A Randomized Clinical Trial Preventive Outreach Targeting Dental Caries and Oral-Health-Related Quality of Life for Refugee Children
Abstract
1. Introduction
2. Materials and Methods
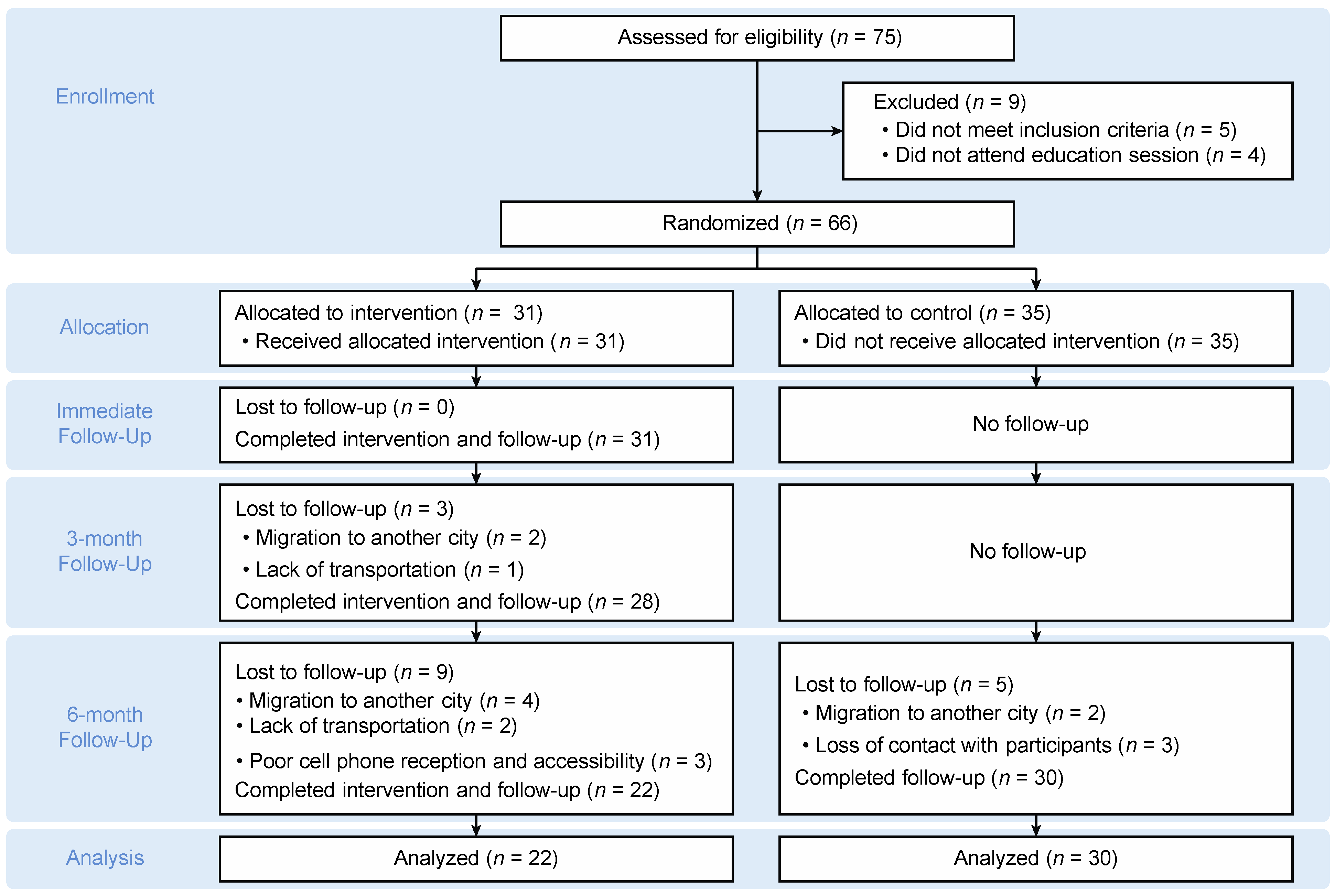
2.1. Study Design
2.2. Study Population
2.3. Inclusion and Exclusion Criteria
2.4. Study Procedures
2.5. Educational Intervention
2.6. Outcome Measurements
2.6.1. Michigan Oral-Health-Related Quality of Life Scale–Parent Version (MOHRQoL-P)
2.6.2. WHO Oral Health Assessment Form
2.7. Statistical Analysis
3. Results
3.1. Demographics of the Participants
3.2. Verification of Randomization and Intraexaminer Reliability
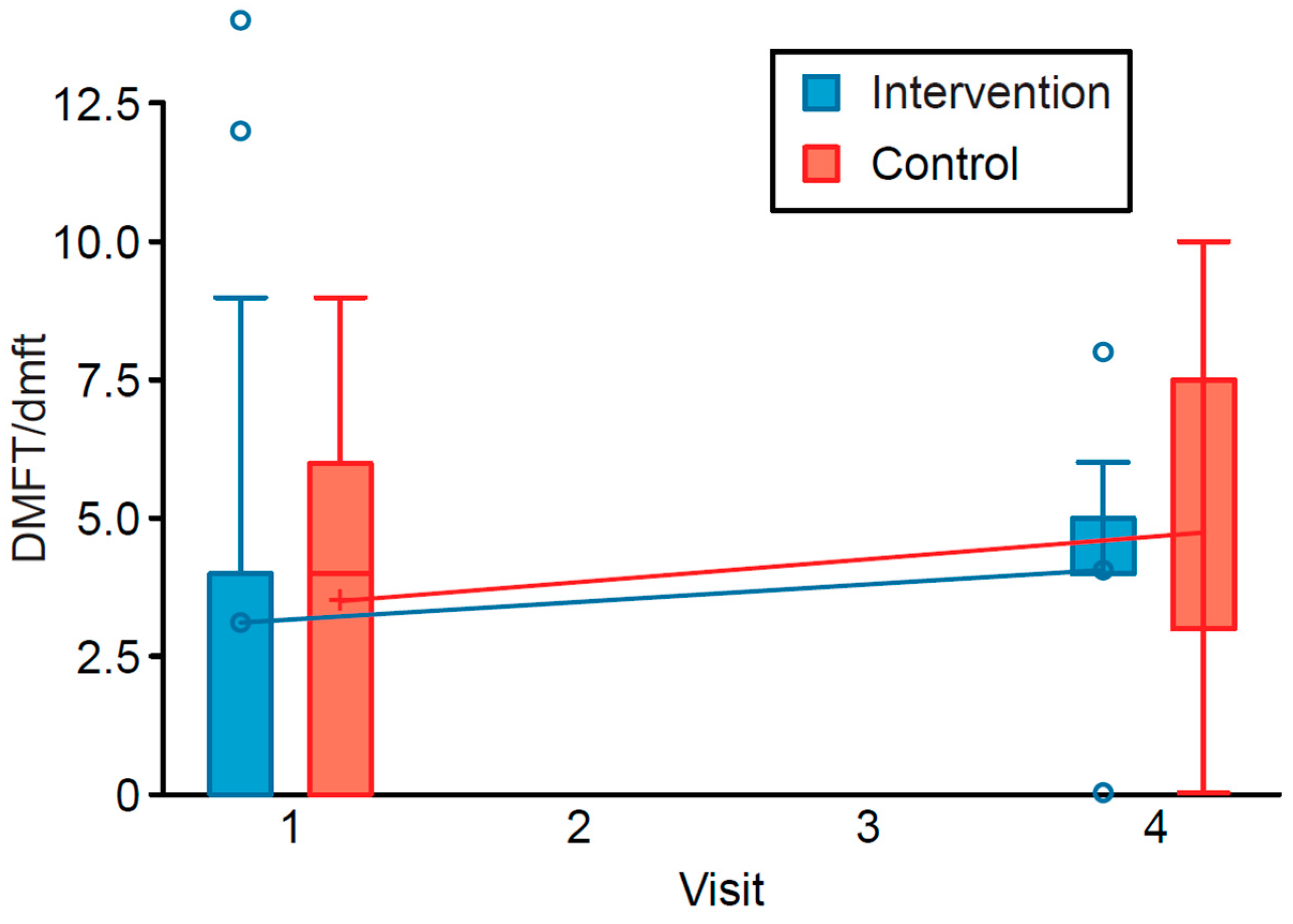
3.3. Outcomes
3.4. MOHRQoL-P Score
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Edelstein, B.L. Disparities in oral health and access to care: Findings of national surveys. Ambul. Pediatr. 2002, 2, 141–147. [Google Scholar] [CrossRef]
- Anil, S.; Anand, P.S. Early childhood caries: Prevalence, risk factors, and prevention. Front. Pediatr. 2017, 5, 157. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Gomez, F.J.; Tomar, S.L.; Ellison, J.; Artiga, N.; Sintes, J.; Vicuna, G. Assessment of early childhood caries and dietary habits in a population of migrant Hispanic children in Stockton, California. ASDC J. Dent. Child. 1999, 66, 395–403. [Google Scholar] [PubMed]
- Lagerweij, M.D.; van Loveren, C. Declining caries trends: Are we satisfied? Curr. Oral Health Rep. 2015, 2, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Horst, J.A.; Tanzer, J.M.; Milgrom, P.M. Fluorides and other preventive strategies for tooth decay. Dent. Clin. N. Am. 2018, 62, 207–234. [Google Scholar] [CrossRef]
- Gupta, N.; Vujicic, M.; Yarbrough, C.; Harrison, B. Disparities in untreated caries among children and adults in the U.S., 2011–2014. BMC Oral Health 2018, 18, 30. [Google Scholar] [CrossRef] [PubMed]
- Patrick, D.L.; Lee, R.S.; Nucci, M.; Grembowski, D.; Jolles, C.Z.; Milgrom, P. Reducing oral health disparities: A focus on social and cultural determinants. BMC Oral Health 2006, 6, 1–17. [Google Scholar] [CrossRef]
- Castañeda, X.; Ruelas, M.R.; Ramos-Gomez, F.; Ojeda, G. Oral Health and Latinos in the US (Fact Sheet); Health Initiative of America, School of Public Health, University of California Berkeley: Berkeley, CA, USA, 2010. [Google Scholar]
- Singh, H.K.; Scott, T.E.; Henshaw, M.M.; Cote, S.E.; Grodin, M.A.; Piwowarczyk, L.A. Oral health status of refugee torture survivors seeking care in the United States. Am. J. Public Health 2008, 98, 2181–2182. [Google Scholar] [CrossRef]
- Keboa, M.T.; Hiles, N.; Macdonald, M.E. The oral health of refugees and asylum seekers: A scoping review. Glob. Health 2016, 12, 1–11. [Google Scholar] [CrossRef]
- Adams, J.H.; Young, S.; Laird, L.D.; Geltman, P.L.; Cochran, J.J.; Hassan, A.; Egal, F.; Paasche-Orlow, M.K.; Barnes, L.L. The cultural basis for oral health practices among Somali refugees pre-and post-resettlement in Massachusetts. J. Health Care Poor Underserved 2013, 24, 1474–1485. [Google Scholar] [CrossRef]
- Yawary, R.; Anthonappa, R.P.; Ekambaram, M.; McGrath, C.; King, N.M. Changes in the oral health-related quality of life in children following comprehensive oral rehabilitation under general anaesthesia. Int. J. Paediatr. Dent. 2016, 26, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Cantekin, K.; Yildirim, M.D.; Cantekin, I. Assessing change in quality of life and dental anxiety in young children following dental rehabilitation under general anesthesia. Pediatr. Dent. 2014, 36, 12E–17E. [Google Scholar] [PubMed]
- Schulz, K.F.; Altman, D.G.; Moher, D.; Group, C. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMC Med. 2010, 8, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Alrashdi, M.; Hameed, A.; Cervantes Mendez, M.J.; Farokhi, M. Education intervention with respect to the oral health knowledge, attitude, and behaviors of refugee families: A randomized clinical trial of effectiveness. J. Public Health Dent. 2020. [Google Scholar] [CrossRef]
- National Institute of Dental and Craniofacial Research, National Institutes of Health. A Healthy Mouth for Baby; National Institute of Dental and Craniofacial Research, National Institutes of Health: Bethesda, MD, USA, 2020.
- Pennington, J.A.; Hubbard, V.S. Nutrition education materials from the national institutes of health: Development, review, and availability. J. Nutr. Educ. Behav. 2002, 34, 53–58. [Google Scholar] [CrossRef]
- National Center on Early Childhood Health and Wellness. Healthy Habits for Happy Smiles; National Center on Early Childhood Health and Wellness: Elk Grove Village, IL, USA, 2016.
- Filstrup, S.L.; Briskie, D.; da Fonseca, M.; Lawrence, L.; Wandera, A.; Inglehart, M.R. Early childhood caries and quality of life: Child and parent perspectives. Pediatr. Dent. 2003, 25, 431–440. [Google Scholar] [PubMed]
- World Health Organization. Oral Health Surveys: Basic Methods; WHO: Geneva, Switzerland, 2013. [Google Scholar]
- Ballinger, G.A. Using generalized estimating equations for longitudinal data analysis. Organ. Res. Methods 2004, 7, 127–150. [Google Scholar] [CrossRef]
- Low, W.; Tan, S.; Schwartz, S. The effect of severe caries on the quality of life in young children. Pediatr. Dent. 1999, 21, 325–326. [Google Scholar] [PubMed]
- Acs, G.; Pretzer, S.; Foley, M.; Ng, M.W. Perceived outcomes and parental satisfaction following dental rehabilitation under general anesthesia. Pediatr. Dent. 2001, 23, 419–423. [Google Scholar]
- Thomas, C.W.; Primosch, R.E. Changes in incremental weight and well-being of children with rampant caries following complete dental rehabilitation. Pediatr. Dent. 2002, 24, 109–113. [Google Scholar] [PubMed]
- Geltman, P.L.; Adams, J.H.; Cochran, J.; Doros, G.; Rybin, D.; Henshaw, M.; Barnes, L.L.; Paasche-Orlow, M. The impact of functional health literacy and acculturation on the oral health status of Somali refugees living in Massachusetts. Am. J. Public Health 2013, 103, 1516–1523. [Google Scholar] [CrossRef] [PubMed]
- Marino, R.; Stuart, G.W.; Wright, F.A.; Minas, I.H.; Klimidis, S. Acculturation and dental health among Vietnamese living in Melbourne, Australia. Commun. Dent. Oral Epidemiol. 2001, 29, 107–119. [Google Scholar] [CrossRef]
- Cascaes, A.M.; Bielemann, R.M.; Clark, V.L.; Barros, A.J. Effectiveness of motivational interviewing at improving oral health: A systematic review. Rev. Saude Publica 2014, 48, 142–153. [Google Scholar] [CrossRef] [PubMed]
- Garcia, R.I.; Cadoret, C.A.; Henshaw, M. Multicultural issues in oral health. Dent. Clin. N. Am. 2008, 52, 319–332. [Google Scholar] [CrossRef] [PubMed]
| Variables | Intervention Group | Control Group | Total |
|---|---|---|---|
| % (n) | % (n) | % (n) | |
| Gender | |||
| Male | 23 (7) | 37 (13) | 30 (20) |
| Female | 77 (24) | 63 (22) | 70 (46) |
| Marital status | |||
| Married/living with partner | 94 (29) | 100 (35) | 97 (64) |
| Single/separated/divorced/widowed | 6 (2) | 0 (0) | 3 (2) |
| Education | |||
| Elementary or middle school | 52 (16) | 49 (17) | 50 (33) |
| High school | 19 (6) | 17 (6) | 18 (12) |
| Some college but not a degree | 19 (6) | 6 (2) | 12 (8) |
| Bachelor’s degree | 7 (2) | 17 (6) | 12 (8) |
| Master’s degree | 3 (1) | 11 (4) | 8 (5) |
| Race | |||
| Southeast and South Asian | 58 (18) | 60 (21) | 59 (39) |
| Middle Eastern | 32 (10) | 20 (7) | 26 (17) |
| African/Hispanic | 10 (3) | 20 (7) | 15 (10) |
| Country of origin | |||
| Myanmar | 49 (15) | 31 (11) | 39 (26) |
| Nepal | 26 (8) | 14 (5) | 20 (13) |
| Turkey | 13 (4) | 20 (7) | 17 (11) |
| Iraq | 3 (1) | 20 (7) | 12 (8) |
| Afghanistan | 3 (1) | 6 (2) | 4 (3) |
| Cameroon | 3 (1) | 3 (1) | 3 (2) |
| Eritrea | 3 (1) | 3 (1) | 3 (2) |
| Mexico | 0 (0) | 3 (1) | 2 (1) |
| Language | |||
| Burmese | 48 (15) | 31.4 (11) | 39 (26) |
| Nepalese | 26 (8) | 14.3 (5) | 20 (13) |
| Turkish | 13 (4) | 20 (7) | 17 (11) |
| Arabic | 3 (1) | 20 (7) | 12 (8) |
| English | 10 (3) | 12 (4) | 10 (7) |
| Spanish | 0 | 3 (1) | 2 (1) |
| Monthly income | |||
| <$2000 | 64 (20) | 80 (28) | 73 (48) |
| >$2000 | 36 (11) | 20 (7) | 27 (18) |
| Parent or caregiver’s Age | |||
| 18–24 years | 16 (5) | 17 (6) | 17 (11) |
| 25–34 years | 45 (14) | 49 (17) | 47 (31) |
| 35–44 years | 29 (9) | 31 (11) | 30 (20) |
| >45 years | 10 (3) | 3 (1) | 6 (4) |
| Child’s age | |||
| 3–5 years | 29 (9) | 28 (10) | 29 (19) |
| 6–8 years | 45 (14) | 43 (15) | 44 (29) |
| 9–11 years | 23 (7) | 26 (9) | 24 (16) |
| 12 years | 3 (1) | 3 (1) | 3 (2) |
| Outcome | Parameter | Estimate | 95% Confidence Interval | p-Value | |
|---|---|---|---|---|---|
| DMFT/dmft | Intervention | −0.2310 | −0.57 | 0.11 | 0.18 |
| Time (T4 vs. T1) | 0.2814 | 0.06 | 0.50 | 0.01 | |
| Income (high vs. low) | −0.1293 | −0.60 | 0.34 | 0.59 | |
| Education | −0.0773 | −0.20 | 0.05 | 0.24 | |
| Outcome | Parameter | Estimate | 95% Confidence Interval | p-Value | |
|---|---|---|---|---|---|
| Interference | Intervention | 0.02 | −0.04 | 0.10 | 0.45 |
| Time (T4 vs. T1) | −0.02 | −0.08 | 0.03 | 0.45 | |
| Income (high vs. low) | −0.03 | −0.14 | 0.08 | 0.60 | |
| Education | 0.01 | −0.02 | 0.04 | 0.50 | |
| Function | Intervention | −0.04 | −0.16 | 0.08 | 0.52 |
| Time (T4 vs. T1) | −0.01 | −0.09 | 0.05 | 0.66 | |
| Income (high vs. low) | −0.06 | −0.25 | 0.12 | 0.47 | |
| Education | 0.02 | −0.03 | 0.08 | 0.39 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alrashdi, M.; Cervantes Mendez, M.J.; Farokhi, M.R. A Randomized Clinical Trial Preventive Outreach Targeting Dental Caries and Oral-Health-Related Quality of Life for Refugee Children. Int. J. Environ. Res. Public Health 2021, 18, 1686. https://doi.org/10.3390/ijerph18041686
Alrashdi M, Cervantes Mendez MJ, Farokhi MR. A Randomized Clinical Trial Preventive Outreach Targeting Dental Caries and Oral-Health-Related Quality of Life for Refugee Children. International Journal of Environmental Research and Public Health. 2021; 18(4):1686. https://doi.org/10.3390/ijerph18041686
Chicago/Turabian StyleAlrashdi, Murad, Maria Jose Cervantes Mendez, and Moshtagh R. Farokhi. 2021. "A Randomized Clinical Trial Preventive Outreach Targeting Dental Caries and Oral-Health-Related Quality of Life for Refugee Children" International Journal of Environmental Research and Public Health 18, no. 4: 1686. https://doi.org/10.3390/ijerph18041686
APA StyleAlrashdi, M., Cervantes Mendez, M. J., & Farokhi, M. R. (2021). A Randomized Clinical Trial Preventive Outreach Targeting Dental Caries and Oral-Health-Related Quality of Life for Refugee Children. International Journal of Environmental Research and Public Health, 18(4), 1686. https://doi.org/10.3390/ijerph18041686







