Efficacy of an Intervention to Reduce Stigma Beliefs and Attitudes among Primary Care and Mental Health Professionals: Two Cluster Randomised-Controlled Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Co-Creation Process
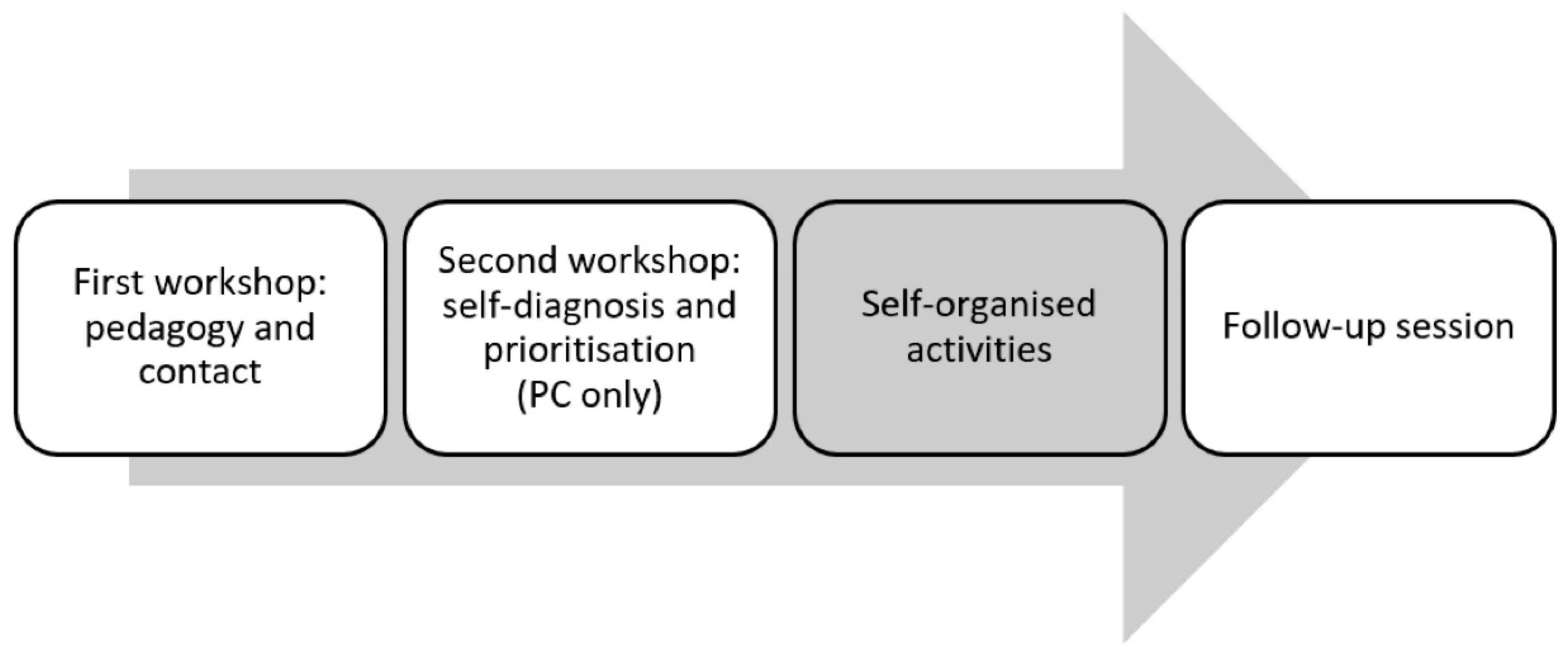
2.2. Awareness Interventions
2.2.1. Training Workshop
First Block: Mental Health and Mental Illness
Second Block: Stigma and Discrimination
Third Block: Healthcare and Primary Care/Mental Health Care
Fourth Block: Fighting Stigma
2.2.2. Self-Diagnosis Session
2.2.3. Follow-Up Session
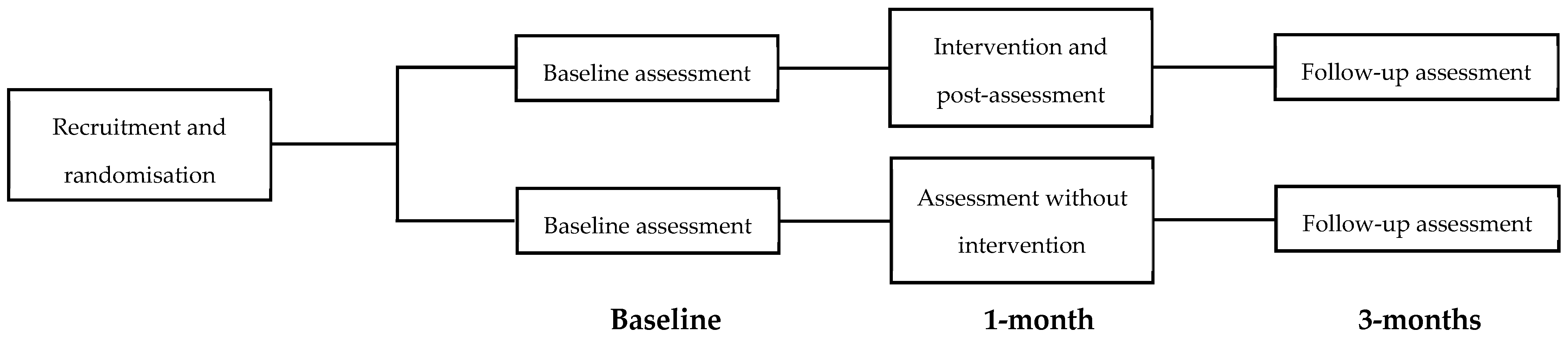
2.3. Procedure
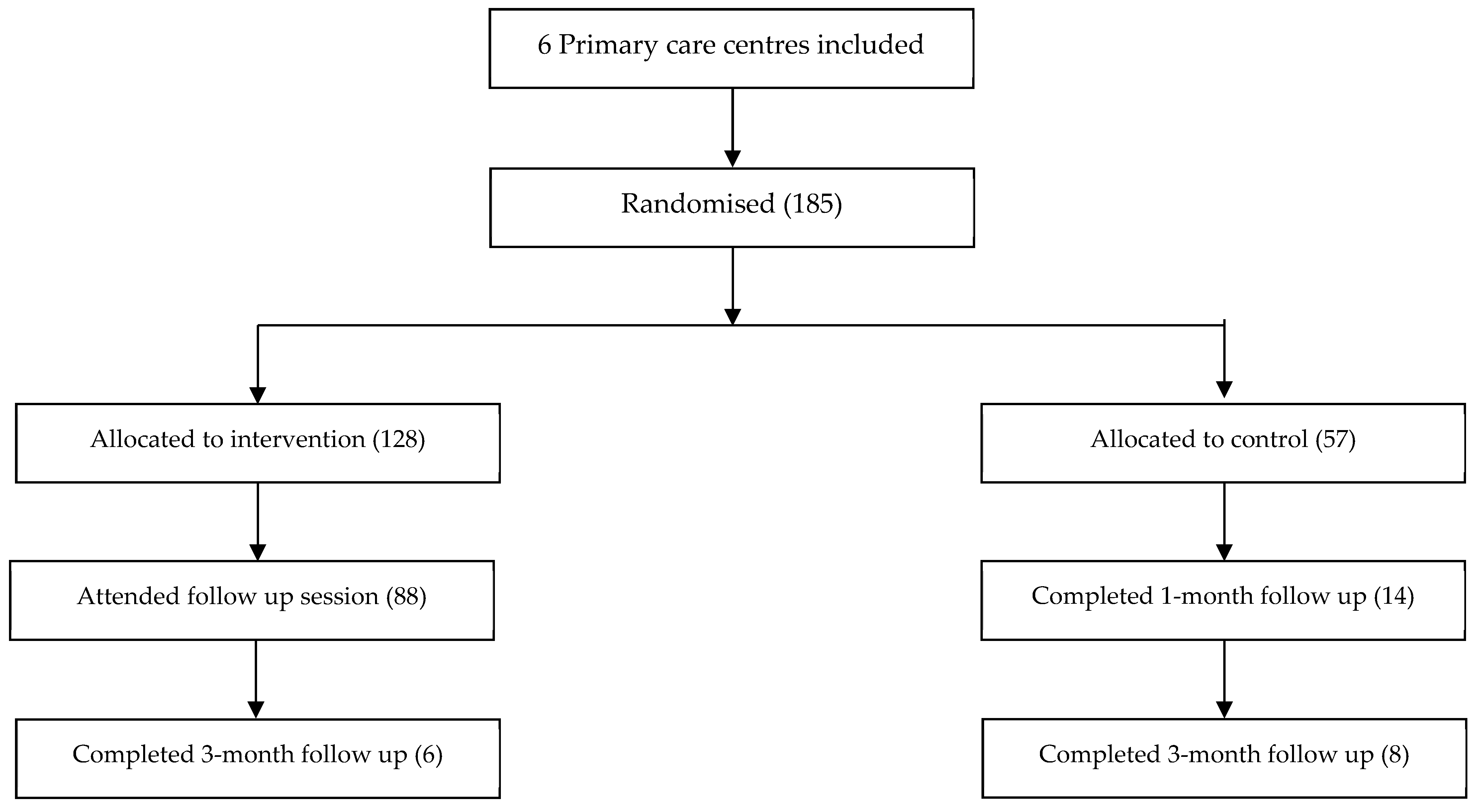
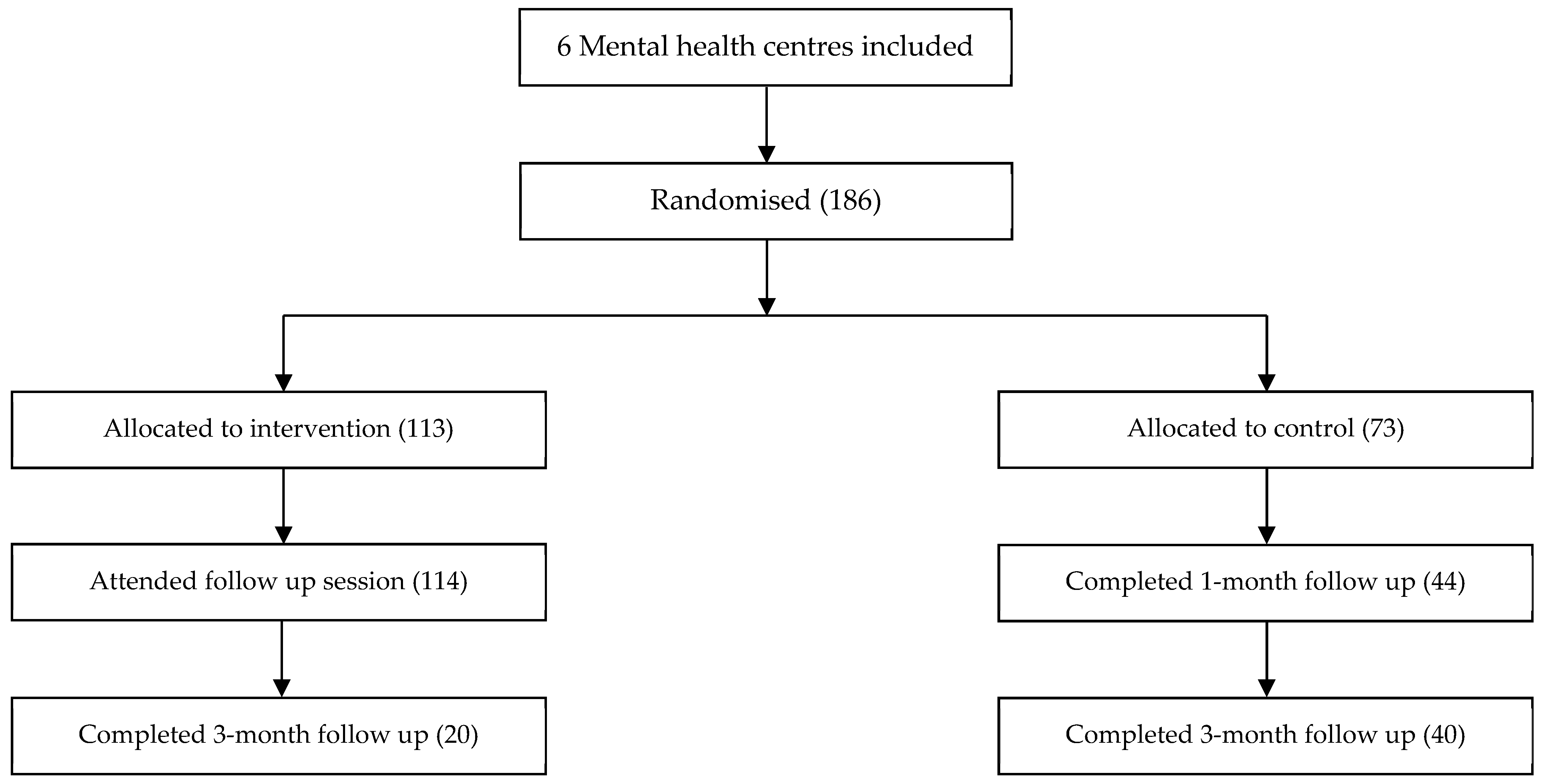
2.4. Participants
2.5. Instruments
2.6. Statistical Analyses
3. Results
3.1. Primary Care
3.2. Mental Health
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Henderson, C.; Noblett, J.; Parke, H.; Clement, S.; Caffrey, A.; Gale-Grant, O.; Schulze, B.; Druss, B.; Thornicroft, G. Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry 2014, 1, 467–482. [Google Scholar] [CrossRef]
- Schulze, B. Stigma and mental health professionals: A review of the evidence on an intricate relationship. Int. Rev. Psychiatry 2007, 19, 137–155. [Google Scholar] [CrossRef] [PubMed]
- Lauber, C.; Nordt, C.; Braunschweig, C.; Rossler, W. Do mental health professionals stigmatize their patients? Acta Psychiatr. Scand. 2006, 113, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Hansson, L.; Jormfeldt, H.; Svedberg, P.; Svensson, B. Mental health professionals’ attitudes towards people with mental illness: Do they differ from attitudes held by people with mental illness? Int. J. Soc. Psychiatry 2013, 59, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Vistorte, A.O.R.; Ribeiro, W.S.; Jaen, D.; Jorge, M.R.; Evans-Lacko, S.; Mari, J.D.J. Stigmatizing attitudes of primary care professionals towards people with mental disorders: A systematic review. Int. J. Psychiatry Med. 2018, 53, 317–338. [Google Scholar] [CrossRef] [PubMed]
- Jorm, A.F.; Korten, A.E.; Jacomb, P.A.; Christensen, H.; Henderson, S. Attitudes Towards People with a Mental Disorder: A Survey of the Australian Public and Health Professionals. Aust. New Zeal. J. Psychiatry 1999, 33, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Ronzani, T.M.; Higgins-Biddle, J.; Furtado, E.F. Stigmatization of alcohol and other drug users by primary care providers in Southeast Brazil. Soc. Sci. Med. 2009, 69, 1080–1084. [Google Scholar] [CrossRef]
- Fernández, E.R.; Martínez, F.E.; Jordana, M.C.; Moraga, A.G. Actitud de los médicos de atención primaria sobre los pacientes con consumo excesivo de alcohol. Aten. Primaria 1999, 24, 447–455. [Google Scholar]
- Lauber, C.; Nordt, C.; Falcato, L.; Rössler, W. Public acceptance of restrictions on mentally ill people. Acta Psychiatr. Scand. Suppl. 2000, 102, 26–32. [Google Scholar] [CrossRef]
- Thornicroft, G.; Rose, D.; Kassam, A. Discrimination in health care against people with mental illness. Int. Rev. Psychiatry 2007, 19, 113–122. [Google Scholar] [CrossRef]
- Sapag, J.C.; Sena, B.F.; Bustamante, I.V.; Bobbili, S.J.; Velasco, P.R.; Mascayano, F.; Alvarado, R.; Khenti, A. Stigma towards mental illness and substance use issues in primary health care: Challenges and opportunities for Latin America. Glob. Public Health 2018, 13, 1468–1480. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Link, B.G.; Corrigan, P.W.; Davidson, L.; Flanagan, E. Perceived provider stigma as a predictor of mental health service users’ internalized stigma and disempowerment. Psychiatry Res. 2018, 259, 526–531. [Google Scholar] [CrossRef] [PubMed]
- Corker, E.; Hamilton, S.; Henderson, C.; Weeks, C.; Pinfold, V.; Rose, D.; Williams, P.; Flach, C.; Gill, V.; Lewis-Holmes, E.; et al. Experiences of discrimination among people using mental health services in England 2008-2011. Br. J. Psychiatry 2013, 202, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Lien, Y.Y.; Lin, H.S.; Tsai, C.H.; Lien, Y.J.; Wu, T.T. Changes in attitudes toward mental illness in healthcare professionals and students. Int. J. Environ. Res. Public Health 2019, 16, 6689. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, P.W.; Druss, B.G.; Perlick, D.A. The Impact of Mental Illness Stigma on Seeking and Participating in Mental Health Care. Psychol. Sci. Public Interest 2014, 15, 37–70. [Google Scholar] [CrossRef]
- Daumerie, N.; Vasseur Bacle, S.; Giordana, J.-Y.; Bourdais Mannone, C.; Caria, A.; Roelandt, J.-L. La discrimination vécue par les personnes ayant reçu un diagnostic de troubles schizophréniques. Premiers résultats français de l’étude INDIGO. Encephale 2012, 38, 224–231. [Google Scholar] [CrossRef]
- Loch, A.A.; Rössler, W. Who Is Contributing? In The Stigma of Mental Illness-End of the Story? Springer International Publishing: Cham, Switzerland, 2017; pp. 111–121. [Google Scholar]
- Vaccari, P.; Ramírez-Vielma, R.; Saldivia, S.; Cova, F.; Vielma-Aguilera, A.; Victoriano, V.; Ulloa-Vidal, N.; Grandón, P. Stigma towards people with a diagnosis of severe mental disorder in primary healthcare centers: Perspectives of service users and health teams in Chile. Int. J. Ment. Health Syst. 2020, 14, 6. [Google Scholar] [CrossRef]
- Livingston, J.D.; Milne, T.; Fang, M.L.; Amari, E. The effectiveness of interventions for reducing stigma related to substance use disorders: A systematic review. Addiction 2012, 107, 39–50. [Google Scholar] [CrossRef]
- Lien, Y.Y.; Lin, H.S.; Lien, Y.J.; Tsai, C.H.; Wu, T.T.; Li, H.; Tu, Y.K. Challenging mental illness stigma in healthcare professionals and students: A systematic review and network meta-analysis. Psychol. Health 2020, 1, 1–16. [Google Scholar] [CrossRef]
- Stubbs, A. Reducing mental illness stigma in health care students and professionals: A review of the literature. Australas. Psychiatry 2014, 22, 579–584. [Google Scholar] [CrossRef]
- Gronholm, P.C.; Henderson, C.; Deb, T.; Thornicroft, G. Interventions to reduce discrimination and stigma: The state of the art. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Heim, E.; Kohrt, B.A.; Koschorke, M.; Milenova, M.; Thornicroft, G. Reducing mental health-related stigma in primary health care settings in low- and middle-income countries: A systematic review. Epidemiol. Psychiatr. Sci. 2020, 29, e3. [Google Scholar] [CrossRef] [PubMed]
- Palou, R.G.; Vigué, G.P.; Tort-Nasarre, G. Attitudes and stigma toward mental health in nursing students: A systematic review. Perspect. Psychiatr. Care 2020, 56, 243–255. [Google Scholar] [CrossRef] [PubMed]
- Al-Ma’ani, M.A.Q.M.; Hamdan-Mansour, A.M. The Effect of Contact-Based Interventions on the Attitudes and Behaviors of Nursing Students towards People with Mental Illness: A Literature Review. Open J. Nurs. 2020, 10, 260–276. [Google Scholar] [CrossRef]
- Knaak, S.; Patten, S. A grounded theory model for reducing stigma in health professionals in Canada. Acta Psychiatr. Scand. 2016, 134, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Kassam, A.; Papish, A.; Modgill, G.; Patten, S. The development and psychometric properties of a new scale to measure mental illness related stigma by health care providers: The opening minds scale for Health Care Providers (OMS-HC). BMC Psychiatry 2012, 12. [Google Scholar] [CrossRef] [PubMed]
- Knaak, S.; Szeto, A.C.H.; Kassam, A.; Hamer, A.; Modgill, G.; Patten, S. Understanding Stigma: A Pooled Analysis of a National Program Aimed at Health Care Providers to Reduce Stigma towards Patients with a Mental Illness. J. Ment. Health Addict. Nurs. 2017, 1, e19–e29. [Google Scholar] [CrossRef]
- Knaak, S.; Modgill, G.; Patten, S.B. Key Ingredients of Anti-Stigma Programs for Health Care Providers: A Data Synthesis of Evaluative Studies. Can. J. Psychiatry 2014, 59, 19–26. [Google Scholar] [CrossRef]
- Friedrich, B.; Evans-Lacko, S.; London, J.; Rhydderch, D.; Henderson, C.; Thornicroft, G. Anti-stigma training for medical students: The Education Not Discrimination project. Br. J. Psychiatry 2013, 202, s89–s94. [Google Scholar] [CrossRef]
- Rowe, B.; Hubbard, T.; Harris, C.; Cryer, J. Time to Change Evaluating the Mental Health Professionals Programme; Revealing Reality: London, UK, 2016. [Google Scholar]
- Grandón, P.; Saldivia, S.; Vaccari, P.; Ramirez-Vielma, R.; Victoriano, V.; Zambrano, C.; Ortiz, C.; Cova, F. An Integrative Program to Reduce Stigma in Primary Healthcare Workers Toward People With Diagnosis of Severe Mental Disorders: A Protocol for a Randomized Controlled Trial. Front. Psychiatry 2019, 10, 1–10. [Google Scholar] [CrossRef]
- Corrigan, P.W. Best Practices: Strategic Stigma Change (SSC): Five Principles for Social Marketing Campaigns to Reduce Stigma. Psychiatr. Serv. 2011, 62, 824–826. [Google Scholar] [CrossRef] [PubMed]
- Rubio-Valera, M.; Aznar-Lou, I.; Vives-Collet, M.; Fernández, A.; Gil-Girbau, M.; Serrano-Blanco, A. Reducing the Mental Health–Related Stigma of Social Work Students. Res. Soc. Work Pract. 2018, 28, 164–172. [Google Scholar] [CrossRef]
- Modgill, G.; Patten, S.B.; Knaak, S.; Kassam, A.; Szeto, A.C. Opening Minds Stigma Scale for Health Care Providers (OMS-HC): Examination of psychometric properties and responsiveness. BMC Psychiatry 2014, 14, 120. [Google Scholar] [CrossRef] [PubMed]
- Eiroa-Orosa, F.J.; Limiñana-Bravo, L. An Instrument to Measure Mental Health Professionals’ Beliefs and Attitudes towards Service Users’ Rights. Int. J. Environ. Res. Public Health 2019, 16, 244. [Google Scholar] [CrossRef] [PubMed]
- United Nations. Convention on the rights of persons with disabilities. Treaty Ser. 2006, 2515, 3. [Google Scholar]
- Szeto, A.; Dobson, K.S.; Luong, D.; Krupa, T.; Kirsh, B. Workplace Antistigma Programs at the Mental Health Commission of Canada: Part 2. Lessons Learned. Can. J. Psychiatry 2019, 64, 13S–17S. [Google Scholar] [CrossRef]
| All (n = 185) | Intervention (n = 128) | Control (n = 57) | Statistical Significance | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | OR, 95% CI | p | ||
| Gender (% females) | 137 | 70.6 | 112 | 81.8 | 38 | 66.7 | 2.24. 1.11–4.52 | 0.022 | |
| Experience with mental health issues (%) | 80 | 41.7 | 52 | 38.5 | 28 | 49.1 | 0.649. 0.35–1.21 | 0.173 | |
| Relative with mental health issues (%) | 135 | 69.2 | 96 | 69.6 | 39 | 68.4 | 1.055. 0.54–2.05 | 0.875 | |
| M | SD | M | SD | M | SD | t | p | d | |
| Age (M ± SD) | 44.34 | 10.82 | 44.02 | 11.41 | 45.05 | 9.41 | 0.630. | 0.530 | 0.095 |
| Attitudes S | 2.20 | 0.57 | 2.25 | 0.58 | 2.11 | 0.52 | 1.570 | 0.118 | 0.0897 |
| Disclosure | 2.50 | 0.68 | 2.55 | 0.67 | 2.39 | 0.69 | 1.504 | 0.134 | 0.1073 |
| Social distance | 2.12 | 0.59 | 2.16 | 0.62 | 2.05 | 0.51 | 1.171 | 0.243 | 0.0938 |
| OMS-HC total | 2.36 | 0.40 | 2.40 | 0.41 | 2.26 | 0.37 | 2.138 | 0.034 | 0.0626 |
| First Follow-Up | Second Follow-Up | Statistical Significance | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | First Follow-Up | Second Follow-Up | RM-ANOVA ** | |||||||||||
| M | SD | M | SD | M | SD | M | SD | z | p | d | z | p | d | F | p | ηp2 | |
| Attitudes S | 2.15 | 0.60 | 2.21 | 0.50 | 2.22 | 0.61 | 2.25 | 0.53 | −0.566 | 0.571 | −0.115 | −0.521 | 0.602 | −0.057 | 1.708 | 0.259 | 0.363 |
| Disclosure | 2.43 | 0.74 | 2.43 | 0.40 | 2.17 | 0.38 | 2.66 | 0.60 | −0.015 | 0.988 | −0.003 | −1.511 | 0.131 | −0.948 | 11.878 | 0.008 | 0.798 |
| Social distance | 2.04 | 0.63 | 2.24 | 0.45 | 1.93 | 0.37 | 2.13 | 0.56 | −1.197 | 0.231 | −0.332 | −0.393 | 0.694 | −0.393 | 0.631 | 0.564 | 0.174 |
| OMS-HC total | 2.26 | 0.48 | 2.38 | 0.30 | 2.18 | 0.31 | 2.41 | 0.43 | −0.725 | 0.468 | −0.249 | −1.035 | 0.301 | −0.587 | 1.911 | 0.228 | 0.389 |
| All (n = 186) | Intervention (n = 113) | Control (n = 73) | Statistical Significance | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | OR, 95% CI | p | ||
| Gender (% females) | 177 | 78.3 | 105 | 76.6 | 72 | 80.9 | 1.291. 0.667–4.498 | 0.448 | |
| Experience with mental health issues (%) | 87 | 38.5 | 49 | 35.5 | 38 | 43.2 | 1.380. 0.799–2.386 | 0.248 | |
| Relative with mental health issues (%) | 174 | 78.7 | 106 | 78.5 | 68 | 79.1 | 1.034. 0.533–2.004 | 0.922 | |
| M | SD | M | SD | M | SD | t | p | d | |
| Age (M ± SD) | 41.56 | 12.35 | 41.72 | 12.70 | 41.30 | 11.81 | −0.237 | 0.813 | 0.033 |
| Beliefs | 2.46 | 0.39 | 2.44 | 0.39 | 2.49 | 0.39 | 0.884 | 0.378 | −0.133 |
| Coercion | 2.48 | 0.46 | 2.49 | 0.44 | 2.46 | 0.49 | 0.881 | 0.38 | 0.070 |
| Paternalism | 2.30 | 0.40 | 2.27 | 0.39 | 2.34 | 0.43 | −0.467 | 0.641 | −0.179 |
| Discrimination | 1.91 | 0.42 | 1.93 | 0.45 | 1.88 | 0.38 | −0.456 | 0.649 | 0.120 |
| BAMHS total | 2.36 | 0.27 | 2.35 | 0.27 | 2.39 | 0.28 | 0.910 | 0.364 | −0.137 |
| First Follow-Up | Second Follow-Up | Statistical Significance | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | First Follow-Up | Second Follow-Up | RM-ANOVA ** | |||||||||||
| M | SD | M | SD | M | SD | M | SD | z | p | d | z | p | d | F | p | ηp2 | |
| Beliefs | 2.41 | 0.40 | 2.55 | 0.37 | 2.52 | 0.35 | 2.56 | 0.37 | −2.419 | 0.016 | −0.349 | −0.166 | 0.868 | −0.349 | 0.388 | 0.681 | 0.019 |
| Coercion | 2.38 | 0.42 | 2.47 | 0.49 | 2.42 | 0.39 | 2.43 | 0.48 | −1.449 | 0.147 | −0.195 | −0.360 | 0.719 | −0.195 | 0.478 | 0.624 | 0.023 |
| Paternalism | 2.28 | 0.43 | 2.32 | 0.40 | 2.23 | 0.39 | 2.32 | 0.40 | −1.006 | 0.314 | −0.093 | −0.695 | 0.487 | −0.093 | 0.065 | 0.937 | 0.003 |
| Discrimination | 1.94 | 0.45 | 1.88 | 0.46 | 1.88 | 0.38 | 2.06 | 0.39 | −0.594 | 0.552 | 0.130 | −1.549 | 0.121 | 0.130 | 5.450 | 0.008 | 0.214 |
| BAMHS total | 2.33 | 0.29 | 2.39 | 0.29 | 2.33 | 0.28 | 2.41 | 0.27 | −2.392 | 0.017 | −0.235 | −0.700 | 0.484 | −0.235 | 0.781 | 0.465 | 0.038 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eiroa-Orosa, F.J.; Lomascolo, M.; Tosas-Fernández, A. Efficacy of an Intervention to Reduce Stigma Beliefs and Attitudes among Primary Care and Mental Health Professionals: Two Cluster Randomised-Controlled Trials. Int. J. Environ. Res. Public Health 2021, 18, 1214. https://doi.org/10.3390/ijerph18031214
Eiroa-Orosa FJ, Lomascolo M, Tosas-Fernández A. Efficacy of an Intervention to Reduce Stigma Beliefs and Attitudes among Primary Care and Mental Health Professionals: Two Cluster Randomised-Controlled Trials. International Journal of Environmental Research and Public Health. 2021; 18(3):1214. https://doi.org/10.3390/ijerph18031214
Chicago/Turabian StyleEiroa-Orosa, Francisco José, María Lomascolo, and Anaïs Tosas-Fernández. 2021. "Efficacy of an Intervention to Reduce Stigma Beliefs and Attitudes among Primary Care and Mental Health Professionals: Two Cluster Randomised-Controlled Trials" International Journal of Environmental Research and Public Health 18, no. 3: 1214. https://doi.org/10.3390/ijerph18031214
APA StyleEiroa-Orosa, F. J., Lomascolo, M., & Tosas-Fernández, A. (2021). Efficacy of an Intervention to Reduce Stigma Beliefs and Attitudes among Primary Care and Mental Health Professionals: Two Cluster Randomised-Controlled Trials. International Journal of Environmental Research and Public Health, 18(3), 1214. https://doi.org/10.3390/ijerph18031214







