Assessment of Health Professionals’ Attitudes on Radiation Protection Measures
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Research Instrument
- A:
- Overall Knowledge of Radiation Protection Safety (12 questions).
- A1:
- Basic Knowledge of Radiation Protection Safety (6 questions).
- A2:
- Advanced Knowledge of Radiation Protection Safety (6 questions).
- B:
- Occupational Safety and Health—Radiation Protection Safety equipment (5 questions).
- C:
- Negative Attitude towards Radiation Protection Safety equipment (6 questions).
- C1:
- Discomfort of wearing personal Radiation Protection Safety equipment (4 questions).
- C2:
- Discomfort from unclean personal Radiation Protection Safety equipment (2 questions).
- D:
- Knowledge of Dosimetry (4 questions).
- E:
- Negative feelings due to accidental Radiation Exposure (6 questions).
- E1:
- Fear and anger due to unintentional Radiation Exposure (4 questions).
- E2:
- Guilt for being unintentionally exposed to radiation (2 questions).
- F:
- Psychosomatic symptoms due to negative feelings related to radiation (4 questions).
- G:
- Misconceptions about Radiation—Radiation Protection Safety (6 questions).
- G1:
- Misconceptions about Radiation (4 questions).
- G2:
- Misconceptions about the importance and necessity of Radiation Protection Safety (2 questions).
2.3. Statistical Analysis
3. Results
3.1. Descriptive Analysis of the Sample
3.2. Analysis of the Level of Questionnaire’s Dimensions
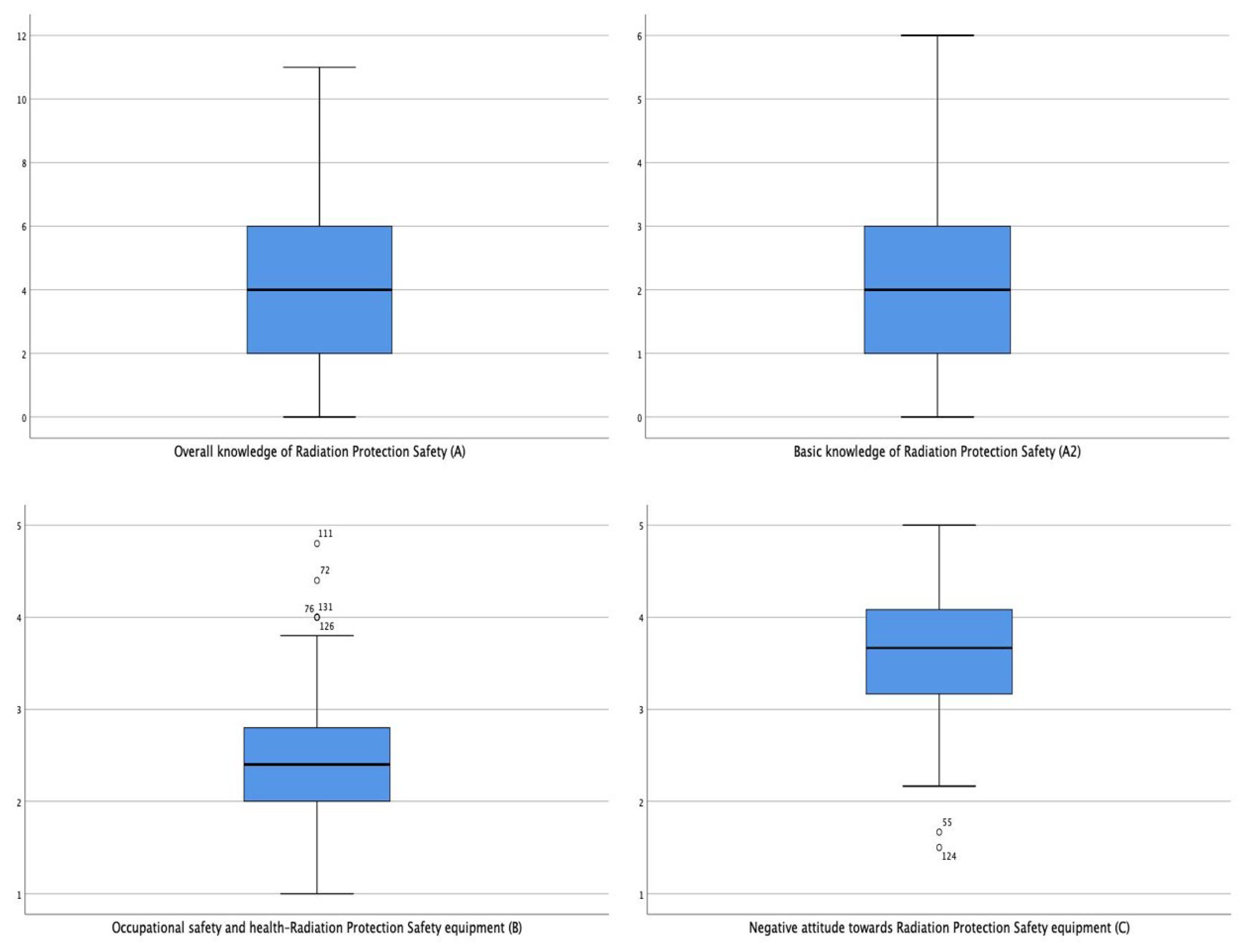
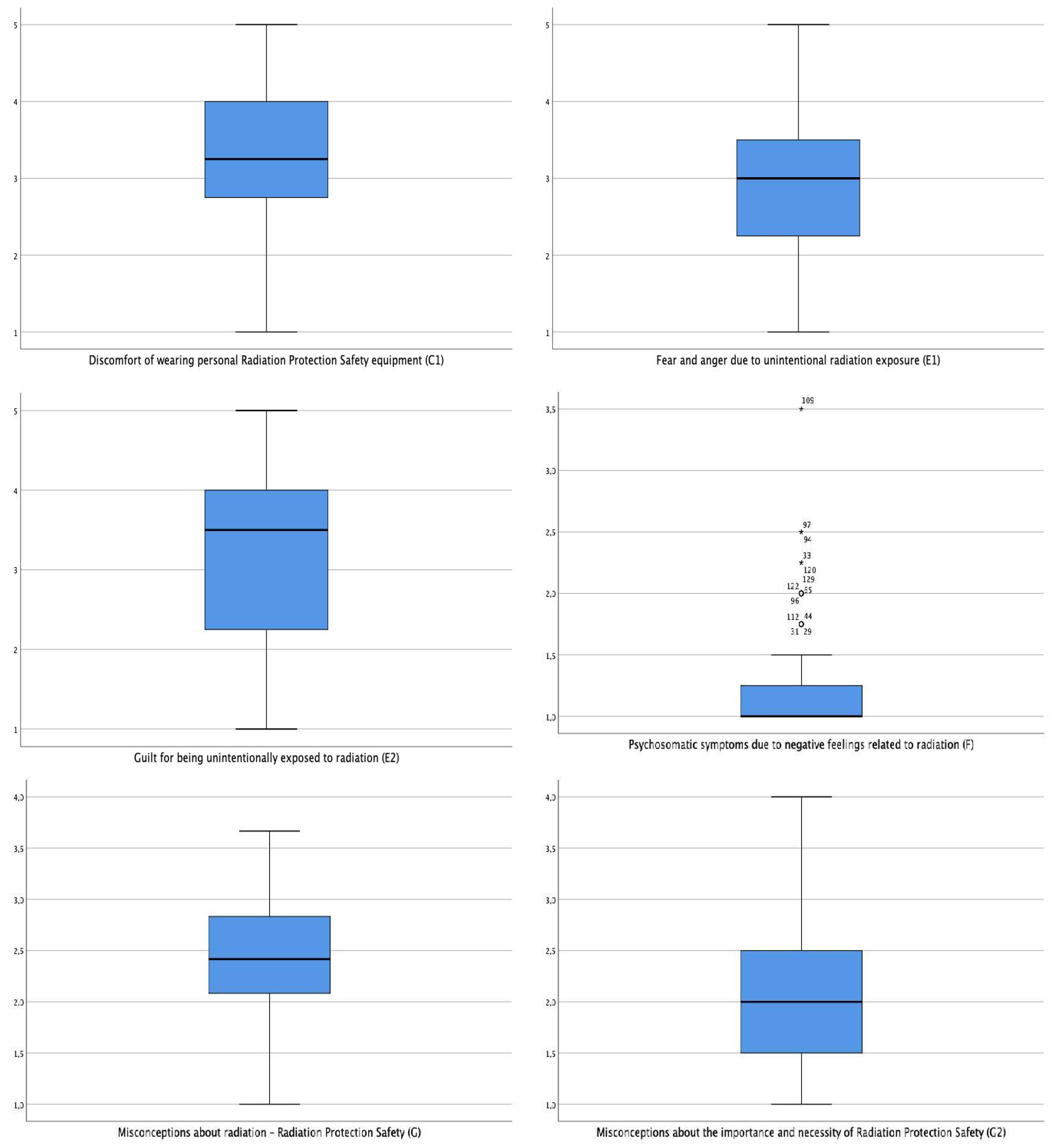
- A:
- it was found that the observed value (value = 4.00) was statistically significantly lower than the control value (value = 6.00). This finding indicates that the level of health professionals’ comprehensive knowledge on radiation protection was not satisfactory.
- A1:
- the test showed that the observed value (value = 2.00) was statistically significantly lower than the control value (value = 3.00). This finding indicates that the level of health professionals’ comprehensive knowledge on radiation protection was not satisfactory.
- A2:
- it was found that the observed value (value = 2.00) was statistically significantly lower than the control value (value = 3.00). This finding shows that the level of health professionals’ specialist knowledge on radiation protection was not satisfactory.
- C:
- it was found that the observed value (value = 3.65) was statistically significantly higher than the control value (value = 3.00), which indicates that health professionals tended to have a negative attitude towards radiation protection equipment.
- C1:
- the test revealed that the observed value (value = 3.50) was statistically significantly higher than the control value (value = 3.00), which shows that health professionals tended to experience discomfort when they needed to wear their radiation protection equipment.
- C2:
- the test showed that the observed value (value = 4.00) was statistically significantly higher than the control value (value = 3.00). This result indicates that health professionals did not consider the radiation protection equipment suitable for use in terms of its level of sanitation and cleanliness.
- D:
- it was found that the observed value (value = 4.00) was statistically significantly higher than the control value (value = 2.00). This finding indicates that health professionals’ knowledge was satisfactory in terms of individual dosimeter use.
- F:
- the test showed that the observed value (value = 1.00) was statistically significantly lower than the control value (value = 2.30). This result indicates that radiation-related negative feelings did not appear to be embodied by health professionals.
- G:
- it was found that the observed value (value = 0.50) was statistically significantly lower than the control value (value = 3.00). This finding shows that health professionals had fewer misconceptions about radiation and radiation protection.
3.3. Demographic Characteristics Impact on Selected Dimensions
3.3.1. Gender Factor
3.3.2. Education Level Factor
3.3.3. Age Groups Factor
3.3.4. Previous Experience Factor
- A:
- the post hoc analysis identified statistically significant differences for the pair (11–20) vs. (21–30), where employees with less previous experience had a higher level of radiation protection knowledge.
- F:
- the post hoc analysis which followed revealed statistically significant differences in the pairs (i) (0–10) vs. (21–30) and (ii) (11–20) vs. (21–30). That means that less experienced employees were more likely to somatise negative emotions due to radiation exposure than more experienced colleagues in both cases checked.
- G2:
- the following post hoc analysis showed that statistically significant differences existed only for the pair (11–20) vs. (31–40), meaning that, employees with less previous experience had fewer misconceptions about the necessity for radiation protection than those with more experience.
3.3.5. Number of Children Factor
4. Discussion
Limitations of Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations Scientific Committee on the Effects of Atomic Radiation. Sources and Effects of Ionizing Radiation, Volume II; UNSCEAR Publication: New York, NY, USA, 2018; Available online: https://www.unscear.org/docs/reports/2008/11-80076_Report_2008_Annex_D.pdf (accessed on 10 January 2020).
- Sanders, R.; Koval, K.J.; Di Pasquale, T.; Schmelling, G.; Stenzler, S.; Ross, E. Exposure of the orthopedic surgeon to radiation. J Bone Jt. Surg. Am. 1993, 75, 326–330. [Google Scholar] [CrossRef]
- Tsalavoutas, I.A.; Tsapaki, V.; Kaliakmanis, A.; Pneumaticos, S.; Tsoronis, F.; Koulentianos, E. Estimation of radiation doses to patients and surgeons from various fluoroscopically guided orthopedic surgeries. Radiat. Prot. Dosim. 2008, 128, 112–119. [Google Scholar] [CrossRef]
- Giordano, B.D.; Baumhauer, J.F.; Morgan, T.L.; Rechtine, R. Patient and surgeon radiation exposure: Comparison of standard and mini-C-arm fluoroscopy. J. Bone Jt. Surg. Am. 2009, 91, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Giordano, B.D.; Baumhauer, J.F.; Morgan, T.L.; Rechtine, R. Cervical spine imaging using standard C-arm fluoroscopy: Patient and surgeon exposure to ionising radiation. Spine 2008, 33, 1970–1976. [Google Scholar] [CrossRef]
- Giordano, B.D.; Grauer, J.N.; Miller, C.P.; Morgan, T.L.; Rechtine, R. Radiation exposure issues in orthopaedics. J. Bone Jt. Surg. Am. 2011, 93, e69. [Google Scholar] [CrossRef] [PubMed]
- United Nations Scientific Committee on the Effects of Atomic Radiation. Report Sources, Effects and Risks of Ionizing Radiation, Report to the General Assembly, Scientific Annexes A and B; UNSCEAR Publication: New York, NY, USA, 2020; Available online: https://www.unscear.org/docs/publications/2019/UNSCEAR_2019_Report.pdf (accessed on 12 December 2021).
- Brenner, D.J.; Doll, R.; Goodhead, D.T.; Hall, E.J.; Charles, E.L.; John, B.L.; Luvin, J.H.; Preston, D.L.; Preson, R.H.; Puskin, J.S.; et al. Cancer risks attributable to low doses of ionizing radiation: Assessing what we really know. Proc. Natl. Acad. Sci. USA 2003, 100, 13761–13766. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mehlman, C.T.; Di Pasquale, T.G. Radiation exposure to the orthopaedic surgical team during fluoroscopy: “How far away is far enough”? J. Orthop. Trauma 1997, 11, 392–398. [Google Scholar] [CrossRef]
- Bouraoui, S.; Mougou, S.; Drira, A.; Tabka, F.; Bouali, N.; Mrizek, N.; Elghezal, H.; Saad, A. A Cytogenetic approach to the effects of low levels of ionizing radiation (IR) on the exposed Tunisian hospital workers. Int. J. Occup. Med. Environ. Health 2013, 26, 144–154. [Google Scholar] [CrossRef]
- Cardoso, R.S.; Takahashi-Hyodo, S.; Peitl, P., Jr.; Ghilardi-Neto, T.; Sakamoto-Hojo, E.T. Evaluation of chromosomal aberrations, micronuclei, and sister chromatic exchanges in hospital workers chronically exposed to ionising radiation. Teratog. Carcinog. Mutagen. 2001, 21, 431–439. [Google Scholar] [CrossRef]
- Dobrzynska, M.M.; Pachocki, K.A.; Gajowik, A.; Radzikowska, J.; Sackiewicz, A. The effect occupational exposure to ionising radiation on the DNA damage in peripheral blood leukocytes of nuclear medicine personnel. J. Occup. Health 2014, 56, 379–386. [Google Scholar] [CrossRef] [Green Version]
- Doukali, H.; Ben Salah, G.; Ben Rhouma, B.; Hajjaji, M.; Jaouadi, A.; Belguith-Mahfouth, N.; Masmoudi, M.L.; Ammar-Keskes, L.; Hassen Kamoun, H. Cytogenetic monitoring of hospital staff exposed to ionising radiation: Optimise protocol considering DNA repair genes variability. Int. J. Radiat. Biol. 2017, 93, 1283–1288. [Google Scholar] [CrossRef]
- Gaetani, S.; Monaco, F.; Bracci, M.; Ciarapica, V.; Impollonia, G.; Valentino, M.; Tomasetti, M.; Santarelli, L.; Amati, M. DNA damage response in workers exposed to low-dose ionising radiation. Occup. Environ. Med. 2018, 75, 724–729. [Google Scholar] [CrossRef]
- Garaj-Vrhovac, V.; Kopjar, N. The alkaline Comet assay as biomarker in assessment of DNA damage in medical personnel occupationally exposed to ionising radiation. Mutagenesis 2018, 18, 265–271. [Google Scholar] [CrossRef] [Green Version]
- Guerci, A.M.; Grillo, C.A.; Dulout, F.N.; Seoane, A.I. Assessment of genotoxic damage in lymphocytes of hospital workers exposed to ionising radiation in Argentina. Arch. Environ. Occup. Health 2006, 61, 163–169. [Google Scholar] [CrossRef]
- Kopjar, N.; Garaj-Vrhovac, V. Assessment of DNA damage in nuclear medicine personnel-comparative study with the alkaline comet assay and the chromosome aberration test. Int. J. Hyg. Environ. Health 2005, 208, 179–191. [Google Scholar] [CrossRef] [PubMed]
- Kumar, D.; Kumari, S.; Salian, S.R.; Uppangala, S.; Kalthur, G.; Challapalli, S.; Chandraguthi, S.G.; Pratap Kumar, P.; Adiga, S.K. Genetic instability in lymphocytes is associated with blood plasma antioxidant levels in health care workers occupationally exposed to ionising radiation. Int. J. Toxicol. 2015, 35, 327–335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sari-Minodier, I.; Orsiere, T.; Auquier, P.; Martin, F.; Botta, A. Cytogenetic monitoring by use of the micronucleus assay among hospital workers exposed to low doses of ionising radiation. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 2007, 629, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Wojewodzka, M.; Kruszewski, M.; Iwanenko, T.; Collins, A.R.; Szumiel, I. Application of the comet assay for monitoring DNA damage in workers exposed to chronic low-dose irradiation I. Strand breakage. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 1998, 416, 21–35. [Google Scholar] [CrossRef]
- Zakeri, F.; Hirobe, T. A cytogenetic approach to the effects of low levels of ionising radiations on occupationally exposed individuals. Eur. J. Radiol. 2010, 73, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Roguin, A.; Goldstein, J.; Bar, O.; Goldstein, J.A. Brain and neck tumors among physicians performing interventional procedures. Am. J. Cardiol. 2013, 111, 1368–1372. [Google Scholar] [CrossRef]
- Chartier, H.; Fassier, P.; Leuraud, K.; Jacob, S.; Baudin, C.; Laurier, D.; Bernier, M.O. Occupational low-dose irradiation and cancer risk among medical radiation workers. Occup. Med. 2020, 70, 476–484. [Google Scholar] [CrossRef]
- Wakeford, R. Radiation in the workplace-a review of studies of the risks of occupational exposure to ionising radiation. J. Radiol. Prot. 2009, 29, 61–79. [Google Scholar] [CrossRef]
- Blakely, E.A.; Kleiman, N.J.; Neriishi, K.; Chodick, G.; Chylack, L.T.; Cucinotta, F.A.; Minamoto, A.; Nakashima, E.; Kumagami, T.; Kitaoka, T.; et al. Radiation cataractogenesis: Epidemiology and biology. Radiat. Res. 2010, 173, 709–717. Available online: https://www.jstor.org/stable/40605562 (accessed on 15 July 2021). [CrossRef] [PubMed]
- Shore, R.E.; Neriishi, K.; Nakashima, E. Epidemiological studies of cataract risk at low to moderate radiation doses: (Not) seeing is believing. Radiat. Res. 2010, 174, 889–894. [Google Scholar] [CrossRef] [Green Version]
- European Nuclear Safety Regulators Group. Greece Nuclear Regulatory Authority 2020. Available online: https://www.ensreg.eu/country-profile/Greece (accessed on 12 December 2021).
- Department of Health. Council Directive 2013/59/Euratom Laying down Basic Safety Standards for Protection against the Dangers Arising from Exposure. Off. J. Eur. Union 2014, 13, 1–73. Available online: https://www.gov.ie/en/news/91ed22-council-directive-201359euratom-laying-down-basic-safety-standards-f (accessed on 12 December 2021).
- Sharma, R.S.; Karjodkar, R.F.; Sansare, P.K.; Saalim, M.; Mishra, D.I.; Johaley, S.; Goyal, N.S. Attitude and awareness of generalp towards radiation hazards and safety: An institutional study. Indian J. Dent. Res. 2019, 30, 27–30. [Google Scholar] [CrossRef] [PubMed]
- Ricketts, M.L.; Baerlocher, M.O.; Murray, R.; Asch, M.R.; Myers, A. Perception of radiation exposure and risk among patients, medical students, and referring physicians at a Tertiary Care Community Hospital. Can. Assoc. Radiol. J. 2013, 64, 208–212. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freudenberg, L.S.; Beyer, T. Subjective perception of radiation risk. J. Nucl. Med. 2011, 52, 29S–35S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okafor, C.H.; Ugwu, A.C.; Okon, I.E. Effects of patient safety culture on patient satisfaction with radiological services in Nigerian radiodiagnostic practice. J. Patient Exp. 2018, 5, 267–271. [Google Scholar] [CrossRef]
- Chatzis, A.; Brilakis, E.; Papadopoulou, D.; Giannouli, V.; Stamouli, M.A.; Goula, A.; Sarris, M.; Soulis, S. Beliefs and behaviours of radiographers and other health professionals concerning radiation protection safety in a high-volume Greek public hospital. Development of a new measuring instrument. Radiography 2021, 27, 1038–1043, Online ahead of printm. [Google Scholar] [CrossRef]
- Son, K.B.; Lee, T.K.; Kim, J.S.; Lee, S.O. Lack of radiation protection for endoscopists performing endoscopic retrograde cholangiopancreatography. Korean J. Gastroenterol. 2011, 58, 93–99. [Google Scholar] [CrossRef] [Green Version]
- Saroki, A.J.; Wijdicks, C.; Philippon, M.J.; Bedi, A. Orthopaedic surgeons’ use and knowledge of ionising radiation during surgical treatment for femoroacetabular impingement. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 3962–3970. [Google Scholar] [CrossRef] [PubMed]
- Tok, A.; Akbas, A.; Aytan, N.; Aliskan, T.; Cicekbilek, I.; Kaba, M.; Tepeler, A. Are the urology operating room personnel aware about the ionising radiation? Int. Braz J. Urol. 2015, 41, 982–989. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brun, A.; Alcaraz, M.R.; Bourrelly, M.; Dalivoust, G.; Gazazian, G.; Boufercha, R.; Lehucher-Michel, M.P.; Sari-Minodier, I. Radiation Protection for Surgeons and Anesthetists: Practices and knowledge before and after Training. J. Radiol. Prot. 2018, 38, 175. Available online: https://hal-amu.archives-ouvertes.fr/hal-02058180/document (accessed on 10 January 2020). [CrossRef]
- Paolicchi, F.; Miniati, F.; Bastiani, L.; Faggioni, L.; Ciaramella, A.; Sottocornola, C.; Dionisi, C.; Caramella, D. Assessment of radiation protection awareness and knowledge about radiological examination doses among Italian radiographers. Insights Imaging 2016, 7, 233–242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, S.; Yang, Y. Factors affecting radiation protection behaviors among emergency room nurses. Int. J. Environ. Res. Public Health 2021, 18, 6238. [Google Scholar] [CrossRef]
- Klein, L.W.; Miller, D.L.; Balter, S.; Laskey, W.; Haines, D.; Norbash, A.; Mauro, M.A.; Goldstein, J.A. Occupational health hazards in the interventional laboratory: Time for a safer environment. J. Radiol. Nurs. 2010, 29, 75–82. [Google Scholar] [CrossRef]
- Goldstein, J.A.; Balter, S.; Cowley, M.; Hodgson, J.; Klein, L.W. Occupational hazards of interventional cardiologists: Prevalence of orthopedic health problems in contemporary practice. Catheter. Cardiovasc. Interv. 2004, 63, 407–411. [Google Scholar] [CrossRef]
- Cremen, S.A.; McNulty, J.P. The availability of appropriately fitting personal protective aprons and jackets for angiographic and interventional radiology personnel. Radiography 2014, 20, 126–130. [Google Scholar] [CrossRef]
- McCaffrey, J.P.; Tessier, F.; Shen, H. Radiation shielding materials and radiation scatter effects for interventional radiology (IR) physicians. Med. Phys. 2012, 39, 4537–4546. [Google Scholar] [CrossRef]
- MohdRidzwan, S.F.; Bhoo-Pathy, N.; Isahak, M.; Wee, L.H. Perceptions on radioprotective garment usage and underlying reasons for non-adherence among medical radiation workers from public hospitals in a middle-income Asian setting: A qualitative exploration. Heliyon 2019, 5, e02478. [Google Scholar] [CrossRef] [Green Version]
- Bushberg, J.T.; Seibert, J.A.; Leidholdt, E.M.J.; Boone, J.M. The Essential Physics of Medical Imaging, 3rd ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2012; p. 1048. [Google Scholar]
- Simon, S.L. Organ-specific external dose coefficients and protective apron transmission factors for historical dose reconstruction for medical personnel. Health Phys. 2011, 101, 13–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Christodoulou, E.G.; Goodsitt, M.M.; Larson, S.C.; Darner, K.L.; Satti, J.; Chan, H.P. Evaluation of the transmitted exposure through lead equivalent aprons used in a radiology department, including the contribution from backscatter. Med. Phys. 2003, 30, 1033–1038. [Google Scholar] [CrossRef] [Green Version]
- Alavi, S.S.; Dabbagh, S.T.; Abbasi, M.; Mehrdad, R. Radiation protection knowledge, attitude and practice (RP-KAP) as predictors of job stress among radiation workers in Tehran Province, Iran. Iran. Red Crescent Med. J. 2016, 18, e29394. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reisi, M.; Javadzade, S.H.; Sharifirad, G. Knowledge, attitudes, and practice of breast self-examination among female health workers in Isfahan, Iran. J. Educ. Health Promot. 2013, 2, 46. [Google Scholar] [CrossRef]
- Dickety, N.; Weyman, A.; Marlow, P. Measuring Workplace Transport Safety Performance; Health and Safety Laboratory: Buxton, UK, 2004. Available online: https://www.hse.gov.uk/research/hsl_pdf/2005/hsl0503.pdf (accessed on 7 June 2021).
- Kiani, F.; Samavtyan, H.; Poorabdiyan, S.; Jafari, E. How Safety Trainings Decrease Perceived Job Stress: The Effects of Improvement in Employees’ Attitude toward Safety Issues. Far East J. Psychol. Bus. 2012, 6, 46–58. Available online: https://ideas.repec.org/a/fej/articl/v6ay2012i4p46-58.html (accessed on 15 July 2021).
- Seifi, D.; HadiHasanzadeh, H.; Bitarafan-Rajabi, A.; Emadi, A.; Bokharaeian, M.; Shabani, F.; Masoumi, H.; Moshfegh, S.; Khani, T.; Pursamimi, M.; et al. Knowledge, Attitude and Practice of Nuclear Medicine Staff towards Radiation Protection. Iran. J. Nucl. Med. 2019, 27, 39–46. Available online: https://irjnm.tums.ac.ir/article_33700_3be44a9e89afc28bc20f149c8920200c.pdf (accessed on 9 June 2021). [CrossRef]
- Mojiri, M.; Moghimbeigi, A. Awareness and attitude of radiographers towards radiation protection. J. Paramed. Sci. 2011, 2, 1–5. [Google Scholar]
- Rahman, N.; Dhakam, S.; Shafqut, A.; Qadir, S.; Tipoo, F.A. Knowledge and practice of radiation safety among invasive cardiologists. J. Pak. Med. Assoc. 2008, 58, 119–122. [Google Scholar] [PubMed]
- Alavi, S.S.; Dabbagh, S.T.; Abbasi, M.; Mehrdad, R. Job satisfaction and its relationship to radiation protection knowledge, attitude and practice (RPKAP) of Iranian radiation workers. East. Mediterr. Health J. 2017, 22, 727–734. [Google Scholar] [CrossRef]
- Do, K.H. General principles of radiation protection in fields of di-agnostic medical exposure. J. Korean Med. Sci. 2016, 31, S6–S9. [Google Scholar] [CrossRef] [PubMed]
| Kolmogorov–Smirnov a | |||
|---|---|---|---|
| Statistic | Df | Sig. | |
| A * | 0.144 | 116 | <0.001 |
| A2 * | 0.167 | 116 | <0.001 |
| Β * | 0.126 | 116 | <0.001 |
| C * | 0.066 | 116 | 0.200 |
| C1 * | 0.098 | 116 | 0.008 |
| Ε1 * | 0.078 | 116 | 0.078 |
| Ε2 * | 0.189 | 116 | <0.001 |
| F * | 0.415 | 116 | <0.001 |
| G * | 0.097 | 116 | 0.009 |
| G2 * | 0.133 | 116 | <0.001 |
| Frequency | Percent (%) | ||
|---|---|---|---|
| Gender | Male | 72 | 54.5 |
| Female | 60 | 45.5 | |
| Age Group | 25–34 | 17 | 12.9 |
| 35–44 | 54 | 40.9 | |
| 45–54 | 45 | 34.1 | |
| 55+ | 16 | 12.1 | |
| Education Level | Secondary Education | 29 | 22.0 |
| Technological Education | 21 | 15.9 | |
| University Education | 82 | 62.1 | |
| Number of Children | 1–2 | 64 | 48.5 |
| 2+ | 66 | 50.0 | |
| Missing Values | 2 | 1.5 | |
| Experience (in years) | 0–10 | 42 | 31.8 |
| 11–20 | 43 | 32.6 | |
| 21–30 | 29 | 22.0 | |
| 31–40 | 18 | 13.6 | |
| Total | 132 | 100.0 | |
| Dimensions | Test Value | Observed Value | Test p-Value |
|---|---|---|---|
| A * | 6.00 | 4.00 | W = 931.50 p < 0.001 ** |
| A1 * | 3.00 | 2.00 | W = 1364.50 p < 0.001 ** |
| A2 * | 3.00 | 2.00 | W = 611.00 p < 0.001 ** |
| B * | 3.00 | 2.41 | t (131) = −9.525 p < 0.001 ** |
| C * | 3.00 | 3.65 | t (131) =9.796 p < 0.001 ** |
| C1 * | 3.00 | 3.50 | W = 5508.00 p < 0.001 ** |
| C2 * | 3.00 | 4.00 | W = 6936.00 p < 0.001 |
| D * | 2.00 | 4.00 | W = 6973.00 p < 0.001 ** |
| E * | 3.00 | 3.00 | W = 3736.50 p = 0.729 |
| Ε1 * | 3.00 | 2.89 | t(131) = −1.231 p = 0.220 |
| Ε2 * | 3.00 | 3.50 | W = 4093.50 p = 0.292 |
| F * | 3.00 | 1.00 | W = 4.50 p < 0.001 ** |
| G * | 3.00 | 2.50 | W = 432.50 p < 0.001 ** |
| Dimensions | Gender | N | Mean Rank | Test p-Value |
|---|---|---|---|---|
| C * | Male | 72 | 58.43 | U = 1579.00 p = 0.008 ** |
| Female | 60 | 76.18 | ||
| C1 * | Male | 72 | 58.18 | U = 1561.00 p = 0.006 ** |
| Female | 60 | 76.48 | ||
| G * | Male | 72 | 56.45 | U = 1436.50 p = 0.001 ** |
| Female | 60 | 78.56 | ||
| G2 * | Male | 72 | 57.68 | U = 1525.00 p = 0.003 ** |
| Female | 60 | 77.08 |
| Dimensions | Level of Education | N | Mean Rank | Test p-Value | Post hoc Analysis |
|---|---|---|---|---|---|
| A * | Secondary education | 26 | 57.35 | H = 1.308 p = 0.520 | - |
| Technological education | 21 | 64.48 | |||
| University education | 81 | 66.80 | |||
| A2 * | Secondary education | 20 | 62.28 | H = 0.524 p = 0.769 | - |
| Technological education | 20 | 55.25 | |||
| University education | 76 | 58.26 | |||
| C * | Secondary education | 28 | 75.91 | H = 2.863 p = 0.239 | - |
| Technological education | 21 | 68.10 | |||
| University education | 82 | 62.08 | |||
| G * | Secondary education | 28 | 88.18 | H = 12.458 p = 0.002 | test statistic = 28.965 p = 0.001 ** |
| Technological education | 21 | 62.93 | |||
| University education | 82 | 5.21 |
| Dimensions | Age Group | N | Mean Rank | Test p-Value | Post hoc Analysis |
|---|---|---|---|---|---|
| Ε | 25–34 | 17 | 53.29 | H = 3.651 p = 0.302 | - |
| 35–44 | 54 | 72.69 | |||
| 45–54 | 45 | 65.46 | |||
| 55+ | 16 | 62.59 | |||
| F | 25–34 | 17 | 75.38 | H = 14.348 p = 0.002 | test statistic = 27.139 p = 0.001 (35–44) − (55 + ) ** |
| 35–44 | 54 | 75.14 | |||
| 45–54 | 45 | 59.36 | |||
| 55+ | 16 | 48.00 |
| Dimensions | Years of Experience | N | Mean Rank | Test p-Value | Post hoc Analysis |
|---|---|---|---|---|---|
| A * | 0–10 | 41 | 64.32 | H = 8.478 p = 0.037 | test statistic = 24.937 p = 0.029 (11–20) − (21–30) ** |
| 11–20 | 42 | 73.38 | |||
| 21–30 | 29 | 48.45 | |||
| 31–40 | 16 | 70.75 | |||
| 11–20 | 39 | 66.44 | |||
| 21–30 | 25 | 45.82 | |||
| 31–40 | 13 | 74.38 | |||
| C * | 0–10 | 42 | 66.24 | H = 3.313 p = 0.958 | - |
| 11–20 | 43 | 65.31 | |||
| 21–30 | 29 | 69.84 | |||
| 31–40 | 18 | 64.56 | |||
| Ε * | 0–10 | 42 | 56,23 | H = 7.042 p = 0.071 | - |
| 11–20 | 43 | 75.85 | |||
| 21–30 | 29 | 61.91 | |||
| 31–40 | 18 | 75.53 | |||
| F * | 0–10 | 42 | 72.74 | H = 13.784 p = 0.003 | test statistic = 22.273 p = 0.033 (0–10) − (21–30) ** test statistic = 22.232 p = 0.013 (11–20) − (21–30) ** |
| 11–20 | 43 | 74.70 | |||
| 21–30 | 29 | 52.47 | |||
| 31–40 | 18 | 54.97 | |||
| G2 * | 0–10 | 42 | 71.80 | H = 8.395 p = 0.039 | test statistic = −27.913 p = 0.049 (11–20) − (31–40) ** |
| 11–20 | 43 | 54.70 | |||
| 21–30 | 29 | 66.33 | |||
| 31–40 | 18 | 82.61 |
| Dimensions | Number of Children | N | Mean Rank | Test p-Value |
|---|---|---|---|---|
| F * | 1–2 | 64 | 71.98 | U = 1697.00 p = 0.013 ** |
| 3+ | 66 | 59.21 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goula, A.; Chatzis, A.; Stamouli, M.-A.; Kelesi, M.; Kaba, E.; Brilakis, E. Assessment of Health Professionals’ Attitudes on Radiation Protection Measures. Int. J. Environ. Res. Public Health 2021, 18, 13380. https://doi.org/10.3390/ijerph182413380
Goula A, Chatzis A, Stamouli M-A, Kelesi M, Kaba E, Brilakis E. Assessment of Health Professionals’ Attitudes on Radiation Protection Measures. International Journal of Environmental Research and Public Health. 2021; 18(24):13380. https://doi.org/10.3390/ijerph182413380
Chicago/Turabian StyleGoula, Aspasia, Athanasios Chatzis, Maria-Aggeliki Stamouli, Martha Kelesi, Evridiki Kaba, and Emmanouil Brilakis. 2021. "Assessment of Health Professionals’ Attitudes on Radiation Protection Measures" International Journal of Environmental Research and Public Health 18, no. 24: 13380. https://doi.org/10.3390/ijerph182413380
APA StyleGoula, A., Chatzis, A., Stamouli, M.-A., Kelesi, M., Kaba, E., & Brilakis, E. (2021). Assessment of Health Professionals’ Attitudes on Radiation Protection Measures. International Journal of Environmental Research and Public Health, 18(24), 13380. https://doi.org/10.3390/ijerph182413380









