Decision-Making in Implantology—A Cross-Sectional Vignette-Based Study to Determine Clinical Treatment Routines for the Edentulous Atrophic Mandible
Abstract
1. Introduction
2. Materials and Methods
2.1. Structure of the Questionnaire
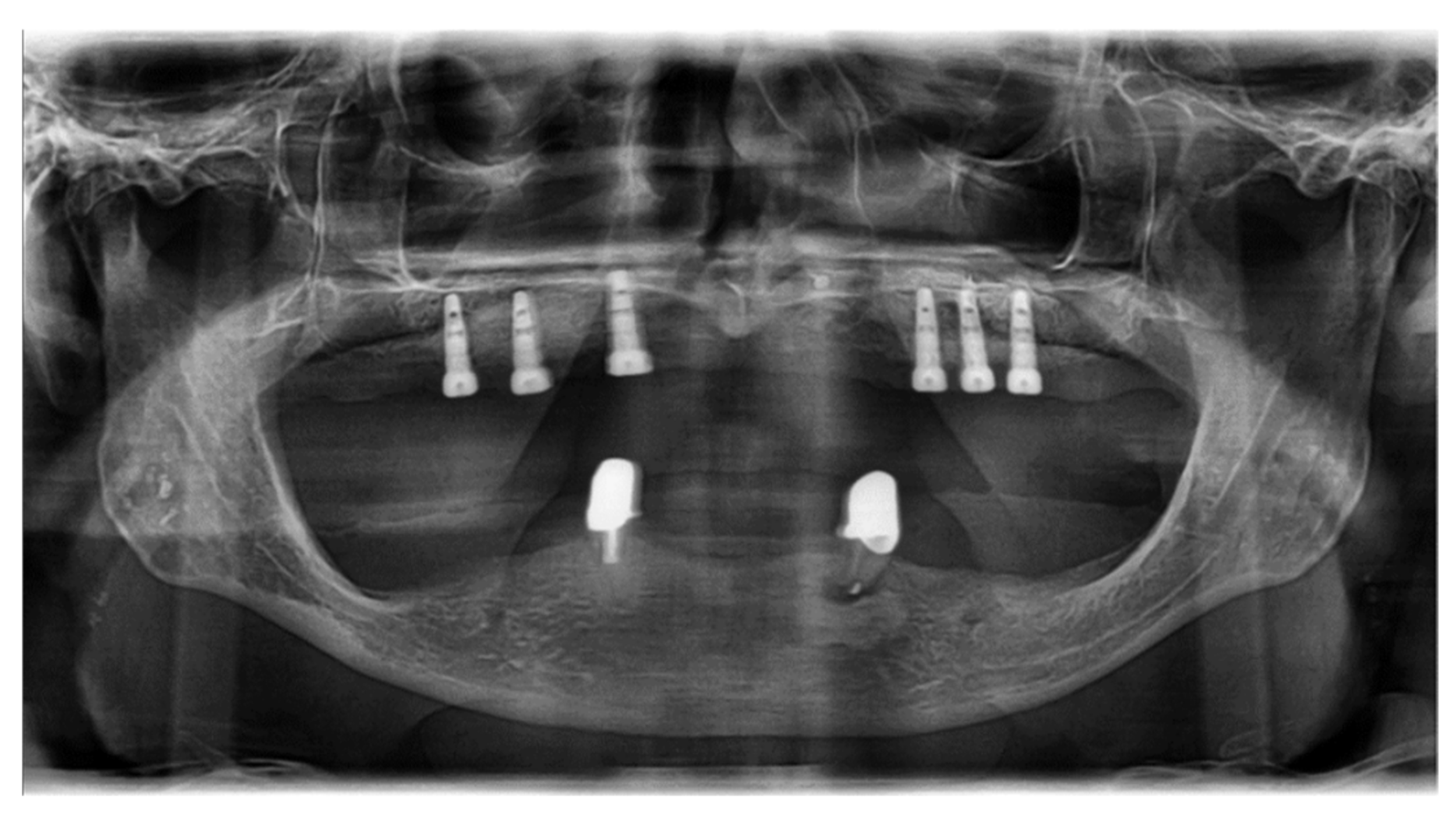
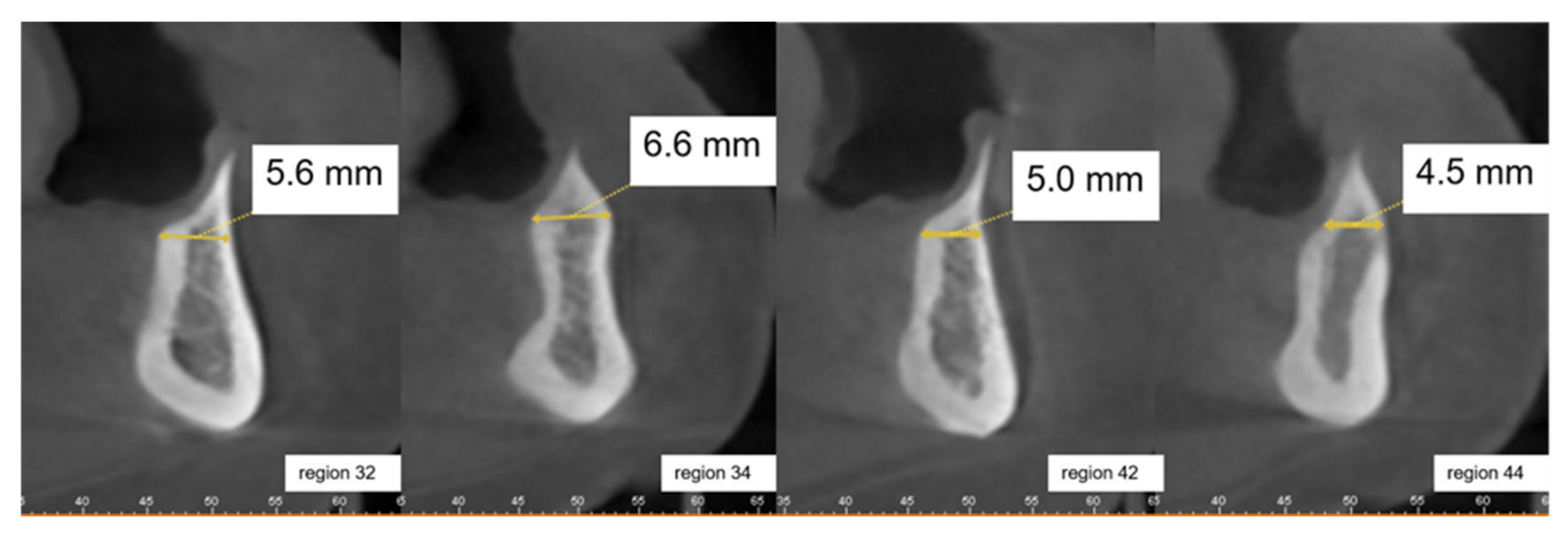
2.2. Clinical Case Vignettes
2.3. Variable Descriptors
2.4. Description of the Clinical Case Vignettes
2.5. Data Evaluation
3. Results
3.1. Physician-Related Characteristics
3.2. Outcome Scale for Case Vignette 1 (Edentulous Lower Jaw)
3.3. Outcome Scale for Case Vignette 2 (Edentulous Lower Jaw)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Manger, D.; Walshaw, M.; Fitzgerald, R.; Doughty, J.; Wanyonyi, K.; White, S.; Gallagher, J.E. Evidence summary: The relationship between oral health and pulmonary disease. Br. Dent. J. 2017, 222, 527–533. [Google Scholar] [CrossRef]
- Batty, G.D.; Jung, K.J.; Mok, Y.; Lee, S.J.; Back, J.H.; Lee, S.; Jee, S.H. Oral health and later coronary heart disease: Cohort study of one million people. Eur. J. Prev. Cardiol. 2018, 25, 598–605. [Google Scholar] [CrossRef] [PubMed]
- Preshaw, P.M.; Alba, A.L.; Herrera, D.; Jepsen, S.; Konstantinidis, A.; Makrilakis, K.; Taylor, R. Periodontitis and diabetes: A two-way relationship. Diabetology 2011, 55, 21–31. [Google Scholar] [CrossRef]
- Sroussi, H.Y.; Epstein, J.B.; Bensadoun, R.-J.; Saunders, D.P.; Lalla, R.V.; Migliorati, C.A.; Heaivilin, N.; Zumsteg, Z.S. Common oral complications of head and neck cancer radiation therapy: Mucositis, infections, saliva change, fibrosis, sensory dysfunctions, dental caries, periodontal disease, and osteoradionecrosis. Cancer Med. 2017, 6, 2918–2931. [Google Scholar] [CrossRef]
- Marconcini, S.; Denaro, M.; Cosola, S.; Gabriele, M.; Toti, P.; Mijiritsky, E.; Proietti, A.; Basolo, F.; Giammarinaro, E.; Covani, U. Myofibroblast Gene Expression Profile after Tooth Extraction in the Rabbit. Materials 2019, 12, 3697. [Google Scholar] [CrossRef]
- Nystrom, E.; Ahlqvist, J.; Gunne, J.; Kahnberg, K.E. 10-year follow-up of onlay bone grafts and implants in severely resorbed maxillae. Int. J. Oral Maxillofac. Surg. 2004, 33, 258–262. [Google Scholar] [CrossRef]
- Cordaro, L.; Torsello, F.; Morcavallo, S.; di Torresanto, V.M. Effect of bovine bone and collagen membranes on healing of mandibular bone blocks: A prospective randomized controlled study. Clin. Oral Implant. Res. 2011, 22, 1145–1150. [Google Scholar] [CrossRef] [PubMed]
- Araújo, M.G.; Sonohara, M.; Hayacibara, R.; Cardaropoli, G.; Lindhe, J. Lateral ridge augmentation by the use of grafts comprised of autologous bone or a biomaterial. An experiment in the dog. J. Clin. Periodontol. 2002, 29, 1122–1131. [Google Scholar] [CrossRef]
- Felice, P.; Marchetti, C.; Piattelli, A.; Pellegrino, G.; Checchi, V.; Worthington, H.V.; Esposito, M. Vertical ridge augmentation of the atrophic posterior mandible with interpositional block grafts: Bone from the iliac crest versus bovine anorganic bone. Eur. J. Oral Implant. 2008, 1, 183–198. [Google Scholar]
- Han, J.-Y.; Shin, S.-I.; Herr, Y.; Kwon, Y.-H.; Chung, J.-H. The effects of bone grafting material and a collagen membrane in the ridge splitting technique: An experimental study in dogs. Clin. Oral Implant. Res. 2011, 22, 1391–1398. [Google Scholar] [CrossRef]
- Thoma, D.S.; Maggetti, I.; Waller, T.; Hämmerle, C.H.F.; Jung, R.E. Clinical and patient-reported outcomes of implants placed in autogenous bone grafts and implants placed in native bone: A case–control study with a follow-up of 5–16 years. Clin. Oral Implant. Res. 2019, 30, 242–251. [Google Scholar] [CrossRef] [PubMed]
- Cruz, R.S.; Lemos, C.A.D.A.; Batista, V.E.D.S.; E Oliveira, H.F.F.; Gomes, J.M.D.L.; Pellizzer, E.P.; Verri, F.R. Short implants versus longer implants with maxillary sinus lift. A systematic review and meta-analysis. Braz. Oral Res. 2018, 32, e86. [Google Scholar] [CrossRef]
- Nadella, K.R.; Kodali, R.M.; Guttikonda, L.K.; Jonnalagadda, A. Osteoradionecrosis of the Jaws: Clinico-Therapeutic Management: A Literature Review and Update. J. Maxillofac. Oral Surg. 2015, 14, 891–901. [Google Scholar] [CrossRef]
- Schwarz, F.; Derks, J.; Monje, A.; Wang, H.L. Peri-implantitis. J. Periodontol. 2018, 89 (Suppl. 1), 267–290. [Google Scholar] [CrossRef] [PubMed]
- Meyle, J.; Casado, P.; Fourmousis, I.; Kumar, P.; Quirynen, M.; Salvi, G.E. General genetic and acquired risk factors, and prevalence of peri-implant diseases—Consensus report of working group 1. Int. Dent. J. 2019, 69, 3–6. [Google Scholar] [CrossRef]
- Vehemente, V.A.; Chuang, S.K.; Daher, S.; Muftu, A.; Dodson, T.B. Risk factors affecting dental implant survival. J. Oral Implant. 2002, 28, 74–81. [Google Scholar] [CrossRef]
- Goertz, O.; Kapalschinski, N.; Skorzinski, T.; Kolbenschlag, J.; Daigeler, A.; Hirsch, T.; Homann, H.H.; Muehlberger, T. Wound healing complications in smokers, non-smokers and after abstinence from smoking. Chirurg 2012, 83, 652–656. [Google Scholar] [CrossRef]
- Kourtis, S.G.; Sotiriadou, S.; Voliotis, S.; Challas, A. Private Practice Results of Dental Implants. Part I: Survival and Evaluation of Risk Factors—Part II: Surgical and Prosthetic Complications. Implant. Dent. 2004, 13, 373–385. [Google Scholar] [CrossRef]
- Cosola, S.; Marconcini, S.; Boccuzzi, M.; Fabris, G.B.M.; Covani, U.; Peñarrocha-Diago, M.; Peñarrocha-Oltra, D. Radiological Outcomes of Bone-Level and Tissue-Level Dental Implants: Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 6920. [Google Scholar] [CrossRef]
- Lalabonova, C.K. Impact of Dental Anxiety on the Decision to Have Implant Treatment. Folia Med. 2015, 57, 116–121. [Google Scholar] [CrossRef]
- Robra, B.P.; Kania, H.; Kuss, O.; Schonfisch, K.; Swart, E. Determinants of hospital admission—investigation by case vignettes. Gesundheitswesen 2006, 68, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Robra, B.P.; Kania, H.; Kuss, O.; Schönfisch, K.; Swart, E. Gleiche Erwartungen, unterschiedliche Dispositionen-niedergelassene Ärzte und Krankenhausärzte im Spiegel systematischer Fallvignetten. Krankenh. Rep. 2005, 1, 117–132. [Google Scholar]
- Peabody, J.W.; Luck, J.; Glassman, P.; Dresselhaus, T.R.; Lee, M. Comparison of vignettes, standardized patients, and chart abstraction: A prospective validation study of 3 methods for measuring quality. JAMA 2000, 283, 1715–1722. [Google Scholar] [CrossRef]
- Schmacke, N. Versorgungsforschung-auf dem Weg zu einer Theorie der “letzten Meile”. Gesundhökon. Qual. Manag. 2004, 9, 167–171. [Google Scholar] [CrossRef]
- Dresselhaus, T.R.; Peabody, J.; Luck, J.; Bertenthal, D. An evaluation of vignettes for predicting variation in the quality of preventive care. J. Gen. Intern. Med. 2004, 19, 1013–1018. [Google Scholar] [CrossRef]
- Peabody, J.W.; Luck, J.; Glassman, P.; Jain, S.; Hansen, J.; Spell, M.; Lee, M. Measuring the Quality of Physician Practice by Using Clinical Vignettes: A Prospective Validation Study. Ann. Intern. Med. 2004, 141, 771–780. [Google Scholar] [CrossRef] [PubMed]
- Converse, L.; Barrett, K.; Rich, E.; Reschovsky, J. Methods of Observing Variations in Physicians’ Decisions: The Opportunities of Clinical Vignettes. J. Gen. Intern. Med. 2015, 30, 586–594. [Google Scholar] [CrossRef]
- Tolstunov, L.; Hamrick, J.F.E.; Broumand, V.; Shilo, D.; Rachmiel, A. Bone Augmentation Techniques for Horizontal and Vertical Alveolar Ridge Deficiency in Oral Implantology. Oral Maxillofac. Surg. Clin. N. Am. 2019, 31, 163–191. [Google Scholar] [CrossRef] [PubMed]
- Korsch, M.; Reutter, C.; Walther, W. Resektion statt Augmentation. Implantologie 2013, 21, 419–426. [Google Scholar]
- Mehlkop, G.; Becker, R. The effects of monetary incentives on the response. Methoden Daten Anal. 2007, 1, 5–24. [Google Scholar]
- Meurer, W.J.; Johnson, P.; Brown, D.; Tsodikov, A.; Rowell, B.; Fagerlin, A.; Telian, S.A.; Damschroder, L.; An, L.C.; Morgenstern, L.B.; et al. An Educational Intervention for Acute Dizziness Care: A Randomized, Vignette-based Study. Otol Neurotol. 2019, 40, e830–e838. [Google Scholar] [CrossRef]
- Rousseau, A.; Rozenberg, P.; Perrodeau, E.; Ravaud, P. Variation in severe postpartum hemorrhage management: A national vignette-based study. PLoS ONE 2018, 13, e0209074. [Google Scholar] [CrossRef]
- Heidari, E.; Newton, J.T.; Andiappan, M.; Banerjee, A. The impact of dental phobia on care planning: A vignette study. Br. Dent. J. 2019, 226, 581–587. [Google Scholar] [CrossRef]
- Ahn, D.-H.; Kim, H.-J.; Joo, J.-Y.; Lee, J.-Y. Prevalence and risk factors of peri-implant mucositis and peri-implantitis after at least 7 years of loading. J. Periodontal Implant. Sci. 2019, 49, 397–405. [Google Scholar] [CrossRef]
- Curtis, D.A.; Lin, G.-H.; Fishman, A.; Sadowsky, S.J.; Daubert, D.M.; Kapila, Y.; Sharma, A.B.; Conte, G.J.; Yonemura, C.Y.; Marinello, C.P.; et al. Patient-Centered Risk Assessment in Implant Treatment Planning. Int. J. Oral Maxillofac. Implant. 2019, 34, 506–520. [Google Scholar] [CrossRef]
- VanDeWeghe, S.; Hawker, P.; De Bruyn, H. An Up to 12-Year Retrospective Follow-Up on Immediately Loaded, Surface-Modified Implants in the Edentulous Mandible. Clin. Implant. Dent. Relat. Res. 2015, 18, 323–331. [Google Scholar] [CrossRef]
- Rignon-Bret, C.; Wulfman, C.; Hadida, A.; Renouard, F.; Gourraud, P.A.; Naveau, A. Immediate Loading of Two Unsplinted Implants in Edentulous Patients with Mandibular Overdentures: A 10-year Retrospective Review of Patients from a Previously Conducted 1-year Cohort Study. Int. J. Oral Maxillofac. Implant. 2019, 34, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Rogulj, A.A.; Brzak, B.L.; Boras, V.V.; Brailo, V.; Milenovic, M.L.O. Oral complications of head and neck irradiation. Libri Oncol. 2017, 45, 89–93. [Google Scholar]
- Brown, D.; Evans, A.; Sándor, G.K. Hyperbaric oxygen therapy in the management of osteoradionecrosis of the mandible. Adv. Otorhinolaryngol. 1998, 54, 14–32. [Google Scholar] [CrossRef]
- Hasegawa, T.; Kawabata, S.; Takeda, D.; Iwata, E.; Saito, I.; Arimoto, S.; Kimoto, A.; Akashi, M.; Suzuki, H.; Komori, T. Survival of Brånemark System Mk III implants and analysis of risk factors associated with implant failure. Int. J. Oral Maxillofac. Surg. 2017, 46, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Stellingsma, K.; Vissink, A.; Meijer, H.; Kuiper, C.; Raghoebar, G. Implantology and the Severely Resorbed Edentulous Mandible. Crit. Rev. Oral Biol. Med. 2004, 15, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Baj, A.; Sollazzo, V.; Lauritano, D.; Candotto, V.; E Mancini, G.; Gianni, A.B. Lights and shadows of bone augmentation in severe resorbed mandible in combination with implant dentistry. J. Boil. Regul. Homeost. Agents 2016, 30, 177–182. [Google Scholar]
- Louis, P.J. Bone Grafting the Mandible. Dent. Clin. N. Am. 2011, 55, 673–695. [Google Scholar] [CrossRef] [PubMed]
- Bruschi, G.B.; Capparé, P.; Bravi, F.; Grande, N.; Gherlone, E.; Gastaldi, G.; Crespi, R. Radiographic Evaluation of Crestal Bone Level in Split-Crest and Immediate Implant Placement: Minimum 5-Year Follow-up. Int. J. Oral Maxillofac. Implant. 2016, 32, 114–120. [Google Scholar] [CrossRef]
- Korsch, M.; Kasprzyk, S.; Walther, W.; Bartols, A. Lateral alveolar ridge augmentation with autogenous block grafts fixed at a distance vs resorbable poly-D-L-lactide foil fixed at a distance: 5-year results of a single-blind, randomised controlled trial. Int. J. Oral Implantol. 2019, 12, 299–312. [Google Scholar]
- Nkenke, E.; Radespiel-Troger, M.; Wiltfang, J.; Schultze-Mosgau, S.; Winkler, G.; Neukam, F.W. Morbidity of harvesting of retromolar bone grafts: A prospective study. Clin. Oral Implant. Res. 2002, 13, 514–521. [Google Scholar] [CrossRef]
- De Groot, R.J.; Oomens, M.A.E.M.; Forouzanfar, T.; Schulten, E.A.J.M. Bone augmentation followed by implant surgery in the edentulous mandible: A systematic review. J. Oral Rehabil. 2018, 45, 334–343. [Google Scholar] [CrossRef] [PubMed]
- Guiol, J.; Campard, G.; Longis, J.; Hoornaert, A. Anterior mandibular bone augmentation techniques. Literature review. Rev. Stomatol. Chir. Maxillofac. Chir. Orale 2015, 116, 353–359. [Google Scholar]




| Case Vignette 1 | Case Vignette 2 | |
|---|---|---|
| n (%) | n (%) | |
| Combination 1 | 31 (27) | 29 (25) |
| Combination 2 | 35 (30) | 28 (24) |
| Combination 3 | 26 (22) | 35 (30) |
| Combination 4 | 25 (21) | 25 (21) |
| Regression Coefficient B | Standard Error | Forest | df | p-Value | Exp(B) | |
|---|---|---|---|---|---|---|
| Bone split | 0.189 | 0.249 | 0.575 | 1 | 0.448 | 1.208 |
| Bone block | 0.069 | 0.253 | 0.075 | 1 | 0.784 | 1.072 |
| Bone substitute material | −0.262 | 0.266 | 0.973 | 1 | 0.324 | 0.769 |
| Bone resection | 0.207 | 0.315 | 0.431 | 1 | 0.511 | 1.230 |
| Therapy recommended | 0.263 | 0.302 | 0.758 | 1 | 0.384 | 1.301 |
| Constant | −0.675 | 0.467 | 2.090 | 1 | 0.148 | 0.509 |
| Regression Coefficient B | Standard Error | Forest | df | p-Value | Exp(B) | |
|---|---|---|---|---|---|---|
| Bone split | 0.137 | 0.257 | 0.284 | 1 | 0.594 | 1.146 |
| Bone block | 0.532 | 0.268 | 3.951 | 1 | 0.047 | 1.702 |
| Bone substitute material | −0.556 | 0.280 | 3.953 | 1 | 0.047 | 0.574 |
| Bone resection | −0.337 | 0.323 | 1.091 | 1 | 0.296 | 0.714 |
| Therapy recommended | 0.217 | 0.316 | 0.473 | 1 | 0.491 | 1.243 |
| Constant | 0.533 | 0.469 | 1.294 | 1 | 0.255 | 1.704 |
| Regression Coefficient B | Standard Error | Forest | df | p-Value | Exp(B) | |
|---|---|---|---|---|---|---|
| Bone split | 0.323 | 0.265 | 1.482 | 1 | 0.223 | 1.381 |
| Bone block | −0.182 | 0.271 | 0.452 | 1 | 0.501 | 0.833 |
| Bone substitute material | 0.226 | 0.277 | 0.666 | 1 | 0.415 | 1.254 |
| Bone resection | −0.369 | 0.333 | 1.229 | 1 | 0.268 | 0.691 |
| Therapy recommended | −1.080 | 0.374 | 8.356 | 1 | 0.004 | 0.340 |
| Constant | 0.508 | 0.482 | 1.111 | 1 | 0.292 | 1.662 |
| Regression Coefficient B | Standard Error | Forest | df | p-Value | Exp(B) | |
|---|---|---|---|---|---|---|
| Bone split | 0.175 | 0.268 | 0.424 | 1 | 0.515 | 1.191 |
| Bone block | −0.438 | 0.380 | 1.332 | 1 | 0.248 | 0.645 |
| Bone substitute material | −0.303 | 0.257 | 1.396 | 1 | 0.237 | 0.738 |
| Bone resection | 0.777 | 0.416 | 3.495 | 1 | 0.062 | 2.175 |
| Therapy recommended | 0.175 | 0.282 | 0.387 | 1 | 0.534 | 1.191 |
| Constant | −0.987 | 0.574 | 2.960 | 1 | 0.085 | 0.373 |
| Regression Coefficient B | Standard Error | Forest | df | p-Value | Exp(B) | |
|---|---|---|---|---|---|---|
| Bone split | 0.607 | 0.276 | 4.829 | 1 | 0.028 | 1.835 |
| Bone block | 0.611 | 0.354 | 2.989 | 1 | 0.084 | 1.843 |
| Bone substitute material | −0.423 | 0.262 | 2.610 | 1 | 0.106 | 0.655 |
| Bone resection | 0.135 | 0.384 | 0.124 | 1 | 0.724 | 1.145 |
| Therapy recommended | −0.330 | 0.296 | 1.246 | 1 | 0.264 | 0.719 |
| Constant | −0.075 | 0.546 | 0.019 | 1 | 0.890 | 0.927 |
| Regression Coefficient B | Standard Error | Forest | df | p-Value | Exp(B) | |
|---|---|---|---|---|---|---|
| Bone split | −0.231 | 0.257 | 0.805 | 1 | 0.369 | 0.794 |
| Bone block | 0.386 | 0.334 | 1.337 | 1 | 0.248 | 1.472 |
| Bone substitute material | −0.307 | 0.247 | 1.544 | 1 | 0.214 | 0.735 |
| Bone resection | 0.153 | 0.371 | 0.171 | 1 | 0.679 | 1.166 |
| Therapy recommended | −0.117 | 0.279 | 0.176 | 1 | 0.675 | 0.890 |
| Constant | 0.393 | 0.534 | 0.540 | 1 | 0.462 | 1.481 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Korsch, M.; Walther, W.; Robra, B.-P.; Sahin, A.; Hannig, M.; Bartols, A. Decision-Making in Implantology—A Cross-Sectional Vignette-Based Study to Determine Clinical Treatment Routines for the Edentulous Atrophic Mandible. Int. J. Environ. Res. Public Health 2021, 18, 1596. https://doi.org/10.3390/ijerph18041596
Korsch M, Walther W, Robra B-P, Sahin A, Hannig M, Bartols A. Decision-Making in Implantology—A Cross-Sectional Vignette-Based Study to Determine Clinical Treatment Routines for the Edentulous Atrophic Mandible. International Journal of Environmental Research and Public Health. 2021; 18(4):1596. https://doi.org/10.3390/ijerph18041596
Chicago/Turabian StyleKorsch, Michael, Winfried Walther, Bernt-Peter Robra, Aynur Sahin, Matthias Hannig, and Andreas Bartols. 2021. "Decision-Making in Implantology—A Cross-Sectional Vignette-Based Study to Determine Clinical Treatment Routines for the Edentulous Atrophic Mandible" International Journal of Environmental Research and Public Health 18, no. 4: 1596. https://doi.org/10.3390/ijerph18041596
APA StyleKorsch, M., Walther, W., Robra, B.-P., Sahin, A., Hannig, M., & Bartols, A. (2021). Decision-Making in Implantology—A Cross-Sectional Vignette-Based Study to Determine Clinical Treatment Routines for the Edentulous Atrophic Mandible. International Journal of Environmental Research and Public Health, 18(4), 1596. https://doi.org/10.3390/ijerph18041596






