemia is endemic on the island of Ischia: Identification of a novel cluster. Blood 2006, 107, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Gordeuk, V.R.; Prchal, J.T. Vascular complications in Chuvash polycythemia. Semin. Thromb. Hemost. 2006, 32, 289–294. [Google Scholar] [CrossRef]
- Bushuev, V.I.; Miasnikova, G.Y.; Sergueeva, A.I.; Polyakova, L.A.; Okhotin, D.; Gaskin, P.R.; Debebe, Z.; Nekhai, S.; Castro, O.L.; Prchal, J.T.; et al. Endothelin-1, vascular endothelial growth factor and systolic pulmonary artery pressure in patients with Chuvash polycythemia. Haematologica 2006, 91, 744–749. [Google Scholar]
- Sable, C.A.; Aliyu, Z.Y.; Dham, N.; Nouraie, M.; Sachdev, V.; Sidenko, S.; Miasnikova, G.Y.; Polyakova, L.A.; Sergueeva, A.I.; Okhotin, D.J.; et al. Pulmonary artery pressure and iron deficiency in patients with upregulation of hypoxia sensing due to homozygous VHL(R200W) mutation (Chuvash polycythemia). Haematologica 2012, 97, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Bond, J.; Gale, D.P.; Connor, T.; Adams, S.; de Boer, J.; Gascoyne, D.M.; Williams, O.; Maxwell, P.H.; Ancliff, P.J. Dysregulation of the HIF pathway due to VHL mutation causing severe erythrocytosis and pulmonary arterial hypertension. Blood 2011, 117, 3699–3701. [Google Scholar] [CrossRef] [PubMed]
- Sarangi, S.; Lanikova, L.; Kapralova, K.; Acharya, S.; Swierczek, S.; Lipton, J.M.; Wolfe, L.; Prchal, J.T. The homozygous VHL(D126N) missense mutation is associated with dramatically elevated erythropoietin levels, consequent polycythemia, and early onset severe pulmonary hypertension. Pediatr. Blood Cancer 2014, 61, 2104–2106. [Google Scholar] [CrossRef]
- Caravita, S.; Deboeck, G.; Vachiery, J.L.; Naeije, R. Pulmonary arterial hypertension associated with a von Hippel-Lindau gene mutation. J. Heart Lung Transplant. Off. Publ. Int. Soc. Heart Transplant. 2016, 35, 1138–1139. [Google Scholar] [CrossRef]
- Botros, L.; Aman, J.; Bogaard, H.J.; Vonk Noordegraaf, A. Pulmonary hypertension with warm hands. Thorax 2017, 72, 1164–1166. [Google Scholar] [CrossRef] [PubMed]
- Perrotta, S.; Roberti, D.; Bencivenga, D.; Corsetto, P.; O’Brien, K.A.; Caiazza, M.; Stampone, E.; Allison, L.; Fleck, R.A.; Scianguetta, S.; et al. Effects of Germline VHL Deficiency on Growth, Metabolism, and Mitochondria. N. Engl. J. Med. 2020, 382, 835–844. [Google Scholar] [CrossRef]
- Smith, T.G.; Brooks, J.T.; Balanos, G.M.; Lappin, T.R.; Layton, D.M.; Leedham, D.L.; Liu, C.; Maxwell, P.H.; McMullin, M.F.; McNamara, C.J.; et al. Mutation of von Hippel-Lindau tumour suppressor and human cardiopulmonary physiology. PLoS Med. 2006, 3, e290. [Google Scholar] [CrossRef]
- Smith, T.G.; Brooks, J.T.; Balanos, G.M.; Lappin, T.R.; Layton, D.M.; Leedham, D.L.; Liu, C.; Maxwell, P.H.; McMullin, M.F.; McNamara, C.J.; et al. Mutation of the von Hippel-Lindau gene alters human cardiopulmonary physiology. Adv. Exp. Med. Biol. 2008, 605, 51–56. [Google Scholar]
- Young, J.M.; Williams, D.R.; Thompson, A.A.R. Thin Air, Thick Vessels: Historical and Current Perspectives on Hypoxic Pulmonary Hypertension. Front. Med. 2019, 6, 93. [Google Scholar] [CrossRef]
- Gassmann, M.; Cowburn, A.; Gu, H.; Li, J.; Rodriguez, M.; Babicheva, A.; Jain, P.P.; Xiong, M.; Gassmann, N.N.; Yuan, J.X.; et al. Hypoxia-induced pulmonary hypertension-Utilizing experiments of nature. Br. J. Pharmacol. 2020, 178, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Yu, A.Y.; Shimoda, L.A.; Iyer, N.V.; Huso, D.L.; Sun, X.; McWilliams, R.; Beaty, T.; Sham, J.S.; Wiener, C.M.; Sylvester, J.T.; et al. Impaired physiological responses to chronic hypoxia in mice partially deficient for hypoxia-inducible factor 1alpha. J. Clin. Investig. 1999, 103, 691–696. [Google Scholar] [CrossRef]
- Brusselmans, K.; Compernolle, V.; Tjwa, M.; Wiesener, M.S.; Maxwell, P.H.; Collen, D.; Carmeliet, P. Heterozygous deficiency of hypoxia-inducible factor-2alpha protects mice against pulmonary hypertension and right ventricular dysfunction during prolonged hypoxia. J. Clin. Investig. 2003, 111, 1519–1527. [Google Scholar] [CrossRef] [PubMed]
- Kapitsinou, P.P.; Rajendran, G.; Astleford, L.; Michael, M.; Schonfeld, M.P.; Fields, T.; Shay, S.; French, J.L.; West, J.; Haase, V.H. The Endothelial Prolyl-4-Hydroxylase Domain 2/Hypoxia-Inducible Factor 2 Axis Regulates Pulmonary Artery Pressure in Mice. Mol. Cell. Biol. 2016, 36, 1584–1594. [Google Scholar] [CrossRef] [PubMed]
- Ball, M.K.; Waypa, G.B.; Mungai, P.T.; Nielsen, J.M.; Czech, L.; Dudley, V.J.; Beussink, L.; Dettman, R.W.; Berkelhamer, S.K.; Steinhorn, R.H.; et al. Regulation of hypoxia-induced pulmonary hypertension by vascular smooth muscle hypoxia-inducible factor-1α. Am. J. Respir. Crit. Care Med. 2014, 189, 314–324. [Google Scholar] [CrossRef]
- Cowburn, A.S.; Crosby, A.; Macias, D.; Branco, C.; Colaço, R.D.; Southwood, M.; Toshner, M.; Crotty Alexander, L.E.; Morrell, N.W.; Chilvers, E.R.; et al. HIF2α-arginase axis is essential for the development of pulmonary hypertension. Proc. Natl. Acad. Sci. USA 2016, 113, 8801–8806. [Google Scholar] [CrossRef]
- Tang, H.; Babicheva, A.; McDermott, K.M.; Gu, Y.; Ayon, R.J.; Song, S.; Wang, Z.; Gupta, A.; Zhou, T.; Sun, X.; et al. Endothelial HIF-2α contributes to severe pulmonary hypertension due to endothelial-to-mesenchymal transition. Am. J. Physiol. Lung Cell Mol. Physiol. 2018, 314, L256–L275. [Google Scholar]
- Hu, C.J.; Poth, J.M.; Zhang, H.; Flockton, A.; Laux, A.; Kumar, S.; McKeon, B.; Mouradian, G.; Li, M.; Riddle, S.; et al. Suppression of HIF2 signalling attenuates the initiation of hypoxia-induced pulmonary hypertension. Eur. Respir. J. 2019, 54, 1900378. [Google Scholar] [CrossRef]
- Tan, Q.; Kerestes, H.; Percy, M.J.; Pietrofesa, R.; Chen, L.; Khurana, T.S.; Christofidou-Solomidou, M.; Lappin, T.R.; Lee, F.S. Erythrocytosis and pulmonary hypertension in a mouse model of human HIF2A gain of function mutation. J. Biol. Chem. 2013, 288, 17134–17144. [Google Scholar] [CrossRef]
- Dai, Z.; Li, M.; Wharton, J.; Zhu, M.M.; Zhao, Y.Y. Prolyl-4 Hydroxylase 2 (PHD2) Deficiency in Endothelial Cells and Hematopoietic Cells Induces Obliterative Vascular Remodeling and Severe Pulmonary Arterial Hypertension in Mice and Humans Through Hypoxia-Inducible Factor-2α. Circulation 2016, 133, 2447–2458. [Google Scholar] [CrossRef]
- Wang, S.; Zeng, H.; Xie, X.J.; Tao, Y.K.; He, X.; Roman, R.J.; Aschner, J.L.; Chen, J.X. Loss of prolyl hydroxylase domain protein 2 in vascular endothelium increases pericyte coverage and promotes pulmonary arterial remodeling. Oncotarget 2016, 7, 58848–58861. [Google Scholar] [CrossRef]
- Hickey, M.M.; Richardson, T.; Wang, T.; Mosqueira, M.; Arguiri, E.; Yu, H.; Yu, Q.C.; Solomides, C.C.; Morrisey, E.E.; Khurana, T.S.; et al. The von Hippel-Lindau Chuvash mutation promotes pulmonary hypertension and fibrosis in mice. J. Clin. Investig. 2010, 120, 827–839. [Google Scholar] [CrossRef]
- Newman, J.H.; Holt, T.N.; Cogan, J.D.; Womack, B.; Phillips, J.A., 3rd; Li, C.; Kendall, Z.; Stenmark, K.R.; Thomas, M.G.; Brown, R.D.; et al. Increased prevalence of EPAS1 variant in cattle with high-altitude pulmonary hypertension. Nat. Commun. 2015, 6, 6863. [Google Scholar] [CrossRef] [PubMed]
- Witt, K.E.; Huerta-Sánchez, E. Convergent evolution in human and domesticate adaptation to high-altitude environments. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 2019, 374, 20180235. [Google Scholar] [CrossRef]
- Bigham, A.W.; Lee, F.S. Human high-altitude adaptation: Forward genetics meets the HIF pathway. Genes Dev. 2014, 28, 2189–2204. [Google Scholar] [CrossRef]
- Peng, Y.; Cui, C.; He, Y.; Ouzhuluobu; Zhang, H.; Yang, D.; Zhang, Q.; Bianbazhuoma; Yang, L.; He, Y.; et al. Down-Regulation of EPAS1 Transcription and Genetic Adaptation of Tibetans to High-Altitude Hypoxia. Mol. Biol. Evol. 2017, 34, 818–830. [Google Scholar]
- Will, D.H.; Hicks, J.L.; Card, C.S.; Reeves, J.T.; Alexander, A.F. Correlation of acute with chronic hypoxic pulmonary hypertension in cattle. J. Appl. Physiol. 1975, 38, 495–498. [Google Scholar] [CrossRef]
- Hanson, W.L.; Boggs, D.F.; Kay, J.M.; Hofmeister, S.E.; Wagner, W.W., Jr. Collateral ventilation and pulmonary arterial smooth muscle in the coati. J. Appl. Physiol. 1993, 74, 2219–2224. [Google Scholar] [CrossRef] [PubMed]
- Hanson, W.L.; Boggs, D.F.; Kay, J.M.; Hofmeister, S.E.; Okada, O.; Wagner, W.W., Jr. Pulmonary vascular response of the coati to chronic hypoxia. J. Appl. Physiol. 2000, 88, 981–986. [Google Scholar] [CrossRef] [PubMed]
- Thompson, B.T.; Hassoun, P.M.; Kradin, R.L.; Hales, C.A. Acute and chronic hypoxic pulmonary hypertension in guinea pigs. J. Appl. Physiol. 1989, 66, 920–928. [Google Scholar] [CrossRef] [PubMed]
- Langleben, D.; Jones, R.C.; Aronovitz, M.J.; Hill, N.S.; Ou, L.C.; Reid, L.M. Pulmonary artery structural changes in two colonies of rats with different sensitivity to chronic hypoxia. Am. J. Pathol. 1987, 128, 61–66. [Google Scholar] [PubMed]
- Ou, L.C.; Sardella, G.L.; Hill, N.S.; Tenney, S.M. Acute and chronic pulmonary pressor responses to hypoxia: The role of blunting in acclimatization. Respir. Physiol. 1986, 64, 81–91. [Google Scholar] [CrossRef]
- He, L.S.; Chang, S.W.; Voelkel, N.F. Pulmonary vascular reactivity in Fischer rats. J. Appl. Physiol. 1991, 70, 1861–1866. [Google Scholar] [CrossRef] [PubMed]
- Malczyk, M.; Veith, C.; Fuchs, B.; Hofmann, K.; Storch, U.; Schermuly, R.T.; Witzenrath, M.; Ahlbrecht, K.; Fecher-Trost, C.; Flockerzi, V.; et al. Classical transient receptor potential channel 1 in hypoxia-induced pulmonary hypertension. Am. J. Respir. Crit. Care Med. 2013, 188, 1451–1459. [Google Scholar] [CrossRef]
- Weissmann, N.; Dietrich, A.; Fuchs, B.; Kalwa, H.; Ay, M.; Dumitrascu, R.; Olschewski, A.; Storch, U.; Mederos y Schnitzler, M.; Ghofrani, H.A.; et al. Classical transient receptor potential channel 6 (TRPC6) is essential for hypoxic pulmonary vasoconstriction and alveolar gas exchange. Proc. Natl. Acad. Sci. USA 2006, 103, 19093–19098. [Google Scholar] [CrossRef]
- Xia, Y.; Yang, X.R.; Fu, Z.; Paudel, O.; Abramowitz, J.; Birnbaumer, L.; Sham, J.S. Classical transient receptor potential 1 and 6 contribute to hypoxic pulmonary hypertension through differential regulation of pulmonary vascular functions. Hypertension 2014, 63, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Leon-Velarde, F.; Maggiorini, M.; Reeves, J.T.; Aldashev, A.; Asmus, I.; Bernardi, L.; Ge, R.L.; Hackett, P.; Kobayashi, T.; Moore, L.G.; et al. Consensus statement on chronic and subacute high altitude diseases. High Alt. Med. Biol. 2005, 6, 147–157. [Google Scholar] [CrossRef]
- Hoffman, J.I. Pulmonary vascular resistance and viscosity: The forgotten factor. Pediatr. Cardiol. 2011, 32, 557–561. [Google Scholar] [CrossRef] [PubMed]
- Richalet, J.P.; Rivera-Ch, M.; Maignan, M.; Privat, C.; Pham, I.; Macarlupu, J.L.; Petitjean, O.; Leon-Velarde, F. Acetazolamide for Monge’s disease: Efficiency and tolerance of 6-month treatment. Am. J. Respir. Crit. Care Med. 2008, 177, 1370–1376. [Google Scholar] [CrossRef]
- Ou, L.C.; Sardella, G.L.; Hill, N.S.; Thron, C.D. Possible role of pulmonary blood volume in chronic hypoxic pulmonary hypertension. J. Appl. Physiol. 1993, 74, 3020–3026. [Google Scholar] [CrossRef]
- Barer, G.R.; Bee, D.; Wach, R.A. Contribution of polycythaemia to pulmonary hypertension in simulated high altitude in rats. J. Physiol. 1983, 336, 27–38. [Google Scholar] [CrossRef]
- Manier, G.; Guenard, H.; Castaing, Y.; Varene, N.; Vargas, E. Pulmonary gas exchange in Andean natives with excessive polycythemia--effect of hemodilution. J. Appl. Physiol. 1988, 65, 2107–2117. [Google Scholar] [CrossRef]
- Winslow, R.M.; Monge, C.C.; Brown, E.G.; Klein, H.G.; Sarnquist, F.; Winslow, N.J.; McKneally, S.S. Effects of hemodilution on O2 transport in high-altitude polycythemia. J. Appl. Physiol. 1985, 59, 1495–1502. [Google Scholar] [CrossRef] [PubMed]
- Naeije, R.; Vanderpool, R. Pulmonary hypertension and chronic mountain sickness. High Alt. Med. Biol. 2013, 14, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Soria, R.; Egger, M.; Scherrer, U.; Bender, N.; Rimoldi, S.F. Pulmonary arterial pressure at rest and during exercise in chronic mountain sickness: A meta-analysis. Eur. Respir. J. 2019, 53, 1802040. [Google Scholar] [CrossRef]
- Stuber, T.; Sartori, C.; Schwab, M.; Jayet, P.Y.; Rimoldi, S.F.; Garcin, S.; Thalmann, S.; Spielvogel, H.; Salmon, C.S.; Villena, M.; et al. Exaggerated pulmonary hypertension during mild exercise in chronic mountain sickness. Chest 2010, 137, 388–392. [Google Scholar] [CrossRef] [PubMed]
- Jayet, P.Y.; Rimoldi, S.F.; Stuber, T.; Salmòn, C.S.; Hutter, D.; Rexhaj, E.; Thalmann, S.; Schwab, M.; Turini, P.; Sartori-Cucchia, C.; et al. Pulmonary and systemic vascular dysfunction in young offspring of mothers with preeclampsia. Circulation 2010, 122, 488–494. [Google Scholar] [CrossRef] [PubMed]
- Julian, C.G.; Gonzales, M.; Rodriguez, A.; Bellido, D.; Salmon, C.S.; Ladenburger, A.; Reardon, L.; Vargas, E.; Moore, L.G. Perinatal hypoxia increases susceptibility to high-altitude polycythemia and attendant pulmonary vascular dysfunction. Am. J. Physiol. Heart Circ. Physiol. 2015, 309, H565–H573. [Google Scholar] [CrossRef]
- Meister, T.A.; Rexhaj, E.; Rimoldi, S.F.; Scherrer, U.; Sartori, C. Effects of perinatal, late foetal, and early embryonic insults on the cardiovascular phenotype in experimental animal models and humans. Vasa. Z. Fur Gefasskrankh. 2016, 45, 439–449. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cotroneo, E.; Ashek, A.; Wang, L.; Wharton, J.; Dubois, O.; Bozorgi, S.; Busbridge, M.; Alavian, K.N.; Wilkins, M.R.; Zhao, L. Iron homeostasis and pulmonary hypertension: Iron deficiency leads to pulmonary vascular remodeling in the rat. Circ. Res. 2015, 116, 1680–1690. [Google Scholar] [CrossRef]
- Ghosh, M.C.; Zhang, D.L.; Jeong, S.Y.; Kovtunovych, G.; Ollivierre-Wilson, H.; Noguchi, A.; Tu, T.; Senecal, T.; Robinson, G.; Crooks, D.R.; et al. Deletion of iron regulatory protein 1 causes polycythemia and pulmonary hypertension in mice through translational derepression of HIF2α. Cell Metab. 2013, 17, 271–281. [Google Scholar] [CrossRef]
- Yu, J.; Yu, L.; Li, Y.; Hu, F. Iron deficiency is a possible risk factor causing right heart failure in Tibetan children living in high altitude area. Medicine 2020, 99, e21133. [Google Scholar] [CrossRef]
- Simonneau, G.; Montani, D.; Celermajer, D.S.; Denton, C.P.; Gatzoulis, M.A.; Krowka, M.; Williams, P.G.; Souza, R. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur. Respir. J. 2019, 53, 1801913. [Google Scholar] [CrossRef] [PubMed]
- Hoeper, M.M.; Humbert, M.; Souza, R.; Idrees, M.; Kawut, S.M.; Sliwa-Hahnle, K.; Jing, Z.C.; Gibbs, J.S. A global view of pulmonary hypertension. Lancet Respir. Med. 2016, 4, 306–322. [Google Scholar] [CrossRef]
- Sydykov, A.; Muratali Uulu, K.; Maripov, A.; Cholponbaeva, M.; Khan, T.; Sarybaev, A. A Case of Chronic Thromboembolic Pulmonary Hypertension in a High-Altitude Dweller. High Alt. Med. Biol. 2019, 20, 303–306. [Google Scholar] [CrossRef] [PubMed]
- Lei, S.; Sun, Z.; He, X.; Li, C.; Zhang, Y.; Luo, X.; Wu, S. Clinical characteristics of pulmonary hypertension patients living in plain and high-altitude regions. Clin. Respir. J. 2019, 13, 485–492. [Google Scholar] [CrossRef]
- Vargas, E.; Spielvogel, H. Chronic mountain sickness, optimal hemoglobin, and heart disease. High Alt. Med. Biol. 2006, 7, 138–149. [Google Scholar] [CrossRef] [PubMed]
- Xiong, H.; Huang, Q.; He, C.; Shuai, T.; Yan, P.; Zhu, L.; Yang, K.; Liu, J. Prevalence of chronic obstructive pulmonary disease at high altitude: A systematic review and meta-analysis. PeerJ 2020, 8, e8586. [Google Scholar] [CrossRef]
- Horner, A.; Soriano, J.B.; Puhan, M.A.; Studnicka, M.; Kaiser, B.; Vanfleteren, L.; Gnatiuc, L.; Burney, P.; Miravitlles, M.; García-Rio, F.; et al. Altitude and COPD prevalence: Analysis of the PREPOCOL-PLATINO-BOLD-EPI-SCAN study. Respir. Res. 2017, 18, 162. [Google Scholar] [CrossRef]
- Guo, Y.; Xing, Z.; Shan, G.; Janssens, J.P.; Sun, T.; Chai, D.; Liu, W.; Wang, Y.; Ma, Y.; Tong, Y.; et al. Prevalence and Risk Factors for COPD at High Altitude: A Large Cross-Sectional Survey of Subjects Living Between 2,100–4,700 m Above Sea Level. Front. Med. 2020, 7, 581763. [Google Scholar] [CrossRef]
- Chun, H.; Yue, Y.; Wang, Y.; Dawa, Z.; Zhen, P.; La, Q.; Zong, Y.; Qu, Y.; Mu, D. High prevalence of congenital heart disease at high altitudes in Tibet. Eur. J. Prev. Cardiol. 2019, 26, 756–759. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.H.; Wang, X.Q.; Qi, S.G. Cross-sectional study of congenital heart disease among Tibetan children aged from 4 to 18 years at different altitudes in Qinghai Province. Chin. Med. J. 2008, 121, 2469–2472. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.Y.; Qiu, Y.G.; Li, D.T.; He, J.C.; Chen, Y.; Cao, Y.; Liu, Y.M.; Li, X.F.; Chi, H.T.; Li, T.C. Prevalence and composition of CHD at different altitudes in Tibet: A cross-sectional study. Cardiol. Young 2017, 27, 1497–1503. [Google Scholar] [CrossRef]
- Peñaloza, D.; Arias-Stella, J.; Sime, F.; Recavarren, S.; Marticorena, E. The heart and pulmonary circulation in children at high altitudes: Physiological, anatomical, and clinical observations. Pediatrics 1964, 34, 568–582. [Google Scholar] [PubMed]
- González-Andrade, F. High Altitude as a Cause of Congenital Heart Defects: A Medical Hypothesis Rediscovered in Ecuador. High Alt. Med. Biol. 2020, 21, 126–134. [Google Scholar] [CrossRef]
- Saxena, A. Status of Pediatric Cardiac Care in Developing Countries. Children 2019, 6, 34. [Google Scholar] [CrossRef]
- Li, J.J.; Liu, Y.; Xie, S.Y.; Zhao, G.D.; Dai, T.; Chen, H.; Mu, L.F.; Qi, H.Y.; Li, J. Newborn screening for congenital heart disease using echocardiography and follow-up at high altitude in China. Int. J. Cardiol. 2019, 274, 106–112. [Google Scholar] [CrossRef]
- Pascall, E.; Tulloh, R.M. Pulmonary hypertension in congenital heart disease. Future Cardiol. 2018, 14, 343–353. [Google Scholar] [CrossRef] [PubMed]
- Kozlik-Feldmann, R.; Hansmann, G.; Bonnet, D.; Schranz, D.; Apitz, C.; Michel-Behnke, I. Pulmonary hypertension in children with congenital heart disease (PAH-CHD, PPHVD-CHD). Expert consensus statement on the diagnosis and treatment of paediatric pulmonary hypertension. The European Paediatric Pulmonary Vascular Disease Network, endorsed by ISHLT and DGPK. Heart (Br. Card. Soc.) 2016, 102 (Suppl. 2), ii42–ii48. [Google Scholar]
- Chen, Q.H.; Lu, L.; Qi, G.R.; Jin, X.H.; Wang, L.M.; Qi, S.G. Susceptibility of patients with congenital heart disease to pulmonary hypertension at a high altitude. Zhonghua Yi Xue Za Zhi 2011, 91, 3120–3122. [Google Scholar]
- Bialkowski, J.; Glowacki, J.; Zabal, C.; Garcia-Montes, A.; Bermudez-Canete, R.; Flores-Arizmendi, R.; Sagado-Sandova, A.; Diaz de Leon, H.; Delagadillo, R.M.; Kreutzer, J. Patent ductus arteriosus at low and high altitudes: Anatomical and haemodynamic features and their implications for transcatheter closure. Kardiol. Pol. 2011, 69, 431–436. [Google Scholar]
- Penaloza, D.; Sime, F.; Ruiz, L. Pulmonary hemodynamics in children living at high altitudes. High Alt. Med. Biol. 2008, 9, 199–207. [Google Scholar] [CrossRef]
- Hart, S.A.; Krasuski, R.A.; Wang, A.; Kisslo, K.; Harrison, J.K.; Bashore, T.M. Pulmonary hypertension and elevated transpulmonary gradient in patients with mitral stenosis. J. Heart Valve Dis. 2010, 19, 708–715. [Google Scholar]
- Leal, M.; Passos, L.S.A.; Guarconi, F.V.; Aguiar, J.M.S.; Silva, R.; Paula, T.M.N.; Santos, R.F.D.; Nassif, M.C.L.; Gomes, N.F.A.; Tan, T.C.; et al. Rheumatic heart disease in the modern era: Recent developments and current challenges. Rev. Soc. Bras. Med. Trop. 2019, 52, e20180041. [Google Scholar] [CrossRef] [PubMed]
- Celermajer, D.S.; Chow, C.K.; Marijon, E.; Anstey, N.M.; Woo, K.S. Cardiovascular disease in the developing world: Prevalences, patterns, and the potential of early disease detection. J. Am. Coll. Cardiol. 2012, 60, 1207–1216. [Google Scholar] [CrossRef] [PubMed]
- Marijon, E.; Ou, P.; Celermajer, D.S.; Ferreira, B.; Mocumbi, A.O.; Jani, D.; Paquet, C.; Jacob, S.; Sidi, D.; Jouven, X. Prevalence of rheumatic heart disease detected by echocardiographic screening. N. Engl. J. Med. 2007, 357, 470–476. [Google Scholar] [CrossRef]
- Burtscher, M. Effects of living at higher altitudes on mortality: A narrative review. Aging Dis. 2014, 5, 274–280. [Google Scholar] [PubMed]
- Wheatley, K.; Creed, M.; Mellor, A. Haematological changes at altitude. J. R. Army Med. Corps 2011, 157, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.C. Platelet count in permanent residents of high altitude. Indian J. Physiol. Pharmacol. 1981, 25, 65–68. [Google Scholar]
- Sharma, S.C.; Balasubramanian, V.; Chadha, K.S. Platelet adhesiveness in permanent residents of high altitude. Thromb. Haemost. 1980, 42, 1508–1512. [Google Scholar] [CrossRef]
- Hurtado, A. Studies at high altitude: Blood Observations on the Indian Natives of the Peruvian Andes. Am. J. Physiol. Leg. Content 1932, 100, 487–505. [Google Scholar] [CrossRef]
- Singh, I.; Chohan, I.S. Blood coagulation changes at high altitude predisposing to pulmonary hypertension. Br. Heart J. 1972, 34, 611–617. [Google Scholar] [CrossRef]
- Grover, R.F.; Vogel, J.H.; Voigt, G.C.; Blount, S.G., Jr. Reversal of high altitude pulmonary hypertension. Am. J. Cardiol. 1966, 18, 928–932. [Google Scholar] [CrossRef]
- Sime, F.; Penaloza, D.; Ruiz, L. Bradycardia, increased cardiac output, and reversal of pulmonary hypertension in altitude natives living at sea level. Br. Heart J. 1971, 33, 647–657. [Google Scholar] [CrossRef] [PubMed]
- Kojonazarov, B.; Isakova, J.; Imanov, B.; Sovkhozova, N.; Sooronbaev, T.; Ishizaki, T.; Aldashev, A.A. Bosentan reduces pulmonary artery pressure in high altitude residents. High Alt. Med. Biol. 2012, 13, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Aldashev, A.A.; Kojonazarov, B.K.; Amatov, T.A.; Sooronbaev, T.M.; Mirrakhimov, M.M.; Morrell, N.W.; Wharton, J.; Wilkins, M.R. Phosphodiesterase type 5 and high altitude pulmonary hypertension. Thorax 2005, 60, 683–687. [Google Scholar] [CrossRef]
- Gidwani, S.; Nair, A. The burden of pulmonary hypertension in resource-limited settings. Glob. Heart 2014, 9, 297–310. [Google Scholar] [CrossRef] [PubMed]
- Dzudie, A.; Dzekem, B.S.; Ojji, D.B.; Kengne, A.P.; Mocumbi, A.O.; Sliwa, K.; Thienemann, F. Pulmonary hypertension in low- and middle-income countries with focus on sub-Saharan Africa. Cardiovasc. Diagn. Ther. 2020, 10, 316–324. [Google Scholar] [CrossRef]
- Prins, K.W.; Thenappan, T.; Weir, E.K.; Kalra, R.; Pritzker, M.; Archer, S.L. Repurposing Medications for Treatment of Pulmonary Arterial Hypertension: What’s Old is New Again. J. Am. Heart Assoc. 2019, 8, e011343. [Google Scholar] [CrossRef] [PubMed]
- Grinnan, D.; Trankle, C.; Andruska, A.; Bloom, B.; Spiekerkoetter, E. Drug repositioning in pulmonary arterial hypertension: Challenges and opportunities. Pulm. Circ. 2019, 9, 2045894019832226. [Google Scholar] [CrossRef]
- Pichon, A.; Connes, P.; Quidu, P.; Marchant, D.; Brunet, J.; Levy, B.I.; Vilar, J.; Safeukui, I.; Cymbalista, F.; Maignan, M.; et al. Acetazolamide and chronic hypoxia: Effects on haemorheology and pulmonary haemodynamics. Eur. Respir. J. 2012, 40, 1401–1409. [Google Scholar] [CrossRef]
- Shimokawa, H.; Sunamura, S.; Satoh, K. RhoA/Rho-Kinase in the Cardiovascular System. Circ. Res. 2016, 118, 352–366. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; LoGrasso, P.V.; Defert, O.; Li, R. Rho Kinase (ROCK) Inhibitors and Their Therapeutic Potential. J. Med. Chem. 2016, 59, 2269–2300. [Google Scholar] [CrossRef]
- Abe, K.; Tawara, S.; Oi, K.; Hizume, T.; Uwatoku, T.; Fukumoto, Y.; Kaibuchi, K.; Shimokawa, H. Long-term inhibition of Rho-kinase ameliorates hypoxia-induced pulmonary hypertension in mice. J. Cardiovasc. Pharmacol. 2006, 48, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Nagaoka, T.; Morio, Y.; Casanova, N.; Bauer, N.; Gebb, S.; McMurtry, I.; Oka, M. Rho/Rho kinase signaling mediates increased basal pulmonary vascular tone in chronically hypoxic rats. Am. J. Physiol. Lung Cell Mol. Physiol. 2004, 287, L665–L672. [Google Scholar] [CrossRef] [PubMed]
- Lopez, N.C.; Ebensperger, G.; Herrera, E.A.; Reyes, R.V.; Calaf, G.; Cabello, G.; Moraga, F.A.; Benaldo, F.A.; Diaz, M.; Parer, J.T.; et al. Role of the RhoA/ROCK pathway in high-altitude associated neonatal pulmonary hypertension in lambs. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2016, 310, R1053–R1063. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.Z.; Li, S.Y.; Tian, X.Y.; Wu, Q.Q. Effect of fasudil on hypoxic pulmonary hypertension and right ventricular hypertrophy in rats. Int. J. Clin. Exp. Pathol. 2015, 8, 9517–9521. [Google Scholar]
- Sun, X.Z.; Li, S.Y.; Tian, X.Y.; Hong, Z.; Li, J.X. Effect of Rho kinase inhibitor fasudil on the expression ET-1 and NO in rats with hypoxic pulmonary hypertension. Clin. Hemorheol. Microcirc. 2019, 71, 3–8. [Google Scholar] [CrossRef]
- Jiang, X.; Wang, Y.F.; Zhao, Q.H.; Jiang, R.; Wu, Y.; Peng, F.H.; Xu, X.Q.; Wang, L.; He, J.; Jing, Z.C. Acute hemodynamic response of infused fasudil in patients with pulmonary arterial hypertension: A randomized, controlled, crossover study. Int. J. Cardiol. 2014, 177, 61–65. [Google Scholar] [CrossRef]
- Fukumoto, Y.; Matoba, T.; Ito, A.; Tanaka, H.; Kishi, T.; Hayashidani, S.; Abe, K.; Takeshita, A.; Shimokawa, H. Acute vasodilator effects of a Rho-kinase inhibitor, fasudil, in patients with severe pulmonary hypertension. Heart (Br. Card. Soc.) 2005, 91, 391–392. [Google Scholar] [CrossRef]
- Fujita, H.; Fukumoto, Y.; Saji, K.; Sugimura, K.; Demachi, J.; Nawata, J.; Shimokawa, H. Acute vasodilator effects of inhaled fasudil, a specific Rho-kinase inhibitor, in patients with pulmonary arterial hypertension. Heart Vessel. 2010, 25, 144–149. [Google Scholar] [CrossRef]
- Ishikura, K.; Yamada, N.; Ito, M.; Ota, S.; Nakamura, M.; Isaka, N.; Nakano, T. Beneficial acute effects of rho-kinase inhibitor in patients with pulmonary arterial hypertension. Circ. J. Off. J. Jpn. Circ. Soc. 2006, 70, 174–178. [Google Scholar] [CrossRef]
- Kojonazarov, B.; Myrzaakhmatova, A.; Sooronbaev, T.; Ishizaki, T.; Aldashev, A. Effects of fasudil in patients with high-altitude pulmonary hypertension. Eur. Respir. J. 2012, 39, 496–498. [Google Scholar] [CrossRef]
- Sommer, N.; Ghofrani, H.A.; Pak, O.; Bonnet, S.; Provencher, S.; Sitbon, O.; Rosenkranz, S.; Hoeper, M.M.; Kiely, D.G. Current and future treatments of pulmonary arterial hypertension. Br. J. Pharmacol. 2021, 178, 6–30. [Google Scholar] [CrossRef]
- Grimminger, F.; Schermuly, R.T.; Ghofrani, H.A. Targeting non-malignant disorders with tyrosine kinase inhibitors. Nat. Rev. Drug Discov. 2010, 9, 956–970. [Google Scholar] [CrossRef] [PubMed]
- Schermuly, R.T.; Dony, E.; Ghofrani, H.A.; Pullamsetti, S.; Savai, R.; Roth, M.; Sydykov, A.; Lai, Y.J.; Weissmann, N.; Seeger, W.; et al. Reversal of experimental pulmonary hypertension by PDGF inhibition. J. Clin. Investig. 2005, 115, 2811–2821. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Ma, J.; Shen, T.; Wang, S.; Ma, C.; Liu, Y.; Ran, Y.; Wang, L.; Liu, L.; Zhu, D. Platelet-derived growth factor (PDGF) induces pulmonary vascular remodeling through 15-LO/15-HETE pathway under hypoxic condition. Cell. Signal. 2012, 24, 1931–1939. [Google Scholar] [CrossRef] [PubMed]
- Rol, N.; Kurakula, K.B.; Happe, C.; Bogaard, H.J.; Goumans, M.J. TGF-beta and BMPR2 Signaling in PAH: Two Black Sheep in One Family. Int. J. Mol. Sci. 2018, 19, 2585. [Google Scholar] [CrossRef]
- Frank, D.B.; Lowery, J.; Anderson, L.; Brink, M.; Reese, J.; de Caestecker, M. Increased susceptibility to hypoxic pulmonary hypertension in Bmpr2 mutant mice is associated with endothelial dysfunction in the pulmonary vasculature. Am. J. Physiol. Lung Cell Mol. Physiol. 2008, 294, L98–L109. [Google Scholar] [CrossRef][Green Version]
- Takahashi, H.; Goto, N.; Kojima, Y.; Tsuda, Y.; Morio, Y.; Muramatsu, M.; Fukuchi, Y. Downregulation of type II bone morphogenetic protein receptor in hypoxic pulmonary hypertension. Am. J. Physiol. Lung Cell Mol. Physiol. 2006, 290, L450–L458. [Google Scholar] [CrossRef]
- Reynolds, A.M.; Holmes, M.D.; Danilov, S.M.; Reynolds, P.N. Targeted gene delivery of BMPR2 attenuates pulmonary hypertension. Eur. Respir. J. 2012, 39, 329–343. [Google Scholar] [CrossRef]
- Reynolds, A.M.; Xia, W.; Holmes, M.D.; Hodge, S.J.; Danilov, S.; Curiel, D.T.; Morrell, N.W.; Reynolds, P.N. Bone morphogenetic protein type 2 receptor gene therapy attenuates hypoxic pulmonary hypertension. Am. J. Physiol. Lung Cell Mol. Physiol. 2007, 292, L1182–L1192. [Google Scholar] [CrossRef]
- Woo, K.V.; Ornitz, D.M.; Singh, G.K. Diagnosis and Pathophysiological Mechanisms of Group 3 Hypoxia-Induced Pulmonary Hypertension. Curr. Treat. Options Cardiovasc. Med. 2019, 21, 16. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Oparil, S.; Sun, J.Z.; Thompson, J.A.; Chen, Y.F. Fibroblast growth factor mediates hypoxia-induced endothelin—A receptor expression in lung artery smooth muscle cells. J. Appl. Physiol. 2003, 95, 643–651, discussion 863. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Ma, C.; Zhang, Q.; Yu, L.; Ma, J.; Zhang, L.; Hao, X.; Cao, F.; Wang, L.; Zhu, D. The key role of transforming growth factor-beta receptor I and 15-lipoxygenase in hypoxia-induced proliferation of pulmonary artery smooth muscle cells. Int. J. Biochem. Cell Biol. 2012, 44, 1184–1202. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Dai, A.; Li, Q.; Hu, R. Hypoxia induces transforming growth factor-beta1 gene expression in the pulmonary artery of rats via hypoxia-inducible factor-1alpha. Acta Biochim. Et Biophys. Sin. 2007, 39, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.F.; Feng, J.A.; Li, P.; Xing, D.; Zhang, Y.; Serra, R.; Ambalavanan, N.; Majid-Hassan, E.; Oparil, S. Dominant negative mutation of the TGF-beta receptor blocks hypoxia-induced pulmonary vascular remodeling. J. Appl. Physiol. 2006, 100, 564–571. [Google Scholar] [CrossRef]
- Partovian, C.; Adnot, S.; Eddahibi, S.; Teiger, E.; Levame, M.; Dreyfus, P.; Raffestin, B.; Frelin, C. Heart and lung VEGF mRNA expression in rats with monocrotaline- or hypoxia-induced pulmonary hypertension. Am. J. Physiol. 1998, 275 Pt 2, H1948–H1956. [Google Scholar] [CrossRef]
- Partovian, C.; Adnot, S.; Raffestin, B.; Louzier, V.; Levame, M.; Mavier, I.M.; Lemarchand, P.; Eddahibi, S. Adenovirus-mediated lung vascular endothelial growth factor overexpression protects against hypoxic pulmonary hypertension in rats. Am. J. Respir. Cell Mol. Biol. 2000, 23, 762–771. [Google Scholar] [CrossRef]
- Taraseviciene-Stewart, L.; Kasahara, Y.; Alger, L.; Hirth, P.; Mc Mahon, G.; Waltenberger, J.; Voelkel, N.F.; Tuder, R.M. Inhibition of the VEGF receptor 2 combined with chronic hypoxia causes cell death-dependent pulmonary endothelial cell proliferation and severe pulmonary hypertension. Faseb J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2001, 15, 427–438. [Google Scholar] [CrossRef]
- Yamamoto, A.; Takahashi, H.; Kojima, Y.; Tsuda, Y.; Morio, Y.; Muramatsu, M.; Fukuchi, Y. Downregulation of angiopoietin-1 and Tie2 in chronic hypoxic pulmonary hypertension. Respiration 2008, 75, 328–338. [Google Scholar] [CrossRef]
- Kugathasan, L.; Dutly, A.E.; Zhao, Y.D.; Deng, Y.; Robb, M.J.; Keshavjee, S.; Stewart, D.J. Role of angiopoietin-1 in experimental and human pulmonary arterial hypertension. Chest 2005, 128 (Suppl. 6), 633s–642s. [Google Scholar] [CrossRef]
- Pullamsetti, S.S.; Mamazhakypov, A.; Weissmann, N.; Seeger, W.; Savai, R. Hypoxia-inducible factor signaling in pulmonary hypertension. J. Clin. Investig. 2020, 130, 5638–5651. [Google Scholar] [CrossRef]
- Li, X.; Zhang, X.; Leathers, R.; Makino, A.; Huang, C.; Parsa, P.; Macias, J.; Yuan, J.X.; Jamieson, S.W.; Thistlethwaite, P.A. Notch3 signaling promotes the development of pulmonary arterial hypertension. Nat. Med. 2009, 15, 1289–1297. [Google Scholar] [CrossRef] [PubMed]
- Qiao, L.; Xie, L.; Shi, K.; Zhou, T.; Hua, Y.; Liu, H. Notch signaling change in pulmonary vascular remodeling in rats with pulmonary hypertension and its implication for therapeutic intervention. PLoS ONE 2012, 7, e51514. [Google Scholar] [CrossRef] [PubMed]
- Savai, R.; Al-Tamari, H.M.; Sedding, D.; Kojonazarov, B.; Muecke, C.; Teske, R.; Capecchi, M.R.; Weissmann, N.; Grimminger, F.; Seeger, W.; et al. Pro-proliferative and inflammatory signaling converge on FoxO1 transcription factor in pulmonary hypertension. Nat. Med. 2014, 20, 1289–1300. [Google Scholar] [CrossRef] [PubMed]
- Dai, Z.; Zhu, M.M.; Peng, Y.; Jin, H.; Machireddy, N.; Qian, Z.; Zhang, X.; Zhao, Y.Y. Endothelial and Smooth Muscle Cell Interaction via FoxM1 Signaling Mediates Vascular Remodeling and Pulmonary Hypertension. Am. J. Respir. Crit. Care Med. 2018, 198, 788–802. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.K.; Lee, J.H.; Oh, Y.M.; Lee, Y.S.; Lee, S.D. Rosiglitazone attenuates hypoxia-induced pulmonary arterial hypertension in rats. Respirology 2010, 15, 659–668. [Google Scholar] [CrossRef]
- Harrington, L.S.; Moreno, L.; Reed, A.; Wort, S.J.; Desvergne, B.; Garland, C.; Zhao, L.; Mitchell, J.A. The PPARbeta/delta agonist GW0742 relaxes pulmonary vessels and limits right heart hypertrophy in rats with hypoxia-induced pulmonary hypertension. PLoS ONE 2010, 5, e9526. [Google Scholar] [CrossRef] [PubMed]
- Nisbet, R.E.; Bland, J.M.; Kleinhenz, D.J.; Mitchell, P.O.; Walp, E.R.; Sutliff, R.L.; Hart, C.M. Rosiglitazone attenuates chronic hypoxia-induced pulmonary hypertension in a mouse model. Am. J. Respir. Cell Mol. Biol. 2010, 42, 482–490. [Google Scholar] [CrossRef] [PubMed]
- Crossno, J.T., Jr.; Garat, C.V.; Reusch, J.E.; Morris, K.G.; Dempsey, E.C.; McMurtry, I.F.; Stenmark, K.R.; Klemm, D.J. Rosiglitazone attenuates hypoxia-induced pulmonary arterial remodeling. Am. J. Physiol. Lung Cell Mol. Physiol. 2007, 292, L885–L897. [Google Scholar] [CrossRef] [PubMed]
- Nizet, V.; Johnson, R.S. Interdependence of hypoxic and innate immune responses. Nat. Rev. Immunol. 2009, 9, 609–617. [Google Scholar] [CrossRef]
- Burke, D.L.; Frid, M.G.; Kunrath, C.L.; Karoor, V.; Anwar, A.; Wagner, B.D.; Strassheim, D.; Stenmark, K.R. Sustained hypoxia promotes the development of a pulmonary artery-specific chronic inflammatory microenvironment. Am. J. Physiol. Lung Cell Mol. Physiol. 2009, 297, L238–L250. [Google Scholar] [CrossRef]
- Scherrer, U.; Rexhaj, E.; Rimoldi, S.F.; Allemann, Y.; Sartori, C. Hypoxic Pulmonary Hypertension, Novel Predisposing Factors, Unsuspected Mechanisms. Curr. Respir. Med. Rev. 2012, 8, 123–130. [Google Scholar] [CrossRef]
- Scherrer, U.; Allemann, Y.; Rexhaj, E.; Rimoldi, S.F.; Sartori, C. Mechanisms and drug therapy of pulmonary hypertension at high altitude. High Alt. Med. Biol. 2013, 14, 126–133. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, M.R.; Aman, J.; Harbaum, L.; Ulrich, A.; Wharton, J.; Rhodes, C.J. Recent advances in pulmonary arterial hypertension. F1000Research 2018, 7, 1128. [Google Scholar] [CrossRef]
- Chan, S.Y.; Rubin, L.J. Metabolic dysfunction in pulmonary hypertension: From basic science to clinical practice. Eur. Respir. Rev. Off. J. Eur. Respir. Soc. 2017, 26, 170094. [Google Scholar] [CrossRef]
- Harvey, L.D.; Chan, S.Y. Emerging Metabolic Therapies in Pulmonary Arterial Hypertension. J. Clin. Med. 2017, 6, 43. [Google Scholar] [CrossRef]
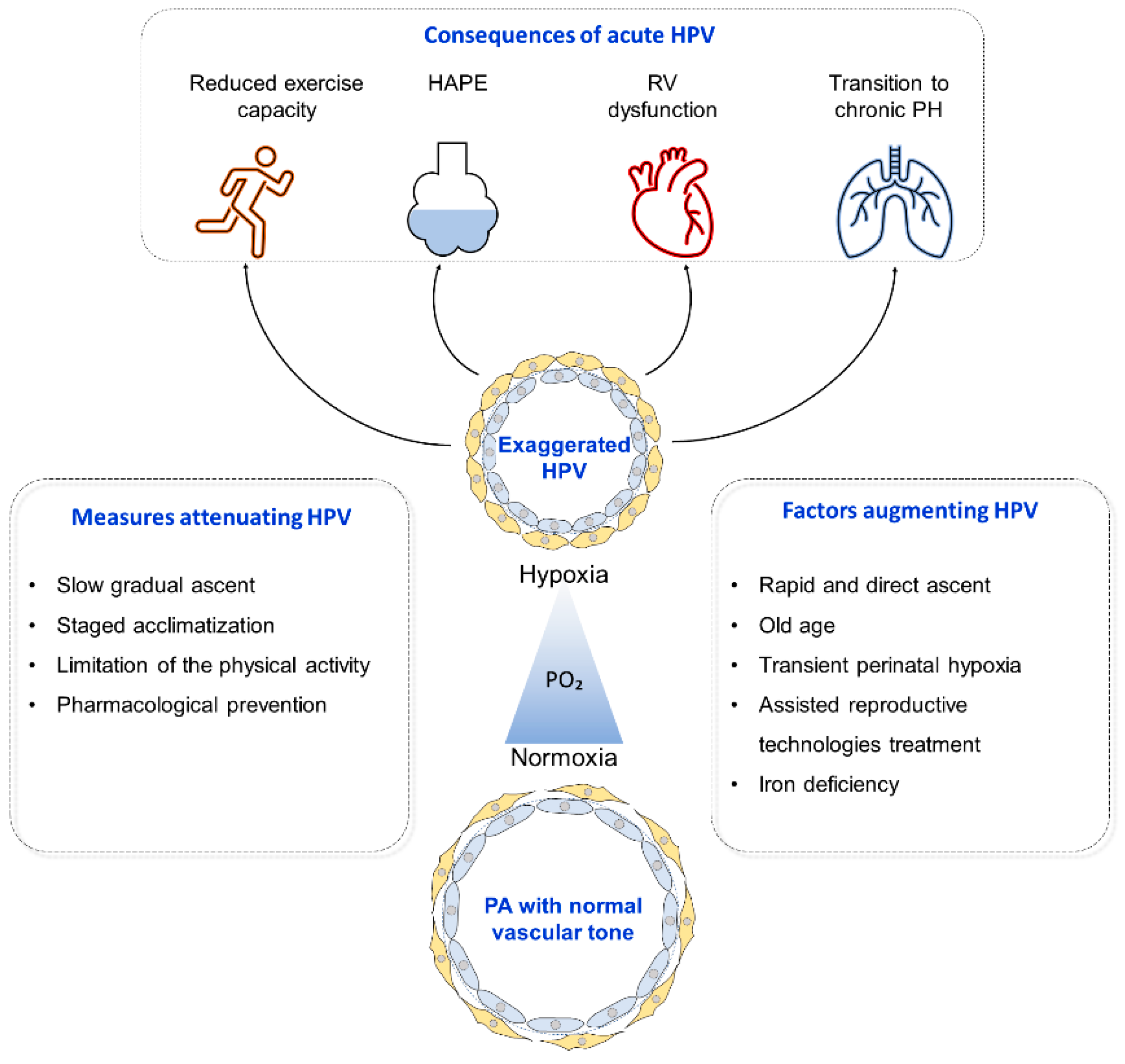
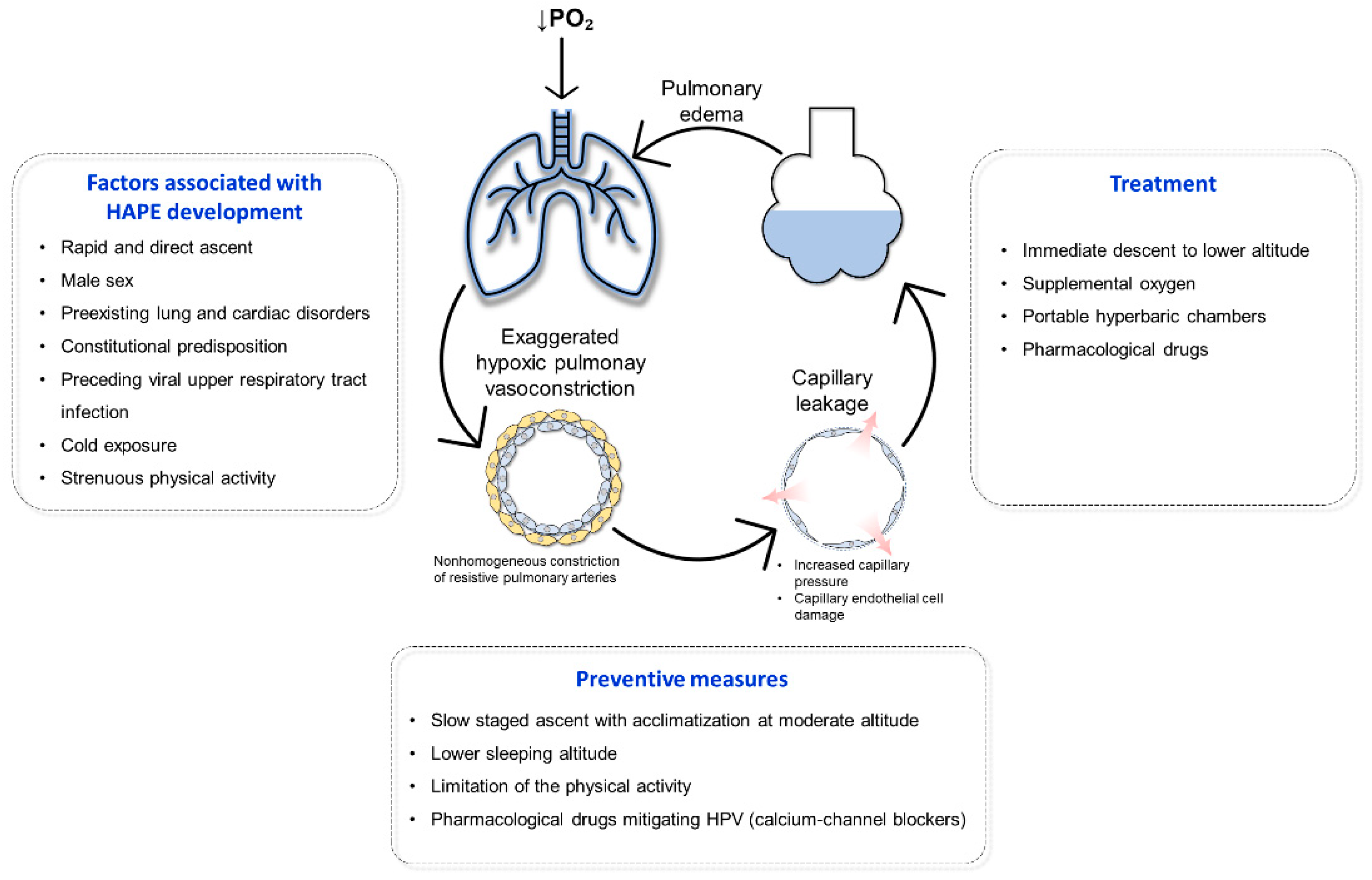
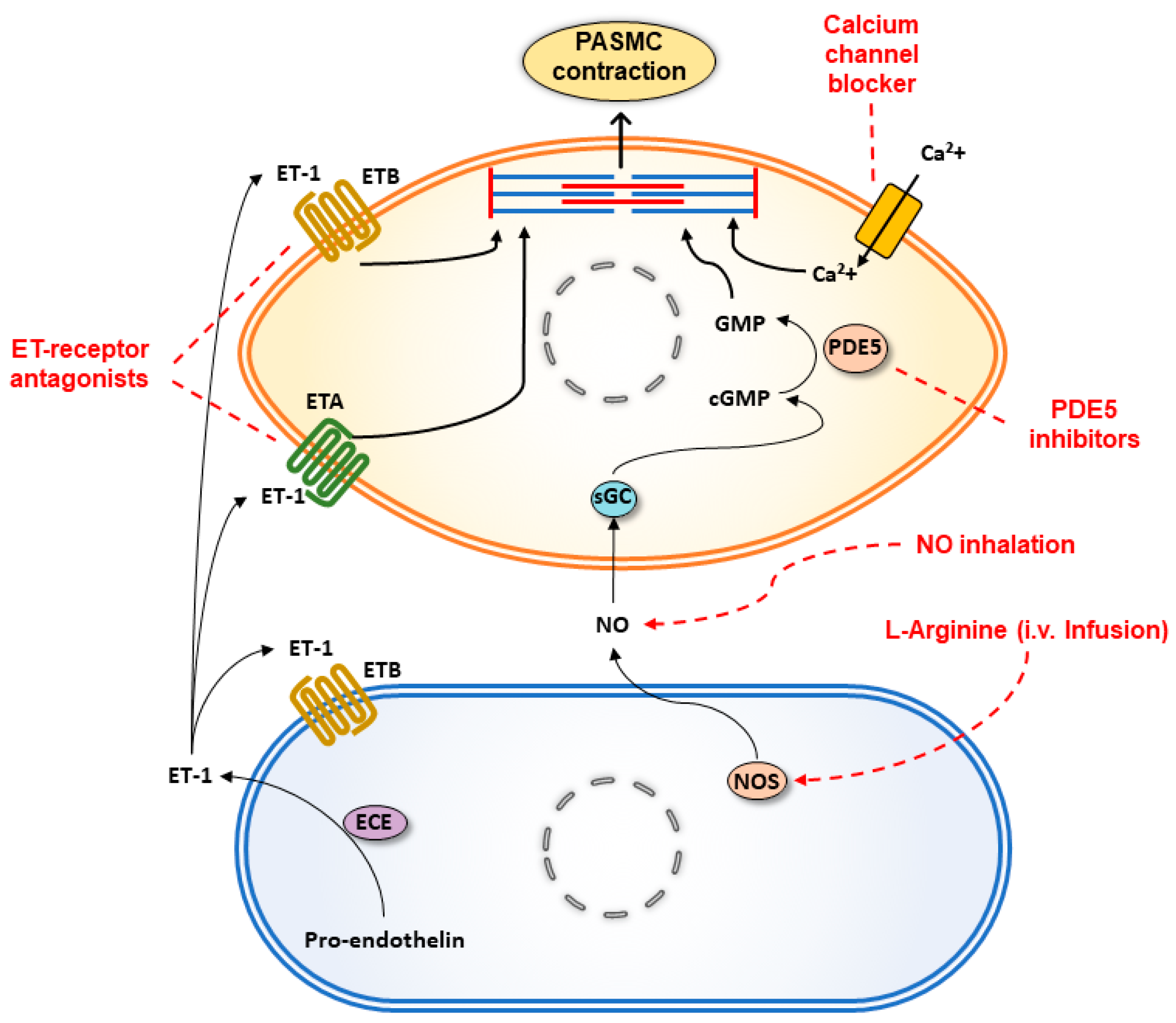
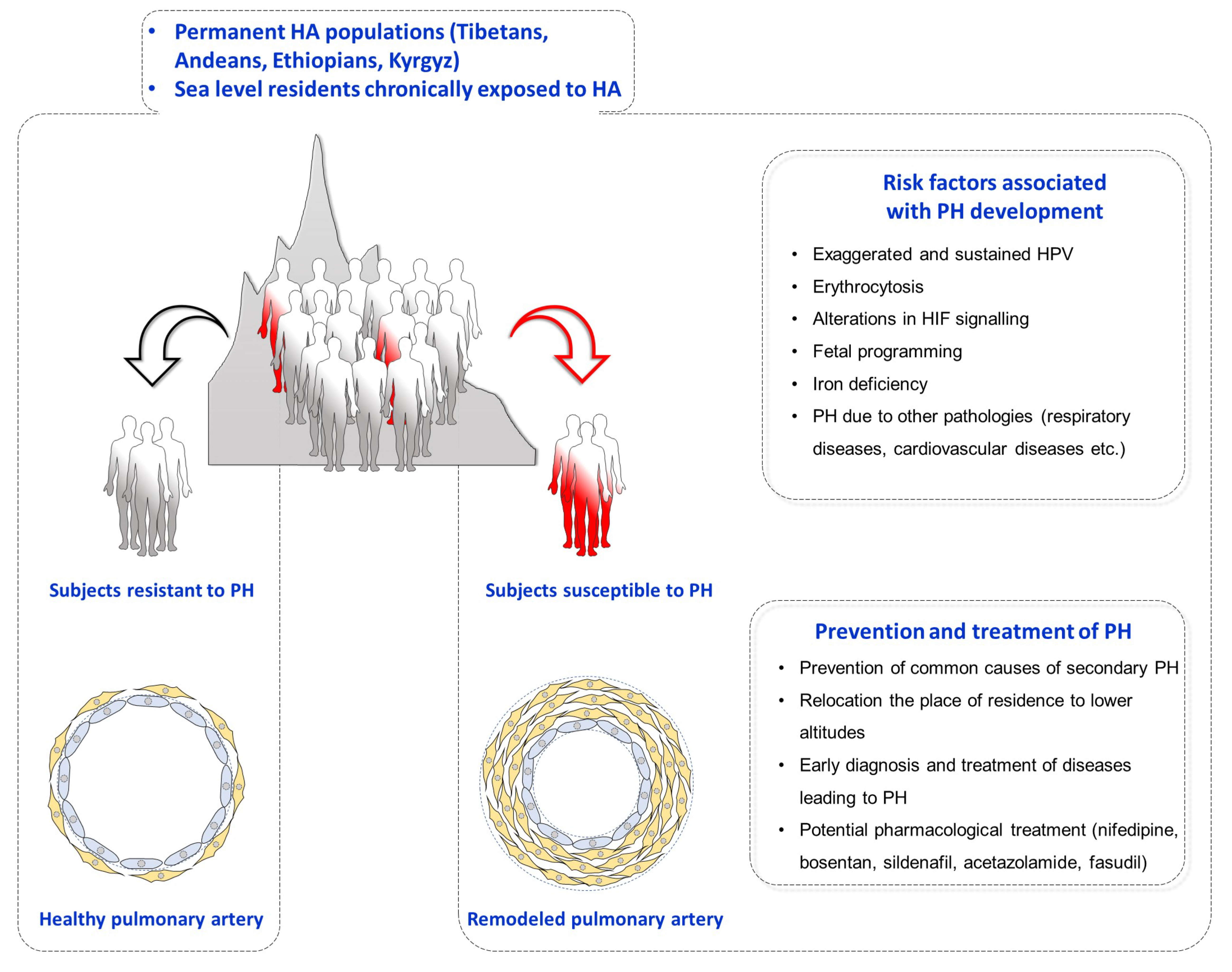
| Drugs | Mechanism of Action | Effects | References |
|---|---|---|---|
| Inhaled NO | Soluble guanylate cyclase stimulator | attenuates hypoxia-induced PVR increase in ventilated dogs | [139] |
| improves survival of HAPE rats at extreme altitude (hypobaric chamber) | [140] | ||
| decreases PAP and PVR in hypoxia-breathing lambs | [105,141] | ||
| Sildenafil | Phosphodiesterase 5 inhibitor | attenuates hypoxia-induced human and rats PA constriction | [142] |
| attenuates hypoxia-induced RVSP increase in ventilated rats | [143] | ||
| Tadalafil | Phosphodiesterase 5 inhibitor | inhibits hypoxia-induced isolated rat PA constriction | [144] |
| prevents an increase in RVSP in ventilated hypoxia-breathing rats | [145] | ||
| Bosentan | Endothelin receptor receptor A/B antagonist | decreases PAP in isolated perfused rat lung | [146] |
| prevents PAP increase in hypoxia exposed rats | [147] | ||
| Nifedipine | Calcium channel blocker | reduces PVR in hypoxia-breathing awake piglets | [148] |
| Dexamethasone | Anti-inflammatory and immunosuppressive agent | increases NOS expression and improves hypoxia-induced PAEC dysfunction | [130] |
| stimulates the expression of Na transporters and prevents hypoxia-induced inhibition of alveolar reabsorption | [133] | ||
| improves lung epithelial Na+ channels and Na+/K+-ATPase and increases alveolar fluid clearance in rats | [132] | ||
| improves pulmonary capillary endothelial permeability and prevents HAPE development in rat model | [131] | ||
| Acetazolamide | Carbonic anhydrase inhibitor | prevents an increase in PAP and PVR in conscious hypoxia-breathing dogs | [149] |
| inhibits hypoxia-induced Ca2+ influx in PASMCs | [150] |
| Drugs | Mechanism of Action | Effects | References |
|---|---|---|---|
| Inhaled NO | Soluble guanylate cyclase stimulator | decreases sPAP and improves oxygenation in HAPE-prone subjects at HA | [112] |
| reduces mPAP and PVR in HAPE patients at HA | [113] | ||
| decreases PAP and PVR in hypoxia-breathing healthy subjects | [112] | ||
| Sildenafil | Phosphodiesterase 5 inhibitor | prevents an increase in PAP and PVR in hypoxia-breathing healthy subjects | [20,151] |
| decreases sPAP and improves exercise capacity under hypoxic breathing and at HA in healthy subjects | [114] | ||
| decreases sPAP and improves blood oxygenation upon acute HA exposure in healthy subjects | [117] | ||
| attenuates sPAP increase and RV dysfunction upon acute HA exposure in healthy subjects | [22] | ||
| Tadalafil | Phosphodiesterase 5 inhibitor | attenuates an increase in PAP and prevents HAPE development | [64] |
| Bosentan | Endothelin receptor receptor A/B antagonist | prevents an increase in sPAP and PVR in hypoxia breathing healthy subjects | [125,126,127] |
| prevents an increase in sPAP and improves arterial oxygen saturation in healthy subjects exposed to HA | [122] | ||
| Sitaxentan | Endothelin receptor antagonist | prevents an increase of PAP and PVR and exercise capacity decline in hypoxia-breathing healthy subjects | [129] |
| reduces PVR and improves lung diffusion capacity and exercise capacity in healthy subjects exposed to HA | [152] | ||
| reduces PAP and PVR and improves exercise capacity in healthy subjects exposed to HA | [129] | ||
| Nifedipine | Calcium channel blocker | reduces PAP and improves HAPE symptoms | [66] |
| attenuates an increase in PAP and prevents HAPE development | [63] | ||
| Dexamethasone | Anti-inflammatory and immunosuppressive agent | attenuates an increase in PAP and prevents HAPE development | [64] |
| attenuates an increase in TRG and PVR and improves oxygenation in COPD patients at HA | [153] | ||
| attenuates an increase in TRG and improves exercise capacity | [154] | ||
| Acetazolamide | Carbonic anhydrase inhibitor | prevents an increase in TRG in hypoxia-breathing healthy subjects | [136] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sydykov, A.; Mamazhakypov, A.; Maripov, A.; Kosanovic, D.; Weissmann, N.; Ghofrani, H.A.; Sarybaev, A.S.; Schermuly, R.T. Pulmonary Hypertension in Acute and Chronic High Altitude Maladaptation Disorders. Int. J. Environ. Res. Public Health 2021, 18, 1692. https://doi.org/10.3390/ijerph18041692
Sydykov A, Mamazhakypov A, Maripov A, Kosanovic D, Weissmann N, Ghofrani HA, Sarybaev AS, Schermuly RT. Pulmonary Hypertension in Acute and Chronic High Altitude Maladaptation Disorders. International Journal of Environmental Research and Public Health. 2021; 18(4):1692. https://doi.org/10.3390/ijerph18041692
Chicago/Turabian StyleSydykov, Akylbek, Argen Mamazhakypov, Abdirashit Maripov, Djuro Kosanovic, Norbert Weissmann, Hossein Ardeschir Ghofrani, Akpay Sh. Sarybaev, and Ralph Theo Schermuly. 2021. "Pulmonary Hypertension in Acute and Chronic High Altitude Maladaptation Disorders" International Journal of Environmental Research and Public Health 18, no. 4: 1692. https://doi.org/10.3390/ijerph18041692
APA StyleSydykov, A., Mamazhakypov, A., Maripov, A., Kosanovic, D., Weissmann, N., Ghofrani, H. A., Sarybaev, A. S., & Schermuly, R. T. (2021). Pulmonary Hypertension in Acute and Chronic High Altitude Maladaptation Disorders. International Journal of Environmental Research and Public Health, 18(4), 1692. https://doi.org/10.3390/ijerph18041692








