Polycystic Ovary Syndrome and Endometriosis as Reasons for Women’s Admission to Outpatient Specialist Care in Poland—A Retrospective Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- van der Zanden, M.; Nap, A.W. Knowledge of, and treatment strategies for, endometriosis among general practitioners. Reprod. Biomed. Online 2016, 32, 527–531. [Google Scholar] [CrossRef] [PubMed]
- Alimi, Y.; Iwanaga, J.; Loukas, M.; Tubbs, R.S. The Clinical Anatomy of Endometriosis: A Review. Cureus 2018, 10. [Google Scholar] [CrossRef]
- Moradi, M.; Parker, M.; Sneddon, A.; Lopez, V.; Ellwood, D. Impact of endometriosis on women’s lives: A qualitative study. BMC Womens Health 2014, 14. [Google Scholar] [CrossRef] [PubMed]
- Hållstam, A.; Stålnacke, B.M.; Svensén, C.; Löfgren, M. Living with painful endometriosis—A struggle for coherence. A qualitative study. Sex. Reprod. Healthc. 2018, 17, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Nnoaham, K.E.; Hummelshoj, L.; Webster, P.; d’Hooghe, T.; de Cicco Nardone, F.; de Cicco Nardone, C.; Jenkinson, C.; Kennedy, S.H.; Zondervan, K.T. Impact of endometriosis on quality of life and work productivity: A multicenter study across ten countries. Fertil. Steril. 2011, 96, 366–373.e8. [Google Scholar] [CrossRef] [PubMed]
- Moran, L.; Gibson-Helm, M.; Teede, H.; Deeks, A. Polycystic ovary syndrome: A biopsychosocial understanding in young women to improve knowledge and treatment options. J. Psychosom. Obstet. Gynecol. 2010, 31, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Lim, A.J.R.; Huang, Z.; Chua, S.E.; Kramer, M.S.; Yong, E.-L. Sleep Duration, Exercise, Shift Work and Polycystic Ovarian Syndrome-Related Outcomes in a Healthy Population: A Cross-Sectional Study. PLoS ONE 2016, 11, e0167048. [Google Scholar] [CrossRef] [PubMed]
- Williams, T.; Mortada, R.; Porter, S. Diagnosis and Treatment of Polycystic Ovary Syndrome. Am. Fam. Physician 2016, 94, 106–113. [Google Scholar]
- Gibson-Helm, M.; Teede, H.; Dunaif, A.; Dokras, A. Delayed diagnosis and a lack of information associated with dissatisfaction in women with Polycystic Ovary Syndrome. J. Clin. Endocrinol. Metab. 2017, 102, 604–612. [Google Scholar] [CrossRef] [PubMed]
- Simoens, S.; Dunselman, G.; Dirksen, C.; Hummelshoj, L.; Bokor, A.; Brandes, I.; Brodszky, V.; Canis, M.; Colombo, G.L.; DeLeire, T.; et al. The burden of endometriosis: Costs and quality of life of women with endometriosis and treated in referral centres. Hum. Reprod. 2012, 27, 1292–1299. [Google Scholar] [CrossRef] [PubMed]
- Dancet, E.A.; Apers, S.; Kremer, J.A.; Nelen, W.L.; Sermeus, W.; D’Hooghe, T.M. The patient-centeredness of endometriosis care and targets for improvement: A systematic review. Gynecol. Obstet. Investig. 2014, 78, 69–80. [Google Scholar] [CrossRef] [PubMed]
- Glover, I.; Novakovic, A.; Hunter, M.S. An exploration of the nature and causes of distress in women attending gynecology outpatient clinics. J. Psychosom. Obstet. Gynecol. 2002, 23, 237–248. [Google Scholar] [CrossRef] [PubMed]
- Bromber, P. The role and functioning of NFZ in the system of health protection. Zeszy. Naukowe Uniw. Szczec. Finans. Rynki Finans. Ubezpieczenia 2014, 65, 541–557. (In Polish) [Google Scholar]
- Ślęzak, D.; Żuratyński, P.; Nadolny, K.; Robakowska, M.; Kalis, A. Health System in Poland. Diagn. Lab. 2017, 53, 107–112. (In Polish) [Google Scholar]
- The Act of 27 October 2017 on Basic Health Care. Available online: http://www.ilo.org/dyn/natlex/natlex4.detail?p_lang=en&p_isn=105978&p_classification=15.01 (accessed on 22 December 2020).
- Kuszewski, K.; Czyżewski, M.; Sagan, A.; Świdrek, M.; Leśniewska, A.; Poznański, D.; Księżak, M.; Terka, A.; Księżak, M. Providing health services. In Outline of the Health Care System. Poland 2012; Golinowska, S., Ed.; National Health Fund: Warsaw, Poland, 2012; pp. 141–176. (In Polish) [Google Scholar]
- Central Statistical Office: NUTS Classification in Poland. Available online: https://stat.gov.pl/statystyka-regionalna/jednostki-terytorialne/klasyfikacja-nuts/klasyfikacja-nuts-w-polsce/ (accessed on 19 March 2020). (In Polish)
- Kupcewicz, E.; Grochans, E.; Mikla, M.; Kadučáková, H.; Jóźwik, M. Role of Global Self-Esteem in Predicting Life Satisfaction of Nursing Students in Poland, Spain and Slovakia. Int. J. Environ. Res. Public Health 2020, 17, 5392. [Google Scholar] [CrossRef]
- Rowlands, I.J.; Teede, H.; Lucke, J.; Dobson, A.J.; Mishra, G.D. Young women’s psychological distress after a diagnosis of polycystic ovary syndrome or endometriosis. Hum. Reprod. 2016, 31, 2072–2081. [Google Scholar] [CrossRef] [PubMed]
- Qian, X.; Wu, H.; Xi, X. Is There A Relationship between Polycystic Ovary Syndrome and Endometriosis? J. Reprod. Contracept. 2011, 22, 177–182. [Google Scholar] [CrossRef]
- De Graaff, A.A.; D’Hooghe, T.M.; Dunselman, G.A.; Dirksen, C.D.; Hummelshoj, L.; WERF EndoCost Consortium; Simoens, S. The significant effect of endometriosis on physical, mental and social wellbeing: Results from an international cross-sectional survey. Hum. Reprod. 2013, 28, 2677–2685. [Google Scholar] [CrossRef] [PubMed]
- Bień, A.; Rzońca, E.; Zarajczyk, M.; Wilkosz, K.; Wdowiak, A.; Iwanowicz-Palus, G. Quality of life in women with endometriosis: A cross-sectional survey. Qual. Life Res. 2020, 29, 2669–2677. [Google Scholar] [CrossRef] [PubMed]
- Lin, A.W.; Bergomi, E.J.; Dollahite, J.S.; Sobal, J.; Hoeger, K.M.; Lujan, M.E. Trust in physicians and medical experience beliefs differ between women with and without Polycystic Ovary Syndrome. J. Endocr. Soc. 2018, 2, 1001–1009. [Google Scholar] [CrossRef]
- Agarwal, S.K.; Chapron, C.; Giudice, L.C.; Laufer, M.R.; Leyland, N.; Missmer, S.A.; Singh, S.S.; Taylor, H.S. Clinical diagnosis of endometriosis: A call to action. ACOG 2019, 220, 354.e1–354.e12. [Google Scholar] [CrossRef]
- Hlimi, T. Association of anemia, pre-eclampsia and eclampsia with seasonality: A realist systematic review. Health Place 2015, 31, 180–192. [Google Scholar] [CrossRef]
- Kim, J.H.; Cheong, H.K. Epidemiologic trends and seasonality of scabies in South Korea, 2010–2017. Korean J. Parasitol. 2019, 57, 399–404. [Google Scholar] [CrossRef] [PubMed]
- Virág, K.; Nyári, T.A. Annual and seasonal trends in mortality rates from cardiovascular diseases in Hungary between 1984 and 2013. Cent. Eur. J. Public Health 2018, 26, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Kyrgios, I.; Giza, S.; Tsinopoulou, V.R.; Maggana, I.; Haidich, A.B.; Galli-Tsinopoulou, A. Seasonality of month of birth in children and adolescents with autoimmune thyroiditis: A continuing conundrum. J. Pediatr. Endocrinol. Metab. 2018, 31, 1123–1131. [Google Scholar] [CrossRef] [PubMed]
- Münster, E.; Letzel, S.; Passet-Wittig, J.; Schneider, N.F.; Schuhrke, B.; Seufert, R.; Zier, U. Who is the gate keeper for treatment in a fertility clinic in Germany?—Baseline results of a prospective cohort study (PinK study). BMC Pregnancy Childbirth 2018, 18. [Google Scholar] [CrossRef]
- Cooney, L.G.; Dokras, A. Beyond fertility: Polycystic ovary syndrome and long-term health. Fertil Steril. 2018, 110, 794–809. [Google Scholar] [CrossRef] [PubMed]
- Apers, S.; Dancet, E.A.F.; Aarts, J.W.M.; Kluivers, K.B.; D’Hooghe, T.M.; Nelen, W.L.D.M. The association between experiences with patient-centred care and health-related quality of life in women with endometriosis. Reprod. Biomed. Online 2018, 36, 197–205. [Google Scholar] [CrossRef] [PubMed]
- Young, K.; Fisher, J.; Kirkman, M. Endometriosis and fertility: Women’s accounts of healthcare. Hum. Reprod. 2016, 31, 554–562. [Google Scholar] [CrossRef] [PubMed]
- Lukas, I.; Kohl-Schwartz, A.; Geraedts, K.; Rauchfuss, M.; Wölfler, M.M.; Häberlin, F.; von Orelli, S.; Eberhard, M.; Imthurn, B.; Imesch, P.; et al. Satisfaction with medical support in women with endometriosis. PLoS ONE 2018, 13. [Google Scholar] [CrossRef]
- MacKichan, F.; Paterson, C.; Henley, W.E.; Britten, N. Self-care in people with long term health problems: A community-based survey. BMC Fam. Pract. 2011, 12. [Google Scholar] [CrossRef] [PubMed]
- Armour, M.; Sinclair, J.; Chalmers, K.J.; Smith, C.A. Self-management strategies amongst Australian women with endometriosis: A national online survey. BMC Complement. Altern. Med. 2019, 19. [Google Scholar] [CrossRef] [PubMed]
- Azevedo e Silva, G.; Valente, J.G.; Almeida, L.M.; Moura, E.C.; Malta, D.C. Tobacco smoking and level of education in Brazil, 2006. Rev. Saude Publica 2009, 43, 48–56. [Google Scholar] [PubMed]
- Tomazelli, J.G.; Silva, G.A.E. Breast cancer screening in Brazil: An assessment of supply and use of Brazilian National Health System health care network for the period 2010–2012. Epidemiol. Serv. Saúde 2017, 26, 713–724. [Google Scholar] [CrossRef]
- Carreno, I.; Bonilha, A.L.; Costa, J.S. Temporal evolution and spatial distribution of maternal death. Rev. Saude Publica 2014, 48, 662–670. [Google Scholar] [CrossRef] [PubMed]
- Wolf, W.M.; Wattick, R.A.; Kinkade, O.N.; Olfert, M.D. Geographical prevalence of Polycystic Ovary Syndrome as determined by region and race/ethnicity. Int. J. Environ. Res. Public Health 2018, 15, 2589. [Google Scholar] [CrossRef] [PubMed]
- Witchel, S.F.; Oberfield, S.E.; Peña, A.S. Polycystic Ovary Syndrome: Pathophysiology, presentation, and treatment with emphasis on adolescent girls. J. Endocr. Soc. 2019, 3, 1545–1573. [Google Scholar] [CrossRef] [PubMed]
- Rothenberg, S.S.; Beverley, R.; Barnard, E.; Baradaran-Shoraka, M.; Sanfilippo, J.S. Polycystic ovary syndrome in adolescents. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 48, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Ibáñez, L.; Oberfield, S.E.; Witchel, S.; Auchus, R.J.; Chang, R.J.; Codner, E.; Dabadghao, P.; Darendeliler, F.; Elbarbary, N.S.; Gambineri, A.; et al. An International Consortium Update: Pathophysiology, diagnosis, and treatment of polycystic ovarian syndrome in adolescence. Horm. Res. Paediatr. 2017, 88, 371–395. [Google Scholar] [CrossRef] [PubMed]
- Kamboj, M.K.; Bonny, A.E. Polycystic ovary syndrome in adolescence: Diagnostic and therapeutic strategies. Transl. Pediatr. 2017, 6, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Spritzer, P.M.; Motta, A.B. Adolescence and polycystic ovary syndrome: Current concepts on diagnosis and treatment. Int. J. Clin. Pract. 2015, 69, 1236–1246. [Google Scholar] [CrossRef]
- Matalliotakis, M.; Matalliotaki, C.; Trivli, A.; Zervou, M.I.; Kalogiannidis, I.; Tzardi, M.; Matalliotakis, I.; Arici, A.; Goulielmos, G.N. Keeping an eye on perimenopausal and postmenopausal endometriosis. Diseases 2019, 12, 29. [Google Scholar] [CrossRef] [PubMed]
- Yoldemir, T. Quality of life for women with endometriosis: Premenopausal and postmenopausal perspectives. Climacteric 2018, 21, 411–412. [Google Scholar] [CrossRef] [PubMed]
- Cope, A.G.; Van Buren, W.M.; Sheedy, S.P. Endometriosis in the postmenopausal female: Clinical presentation, imaging features, and management. Abdom. Radiol. 2020, 45. [Google Scholar] [CrossRef]
- Haas, D.; Wurm, P.; Schimetta, W.; Schabetsberger, K.; Shamiyeh, A.; Oppelt, P.; Binder, H. Endometriosis patients in the postmenopausal period: Pre-and postmenopausal factors influencing postmenopausal health. BioMed Res. Int. 2014, 2014. [Google Scholar] [CrossRef] [PubMed]
- Gemmell, L.C.; Webster, K.E.; Kirtley, S.; Vincent, K.; Zondervan, K.T.; Becker, C.M. The management of menopause in women with a history of endometriosis: A systematic review. Hum. Reprod. Update 2017, 23, 481–500. [Google Scholar] [CrossRef] [PubMed]
| Variables | PCOS 6044 (30.29) | Endometriosis 13,910 (69.71) | Total 19,954 (100.00) | p-Value |
|---|---|---|---|---|
| Age—n (%) | ||||
| Under 18 years old | 584 (9.66) | 76 (0.55) | 660 (3.31) | 0.0000 |
| 18–29 years old | 4014 (66.41) | 2891 (20.78) | 6905 (34.60) | |
| 30–39 years old | 1197 (19.80) | 4906 (35.78) | 6103 (30.59) | |
| 40–49 years old | 227 (3.76) | 4035 (29.01) | 4262 (21.36) | |
| 50–59 years old | 16 (0.26) | 1067 (7.67) | 1083 (5.43) | |
| Over 60 years old | 6 (0.10) | 935 (6.72) | 941 (4.72) | |
| Mean age (years old)—M (SD) | 25.31 (7.02) | 38.21 (10.79) | 34.25 (11.45) | 0.0000 |
| Year—n (%) | ||||
| 2016 | 2492 (41.23) | 6103 (43.87) | 8595 (43.07) | 0.0000 |
| 2017 | 1727 (28.57) | 4207 (30.24) | 5934 (29.74) | |
| 2018 | 1825 (30.20) | 3600 (25.88) | 5425 (27.19) | |
| Season of the year—n (%) | ||||
| Spring | 1740 (28.79) | 3781 (27.18) | 5521 (27.67) | 0.0014 |
| Summer | 1388 (22.96) | 3037 (21.83) | 4425 (22.18) | |
| Autumn | 1389 (22.98) | 3245 (23.33) | 4634 (23.22) | |
| Winter | 1527 (25.26) | 3847 (27.66) | 5374 (26.93) | |
| Place of treatment—n (%) | ||||
| City | 5897 (97.57) | 13,098 (94.16) | 18,995 (95.19) | 0.0000 |
| Village | 147 (2.43) | 812 (5.84) | 959 (4.81) | |
| Type of clinic—n (%) | ||||
| Obstetrics and gynaecology clinic | 3579 (59.22) | 13,214 (95.00) | 16,793 (84.16) | 0.0000 |
| Endocrinology clinic | 2445 (40.45) | 61 (0.44) | 2506 (12.56) | |
| Another clinic | 20 (0.33) | 635 (4.57) | 655 (3.28) | |
| Mode of admission—n (%) | ||||
| No referral | 3501 (57.93) | 13,227 (95.09) | 16,728 (83.83) | 0.0000 |
| With referral | 2543 (42.07) | 683 (4.91) | 3226 (16.17) | |
| Number of visits—n (%) | ||||
| 1 visit | 2036 (33.69) | 5557 (39.95) | 7593 (38.05) | 0.0000 |
| 2–3 visits | 2091 (34.60) | 4172 (29.99) | 6263 (31.39) | |
| 4–5 visits | 960 (15.88) | 1824 (13.11) | 2784 (13.95) | |
| 6 or more visits | 957 (15.83) | 2357 (16.94) | 3314 (16.61) | |
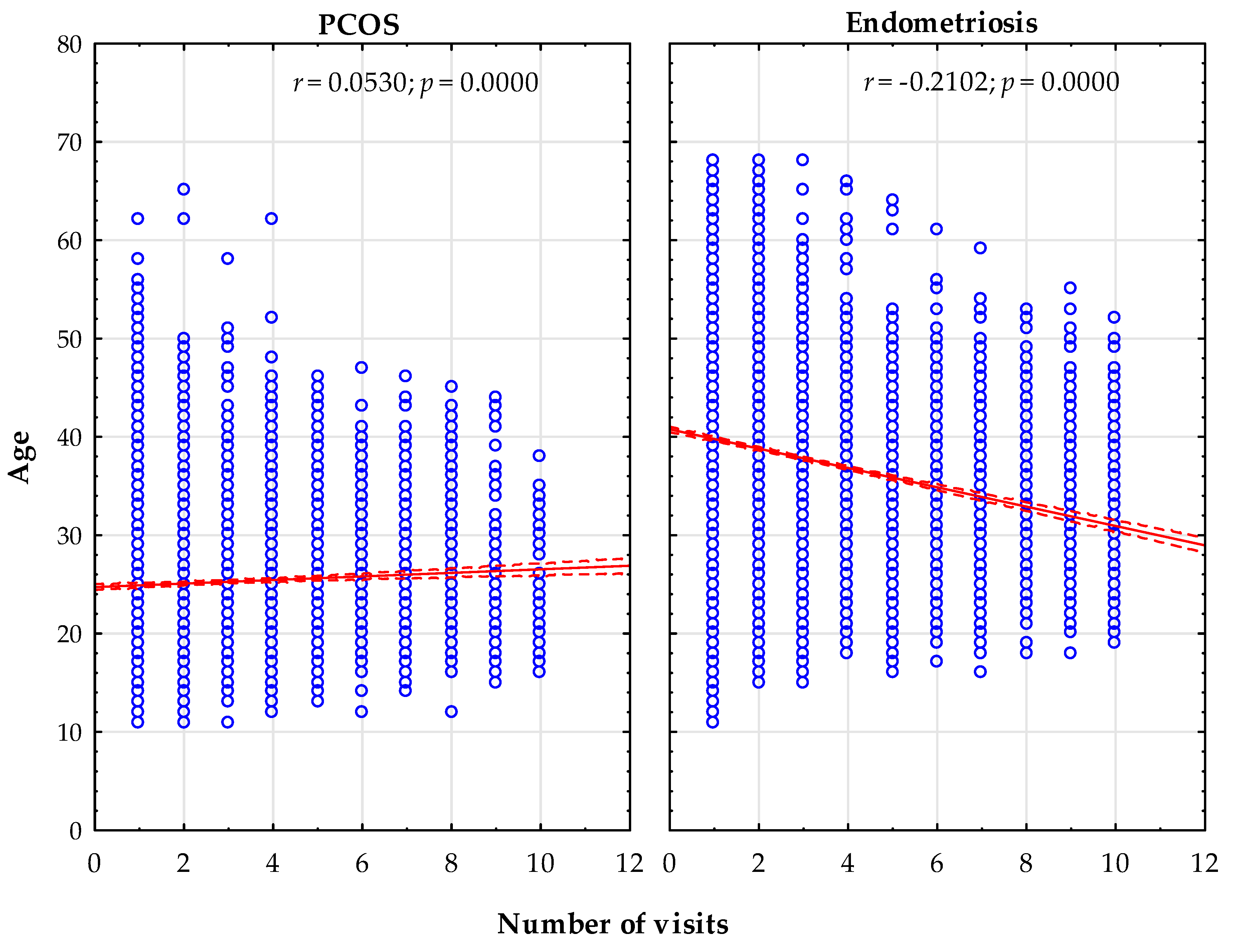
| Number of visits—M (SD) | 3.04 (2.43) | 2.96 (2.61) | 2.99 (2.55) | 0.0000 |
| Macroregion of residence—n (%) | ||||
| South Macroregion | 1378 (22.80) | 2862 (20.58) | 4240 (21.25) | 0.0000 |
| South-West Macroregion | 856 (14.16) | 902 (6.48) | 1758 (8.81) | |
| North-West Macroregion | 1034 (17.11) | 1940 (13.95) | 2974 (14.90) | |
| North Macroregion | 545 (9.02) | 2379 (17.10) | 2924 (14.65) | |
| Central Macroregion | 566 (9.36) | 1810 (13.01) | 2376 (11.91) | |
| East Macroregion | 1064 (17.60) | 2394 (17.21) | 3458 (17.33) | |
| Mazowieckie Province Macroregion | 601 (9.94) | 1623 (11.67) | 2224 (11.15) | |
| Macroregion of treatment—n (%) | ||||
| South Macroregion | 1439 (23.81) | 2848 (20.47) | 4287 (21.48) | 0.0000 |
| South-West Macroregion | 853 (14.11) | 897 (6.45) | 1750 (8.77) | |
| North-West Macroregion | 1084 (17.94) | 1927 (13.85) | 3011 (15.09) | |
| North Macroregion | 480 (7.94) | 2377 (17.09) | 2857 (14.32) | |
| Central Macroregion | 519 (8.59) | 1809 (13.01) | 2328 (11.67) | |
| East Macroregion | 1045 (17.29) | 2389 (17.17) | 3434 (17.21) | |
| Mazowieckie Province Macroregion | 624 (10.32) | 1663 (11.96) | 2287 (11.46) | |
| Treatment in the macroregion of residence—n (%) | ||||
| Yes | 5476 (90.60) | 13,277 (95.45) | 18,753 (93.98) | 0.0000 |
| No | 568 (9.40) | 633 (4.55) | 1201 (6.02) | |
| Variables | PCOS | ||
|---|---|---|---|
| OR | 95% CI | p-Value | |
| Age (reference group: 18–29 years old) | |||
| Under 18 years old | 5.53 | 4.34–7.06 | 0.0000 |
| 30–39 years old | 0.17 | 0.16–0.19 | 0.0000 |
| 40–49 years old | 0.04 | 0.04–0.05 | 0.0000 |
| 50–59 years old | 0.01 | 0.01–0.02 | 0.0000 |
| Over 60 years old | 0.01 | 0.00–0.01 | 0.0000 |
| Macroregion of residence (reference group: Mazowieckie Province Macroregion) | |||
| South Macroregion | 1.30 | 1.16–1.46 | 0.0000 |
| South-West Macroregion | 2.56 | 2.25–2.93 | 0.0000 |
| North-West Macroregion | 1.44 | 1.28–1.62 | 0.0000 |
| North Macroregion | 0.62 | 0.54–0.71 | 0.0000 |
| Central Macroregion | 0.84 | 0.74–0.97 | 0.0127 |
| East Macroregion | 1.20 | 1.07–1.35 | 0.0025 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rzońca, E.; Kosowski, A.; Bień, A.; Gotlib, J.; Wejnarski, A.; Jarzębowska, M.; Gałązkowski, R.; Rzońca, P. Polycystic Ovary Syndrome and Endometriosis as Reasons for Women’s Admission to Outpatient Specialist Care in Poland—A Retrospective Analysis. Int. J. Environ. Res. Public Health 2021, 18, 1442. https://doi.org/10.3390/ijerph18041442
Rzońca E, Kosowski A, Bień A, Gotlib J, Wejnarski A, Jarzębowska M, Gałązkowski R, Rzońca P. Polycystic Ovary Syndrome and Endometriosis as Reasons for Women’s Admission to Outpatient Specialist Care in Poland—A Retrospective Analysis. International Journal of Environmental Research and Public Health. 2021; 18(4):1442. https://doi.org/10.3390/ijerph18041442
Chicago/Turabian StyleRzońca, Ewa, Arkadiusz Kosowski, Agnieszka Bień, Joanna Gotlib, Arkadiusz Wejnarski, Marta Jarzębowska, Robert Gałązkowski, and Patryk Rzońca. 2021. "Polycystic Ovary Syndrome and Endometriosis as Reasons for Women’s Admission to Outpatient Specialist Care in Poland—A Retrospective Analysis" International Journal of Environmental Research and Public Health 18, no. 4: 1442. https://doi.org/10.3390/ijerph18041442
APA StyleRzońca, E., Kosowski, A., Bień, A., Gotlib, J., Wejnarski, A., Jarzębowska, M., Gałązkowski, R., & Rzońca, P. (2021). Polycystic Ovary Syndrome and Endometriosis as Reasons for Women’s Admission to Outpatient Specialist Care in Poland—A Retrospective Analysis. International Journal of Environmental Research and Public Health, 18(4), 1442. https://doi.org/10.3390/ijerph18041442










