Virtual Home Assistant Use and Perceptions of Usefulness by Older Adults and Support Person Dyads
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Recruitment
2.3. Ethical Considerations
2.4. Measures
2.5. Study Procedures
Protocol
2.6. Analyses
3. Results
3.1. Sample Characteristics
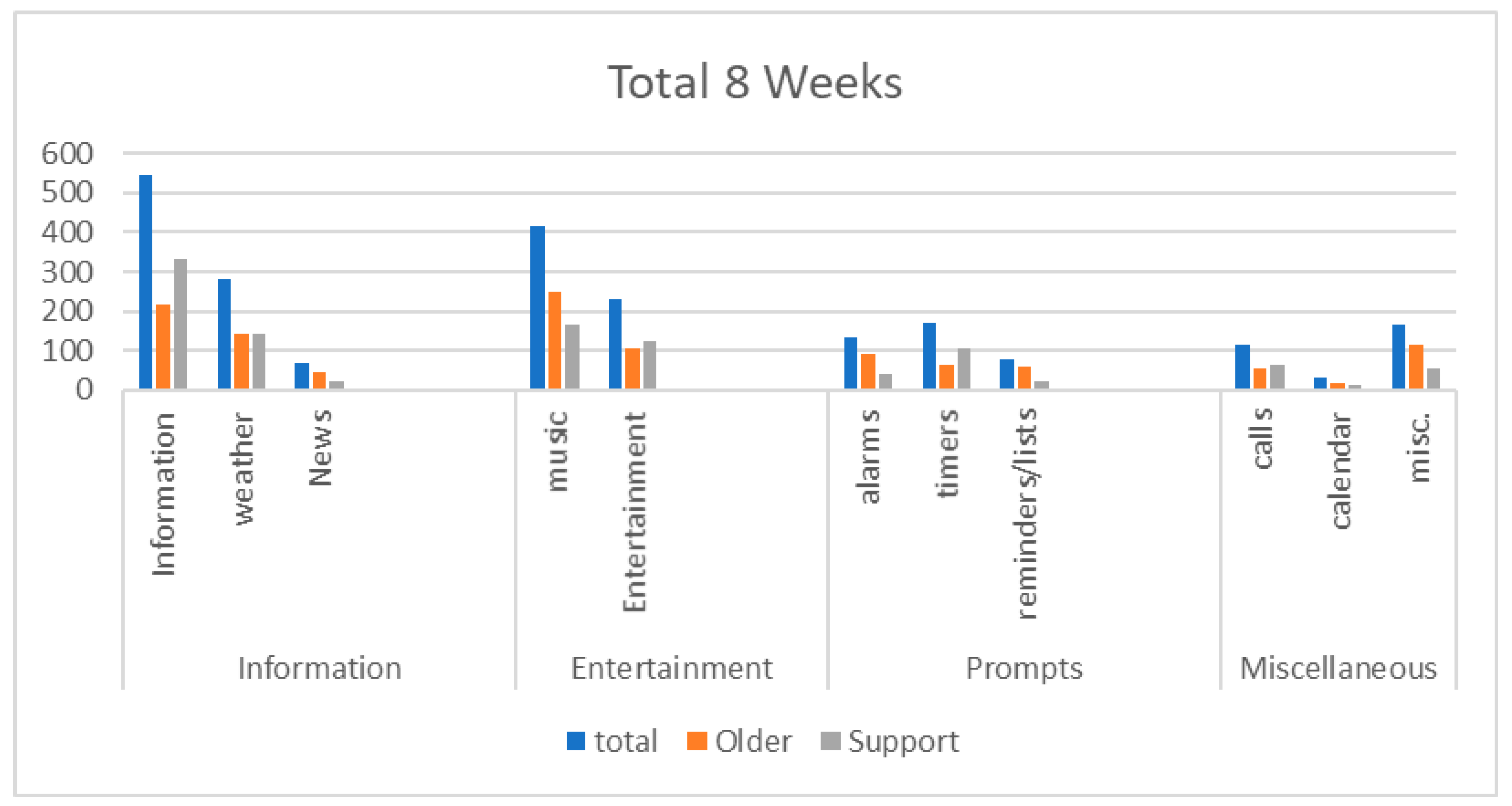
3.2. Quantitative VHA Use Findings
3.3. Qualitative VHA Use Findings
3.3.1. Information: “She’s Good for Information”
3.3.2. Entertainment: “…Just the Music, It Is Just a Gift”
3.3.3. Prompts: “Reminders for What You Are Supposed to be Doing”
3.4. Additional Qualitative Findings
3.4.1. Companionship and Security: “Somebody Is Here with Me…”
3.4.2. Understanding Its Capabilities and Changing Habits: “Getting Used to Another Device”
3.4.3. Suggested Future Applications
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Afshar, S.; Roderick, P.J.; Kowal, P.; Dimitrov, B.D.; Hill, A.G. Multimorbidity and the inequalities of global ageing: A cross-sectional study of 28 countries using the World Health Surveys. BMC Public Health 2015, 115, 776. [Google Scholar] [CrossRef] [PubMed]
- Living Longer: Historical and Projected Life Expectancy in the United States, 1960 to 2060. US Department of Commerce, US Census Bureau. Available online: https://www.census.gov/library/publications/2020/demo/p25-1145.html (accessed on 21 December 2020).
- Boersma, P.; Black, L.I.; Ward, B.W. Prevalence of multiple chronic conditions among US adults, 2018. Prev. Chronic Dis. 2020, 17, 200130. [Google Scholar] [CrossRef] [PubMed]
- Home and Community Preferences Survey: A National Survey of Adults 18-Plus. Available online: https://www.aarp.org/livable-communities/about/info-2018/2018-aarp-home-and-community-preferences-survey.html (accessed on 21 December 2020).
- Kim, K.; Gollamudi, S.S.; Steinhubl, S. Digital technology to enable aging in place. Exp. Gerontol. 2017, 88, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Peek, S.T.M.; Luijkx, K.G.; Rijnaard, M.D.; Nieboer, M.E.; van der Voort, C.S.; Aarts, S.; van Hoof, J.; Vrijhoef, H.J.M.; Wouters, E.J.M. Older adults’ reasons for using technology while aging in place. Gerontology 2016, 62, 226–237. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Damnee, S.; Ware, C.; Rigaud, A. Bridging the digital divide in older adults a study from an initiative to inform older adults about new technologies. Clin. Interv. Aging 2015, 10, 193–201. [Google Scholar] [CrossRef]
- Gustafson, D.H., Sr.; McTavish, F.; Gustafson, D.H., Jr.; Mahoney, J.E.; Johnson, R.A.; Lee, J.D.; Quanbeck, A.; Atwood, A.K.; Isham, A.; Veeramani, R.; et al. The effect of an information and communication technology (ICT) on older adults’ quality of life: Study protocol for a randomized clinical trial. Trials 2015. [Google Scholar] [CrossRef]
- LeRouge, C.; Van Slyke, C.; Seale, D.; Wright, K. Baby boomers’ adoption of consumer health technologies: Survey on readiness and barriers. J. Med. Internet Res. 2014, 16, e200. [Google Scholar] [CrossRef]
- Betts, L.R.; Hill, R.; Gardner, S.E. “There’s not enough knowledge out there”: Examining older adults’ perceptions of digital technology use and digital inclusion classes. J. Appl. Gerontol. 2019, 38, 1147–1166. [Google Scholar] [CrossRef]
- Older Adults Keep Pace on Tech Usage: 2020 Tech Trends of the 50+. Available online: https://www.aarp.org/research/topics/technology/info-2019/2020-technology-trends-older-americans/ (accessed on 7 January 2021).
- Chambers, R.; Beaney, P. The potential of placing a digital assistant in patients’ homes. Br. J. Gen. Pract. 2020. [Google Scholar] [CrossRef]
- Beaney, P.; Kalirai, H.S.; Chambers, R. Alexa what pills do I need to take today? Prescriber 2020, 31, 20–23. [Google Scholar] [CrossRef]
- Wulf, L.; Garschall, M.; Himmelsbach, J.; Tscheligi, M. Hands free—Care free: Elderly people taking advantage of speech-only interaction. In Proceedings of the NordiCHI, Helsinki, Finland, 26–30 October 2014. [Google Scholar]
- Pradhan, A.; Mehta, K.; Findlater, L. “Accessibility came by accident”: Use of voice-controlled intelligent personal assistants by people with disabilities. In Proceedings of the CHI, Montreal, QC, Canada, 21–26 April 2018. [Google Scholar]
- O’Brien, K.; Liggett, A.; Ramirez-Zohfeld, V.; Sunkara, P.; Lindquist, L.A. Voice-controlled intelligent personal assistants to support aging in place. J. Am. Geriartr. Soc. 2020, 68, 176–179. [Google Scholar] [CrossRef]
- Koon, L.M.; McGlynn, S.A.; Blocker, K.A.; Rodgers, W.A. Perceptions of digital assistants from early adopters aged 55+. Ergon. Des. 2020. [Google Scholar] [CrossRef]
- Tiwari, V.; Hasmi, M.F.; Keskar, A.; Shivaprakash, N.C. Virtual home assistant for voice based controlling and scheduling with short speech speaker identification. Multimed. Tools Appl. 2018, 79, 5243–5268. [Google Scholar] [CrossRef]
- Owens, O.L.; Beer, J.M.; Revels, A.A.; White, K. The lived experiences of older low-income African Americans living alone: Implications for aging in place in the United States. J. Aging Environ. 2020. [Google Scholar] [CrossRef]
- Lee, A.; Piette, J.D.; Heisler, M.; Janevic, M.; Langa, K.M.; Rosland, A.M. Family members’ experiences supporting adults with chronic illness: A national survey. Fam. Syst. Health 2017, 25, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Yap, A.F.; Thirumoorthy, T.; Kwan, Y.H. Medication adherence in the elderly. J. Clin. Gerontol. Geriatr. 2016, 7, 64–67. [Google Scholar] [CrossRef]
- Beach, S.R.; Schulz, R. Family caregiver factors associated with unmet needs for care of older adults. J. Am. Geriatr. Soc. 2017, 65, 560–566. [Google Scholar] [CrossRef]
- Lin, S.-F.; Beck, A.N.; Finch, B.K.; Hummer, R.A.; Master, R.K. Trends in US older adult disability: Exploring age, period, and cohort effects. AJPH 2021, 102, 2157–2163. [Google Scholar] [CrossRef]
- Scheel-Hincke, L.L.; Moller, S.; LIndahl-Jacobsen, R.; Jeune, B.; Ahrenfeldt, L.J. Cross-national comparison of sex differences in ADL and IADL in Europe: Findings from SHARE. EJA 2020, 17, 69–79. [Google Scholar] [CrossRef]
- Schoonenboom, J.; Johnson, R.B. How to construct a mixed methods research design. Köln. Z. Soziol. Sozialpsychol. 2017, 69, 107–131. [Google Scholar] [CrossRef]
- Millán-Calenti, J.C.; Tubío, J.; Pita-Fernández, S.; González-Abraldes, I.; Lorenzo, T.; Fernández-Arruty, T.; Maseda, A. Prevalence of functional disability in activities of daily living (ADL), instrumental activities of daily living (IADL) and associated factors, as predictors of morbidity and mortality. Arch. Gerontol. Geriatr. 2010, 50, 306–310. [Google Scholar] [CrossRef] [PubMed]
- Cella, D.; Riley, W.; Stone, A.; Rothrock, N.; Reeve, B.; Yount, S.; Amtmann, D.; Bode, R.; Buysse, D.; Choi, S.; et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J. Clin. Epidemiol. 2010, 63, 1179–1194. [Google Scholar] [CrossRef] [PubMed]
- International Well-Being Group. Personal Well-Being Index (PWI, Adult): English, 5th ed.; Deaken University: Melbourne, Australia, 2013. [Google Scholar]
- Omani, S.R.; Maroufizadeh, S.; Almas-Hashiani, A.; Sepidarkish, M.; Amini, P. The WHO-5 well-being index: A validation study in people with infertility. Iran. J. Public Health 2019, 48, 2058–2064. [Google Scholar]
- Measurement Instrument Database for the Social Sciences. Caregiver Burden Scale. Available online: https://www.midss.org/content/caregiver-burden-scale (accessed on 21 December 2020).
- Nearly 70% for US Smart Speaker Owners Uses Amazon Echo Devices. Available online: https://techcrunch.com/2020/02/10/nearly-70-of-u-s-smart-speaker-owners-use-amazon-echo-devices/#:~:text=Specifically%2C%2069.7%25%20of%20U.S.%20smart,owners%20using%20an%20Echo%20device. (accessed on 21 December 2020).
- Seale, C. Quality in qualitative research. Qual. Inq. 1999, 5, 465–478. [Google Scholar] [CrossRef]
- Tankovska, H. Number of Amazon Alexa Compatible Smart Home Devices 2017–2020. Available online: https://www.statista.com/statistics/912893/amazon-alexa-smart-home-compatible/#:~:text=Number%20of%20Amazon%20Alexa%20compatible%20smart%20home%20devices%202017%2D2020&text=As%20of%20July%202020%2C%20the,it%20was%20at%20four%20thousand. (accessed on 21 December 2020).
- Sciuto, A.; Saini, A.; Forlizzi, J.; Hong, J.I. “Hey Alexa, what’s up?”: Studies of in-home conversational agent usage. In Proceedings of the DIS, Hong Kong, China, 9–13 June 2018. [Google Scholar]
- Scherr, S.A.; Meier, A.; Cihan, S. Alexa, tell me more—About new best friends, the advantage of hands-free operation and life-long learning. In Proceedings of the Mensch und Computer, Berlin, Germany, 6–9 September 2020. [Google Scholar] [CrossRef]
- Trajkova, M.; Martin-Hammond, A. “Alexa is a toy”: Exploring older adults’ reasons for using, limiting, and abandoning Echo. In Proceedings of the Conference of Human-Computer Interaction, Honolulu, HI, USA, 25–30 April 2020. [Google Scholar] [CrossRef]
- Cowan, B.R.; Pantidi, N.; Coyle, D.; Morrissey, K.; Clarke, P.; Al-Shehri, S.; Earley, D.; Bandeira, N. “What can I help you with?”: Infrequent users’ experiences of intelligent personal assistants. In Proceedings of the International Conference on Human-Computer Interaction with Mobile Devices and Services, Vienna, Austria, 4–7 September 2017. [Google Scholar] [CrossRef]
- Johnson, S.A.; Romanello, M.L. Generational diversity: Teaching and learning approaches. Nurse Edu. 2005, 30, 212–216. [Google Scholar] [CrossRef]
- Urick, M. Adapting training to meet the preferred learning styles of different generations. Int. J. Train Dev. 2016, 21, 53–59. [Google Scholar] [CrossRef]
- Li, J.; Maharjan, B.; Xie, B.; Tao, C. A personalized voice-based diet assistant for caregivers of Alzheimer Disease and related dementias: System development and validation. J. Med. Internet Res. 2020, 22, e19897. [Google Scholar] [CrossRef]
- Maharjan, B.; Li, J.; Kong, J.; Tao, C. Alexa, what should I eat? A personalized virtual nutrition coach for native American diabetes patients using Amazon’s smart speaker technology. In Proceedings of the IEEE International Conference on E-Health Networking, Application & Services (HealthCom), Bogotá, Colombia, 14–16 October 2019. [Google Scholar]
- AmazonDeveloper. Alexa Skills Business Associate Agreement. Available online: https://developer.amazon.com/support/legal/alexa-hipaa-baa. (accessed on 21 December 2020).
- Krasniansky, A. Diving deeper into Amazon Alexa’s HIPPA Compliance. The Hastings Center. Available online: https://www.thehastingscenter.org/diving-deeper-into-amazon-alexas-hipaa-compliance/ (accessed on 21 December 2020).
- Wang, S.; Bolling, K.; Mao, W.; Reichstadt, J.; Jeste, D.; Kim, H.C.; Nebeker, C. Technology to support aging in place: Older adults’ perspectives. Healthcare 2019, 7, 60. [Google Scholar] [CrossRef]
- Purington, A.; Taft, J.G.; Sannon, S.; Bazarova, N.N.; Taylor, S.H. “Alexa is my new BFF”: Social roles, user satisfaction, and personification of the Amazon Echo. In Proceedings of the Conference on Human Factors in Computing Systems, Denver, CO, USA, 11 May 2017. [Google Scholar]
| Demographics 1 | Older Adults | Support Persons | ||
|---|---|---|---|---|
| n | % | n | % | |
| Sex | ||||
| Female | 9 | 90 | 4 | 44.4 |
| Male | 1 | 10 | 5 | 55.5 |
| Race/Ethnicity | ||||
| White | 8 | 80 | 7 | 77.7 |
| Black | 2 | 20 | 1 | 11.1 |
| Asian | 0 | 0 | 1 | 11.1 |
| Highest educational level | ||||
| Less than High School Diploma | 0 | 0 | 0 | 0 |
| High School Diploma/GED | 2 | 20 | 2 | 22.2 |
| Associates Degree/Certification | 2 | 20 | 3 | 33.3 |
| Bachelor’s Degree | 3 | 30 | 1 | 11.1 |
| Master’s and above | 3 | 16 | 3 | 33.3 |
| Living Alone | ||||
| Yes | 8 | 80 | 2 | 22.2 |
| No | 2 | 20 | 7 | 77.7 |
| Subscale 1 | n | Mean (SD) | Range |
|---|---|---|---|
| 1. Global Physical Health | 9 | 42.00 (6.14) | 37.4–54.1 |
| 2. Global Mental Health | 9 | 47.01 (9.74) | 41.1–59 |
| 3. Personal Well-Being Index | 9 | 76.94 (21.55) | 34–97 |
| 4. WHO-5 3 Well Being Index | 9 | 59.60 (20.45) | 36–80 |
| 5. Short Flourishing Scale | 9 | 42.88 (10.47) | 23–55 |
| Subscale | n | Mean (SD) | Range |
|---|---|---|---|
| 1. Patient Needs Domain | 9 | 3.88 (2.30) | 0–6 |
| 2. Caregiver Tasks Domain | 9 | 2.88 (2.23) | 0–5 |
| 3. Caregiver Burden Domain | 9 | 7.63 (4.93) | 0–13 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
F. Corbett, C.; M. Combs, E.; J. Wright, P.; L. Owens, O.; Stringfellow, I.; Nguyen, T.; Van Son, C.R. Virtual Home Assistant Use and Perceptions of Usefulness by Older Adults and Support Person Dyads. Int. J. Environ. Res. Public Health 2021, 18, 1113. https://doi.org/10.3390/ijerph18031113
F. Corbett C, M. Combs E, J. Wright P, L. Owens O, Stringfellow I, Nguyen T, Van Son CR. Virtual Home Assistant Use and Perceptions of Usefulness by Older Adults and Support Person Dyads. International Journal of Environmental Research and Public Health. 2021; 18(3):1113. https://doi.org/10.3390/ijerph18031113
Chicago/Turabian StyleF. Corbett, Cynthia, Elizabeth M. Combs, Pamela J. Wright, Otis L. Owens, Isabel Stringfellow, Thien Nguyen, and Catherine R. Van Son. 2021. "Virtual Home Assistant Use and Perceptions of Usefulness by Older Adults and Support Person Dyads" International Journal of Environmental Research and Public Health 18, no. 3: 1113. https://doi.org/10.3390/ijerph18031113
APA StyleF. Corbett, C., M. Combs, E., J. Wright, P., L. Owens, O., Stringfellow, I., Nguyen, T., & Van Son, C. R. (2021). Virtual Home Assistant Use and Perceptions of Usefulness by Older Adults and Support Person Dyads. International Journal of Environmental Research and Public Health, 18(3), 1113. https://doi.org/10.3390/ijerph18031113






