The Chinese Mandarin Version of the Crisis Triage Rating Scale for Taiwanese with Mental Illness to Compulsory Hospitalization
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Study Patients
2.2. Instruments
2.2.1. Demographic Data Sheet
2.2.2. Chinese Mandarin Version of the Crisis Triage Rating Scale (CMCTRS)
2.2.3. Taiwan Urgency of Response Scale (TURS)
2.3. Study Procedure and Ethical Considerations
2.4. Study Analysis
3. Results
3.1. Demographic Data
3.2. The CMCTRS
3.3. The TURS
3.4. The Cut-Off Point Analysis of CMCTRS
4. Discussion
4.1. Main Findings
4.2. Limitations and Recommendations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The Department of Mental and Oral Health, the Ministry of Health and Welfare. National Mental Hospital Statistics. Available online: https://dep.mohw.gov.tw/domhaoh/cp-401-51545-107.html (accessed on 10 November 2021).
- Griffith, K.N.; Li, D.; Davies, M.; Pizer, S.; Prentice, J. Call center performance affects patient perceptions of access and satisfaction. Am. J. Manag. Care 2021, 25, e282–e287. [Google Scholar]
- Silva, B.; Golay, P.; Morandi, S. Factors associated with involuntary hospitalisation for psychiatric patients in Switzerland: A retrospective study. BMC Psychiatry 2018, 18, 401. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Law & Regulations Database, The Republic of China. Mental Health Act. Available online: https://law.moj.gov.tw/LawClass/LawAll.aspx?pcode=L0020030 (accessed on 10 December 2020).
- The Department of Mental and Oral Health, the Ministry of Health and Welfare. Mental Illness Mandatory Assessment and Community Treatment Review Committee Report. Available online: https://dep.mohw.gov.tw/DOMHAOH/lp-406-107.html (accessed on 17 December 2021).
- Weich, S.; McBride, O.; Twigg, L.; Duncan, C.; Keown, P.; Crepaz-Keay, D.; Cyhlarova, E.; Parsons, H.; Scott, J.; Bhui, K. Variation in compulsory psychiatric inpatient admission in England: A cross-classified, multilevel analysis. Lancet Psychiatry 2017, 4, 619–626. [Google Scholar] [CrossRef] [Green Version]
- Raboch, J.; Kališová, L.; Nawka, A.; Kitzlerová, E.; Onchev, G.; Karastergiou, A.; Magliano, L.; Dembinskas, A.; Kiejna, A.; Torres-Gonzales, F. Use of coercive measures during involuntary hospitalization: Findings from ten European countries. Psychiatr. Serv. 2010, 61, 1012–1017. [Google Scholar] [CrossRef]
- Lepping, P.; Steinert, T.; Gebhardt, R.P.; Röttgers, H.R. Attitudes of mental health professionals and lay-people towards involuntary admission and treatment in England and Germany—A questionnaire analysis. Eur. Psychiatry 2004, 19, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Lay, B.; Kawohl, W.; Rossler, W. Outcomes of a psycho-education and monitoring programme to prevent compulsory admission to psychiatric inpatient care: A randomised controlled trial. Psychol. Med. 2018, 48, 849–860. [Google Scholar] [CrossRef]
- Bengelsdorf, H.; Levy, L.E.; Emerson, R.L.; Barile, F.A. A crisis triage rating scale. Brief dispositional assessment of patients at risk for hospitalization. J. Nerv. Ment. Dis. 1984, 172, 424–430. [Google Scholar] [CrossRef]
- Adeosun, I.I.; Adegbohun, A.A.; Akinjola, O.; Jejeloye, A.; Ajayi, B.; Adenusi, T. Validity of the Crisis Triage Rating Scale among Attendees of a Psychiatric Emergency Department in Nigeria. Int. J. Ment. Health Psychiatry 2017, 3, 4. [Google Scholar] [CrossRef]
- Department of Health Victoria. Statewide Mental Health Triage Scale Guidelines. State of Victoria, Department of Health. Australia. Available online: https://www2.health.vic.gov.au/mental-health/practice-andservice-quality/service-quality/mental-health-triage-service (accessed on 30 October 2018).
- Natisha, S.; Stephen, E.; Robert, C.; Helen, H.; Roshani, P. Development and interrater reliability of the UK mental health triage scale. J Psychiatr. Ment. Health Nurs. 2016, 25, 330–336. [Google Scholar]
- Hoffman, R.; Hirdes, J.; Brown, P.G.; Dubin, A.J.; Barbaree, H. The use of a brief mental health screener to enhance the ability of police officers to identify persons with serious mental disorders. Int. J. Law Psychiatry 2016, 47, 28–35. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health, NSW. Mental Health Triage Policy. Ministry of Health, NSW, Australia. Available online: https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/PD2012_053.pdf (accessed on 30 October 2018).
- Turner, P.M.; Turner, T.J. Validation of the Crisis Triage Rating Scale for psychiatric emergencies. Can. J. Psychiatry 1991, 36, 651–654. [Google Scholar] [CrossRef]
- Adeosun, I.I.; Adegbohun, A.; Jeje, O.O.; Oyekunle, O.O.; Omoniyi, M.O. Urgent and Nonurgent Presentations to a Psychiatric Emergency Service in Nigeria: Pattern and Correlates. Emerg. Med. Int. 2014, 6, 479081. [Google Scholar] [CrossRef] [Green Version]
- Schisterman, E.F.; Perkins, N.J.; Liu, A.; Bondell, H. Optimal cut-point and its corresponding Youden Index to discriminate individuals using pooled blood samples. Epidemiology 2005, 16, 73–81. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Mental Health Services in Australia. Available online: https://www.aihw.gov.au/reports/mental-health-services/mental-health-services-in-australia/report-contents/specialised-mental-health-care-facilities/specialised-mental-health-beds-and-patient-days. (accessed on 18 June 2021).
- Pinals, D.A.; Fuller, D.A. The Vital Role of a Full Continuum of Psychiatric Care Beyond Beds. Psychiatr. Serv. 2020, 71, 713–721. [Google Scholar] [CrossRef]
- United Nations. Convention on the Rights of Persons with Disabilities (CRPD). Available online: https://www.un.org/development/desa/disabilities/convention-on-the-rights-of-persons-with-disabilities.html (accessed on 10 December 2021).
- Hsiao, H.J. The Study on Police Officers’ Involuntary Escort Services for Medical Treatments—Focusing on Article 32 of Mental Health Law. Master Thesis, College of Law, National Taiwan University, Taipei, Taiwan. Available online: https://ndltd.ncl.edu.tw/cgi-bin/gs32/gsweb.cgi/login?o=dnclcdr&s=id=%22105NTU05194070%22.&searchmode=basic (accessed on 20 November 2017).
- Balfour, M.E.; Hahn Stephenson, A.; Delany-Brumsey, A.; Winsky, J.; Goldman, M.L. Cops, Clinicians, or Both? Collaborative Approaches to Responding to Behavioral Health Emergencies. Psychiatr. Serv. 2021. [Google Scholar] [CrossRef]
- Australian Government, Department of Health. Emergency Triage Education Kit. Available online: https://www1.health.gov.au/internet/main/publishing.nsf/Content/casemix-ED-Triage%20Review%20Fact%20Sheet%20Documents (accessed on 10 September 2009).
- Sæbye, D.; Høegh, E.B.; Knop, J. Triage in psychiatric emergency services in Copenhagen: Results from a descriptive 1-year evaluation study. Nord. J. Psychiatry 2017, 71, 536–542. [Google Scholar] [CrossRef] [PubMed]
- Brooker, C.; Ricketts, T.; Bennett, S.; Lemme, F. Admission decisions following contact with an emergency mental health assessment and intervention service. J. Clin. Nurs. 2007, 16, 1313–1322. [Google Scholar] [CrossRef]
- Molina, L.A.; Cruz Islas, J.B.; Palma, C.M.; Guizar-Sánchez, D.P.; Garfias-Rau, C.Y.; Ontiveros-Uribe, M.P.; Fresán, O.A. Validity and reliability of a novel Color-Risk Psychiatric Triage in a psychiatric emergency department. BMC Psychiatry 2016, 16, 30. [Google Scholar] [CrossRef] [Green Version]
- Nyttingnes, O.; Ruud, T.; Rugkåsa, J. It’s unbelievably humiliating’—Patients’ expressions of negative effects of coercion in mental health care. Int. J. Law Psychiatry 2016, 49, 147–153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomsen, C.; Starkopf, L.; Hastrup, L.H.; Andersen, P.K.; Nordentoft, M.; Benros, M. Risk factors of coercion among psychiatric inpatients: A nationwide registerbased cohort study. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 979–987. [Google Scholar] [CrossRef]
- Wang, J.P.; Wu, C.Y.; Chiu, C.C.; Yang, T.H.; Liu, T.H.; Chou, P. Police referrals at the psychiatric emergency service in Taiwan. Asia-Pac. Psychiatry 2015, 7, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Curto, M.; Pompili, E.; Silvestrini, C.; Bellizzi, P.; Navari, S.; Pompili, P.; Manzi, A.; Bianchini, V.; Carlone, C.; Ferracuti, S.; et al. A novel SCL-90-R six-item factor identifies subjects at risk of early adverse outcomes in public mental health settings. Psychiatry Res. 2018, 267, 376–381. [Google Scholar] [CrossRef] [PubMed]
| Score | Rating A: Dangerousness | Rating C: Support System | Rating B: Ability to Cooperate |
|---|---|---|---|
| 1 | 53 (17.6%) | 39 (12.9%) | 95 (31.5%) |
| 2 | 74 (24.5%) | 43 (14.2%) | 93 (30.8%) |
| 3 | 53 (17.6%) | 134 (44.4%) | 27 (8.9%) |
| 4 | 63 (20.9%) | 45 (14.9%) | 76 (25.2%) |
| 5 | 59 (19.5%) | 41 (13.6%) | 11 (3.6%) |
| Variable | Other-Option | Hospitalization | p-Value |
|---|---|---|---|
| All | 44.9 (17.1) | 46.3 (15.1) | 0.4592 |
| Age Range | |||
| 12–24.9 | 10 (31.3%) | 22 (68.8%) | 0.0824 |
| 25–34.9 | 19 (46.3%) | 22 (53.7%) | |
| 35–44.9 | 19 (27.5%) | 50 (72.5%) | |
| 45–54.9 | 17 (20.7%) | 65 (79.3%) | |
| 55–64.9 | 17 (37.0%) | 29 (63.0%) | |
| Over 65 | 10 (31.3%) | 22 (68.8%) | |
| Gender | |||
| Male | 47 (35.9%) | 84 (64.1%) | 0.0736 |
| Female | 45 (26.3%) | 126 (73.7%) | |
| Marital Status | |||
| Married | 23 (33.8%) | 45 (66.2%) | 0.6802 |
| Single | 56 (29.3%) | 135 (70.7%) | |
| Widowed | 5 (41.7%) | 7 (58.3%) | |
| Divorced | 8 (25.8%) | 23 (74.2%) | |
| Experience of Staying at an Acute Psychiatric Ward | |||
| Yes | 43 (50.6%) | 42 (49.4%) | <0.0001 |
| No | 49 (22.6%) | 168 (77.4%) | |
| CMCTRS Score | Hospitalization (n = 210) | Other-Option (n = 92) | p-Value |
|---|---|---|---|
| Rating A: Dangerousness | 3.3 (1.3) | 2.2 (1.2) | <0.0001 |
| 1 (Less) | 24 (45.3%) | 29 (54.7%) | |
| 2 | 41 (55.4%) | 33 (44.6%) | |
| 3 | 38 (71.7%) | 15 (28.3%) | |
| 4 | 54 (85.7%) | 9 (14.3%) | |
| 5 (Greater) | 53 (89.8%) | 6 (10.2%) | |
| Rating B: Support System | 2.6 (1.3) | 1.9 (1.1) | <0.0001 |
| 1 (Higher) | 55 (57.9%) | 40 (42.1%) | |
| 2 | 60 (64.5%) | 33 (35.5%) | |
| 3 | 20 (74.1%) | 7 (25.9%) | |
| 4 | 67 (88.2%) | 9 (11.8%) | |
| 5 (Poor) | 8 (72.7%) | 3 (27.3%) | |
| Rating B: Ability to Cooperate | 3.3 (1.1) | 2.3 (1.1) | <0.0001 |
| 1 (More) | 13 (33.3%) | 26 (66.7%) | |
| 2 | 19 (44.2%) | 24 (55.8%) | |
| 3 | 104 (77.6%) | 30 (22.4%) | |
| 4 | 36 (80.0%) | 9 (20.0%) | |
| 5 (Lower) | 38 (92.7%) | 3 (7.3%) |
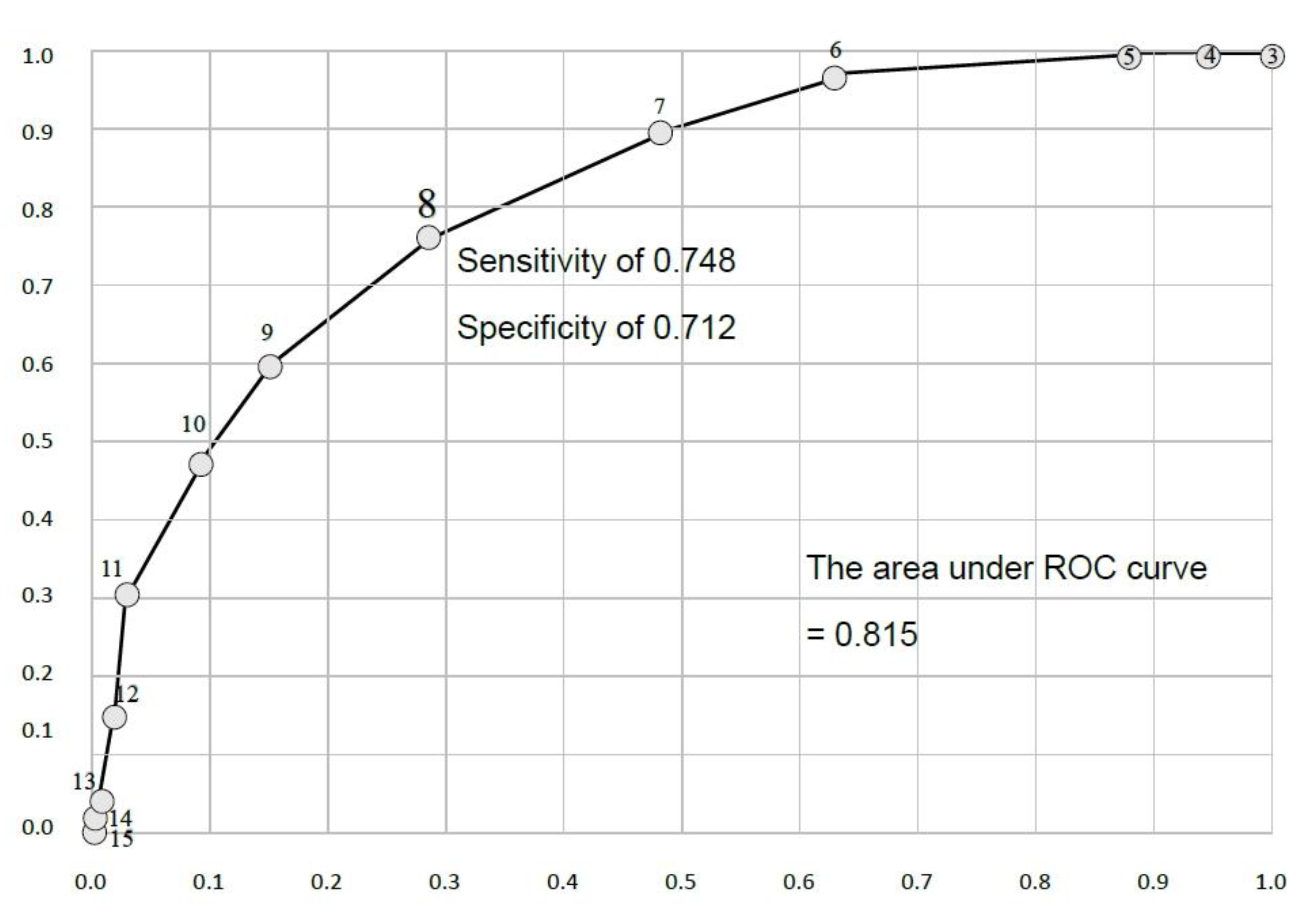
| CMCTRS Score | Sensitivity | Specificity | Youden Index |
|---|---|---|---|
| 3 | 1.000 | 0.000 | 1.000 |
| 4 | 1.000 | 0.054 | 1.054 |
| 5 | 0.990 | 0.130 | 1.121 |
| 6 | 0.962 | 0.370 | 1.331 |
| 7 | 0.890 | 0.522 | 1.412 |
| 8 | 0.762 | 0.717 | 1.479 |
| 9 | 0.595 | 0.848 | 1.443 |
| 10 | 0.471 | 0.913 | 1.384 |
| 11 | 0.314 | 0.967 | 1.282 |
| 12 | 0.157 | 0.978 | 1.135 |
| 13 | 0.062 | 0.989 | 1.051 |
| 14 | 0.033 | 1.000 | 1.033 |
| 15 | 0.005 | 1.000 | 1.005 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ting, S.-Y.; Lan, T.-H.; Shen, L.-J.; Lin, C.-Y.; Lee, S.-K.; Ma, W.-F. The Chinese Mandarin Version of the Crisis Triage Rating Scale for Taiwanese with Mental Illness to Compulsory Hospitalization. Int. J. Environ. Res. Public Health 2021, 18, 13392. https://doi.org/10.3390/ijerph182413392
Ting S-Y, Lan T-H, Shen L-J, Lin C-Y, Lee S-K, Ma W-F. The Chinese Mandarin Version of the Crisis Triage Rating Scale for Taiwanese with Mental Illness to Compulsory Hospitalization. International Journal of Environmental Research and Public Health. 2021; 18(24):13392. https://doi.org/10.3390/ijerph182413392
Chicago/Turabian StyleTing, Shuo-Yen, Tsuo-Hung Lan, Lih-Jong Shen, Chun-Yuan Lin, Shih-Kai Lee, and Wei-Fen Ma. 2021. "The Chinese Mandarin Version of the Crisis Triage Rating Scale for Taiwanese with Mental Illness to Compulsory Hospitalization" International Journal of Environmental Research and Public Health 18, no. 24: 13392. https://doi.org/10.3390/ijerph182413392
APA StyleTing, S.-Y., Lan, T.-H., Shen, L.-J., Lin, C.-Y., Lee, S.-K., & Ma, W.-F. (2021). The Chinese Mandarin Version of the Crisis Triage Rating Scale for Taiwanese with Mental Illness to Compulsory Hospitalization. International Journal of Environmental Research and Public Health, 18(24), 13392. https://doi.org/10.3390/ijerph182413392






