The Effectiveness of a Board Game-Based Oral Hygiene Education Program on Oral Hygiene Knowledge and Plaque Index of Adults with Intellectual Disability: A Pilot Study
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Study Population
2.3. Ethical Approval
2.4. Assessment
2.4.1. Oral Health Knowledge
2.4.2. Plaque Index
2.5. Intervention
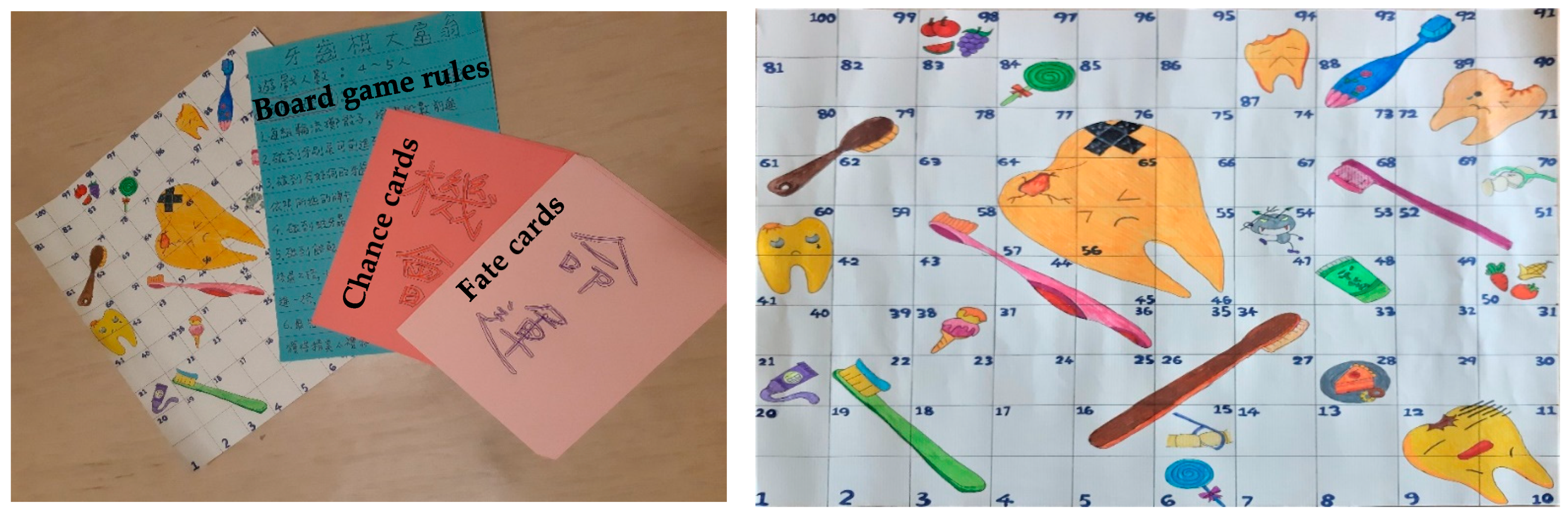
2.5.1. Development of the Board Game
2.5.2. Implementation of the Board Game
2.6. Statistical Analysis
2.7. Ethical Approval
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Kancherla, V.; Braun, K.V.N.; Yeargin-Allsopp, M. Dental care among young adults with intellectual disability. Res. Dev. Disabil. 2013, 34, 1630–1641. [Google Scholar] [CrossRef] [PubMed]
- McGrath, C.; Zhou, N.; Wong, H.M. A systematic review and meta-analysis of dental plaque control among children and adolescents with intellectual disabilities. J. Appl. Res. Intellect. Disabil. 2019, 32, 522–532. [Google Scholar] [CrossRef] [PubMed]
- Barry Waldman, H.; Perlman, S.P.; Swerdloff, M. What if dentists did not treat people with disabilities? J. Dent. Child. 1998, 65, 96–101. [Google Scholar]
- Wilson, K. Treatment accessibility for physically and mentally handicapped people--a review of the literature. Community Dent. Health 1992, 9, 187–192. [Google Scholar] [PubMed]
- Anders, P.L.; Davis, E.L. Oral health of patients with intellectual disabilities: A systematic review. Spec. Care Dentist. 2010, 30, 110–117. [Google Scholar] [CrossRef]
- Zhou, N.; Wong, H.M.; Wen, Y.F.; McGrath, C. Oral health status of children and adolescents with intellectual disabilities: A systematic review and meta-analysis. Dev. Med. Child Neurol. 2017, 59, 1019–1026. [Google Scholar] [CrossRef]
- Liu, H.-Y.; Huang, S.-T.; Hsuao, S.-Y.; Chen, C.-C.; Hu, W.-C.; Yen, Y.-Y. Dental caries associated with dietary and toothbrushing habits of 6-to 12-year-old mentally retarded children in Taiwan. J. Dent. Sci. 2009, 4, 61–74. [Google Scholar] [CrossRef]
- Liu, H.-Y.; Chen, C.-C.; Hu, W.-C.; Tang, R.-C.; Chen, C.-C.; Tsai, C.-C.; Huang, S.-T. The impact of dietary and tooth-brushing habits to dental caries of special school children with disability. Res. Dev. Disabil. 2010, 31, 1160–1169. [Google Scholar] [CrossRef]
- Yao, J.H.; Chen, H.H.; Chi, L.Y.; Hunag, Y.H. Oral Health Status and Treatment Needs of People with Disabilities at Iinstitutions in Taiwan 2013. J. Family Dent. 2017, 12, 4–13. [Google Scholar]
- Ministry of Health and Welfare. Oral Health Survey of Adults and Elders in Taiwan. Available online: https://dep.mohw.gov.tw/DOMHAOH/cp-486-39243-107.html (accessed on 26 November 2020).
- Yen, S.-M.; Kung, P.-T.; Chiu, L.-T.; Tsai, W.-C. Related factors and use of free preventive health services among adults with intellectual disabilities in Taiwan. BMC Health Serv. Res. 2014, 14, 248. [Google Scholar] [CrossRef]
- Kelly, G. How do intellectual disabilities affect oral health? Evid. Based Dent. 2020, 21, 26–27. [Google Scholar] [CrossRef] [PubMed]
- Petrovic, B.B.; Peric, T.O.; Markovic, D.L.; Bajkin, B.B.; Petrovic, D.; Blagojevic, D.B.; Vujkov, S. Unmet oral health needs among persons with intellectual disability. Res. Dev. Disabil. 2016, 59, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.-C.; Kung, P.-T.; Su, H.-P.; Yen, S.-M.; Chiu, L.-T.; Tsai, W.-C. Utilization of tooth filling services by people with disabilities in Taiwan. Int. J. Equity Health 2016, 15, 58. [Google Scholar] [CrossRef] [PubMed]
- Waldron, C.; Nunn, J.; Phadraig, C.M.G.; Comiskey, C.; Guerin, S.; van Harten, M.T.; Donnelly-Swift, E.; Clarke, M.J. Oral hygiene interventions for people with intellectual disabilities. Cochrane Database Syst. Rev. 2019, 5, Cd012628. [Google Scholar] [CrossRef] [PubMed]
- Nakre, P.D.; Harikiran, A. Effectiveness of oral health education programs: A systematic review. J. Int. Soc. Prev. Community Dent. 2013, 3, 103. [Google Scholar] [CrossRef]
- Avenali, L.; Guerra, F.; Cipriano, L.; Corridore, D.; Ottolenghi, L. Disabled patients and oral health in Rome, Italy: Long-term evaluation of educational initiatives. Ann. Stomatol. 2011, 2, 25–30. [Google Scholar]
- Hartwig, A.D.; Stuermer, V.M.; da Silva-Junior, I.F.; Schardosim, L.R.; Azevedo, M.S. Effectiveness of an oral health educational intervention for individuals with special health care needs from a southern Brazilian city. Spec. Care Dentist. 2017, 37, 246–252. [Google Scholar] [CrossRef]
- Makuch, A.; Reschke, K. Playing games in promoting childhood dental health. Patient Educ. Couns. 2001, 43, 105–110. [Google Scholar] [CrossRef]
- Maheswari, U.N.; Asokan, S.; Asokan, S.; Kumaran, S.T. Effects of conventional vs game-based oral health education on children’s oral health-related knowledge and oral hygiene status—A prospective study. Oral Health Prev. Dent. 2014, 12, 331–336. [Google Scholar]
- GeethaPriya, P.; Asokan, S.; Kandaswamy, D.; Shyam, S. Impact of different modes of school dental health education on oral health-related knowledge, attitude and practice behaviour: An interventional study. Eur. Arch Paediatr. Dent. 2020, 21, 347–354. [Google Scholar] [CrossRef]
- Kourakli, M.; Altanis, I.; Retalis, S.; Boloudakis, M.; Zbainos, D.; Antonopoulou, K. Towards the improvement of the cognitive, motoric and academic skills of students with special educational needs using Kinect learning games. Int. J. Child Comput. Interact. 2017, 11, 28–39. [Google Scholar] [CrossRef]
- Treher, E. Learning with Board Games. In Play for Performance. Tools for Learning and Retention. The Learning Key Inc. 2011. Available online: https://thelearningkey.com/pdf/Board_Games_TLKWhitePaper_May16_2011.pdf (accessed on 26 November 2020).
- Bartfay, W.J.; Bartfay, E. Promoting health in schools through a board game. West. J. Nurs. Res. 1994, 16, 438–446. [Google Scholar] [CrossRef] [PubMed]
- Klein, J.D.; Freitag, E. Effects of using an instructional game on motivation and performance. J. Educ. Res. 1991, 84, 303–308. [Google Scholar] [CrossRef]
- Klein, J.D. Effect of instructional gaming and reentry status on performance and motivation. Contemp. Educ. Psychol. 1992, 17, 364–370. [Google Scholar] [CrossRef]
- Wilde, J. The effects of the Let’s Get Rational board game on rational thinking, depression, and self-acceptance in adolescents. J. Ration. Emot. Cogn. Behav. Ther. 1994, 12, 189–196. [Google Scholar] [CrossRef]
- Aboalshamat, K.; Khayat, A.; Halwani, R.; Bitan, A.; Alansari, R. The effects of gamification on antimicrobial resistance knowledge and its relationship to dentistry in Saudi Arabia: A randomized controlled trial. BMC Public Health 2020, 20, 1–9. [Google Scholar] [CrossRef]
- Caldwell, M.L. Parents, board games, and mathematical learning. Teach. Child. Math. 1998, 4, 365–368. [Google Scholar] [CrossRef]
- Selvidge, E. Journey to Egypt: A board game. Montessori Life 2006, 18, 36. [Google Scholar]
- Siegler, R.S.; Ramani, G.B. Playing linear numerical board games promotes low-income children’s numerical development. Dev. Sci. 2008, 11, 655–661. [Google Scholar] [CrossRef]
- Ramani, G.B.; Siegler, R.S. Promoting broad and stable improvements in low-income children’s numerical knowledge through playing number board games. Child Dev. 2008, 79, 375–394. [Google Scholar] [CrossRef]
- Boat, T.F.; Wu, J.T. Clinical characteristics of intellectual disabilities. In Mental Disorders and Disabilities among Low-Income Children; National Academies Press: Washington, DC, USA, 2015. [Google Scholar]
- Leahy, W.; Fuzy, J.L.; Grafe, J. Providing Home Care: A Textbook for Home Health Aides; Hartman Publishing Inc.: Albuquerque, NM, USA, 2004. [Google Scholar]
- Binkley, C.J.; Johnson, K.W.; Abadi, M.; Thompson, K.; Shamblen, S.R.; Young, L.; Zaksek, B. Improving the oral health of residents with intellectual and developmental disabilities: An oral health strategy and pilot study. Eval. Program Plann. 2014, 47, 54–63. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, T.J.; Drake, R.B.; Naylor, J.E. The plaque control record. J. Periodontol. 1972, 43, 38. [Google Scholar] [CrossRef]
- Malik, A.; Sabharwal, S.; Kumar, A.; Samant, P.S.; Singh, A.; Pandey, V.K. Implementation of game-based Oral health education vs conventional Oral health education on Children’s Oral health-related knowledge and Oral hygiene status. Int. J. Clin. Pediatr. Dent. 2017, 10, 257. [Google Scholar]
- Faulks, D.; Hennequin, M. Evaluation of a long-term oral health program by carers of children and adults with intellectual disabilities. Spec. Care Dentist. 2000, 20, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Ningrum, V.; Wang, W.-C.; Liao, H.-E.; Bakar, A.; Shih, Y.-H. A special needs dentistry study of institutionalized individuals with intellectual disability in West Sumatra Indonesia. Sci. Rep. 2020, 10, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.R.; Apple, R.; Kanungo, S.; Akkal, A. Intellectual disability: Definitions, evaluation and principles of treatment. Pediatr. Med. 2018, 1, 11. [Google Scholar] [CrossRef]
- Katz, G.; Lazcano-Ponce, E. Intellectual disability: Definition, etiological factors, classification, diagnosis, treatment and prognosis. Salud Publica Mex. 2008, 50, 132–141. [Google Scholar] [CrossRef]
- Gudjonsson, G.H.; Henry, L. Child and adult witnesses with intellectual disability: The importance of suggestibility. Legal. Criminol. Psychol. 2003, 8, 241–252. [Google Scholar] [CrossRef]
- Drew, C.J.; Logan, D.R.; Hardman, M.L. Mental Retardation: A Life Cycle Approach; Times Mirror/Mostle College Publishing: St. Louis, MO, USA, 1984. [Google Scholar]
- Schultz, J.E. Depth of processing by mentally retarded and MA-matched nonretarded individuals. Am. J. Ment. Defic. 1983, 88, 307–313. [Google Scholar]
- Carr, J. Stability and change in cognitive ability over the life span: A comparison of populations with and without Down’s syndrome. J. Intellect. Disabil. Res. 2005, 49, 915–928. [Google Scholar] [CrossRef]
- Couzens, D.; Haynes, M.; Cuskelly, M. Individual and environmental characteristics associated with cognitive development in Down syndrome: A longitudinal study. J. Appl. Res. Intellect. Disabil. 2012, 25, 396–413. [Google Scholar] [CrossRef] [PubMed]
- Westling, D.L.; Fox, L.; Carter, E.W. Teaching Students with Severe Disabilities, 2nd ed.; Merrill/Prentice Hall: Upper Saddle River, NJ, USA, 2000. [Google Scholar]
- Ebel, S.; Blättermann, H.; Weik, U.; Margraf-Stiksrud, J.; Deinzer, R. High plaque levels after thorough toothbrushing: What impedes efficacy? JDR Clin. Trans. Res. 2019, 4, 135–142. [Google Scholar] [CrossRef] [PubMed]
| Variable | N | Oral Health Related Knowledge Score | Plaque Index | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control Phase | p-Value | Intervention Phase | p-Value | Control Phase | p-Value | Intervention Phase | p-Value | ||||||
| Mean | (SD) | Mean | (SD) | Mean | (SD) | Mean | (SD) | ||||||
| Gender | |||||||||||||
| Male | 18 | 14.44 | (4.53) | 0.800 | 13.75 | (4.37) | 0.848 | 86.94 | (19.52) | 0.340 | 80.25 | (17.07) | 0.323 |
| Female | 24 | 14.13 | (3.59) | 14.00 | (3.49) | 80.29 | (23.81) | 73.00 | (27.98) | ||||
| Severity of disability | |||||||||||||
| Moderate | 25 | 15.32 | (3.20) | 0.035 | 14.95 | (3.06) | 0.040 | 81.92 | (22.35) | 0.669 | 73.50 | (26.45) | 0.425 |
| Severe | 17 | 12.71 | (4.55) | 12.33 | (4.42) | 84.94 | (22.21) | 79.93 | (20.03) | ||||
| Age group | |||||||||||||
| 20–44 years old | 30 | 14.67 | (3.96) | 0.302 | 14.32 | (3.78) | 0.236 | 82.70 | (22.96) | 0.840 | 76.04 | (23.26) | 0.980 |
| ≥45 years old | 12 | 13.25 | (3.98) | 12.56 | (3.94) | 84.25 | (20.61) | 75.82 | (27.35) | ||||
| Variable | Baseline | p-Value | 1st Post-Test | p-Value | 2nd Post-Test | p-Value | 3rd Post-Test | p-Value | Difference Between Pre-Test and 3rd Post-Tests | p-Value | % of Improvement | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | (SD) | Mean | (SD) | Mean | (SD) | Mean | (SD) | Mean | (SD) | |||||||
| Oral health related knowledge score | ||||||||||||||||
| Intervention phase | 14.26 | (4.08) | 0.995 | 15.87 | (3.89) | 0.019 | 17.08 | (4.15) | 0.003 | 17.97 | (4.34) | <0.001 | 4.31 | (3.42) | <0.001 | 42.29 |
| Control phase | 14.26 | (3.97) | 13.61 | (4.05) | 14.23 | (4.06) | 13.89 | (3.84) | −0.24 | (0.98) | −1.34 | |||||
| Plaque index | ||||||||||||||||
| Intervention phase | 75.97 | (24.11) | 0.166 | 63.03 | (30.51) | 0.050 | 34.65 | (28.91) | <0.001 | 48.00 | (30.13) | <0.001 | −30.06 | (30.03) | <0.001 | −33.28 |
| Control phase | 83.14 | (22.07) | 75.94 | (22.70) | 77.64 | (23.14) | 78.78 | (21.08) | −4.57 | (18.58) | −1.40 | |||||
| Variable | Term | Estimate | SE | t Ratio | 95%CI | p-Value | R2 | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Oral health related knowledge score | ||||||||
| Group | Intervention group vs. Control group | 4.55 | 0.59 | 7.77 | 3.40 | 5.70 | <0.001 | 0.459 |
| Plaque index | ||||||||
| Group | Intervention group vs. Control group | −25.49 | 5.83 | −4.37 | −36.91 | −14.07 | <0.001 | 0.212 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, H.-Y.; Chen, P.-H.; Chen, W.-J.; Huang, S.-S.; Chen, J.-H.; Yao, C.-T. The Effectiveness of a Board Game-Based Oral Hygiene Education Program on Oral Hygiene Knowledge and Plaque Index of Adults with Intellectual Disability: A Pilot Study. Int. J. Environ. Res. Public Health 2021, 18, 946. https://doi.org/10.3390/ijerph18030946
Liu H-Y, Chen P-H, Chen W-J, Huang S-S, Chen J-H, Yao C-T. The Effectiveness of a Board Game-Based Oral Hygiene Education Program on Oral Hygiene Knowledge and Plaque Index of Adults with Intellectual Disability: A Pilot Study. International Journal of Environmental Research and Public Health. 2021; 18(3):946. https://doi.org/10.3390/ijerph18030946
Chicago/Turabian StyleLiu, Hsiu-Yueh, Ping-Ho Chen, Wun-Jyun Chen, Shan-Shan Huang, Jen-Hao Chen, and Ching-Teng Yao. 2021. "The Effectiveness of a Board Game-Based Oral Hygiene Education Program on Oral Hygiene Knowledge and Plaque Index of Adults with Intellectual Disability: A Pilot Study" International Journal of Environmental Research and Public Health 18, no. 3: 946. https://doi.org/10.3390/ijerph18030946
APA StyleLiu, H.-Y., Chen, P.-H., Chen, W.-J., Huang, S.-S., Chen, J.-H., & Yao, C.-T. (2021). The Effectiveness of a Board Game-Based Oral Hygiene Education Program on Oral Hygiene Knowledge and Plaque Index of Adults with Intellectual Disability: A Pilot Study. International Journal of Environmental Research and Public Health, 18(3), 946. https://doi.org/10.3390/ijerph18030946






